Professional Documents
Culture Documents
The Thorax and Lungs - BATES
Uploaded by
sitalcoolkOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Thorax and Lungs - BATES
Uploaded by
sitalcoolkCopyright:
Available Formats
The Thorax and Lungs 1.
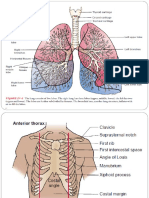
2nd intercostal space for needle insertion for tension pneumothorax; 4th intercostal space for chest tube insertion; T4 for lower margin of endotracheal tube on chest xray. T7-8 interspace as landmark for thoracentesis THE HEALTH HISTORY 2. Common or Concerning Symptoms Chest pain Shortness of breath (dyspnea) Wheezing Cough Blood-streaked sputum (hemoptysis)
3. A clenched fist over the sternum suggests angina pectoris; a finger pointing to a tender area on the chest wall suggests musculoskeletal pain; a hand moving from neck to epigastrum. suggests heartburn. 4. Anxiety is the most frequent cause of chest pain in children; costochondritis is also common. 5. Anxious patients may have episodic dyspnea during both rest and exercise, and hyperventilation, or rapid, shallow breathing. At other times, they may sigh frequently. 6. Wheezing suggests partial airway obstruction from secretions, tissue inflammation, or a foreign body.
7. Cough can be a symptom of left-sided heart failure. 8. Viral upper respiratory infections are the most common cause of acute cough; also consider acute bronchitis, pneumonia, left ventricular heart failure, asthma, foreign body. Postinfectious cough, bacterial sinusitis, asthma in subacute cough; postnasal drip, asthma, gastroesophageal reflux, chronic bronchitis, bronchiectasis in chronic cough.
9. Mucoid sputum is translucent, white, or gray; purulent sputum is yellowish or greenish. 10. Foul-smelling sputum in anaerobic lung abscess; tenacious(Sticking together) sputum in cystic fibrosis 11. Large volumes of purulent sputum in bronchiectasis or lung abscess. Diagnostically helpful symptoms include fever, chest pain, dyspnea, orthopnea, and wheezing. 12. Blood originating in the stomach is usually darker than blood from the respiratory tract and may be mixed with food particles. 13. ASSESSING READINESS TO QUIT SMOKING: THE 5 A'S i. ii. iii. iv. v. Ask about tobacco use. Advise to quit through clear, personalized messages. Assess willingness to quit. Assist to quit. Arrange follow-up and support.
14. Cyanosis signals hypoxia. Clubbing of the nails in lung abscesses, malignancy, congenital heart disease
15. Audible stridor, a high-pitched wheeze, is an ominous sign of airway obstruction in the larynx or trachea. 16. Inspiratory contraction of the sternomastoids and scalenes at rest signals severe difficulty in breathing. Lateral displacement of the trachea in pneumothorax, pleural effusion, or atelectasis 17. The AP diameter also may increase in chronic obstructive pulmonary disease (COPD), although evidence is not definitive.15 18. Retraction in severe asthma, COPD, or upper airway obstruction 19. Unilateral impairment or lagging of respiratory movement suggests disease of the underlying lung or pleura. 20. Intercostal tenderness over inflamed pleura 21. Bruises over a fractured rib 22. Although rare, sinus tracts usually indicate infection of the underlying pleura and lung (as in tuberculosis, actinomycosis). 23. Causes of unilateral decrease or delay in chest expansion include chronic fibrosis of the underlying lung or pleura, pleural effusion, lobar pneumonia, pleural pain with associated splinting, and unilateral bronchial obstruction. 24. Fremitus is decreased or absent when the voice is soft or when the transmission of vibrations from the larynx to the surface of the chest is impeded. Causes include a very thick chest wall; an obstructed bronchus; COPD; separation of the pleural surfaces by fluid (pleural effusion), fibrosis (pleural thickening), air (pneumothorax), or an infiltrating tumor. 25. Look for asymmetric fremitus: asymmetric decreased fremitus in unilateral pleural effusion, pneumothorax, neoplasm from decreased transmission of low frequency sounds; asymmetric increased fremitus in unilateral pneumonia from increased transmission.15 26. Percussion Notes and Their Characteristics Relative Relative Relative Example of Pathologic Intensity Pitch Duration Location Examples Flatness Dullness Resonance Hyperresonance Tympany Soft Medium Loud Very loud Loud High Short Thigh Large pleural effusion Liver Lobar pneumonia Healthy lung Simple chronic bronchitis Usually none COPD, pneumothorax Gastric air bubble Large or puffed-out pneumothorax cheek
Medium Medium Low Long Lower High* Longer
*
Distinguished mainly by its musical timbre. 27. Dullness replaces resonance when fluid or solid tissue replaces air-containing lung or occupies the pleural space beneath your percussing fingers. Examples include: lobar pneumonia, in which the alveoli are filled with fluid and blood cells; and pleural accumulations of serous fluid (pleural effusion), blood (hemothorax), pus (empyema), fibrous tissue, or tumor.
