Professional Documents
Culture Documents
OS 213 Pediatric Asthma
Uploaded by
2012Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
OS 213 Pediatric Asthma
Uploaded by
2012Copyright:
Available Formats
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
Lecture Outline Primary physiologic manifestation is
spontaneously variable airway obstruction which
I. Epidmemiology can be modulated by:
II. Definition Increased obstruction caused by many
III. Review of Anatomy stimuli
IV. Pathophysiology Alleviation of obstruction by
bronchodilators and/or anti-inflammatory
V. Risk Factors
agents
VI. Clinical Features/Diagnosis
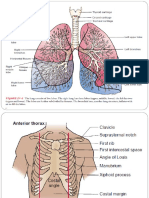
VII. Management REVIEW OF ANATOMY
EPIDEMIOLOGY
Asthma ranked number 1 among the non-
infections admissions in 57 of accredited
hospitals
PPS Registry of Diseases, 1994
Prevalence of wheezing among 6-19 years in
Metro Manila schools was 27.45%
Del Mundo, textbook of Pediatrics 2002
A large international survey study of childhood
asthma prevalence in 56 countries found a wide
range in asthma prevalence, from 1.6 to 36.8%
ISAAC Study
Source: Masoli M et al. Allergy 2004
DEFINITION
a chronic inflammatory disorder of the airways in
which many cells play a role, including mast cells
and eosinophils
this inflammation causes symptoms that are
usually associated with widespread but variable
airflow obstruction that is often reversible either
spontaneously or with treatment, and causes
associated increase in airway PATHOPHYSIOLOGY
hyperresponsiveness to a variety of stimuli.
a disorder defined by its clinical, physiological is complex and involves the following components:
and pathological characteristics
Clinically, asthma is characterized by airway 1) Airway inflammation
hyperresponsiveness presenting as widespread 2) Intermittent airflow obstruction
narrowing of the airway which results from a 3) Bronchial hyperresponsiveness
variety of stimuli like allergens, exercise, physical
factors and irritant gases
Dec 11, 2008 | Thursday Page 1 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
Asthma Inflammation: Cells and Mediators
Key Mediators of Asthma:
Chemokines
Mechanisms Of Airway Narrowing in Asthma
recruitment of inflammatory cells into the
airways and are mainly expressed in
airway epithelial cells Contraction of Airway smooth muscle (ASM) is
the predominant mechanism largely reversed by
Cysteinyl leukotrienes
bronchodilators
potent bronchoconstrictors and
Airway wall thickening
proinflammatory mediators mainly
derived from mast cells and eosinophils Accumulation of airway secretions, mucus casts,
and cellular debris may partially occlude the
only mediator whose inhibition has been
lumen
associated with an improvement in lung
function and asthma symptoms
Regulation of Airway Caliber
Cytokines
Cholinergic (parasympathetic) motoneurons
orchestrate the inflammatory response
innervate the airways via the vagus nerve
in asthma and determine its severity
Nonadrenergic Noncholinergic (NANC) Nervous
Histamine
system
contributes to bronchoconstriction and NANC system neurons in the vagus nerve
to the inflammatory response
release the peptides, SUBSTANCE P and
Nitric Oxide VASOACTIVE INTESTINAL PEPTIDE
a potent vasodilator, produced Appears to be the most potent relaxant
predominantly from the action of component of the nervous system involved in
inducible nitric oxide synthase in airway regulation of airway diameter
epithelial cell
Factors that Influence Asthma Development and
Asthma Inflammation: Cells and Mediators Expression
Host Factors
Genetic
Atopy
Airway hyperresponsiveness
Gender
Obesity
Environmental Factors
Indoor allergens
Outdoor allergens
Occupational sensitizers
Tobacco smoke
Air Pollution
Respiratory Infections
Diet
RISK FACTORS FOR ASTHMA
Host factors: predispose individuals to, or protect
them from, developing asthma
Environmental factors: influence susceptibility to
development of asthma in predisposed
individuals, precipitate asthma exacerbations,
and/or cause symptoms to persist
Who gets asthma? Anyone!!!