28. Generalized hyperresonance may be heard over the hyperinflated lungs of COPD or asthma, but is not a reliable sign. Unilateral hyperresonance suggests a large pneumothorax or possibly a large air-filled bulla in the lung. 29. An abnormally high level suggests pleural effusion, or a high diaphragm as in atelectasis or diaphragmatic paralysis. 30. Sounds from bedclothes, paper gowns, and the chest itself can generate confusion in auscultation. Hair on the chest may cause crackling sounds. Either press harder or wet the hair. If the patient is cold or tense, you may hear muscle contraction sounds muffled, low-pitched rumbling or roaring noises. A change in the patient's position may eliminate this noise. You can reproduce this sound on yourself by doing a Valsalva maneuver (straining down) as you listen to your own chest. 31. Breath sounds may be decreased when air flow is decreased (as in obstructive lung disease or muscular weakness) or when the transmission of sound is poor (as in pleural effusion, pneumothorax, or COPD). 32. Characteristics of Breath Sounds Intensity of Pitch of Locations Where Duration of Expiratory Expiratory Heard Normally Sounds Sound Sound Inspiratory sounds Soft Relatively low Over most of both Vesicular* last longer than lungs expiratory ones. Intermediate Intermediate Often in the 1st and BronchovesicularInspiratory and expiratory sounds 2nd interspaces are about equal. anteriorly and between the scapulae Expiratory sounds Loud Relatively high Over the manubrium, if Bronchial last longer than heard at all inspiratory ones. Inspiratory and Very loud Relatively high Over the trachea in the Tracheal expiratory sounds neck are about equal. * The thickness of the bars indicates intensity; the steeper their incline, the higher the pitch. 33. If bronchovesicular or bronchial breath sounds are heard in locations distant from those listed, suspect that air-filled lung has been replaced by fluid-filled or solid lung tissue. 34. A gap between inspiratory and expiratory sounds suggests bronchial breath sounds. 35. Fine late inspiratory crackles that persist from breath to breath suggest abnormal lung tissue.
36. Crackles may be from abnormalities of the lungs (pneumonia, fibrosis, early congestive heart failure) or of the airways (bronchitis, bronchiectasis). 37. Wheezes suggest narrowed airways, as in asthma, COPD, or bronchitis. 38. Rhonchi suggest secretions in large airways. 39. Clearing of crackles, wheezes, or rhonchi after coughing or position change suggests inspissated secretions, as in bronchitis or atelectasis. 40. Findings predictive of COPD include combinations of symptoms and signs, especially wheezing by self-report or examination, plus history of smoking, age, and decreased breath sounds. Diagnosis requires pulmonary function tests such as spirometry.