Most children develop asthma before age 8 years
and over half before 3 years
Dec 11, 2008 | Thursday Page 2 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
30% < 1 year Masqueraders of asthma in children
80-90% before 4-5 years old
Before puberty: asthma occurs 11/2-3x male > Upper airway noise/congestion
female Cystic fibrosis (CF)
Adolescence male=female Gastroesophageal reflux disease (GERD)
Bronchopulmonary dysplasia (BPD)
Predisposing Factors involved in the Development of Foreign body aspiration
Asthma Immunodeficiency (ID)
Vocal cord dysfunction
Atopy
defined as the preponderance to CLINICAL FEATURES
produce abnormal amounts of IgE in
response to environmental allergens Frequent episodes of wheeze (more than once a
Familial association among asthma, month)
allergic rhinitis and atopic dermatitis Activity induced cough or wheeze
suggests a common genetic basis Nocturnal coughs in periods without viral
-chromosomes 5, 11 infections
90% of asthmatic children have an Absence of seasonal variations in wheeze
allergic component Symptoms that persist after the age of 3
64-84% (+) family history of asthma Wheeze before the age of 3 and one major risk
among 1st degree relatives factor
30% & 3.5% of asthmatic patients parental history of asthma or eczema or
reported asthma in one parent and in two or three risk factors (eosinophilia,
none respectively wheezing without colds, and allergic
Gender rhinitis) has been shown to predict the
Male preponderance presence of asthma in later childhood
Triggers DIAGNOSIS
Risk factors that cause asthma exacerbation by Signs and symptoms to look for include:
inducing inflammation or provoking acute Frequent coughing spells, which may occur
bronchoconstriction or both during play, at night, or while laughing. It is
important to know that cough may be the only
Trigger Factors of Asthma in Various Age Groups symptom present.
Less energy during play
Rapid breathing
Complaint of chest tightness or chest "hurting”
Whistling sound (wheezing) when breathing in
or out
See-saw motions (retractions) in the chest
from labored breathing
Shortness of breath, loss of breath
Tightened neck and chest muscles
Feelings of weakness or tiredness
Anatomic and physiologic peculiarities that predispose to
obstructive airway disease
1. Decreased amount of smooth muscle in
peripheral airways
2. Mucosal gland hyperplasia in the major bronchi
compared to adults favors increased intraluminal
mucus production
3. Disproportionately narrow peripheral airways up
to 5 years of age
4. Decreased static elastic recoil of the young lung
predisposes to early airway closure during tidal
breathing
5. Highly compliant rib cage and mechanically
disadvantageous angle of insertion of diaphragm
to ribcage increases diaphragmatic work of
breathing
6. Decreased number of fatigue-resistant skeletal
muscles in the diaphragm Spirometry
7. Deficient collateral ventilation with the pores of
Kohn and the Lambert canals deficient in number
Recommended in the initial assessment of
and size
patients suspected to have asthma
Dec 11, 2008 | Thursday Page 3 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
Usually feasible in children from age >5 years
Useful in assessing
Degree of airway obstruction
Disturbances in gas exchange
Response of airways to inhaled
allergens/ chemicals/exercise
Assessing response to therapeutic
agents
Evaluating long-term course of disease
FEV1 is the single best measure for assessing
severity of airflow obstruction
FEV1 measurements <80% of predicted value is
evidence of airway obstruction and reversibility
with use of inhaled ß2-agonist (increase in FEV1
by 15%) makes a definitive diagnosis of asthma
Diagnosis of Asthma
Other Tests to help establish the diagnosis of
asthma
1) Methacholine/Histamine bronchoprovocation test
2) Exercise challenge test
3) Twice daily recording of peak flow to determine
diurnal variation
4) Therapeutic trial of five days steroid and
bronchodilator course
Portable Peak Flow Meter
measure PEFR where spirometry is not available
less sensitive, but correlates well with FEV1
offers an acceptable alternative to assess
response to exercise challenge and peak flow
variability
The predicted normal PEFR for Filipino children
between 6 and 17 years of age with height of at
least 100 cm can be calculated:
Males: (Height in cm - 100) 5 + 175
Females: (Height in cm - 100) 5 + 170
MANAGEMENT
“Basically longterm, involving both pharmacological and
non pharmacological interventions”
Philippine Consensus Report 2002
Goals of Therapy
1. to maintain normal activity levels including
exercise;
Dec 11, 2008 | Thursday Page 4 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
2. to maintain ( near ) normal pulmonary function • Should be seen one to three months after the
test; initial visit and every 3 months thereafter
3. to prevent chronic and troublesome symptoms; • After an exacerbation, follow-up should be within
4. to prevent recurrent exacerbations; and, two weeks to one month
5. to avoid adverse effects from asthma
medications ALLERGEN IMMUNOTHERAPY IN ASTHMA
• Administration of increasing quantities of specific
Components of asthma care allergic extracts to patients with IgE-mediated
allergic rhinitis, asthma or stinging insect
1) Develop patient/doctor partnership anaphylaxis
2) Identify and reduce exposure to risk factors
• Should be considered
3) Assess, treat and monitor asthma
o avoiding allergens is not possible
4) Manage asthma exacerbations
o less than complete control of symptoms
Outcome is achieved with bronchodilators or
Successful management of asthma should lead to an inhaled steroids
improvement or normalization of the child’s daily activities, • Greatest benefit of specific immunotherapy using
respiratory symptoms, pulmonary function and personal allergen extracts has been obtained in the
and family psychosocial functioning. treatment of allergic rhinitis
• Role of specific immunotherapy in asthma is
Richel: Haaaaaay. High stress itong trans na to. Half pa lang ng limited
coverage ang nababasa ko :s at kailangan ko pa tong unahin, • Specific immunotherapy should be considered
kaya basahin niyo to! Hello octetmates! Goodluck tom. Haha. only after strict environmental avoidance and
:D pharmacologic intervention, including inhaled
glucocorticosteroids, have failed to control
asthma
• Performed only by trained physician
Objectives
MANAGING EXACERBATIONS OF ASTHMA
IDEAL MINIMAL
Minimal or no chronic symptoms Least symptoms
Exacerbations of asthma
Minimal episodes Least need for PRN β2- agonist
No ER visits Least limitation of activity
• Acute or sub-acute episodes of progressively
Minimal need for PRN β2- agonist worsening symptoms of shortness of breath,
No limitation on activities Best PEFR cough, wheeze and chest tightness or a
PEF circadian variation < 20% Least adverse effects combination of these
( Near) normal PEF Minimal or no adverse effect • Exacerbations may be mild, moderate severe or
even life threatening
Long-term Management of Asthma in Children
ASSESSMENT Key points
• Prevention of exacerbations is the optimal goal
Asthmatic child is classified to an asthma severity
category • Severity of future attacks cannot be predicted,
Category of severity will suggest the initial pharmacologic thus early recognition is imperative
treatment Note: most cases of asthma morbidity and mortality are
Pharmacologic therapy is described as “step care” due to underassessment and undertreatment
control of symptoms should be established as • In the event of an attack, early treatment is
soon as possible advised
short course of oral corticosteroids or higher o Recognition of early signs of attack or
doses of inhaled corticosteroids may be worsening asthma
considered for faster control o Appropriate use of relievers
therapy should be decreased as soon as possible o Prompt communication between patient
to that which is required based on the identified and physician
asthma severity category • Management of asthma attack may include, but
is not limited to:
On follow up:
o Inhaled short-acting β2 agonist for
if control is attained and sustained for at least
immediate relief of airway obstruction
three months, a gradual reduction in treatment
o Systemic corticosteroids
may be possible
o Oxygen
if control is not achieved within 2-6 weeks
o Other agents (e.g. ipratropium bromide,
review patient’s inhaler technique
theophylline)
review compliance and environmental
Note: close monitoring of patient’s condition as well as
control measures (such as: avoidance
response to therapy is crucial
of allergens or other triggers)
diagnosis should be re-evaluated and
Anticholinergics
treatment should be advanced to the
next step • Recent studies have shown that anticholinergics
(e.g. ipratropium bromide) offer some benefit
*see Appendix for long term management when used early and in combination with short-
acting β2 agonists
Monitoring to maintain control • In children with acute asthma, addition of
• Control should be monitored to maintain control anticholinergics to inhaled β2 agonists for 3
and establish lowest step and dose doses given every 20 minutes appears to
Dec 11, 2008 | Thursday Page 5 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
improve lung function modestly and decrease From the Emergency Room
hospital admissions. 1) symptoms are absent or minimal
2) PEFR > 80% predicted
High risk patients 3) sustained response for at least four (4) hours
These are the patients who have the potential to go into
sudden and severe airway obstruction which may From the Hospital
lead to respiratory failure or death. 1) physical examination is normal or near normal
They should be educated to seek medical care early 2) no nocturnal awakenings
during an exacerbation. 3) PEFR > 80% predicted
• infants in moderate/severe exacerbation 4) sustained response to inhaled short-acting
• current use or recent withdrawal (< 1 week) from β2 agonist (at least 4 hours)
systemic corticosteroids
• hospitalization for moderate or severe asthma in Discharge Instructions
the past year Identify and avoid the trigger(s) that precipitated
• prior intubation or history of impending the attack
respiratory failure from asthma Prescribe sufficient medications to continue
• psychiatric disease or psychosocial problems treatment after discharge
• difficulty perceiving airflow obstruction or its Review inhaler technique
severity, and If peak flow meter is available, provide an action
• non-compliance with asthma medication plan plan
Emphasize regular, continuous follow-up with the
IMMEDIATE CASE OF ASTHMA EXACERBATIONS physician
• Treatment should be started as soon as an
Drug Therapy
asthma attack is recognized.