41. Adventitious or Added Breath Sounds16 Crackles (or Rales) Wheezes and Rhonchi Discontinuous Continuous Intermittent, nonmusical, and brief 250 msec, musical, prolonged (but not necessarily persisting throughout the respiratory cycle) Like dots in time Like dashes in time Fine crackles: soft, high-pitched, very Wheezes: relatively high-pitched (400 Hz) with brief (5-10 msec) hissing or shrill quality Coarse crackles: somewhat louder, lower in pitch, brief (20-30 msec) Rhonchi: relatively low-pitched (200 Hz) with snoring quality
42. Increased transmission of voice sounds suggests that air-filled lung has become airless. 43. Louder, clearer voice sounds are called bronchophony. 44. When ee is heard as ay, an E-to-A change (egophony) is present, as in lobar consolidation from pneumonia. The quality sounds nasal. 45. Louder, clearer whispered sounds are called whispered pectoriloquy. 46. Persons with severe COPD may prefer to sit leaning forward, with lips pursed during exhalation and arms supported on their knees or a table. 47. Tender pectoral muscles or costal cartilages corroborate, but do not prove, that chest pain has a musculoskeletal origin. 48. Dullness replaces resonance when fluid or solid tissue replaces air-containing lung or occupies the pleural space. Because pleural fluid usually sinks to the lowest part of the pleural space (posteriorly in a supine patient), only a very large effusion can be detected anteriorly. 49. The hyperresonance of COPD may totally replace cardiac dullness. 50. The dullness of right middle lobe pneumonia typically occurs behind the right breast. Unless you displace the breast, you may miss the abnormal percussion note. 51. A lung affected by COPD often displaces the upper border of the liver downward. It also lowers the level of diaphragmatic dullness posteriorly. 52. The walk test (Time an 8-foot walk at the patient's normal pace): Nondisabled older adults taking 5.6 seconds or longer are more likely to be disabled over time than those taking 3.1 seconds or fewer. Early intervention may prevent onset of subsequent disability.26 53. Patients older than 60 years with a forced expiratory time of 6 to 8 seconds are twice as likely to have COPD. 54. An increase in the local pain (distant from your hands) suggests rib fracture rather than just soft-tissue injury. Recording the Physical Examinationthe Thorax and Lungs a. Thorax is symmetric with good expansion. Lungs resonant. Breath sounds vesicular; no rales, wheezes, or rhonchi. Diaphragms descend 4 cm bilaterally. OR b. Thorax symmetric with moderate kyphosis and increased anteroposterior (AP) diameter, decreased expansion. Lungs are hyperresonant. Breath sounds distant with delayed expiratory phase and scattered expiratory wheezes. Fremitus decreased; no bronchophony, egophony, or whispered pectoriloquy. Diaphragms descend 2 cm bilaterally.
You might also like
- Nusing Skills Output (Nso)Document3 pagesNusing Skills Output (Nso)leroux2890No ratings yet
- Chapter 24 HomeworkDocument9 pagesChapter 24 HomeworkKvn4N6No ratings yet
- Chapter 55Document8 pagesChapter 55DelindaEvansNo ratings yet
- Physical Assessment Learning Guide Med SurgDocument4 pagesPhysical Assessment Learning Guide Med SurgTremain LinsonNo ratings yet
- Comprehensive Uworld ReviewDocument190 pagesComprehensive Uworld ReviewJoe JNo ratings yet
- Assessment of The Chest and LungsDocument46 pagesAssessment of The Chest and LungsSumathi GopinathNo ratings yet
- Monitor elderly female with small bowel obstructionDocument2 pagesMonitor elderly female with small bowel obstructionimthebossNo ratings yet
- Spontaneously, Without A Known CauseDocument6 pagesSpontaneously, Without A Known CauseAnalyn SarmientoNo ratings yet
- CCCCO NA Model Curriculum Module 10 PDFDocument46 pagesCCCCO NA Model Curriculum Module 10 PDFjebashanthini0% (1)
- Chapter 30 StudyGuide WorkbookDocument5 pagesChapter 30 StudyGuide WorkbookJacqueline GreerNo ratings yet
- New Born Care 1Document12 pagesNew Born Care 1gilbertgarciaNo ratings yet