• Initial treatment will include inhaled short-acting 2 TYPES
β2 and if necessary, oxygen. RESCUE/RELIEVER
o PE should be done to determine -for acute relief of symptoms
severity of exacerbation to serve as PROPHYLACTIC/CONTROLLER
a guide to the type of management -to prevent exacerbations
appropriate for the case.
o Brief but focused history pertinent RELIEVER
to the attack
-bronchodilators which relax airway muscles that
Pertinent points to ask tighten in and around the airways
• Severity of symptoms
• History of prior attacks -provide quick relief of symptoms but does not
treat underlying airway inflammation
• Visits to the emergency room
• Hospitalization (including history of intubation) Reliever Medications:
due to asthma Rapid-acting inhaled beta2-agonist
• Current medications Systemic glucocorticosteroids
• Any of other complicating illnesses (e.g. other Anticholinergics
pulmonary or cardiac problems) Theophylline
Short-acting oral beta2-agonist
Particular attention should be given to patients who
present with the following features, as they are the ones
CONTROLLER
most prone to develop acute respiratory failure:
• Cyanosis -Consists of anti-inflammatory agents which
• absence of wheeze prevent asthma attacks by reversing the underlying
• bradycardia and bradypnea inflammatory changes
• paradoxical thoraco-abdominal movement
• drowsiness or confusion -Prevents further inflammation of airways and
• a normal or elevated pCO2 in a patient with controls chronic symptoms
severe distress
Controller Medications:
Appendix. Severity of Asthma Exacerbations Inhaled glucocorticosteroids
Leukotriene modifiers
Admission to Intensive Care Unit Long-acting inhaled β2-agonists
Systemic glucocorticosteroids
Recommended in the following situations: Theophylline
Cromones
1) progressive worsening of asthma symptoms despite
initial Management Long-acting oral β2-agonists
2) presence of sensorial changes (drowsiness, confusion) Anti-IgE
or loss of consciousness Systemic glucocorticosteroids
3) signs of respiratory fatigue (e.g. declining respiratory
rate)
4) impending respiratory arrest (paO2 < 60 mmHg on
supplemental oxygen, pCO2 > 45 mmHg)
Patient Discharge
Dec 11, 2008 | Thursday Page 6 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
On your way to ER, continue your quick relief inhaled
bronchodilator every 20 minutes and take 1 dose of oral
steroids _________
RED ZONE: EMERGENCY!!!
- Presence of any:(Trouble walking or talking due to
shortness of breath, lips and fingernails are blue)
-Quick relief medicines have not helped
-Cannot do usual activities
-Symptoms are getting worse
-Peak flow meter: _____ (< 60 % of your personal
best)
ACTION:
- Proceed to ER
- Take immediately 1 dose of your quick relief inhaled
bronchodilator and continue your inhaled bronchodilator
every 20 minutes while in transit
Key Points to Inhalational Devices - Take 1 dose oral steroids __________
1) There is little difference in the therapeutic effect
between a correctly used MDI with or without a *may mga blanks talaga yan ha ;)
spacer, DPI, and a nebulizer
2) MDI spacer can increase ling deposition References
3) MDI spacer can decrease oropharyngeal Philippine Consensus For The Management Of
deposition Childhood Asthma Revised 2002
4) MDI with a spacer, DPI, or nebulizers can be Global Initiative For Asthma Revised 2006
used for patients who have difficulty coordinating Nelson Textbook of Pediatircs
with MDI activation, those with optimal breathing Lippincott’s Pathophysiology Series Pulonary
pattern, in children, and patients with severe Pathophysiology 1995 By Michael Grippi
illness Textbook Of Pediatric and Health Care 4th Edition By Del
Mundo
Non-pharmacologic interventions include Kendig’s Disorders of the Respiratory Tract in Children
Environmental control 7th Edition
Monitoring of the status of the disease
Asthma education
Action Plan
The asthma action plan is a written asthma management
plan that is jointly prepared by the doctor and the patient.