- HO in Spinal Cord InjuryDocument3 pagesHO in Spinal Cord InjuryDarren Mae MosadaNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 23Document5 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 23sarasjunkNo ratings yet
- Cns LectureDocument10 pagesCns Lectureferg jeanNo ratings yet
- GI Part 2 2016 StudentDocument131 pagesGI Part 2 2016 StudentDaniel RayNo ratings yet
- 4 ConvulsionDocument40 pages4 ConvulsionMohamed Na3eemNo ratings yet
- MS Final 46 Blood or Lymphatic DisorderDocument4 pagesMS Final 46 Blood or Lymphatic DisorderZachary T Hall0% (1)
- Cardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Document36 pagesCardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Melodia Turqueza GandezaNo ratings yet
- Posttest UrinaryDocument7 pagesPosttest UrinaryAilatiLiamNo ratings yet
- Unit 3 Maternal Health Care Edited 2015Document43 pagesUnit 3 Maternal Health Care Edited 2015Londera BainNo ratings yet
- Chest Tubes: Draining Fluids and Air from the Pleural SpaceDocument21 pagesChest Tubes: Draining Fluids and Air from the Pleural SpaceAnusha VergheseNo ratings yet
- Cardiovascular (CVS) Examination: Procedure StepsDocument15 pagesCardiovascular (CVS) Examination: Procedure StepsGeorich NarcisoNo ratings yet
- Week 4 - The Nursing ProcessDocument10 pagesWeek 4 - The Nursing ProcessMiss VinaNo ratings yet
- Chapter 39: Nursing Assessment: Gastrointestinal System Test BankDocument6 pagesChapter 39: Nursing Assessment: Gastrointestinal System Test BankNurse UtopiaNo ratings yet
- ATI Pain and InflammationDocument3 pagesATI Pain and InflammationAnna100% (1)
- Critical Care Monitoring ProblemsDocument18 pagesCritical Care Monitoring Problemshops23No ratings yet
- Spinal Cord Injury Spinal Cord InjuriesDocument6 pagesSpinal Cord Injury Spinal Cord InjuriesJamaica Leslie NovenoNo ratings yet
- Physical Examination Techniques and ManueversDocument160 pagesPhysical Examination Techniques and ManueversMa-anJaneDiamosNo ratings yet
- A Sense of Humor DrivingDocument160 pagesA Sense of Humor DrivingSidraGhafoorNo ratings yet
- Congenital Heart DiseaseDocument45 pagesCongenital Heart DiseaseBrandedlovers OnlineshopNo ratings yet
- Students' Guide to PneumoniaDocument15 pagesStudents' Guide to PneumoniaArgenic BernzNo ratings yet
- Surg Wound Clas TreeDocument1 pageSurg Wound Clas TreeCita Rahma SwastikaNo ratings yet
- Pediatric Nursing-Cardiovascular DisordersDocument10 pagesPediatric Nursing-Cardiovascular Disordershasan ahmd100% (1)
- Lowdermilk: Maternity & Women's Health Care, 10th EditionDocument12 pagesLowdermilk: Maternity & Women's Health Care, 10th Editionvanassa johnson100% (1)
- Nursing Care Plans for Cardiovascular Case ScenariosDocument14 pagesNursing Care Plans for Cardiovascular Case ScenariosOrlino PeterNo ratings yet
- Chapter 25: Assessment: Respiratory System Harding: Lewis's Medical-Surgical Nursing, 11th EditionDocument9 pagesChapter 25: Assessment: Respiratory System Harding: Lewis's Medical-Surgical Nursing, 11th EditionKrishna RamaNo ratings yet
- Global Nephro Training ReviewerDocument13 pagesGlobal Nephro Training Reviewersean blaze100% (1)
- N3102 Case Study: Musculoskeletal - Instructor Copy: Day 1 - Patient AssignmentDocument17 pagesN3102 Case Study: Musculoskeletal - Instructor Copy: Day 1 - Patient AssignmentBrittany LynnNo ratings yet
- HemiplegiaDocument17 pagesHemiplegiaStefany CelineNo ratings yet
- BluePrint 5th QuestionsDocument25 pagesBluePrint 5th QuestionsAbuFreihNo ratings yet
- MedSurg Nursing Case Study: Care Plans for Liver Disease PtDocument1 pageMedSurg Nursing Case Study: Care Plans for Liver Disease PtShahab SaqibNo ratings yet
- HIV AIDS NCLEX Questions Nursing Review QuizDocument10 pagesHIV AIDS NCLEX Questions Nursing Review QuizShella Mae UsquisaNo ratings yet
- Concept MapDocument6 pagesConcept Mapapi-499028250No ratings yet
- Major Hormone Glands and Their FunctionsDocument5 pagesMajor Hormone Glands and Their FunctionsSTEFFI GABRIELLE GOLEZNo ratings yet
- Concept Map TemplateDocument16 pagesConcept Map Templatenursing concept mapsNo ratings yet
- Module 2: Patient/Resident Rights Minimum Number of Theory Hours: 3 Suggested Theory Hours: 5 Recommended Clinical Hours: 1 Statement of PurposeDocument23 pagesModule 2: Patient/Resident Rights Minimum Number of Theory Hours: 3 Suggested Theory Hours: 5 Recommended Clinical Hours: 1 Statement of PurposefareehaNo ratings yet
- CH 31 - Assessment and Management of Patients With Vascular Disorders and Problems of PeripheralDocument16 pagesCH 31 - Assessment and Management of Patients With Vascular Disorders and Problems of PeripheralPye Antwan DelvaNo ratings yet
- Cardio-Physiology Exam QuestionsDocument17 pagesCardio-Physiology Exam Questionsjimmy100% (1)
- Normal Laboratory Values With Nursing Consideration - UsnganDocument8 pagesNormal Laboratory Values With Nursing Consideration - UsnganPrincess Nasima M. UsnganNo ratings yet
- TXTDocument356 pagesTXTJec AmracNo ratings yet
- Cardiovascular System: Complications of Positive Pressure VentilationDocument5 pagesCardiovascular System: Complications of Positive Pressure VentilationjefrocNo ratings yet
- Cardio AssessmentDocument2 pagesCardio AssessmentMabesNo ratings yet
- Assessment of Respiratory Function Chpt.20Document32 pagesAssessment of Respiratory Function Chpt.20Maricar RosasNo ratings yet
- Genito Urinary TractDocument199 pagesGenito Urinary TractKim GonzalesNo ratings yet
- OB Gyne Assessment ToolDocument5 pagesOB Gyne Assessment ToolKyla CsyNo ratings yet
- Medical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100Document7 pagesMedical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100ianshirow834No ratings yet
- Perry: Maternal Child Nursing Care, 4 Edition: Chapter 16: Management of Discomfort Test Bank Multiple ChoiceDocument12 pagesPerry: Maternal Child Nursing Care, 4 Edition: Chapter 16: Management of Discomfort Test Bank Multiple ChoiceChristopher Endicott100% (3)
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- Lung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesFrom EverandLung Metabolism: Proteolysis and Antioproteolysis Biochemical Pharmacology Handling of Bioactive SubstancesAlain JunodNo ratings yet
- Fistula in Ano Treatment Options and ClassificationDocument49 pagesFistula in Ano Treatment Options and ClassificationsitalcoolkNo ratings yet
- Physiologic Changes in PregnancyDocument4 pagesPhysiologic Changes in PregnancysitalcoolkNo ratings yet
- Uterine SarcomasDocument22 pagesUterine SarcomassitalcoolkNo ratings yet
- Morbidity Causes Top Ten Diseases in Nepal (In Patients) : Sources: Nepal Census 2011, Ministry of Health, NepalDocument2 pagesMorbidity Causes Top Ten Diseases in Nepal (In Patients) : Sources: Nepal Census 2011, Ministry of Health, NepalsitalcoolkNo ratings yet
- Maternal Mortality in NepalDocument18 pagesMaternal Mortality in NepalsitalcoolkNo ratings yet
- Placental HormonesDocument6 pagesPlacental Hormonessitalcoolk100% (1)
- Pediatrics Specific DisordersDocument6 pagesPediatrics Specific DisorderssitalcoolkNo ratings yet
- Normal DistributionDocument16 pagesNormal DistributionsitalcoolkNo ratings yet
- Interpretation of Widal TestDocument2 pagesInterpretation of Widal TestsitalcoolkNo ratings yet
- Difference Between Kwashiorkor and MarasmusDocument3 pagesDifference Between Kwashiorkor and Marasmussitalcoolk100% (1)
- Medpage Guide To Epi and BiostatisticsDocument11 pagesMedpage Guide To Epi and Biostatisticsnet2020100% (1)
- Personality DisordersDocument5 pagesPersonality DisorderssitalcoolkNo ratings yet
- Diagnostic UltrasoundDocument9 pagesDiagnostic UltrasoundsitalcoolkNo ratings yet
- Chi Square T TestDocument17 pagesChi Square T TestsitalcoolkNo ratings yet
- CoughDocument7 pagesCoughsitalcoolkNo ratings yet
- Master Question Bank Bio 722008Document56 pagesMaster Question Bank Bio 722008sitalcoolkNo ratings yet
- Characteristics of Neuromuscular BlockersDocument2 pagesCharacteristics of Neuromuscular BlockerssitalcoolkNo ratings yet
- Tuneup Utilites 2012 KeysDocument1 pageTuneup Utilites 2012 KeyssitalcoolkNo ratings yet
- How Drugs Are Developed and ApprovedDocument2 pagesHow Drugs Are Developed and ApprovedsitalcoolkNo ratings yet