This written instruction to the patient should be updated Richel: Greetings ulit Hello Phinoms! Sarap ng potatoes no?
Hehe. Saka na ulit yung next supply. Family day ulit? :p
every visit as changes in peak flow measurements or
Tinatamad na ako bumati, hello na lang to everyone! Malunggays,
asthma severity category may occur. sana matapos na natin itong research. Pahiraaaaaaaap. :D
Happy birthday Lani, Fides, and Dr.Gana! :D Hello Raphael.
GREEN ZONE: Doing Well Thank you
- No symptoms day and night (cough, wheeze,
chest tightness and shortness of breath)
- Can do usual activities
- Peak flow meter __________
(>80 % of your personal best or predicted)
ACTION:
- Continue with your current
medication as prescribed _________
YELLOW ZONE: Acute Attack
- Presence of at least 1 of the following: (cough,
wheeze, chest tightness or shortness of breath)
- Waking at night due to asthma
- Can do some but not all usual activities
- Peak flow meter: _____ to _____
(60 to 79% of your personal best)
ACTION:
-Take your quick-relief inhaled
brochodilator_______________
every 20 minutes up to 3 doses until relieved
- Proceed to ER for further evaluation & possible
admission if:
1. getting worse at anytime
2. if no relief after 3 doses of inhaled β2 agonist
Dec 11, 2008 | Thursday Page 7 of 8
SexyBacks
OS 213: Pulmunology Maria Liza B. Zabala, M.D.
Pediatric Asthma Exam 1
Dec 11, 2008 | Thursday Page 8 of 8
SexyBacks
You might also like
- Pediatric Asthma PDFDocument12 pagesPediatric Asthma PDFzie_luph_taz13No ratings yet
- Meconium Aspiration Syndrome: Walter Otieno Consultant PaediatricianDocument27 pagesMeconium Aspiration Syndrome: Walter Otieno Consultant PaediatricianMalueth AnguiNo ratings yet
- Practice Essentials: Signs and SymptomsDocument49 pagesPractice Essentials: Signs and SymptomsRhahima SyafrilNo ratings yet
- Childhood AsthmaDocument40 pagesChildhood AsthmachinchuNo ratings yet
- Appproach To A Case of Status Epilepticus in PaediatricsDocument45 pagesAppproach To A Case of Status Epilepticus in PaediatricsChin NamNo ratings yet
- Asthma in Children My PresentationDocument49 pagesAsthma in Children My PresentationPutra Skate100% (2)
- Respiratory Distress SyndromeDocument10 pagesRespiratory Distress SyndromeKomang Rendy KrisnadiNo ratings yet
- Respiratory Distress SyndromeDocument3 pagesRespiratory Distress SyndromeAshNo ratings yet
- Respiratory Distress Syndrome 1Document35 pagesRespiratory Distress Syndrome 1Marrah Avila AcuinNo ratings yet
- Sacrococcygeal TeratomaDocument21 pagesSacrococcygeal TeratomaEm VelascoNo ratings yet
- Pediatric AsthmaDocument63 pagesPediatric Asthmasrober0565No ratings yet
- Growth and Development With Pediatric ConditionDocument28 pagesGrowth and Development With Pediatric ConditionMaynard King BairdNo ratings yet
- ASTHMADocument51 pagesASTHMAMOSES M CHILALANo ratings yet
- Pediatric Vital Signs MeasurementsDocument3 pagesPediatric Vital Signs MeasurementsJheDelaPazValenzuelaNo ratings yet
- Tetralogy of FallotDocument22 pagesTetralogy of FallotHusna Aje100% (1)
- Physical ExaminationgiDocument61 pagesPhysical ExaminationgiHei LeeNo ratings yet
- Pediatrics Respiratory SystemDocument42 pagesPediatrics Respiratory Systemmuarif100% (1)
- Croup SyndromeDocument3 pagesCroup SyndromeMabesNo ratings yet
- Bronchial AsthmaDocument71 pagesBronchial AsthmaHero MondaresNo ratings yet
- Cystic FibrosisDocument25 pagesCystic FibrosisAhmad Nazir AfiqNo ratings yet