- Vital Signs and JVPDocument3 pagesVital Signs and JVPsitalcoolkNo ratings yet
- Interpretation of Widal TestDocument2 pagesInterpretation of Widal TestsitalcoolkNo ratings yet
- Respiratory Physiology DiseasesDocument1 pageRespiratory Physiology DiseasessitalcoolkNo ratings yet
- Share The WifiDocument1 pageShare The WifisitalcoolkNo ratings yet
- MCQs in BasicDocument87 pagesMCQs in Basictausif0675% (4)
- Ecg PhysioDocument2 pagesEcg PhysiositalcoolkNo ratings yet
- Ecg DeterminationDocument2 pagesEcg DeterminationsitalcoolkNo ratings yet
- PAGAL by Laxmi P DevkotaDocument1 pagePAGAL by Laxmi P DevkotasitalcoolkNo ratings yet
- Respiratory PhysiologyDocument1 pageRespiratory PhysiologysitalcoolkNo ratings yet
- Lymph Node Levels of The Nec1Document2 pagesLymph Node Levels of The Nec1sitalcoolkNo ratings yet
- Adventitious Breath SoundsDocument46 pagesAdventitious Breath SoundsSuyanto nduduNo ratings yet
- Respiratory SoundsDocument2 pagesRespiratory SoundsMuhammad NaeemjakNo ratings yet
- Assessment On Respiratory ProblemsDocument7 pagesAssessment On Respiratory ProblemsSetiaty PandiaNo ratings yet
- 8 Nursing Notes and 8 SBARDocument8 pages8 Nursing Notes and 8 SBARjunie048514% (7)
- Wheezing DisorderDocument497 pagesWheezing DisorderVincent LivandyNo ratings yet
- Testmanship - Medical Surgical Nursing Test Taking Strategy-Based June 2009 Nursing Licensure ExaminationDocument16 pagesTestmanship - Medical Surgical Nursing Test Taking Strategy-Based June 2009 Nursing Licensure ExaminationJennine Reyes100% (1)
- 3 3 1 Medical History Visit 1Document2 pages3 3 1 Medical History Visit 1Amaris HopkinsNo ratings yet
- E000367 FullDocument15 pagesE000367 FullBBD BBDNo ratings yet
- Test Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition WilkinsDocument36 pagesTest Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition Wilkinscreutzerpilement1x24a100% (34)
- Drug Study Amlodipine & HydrocortisoneDocument4 pagesDrug Study Amlodipine & HydrocortisoneJohn Kristoffer JisonNo ratings yet
- Respiratory Exam GuideDocument18 pagesRespiratory Exam GuideIbi Yulia Setyani100% (1)
- Case StudyDocument13 pagesCase StudyLeong Ka YeeNo ratings yet
- Master Dentistry2Document275 pagesMaster Dentistry2Isak Shatika0% (1)
- Assessing and Managing Wheezing in Preschool ChildrenDocument8 pagesAssessing and Managing Wheezing in Preschool ChildrenEndy Widya PutrantoNo ratings yet
- 6 - Breath SoundsDocument31 pages6 - Breath SoundsggNo ratings yet
- Answer Key CicDocument3 pagesAnswer Key Cictiburshoc16No ratings yet
- Adventitious Breath Sounds - HandoutDocument2 pagesAdventitious Breath Sounds - Handoutkaren solibaNo ratings yet
- Lung Sounds 3Document1 pageLung Sounds 3Kyle LatayanNo ratings yet
- Examination of Respiratory SystemDocument78 pagesExamination of Respiratory Systemwidya sri hastutiNo ratings yet
- Docsbookstoreacsapac2022b1 Sample PDFDocument30 pagesDocsbookstoreacsapac2022b1 Sample PDFFaheem Mahmood ButtNo ratings yet
- Respiration AssessmentDocument7 pagesRespiration AssessmentWen RodsaNo ratings yet
- Asthma FinalDocument71 pagesAsthma FinalVariya HemangiNo ratings yet
- Preskas Abritho Zaifar AsmaDocument18 pagesPreskas Abritho Zaifar AsmaAbritho ZaifarNo ratings yet
- Jurnal AsmaDocument11 pagesJurnal AsmaAi Siti Rika FauziahNo ratings yet
- Pediatric Ist SeminarDocument21 pagesPediatric Ist SeminarAsha jiluNo ratings yet
- Test Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition by WilkinsDocument10 pagesTest Bank For Respiratory Disease A Case Study Approach To Patient Care 3rd Edition by Wilkinsa498226706No ratings yet
- Psychosomatic Theory of Bronchia AsthmaDocument11 pagesPsychosomatic Theory of Bronchia AsthmaMaria RiveraNo ratings yet
- Notes On CVS and Respiratory ExaminationDocument2 pagesNotes On CVS and Respiratory Examinationwel2332No ratings yet
- Egypt 2023 First SessionDocument5 pagesEgypt 2023 First SessionessamwahbaNo ratings yet
- MAPEH 7 Health TestDocument2 pagesMAPEH 7 Health TestSHEILA MAE PERTIMOSNo ratings yet