- Pathophysiology of AsthmaDocument71 pagesPathophysiology of AsthmaChin ChanNo ratings yet
- Lower Respiratory Tract Diseases - KeyDocument45 pagesLower Respiratory Tract Diseases - KeyYugmaPandyaNo ratings yet
- Bronchial AsthmaDocument29 pagesBronchial AsthmaDrShaheen100% (5)
- Congenital Heart DefectsDocument13 pagesCongenital Heart DefectsGheluzee Herrera100% (2)
- AL KHAFJI NATIONAL HOSPITAL CLINICAL PRACTICE GUIDELINES FOR NEONATAL JAUNDICEDocument35 pagesAL KHAFJI NATIONAL HOSPITAL CLINICAL PRACTICE GUIDELINES FOR NEONATAL JAUNDICEprinsepejesseNo ratings yet
- Asthma MimickersDocument6 pagesAsthma MimickersHarpreet SinghNo ratings yet
- Thalassemia: Dr. Deep Shah Under Guidance of Dr. Krutika Ma'Am and Dr. Rahul SirDocument46 pagesThalassemia: Dr. Deep Shah Under Guidance of Dr. Krutika Ma'Am and Dr. Rahul SirDeep ShahNo ratings yet
- Acute Respiratory Distress Syndrome (Ards)Document12 pagesAcute Respiratory Distress Syndrome (Ards)Vin Grace Tiqui - GuzmanNo ratings yet
- Neonatal Respiratory DistressDocument54 pagesNeonatal Respiratory DistressMohamad Saleh100% (1)
- CASE 2 PneumoniaDocument12 pagesCASE 2 PneumoniaKenneth MiguelNo ratings yet
- Stanley T. Agor, MD, DPPS, MSPH Department of Pediatrics Cagayan Valley Medical CenterDocument35 pagesStanley T. Agor, MD, DPPS, MSPH Department of Pediatrics Cagayan Valley Medical CenterLuis PadillaNo ratings yet
- Acute Rheumatic FeverDocument50 pagesAcute Rheumatic Feversunaryo lNo ratings yet
- RicketsDocument5 pagesRicketsNader SmadiNo ratings yet
- Preventive Pediatrics Part 3Document5 pagesPreventive Pediatrics Part 3mkct111No ratings yet
- Acute Rheumatic Fever Causes, Symptoms and TreatmentDocument49 pagesAcute Rheumatic Fever Causes, Symptoms and Treatmentbereket gashuNo ratings yet
- Tetanus RabiesDocument67 pagesTetanus RabiesWaNda GrNo ratings yet
- Pediatric Respiratory DiseaseDocument90 pagesPediatric Respiratory DiseasePrashant MishraNo ratings yet
- Preeclampsia Diagnosis and ManagementDocument3 pagesPreeclampsia Diagnosis and ManagementLanaNo ratings yet
- PG Curriculum MD Pediatrics IndexDocument17 pagesPG Curriculum MD Pediatrics IndexCh RajeshNo ratings yet
- Pedia History TakingDocument6 pagesPedia History TakingShaula de OcampoNo ratings yet
- How Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Document14 pagesHow Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Sudhir TyagiNo ratings yet
- Case Study - Pediatric HirshsprungDocument7 pagesCase Study - Pediatric Hirshsprungtruevine_ministryNo ratings yet
- Nursing Care of Respiratory Disorders in ChildrenDocument7 pagesNursing Care of Respiratory Disorders in ChildrenMaikaylaNo ratings yet
- Birth Asphyxia: Prof RL Mbise PCH, ImtuDocument38 pagesBirth Asphyxia: Prof RL Mbise PCH, ImtuCharles FrankNo ratings yet
- Obstetrics Case Proforma TemplateDocument4 pagesObstetrics Case Proforma TemplateSwapneelShah100% (1)
- Neonatal Respiratory DistressDocument59 pagesNeonatal Respiratory DistressMohamad Saleh100% (7)
- Neonatal: HypoglycemiaDocument10 pagesNeonatal: Hypoglycemiamarkus_danusantosoNo ratings yet
- Congenital Heart DefectsDocument45 pagesCongenital Heart Defectskathylaine100% (1)
- Module 4: General Gynecology Topic 1: Family Planning: Preceptor HandoutDocument9 pagesModule 4: General Gynecology Topic 1: Family Planning: Preceptor HandoutMarhama Magarang100% (1)
- Rheumatic FeverDocument15 pagesRheumatic FeverJeaneta Cheryl PatrickNo ratings yet
- Types of PneumothoraxDocument13 pagesTypes of PneumothoraxumarNo ratings yet
- Hiv in Pregnancy FinalDocument73 pagesHiv in Pregnancy Finalapi-3797079No ratings yet
- Pediatric History FormatDocument3 pagesPediatric History Formatthebidaman1No ratings yet
- Children Born Small For Gestational Age Differential Diagnosis, Molecular Genetic Evaluation, and ImplicationsDocument44 pagesChildren Born Small For Gestational Age Differential Diagnosis, Molecular Genetic Evaluation, and ImplicationsErika AvilaNo ratings yet
- Pathophysiology of RHDDocument4 pagesPathophysiology of RHDshmily_0810No ratings yet
- Non Hodgkin's LymphomaDocument8 pagesNon Hodgkin's LymphomaCh RajeshNo ratings yet
- Intestinal ObstructionDocument58 pagesIntestinal ObstructionTUSHAR PARMARNo ratings yet
- Prepared by Mary Ann A. Cubon, RN, RM, ManDocument35 pagesPrepared by Mary Ann A. Cubon, RN, RM, ManCarlaLuisaVillalunaNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- General Recommendation ImmunizationDocument69 pagesGeneral Recommendation Immunization2012No ratings yet
- Fa Step 1 ScheduleDocument5 pagesFa Step 1 ScheduleDinesh DalviNo ratings yet
- SCOPING DOCUMENT For WHO Treatment Guidelines On Pain Related ToDocument10 pagesSCOPING DOCUMENT For WHO Treatment Guidelines On Pain Related To2012No ratings yet
- Diseases of The Anus Rev#1CDocument77 pagesDiseases of The Anus Rev#1C2012No ratings yet
- CEBM Levels of EvidenceDocument2 pagesCEBM Levels of Evidence2012100% (2)
- PCAP UpdatesDocument60 pagesPCAP Updates2012No ratings yet
- ADA Summary of Guidelines 2011Document7 pagesADA Summary of Guidelines 2011IffatNaeemNo ratings yet
- USMLEboardswhatworked 2008Document32 pagesUSMLEboardswhatworked 20082012No ratings yet
- Clin Tox Oral Vs IV ActylcysteineDocument19 pagesClin Tox Oral Vs IV Actylcysteine2012No ratings yet
- CSAP Full 2002Document125 pagesCSAP Full 20022012No ratings yet
- Review Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases PharmacologyDocument110 pagesReview Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases Pharmacologyupmed2012block9No ratings yet
- Review of The Evidence For Herbal Medications and NutraceuticalsDocument5 pagesReview of The Evidence For Herbal Medications and Nutraceuticals2012No ratings yet
- The Division of Plastic SurgeryDocument36 pagesThe Division of Plastic Surgery2012No ratings yet
- American Diabetes Association (ADA) gUIDELINESDocument43 pagesAmerican Diabetes Association (ADA) gUIDELINESSamuel Rudolf Maranatha JulioNo ratings yet
- Pharma EvaluationDocument1 pagePharma Evaluation2012No ratings yet
- Cancer Pain Relief Who 1998Document86 pagesCancer Pain Relief Who 19982012100% (1)
- Test Blueprint For Final Exam 2008-2009 For 75 PtsDocument3 pagesTest Blueprint For Final Exam 2008-2009 For 75 Pts2012No ratings yet
- Patho Lab Trans - ButchDocument6 pagesPatho Lab Trans - Butch2012No ratings yet
- Organ Transplantation, Immunology and RejectionDocument2 pagesOrgan Transplantation, Immunology and Rejection2012No ratings yet
- Trans Pulmopatho ColoredDocument8 pagesTrans Pulmopatho Colored2012No ratings yet
- Renal Patho Lab 2 PART 1 ColoredDocument8 pagesRenal Patho Lab 2 PART 1 Colored2012No ratings yet
- Art of Med Trans Feb 28Document9 pagesArt of Med Trans Feb 282012No ratings yet
- 434 OS 212 PictoTrans - Cutaneous SymptomatologyDocument51 pages434 OS 212 PictoTrans - Cutaneous Symptomatology2012No ratings yet
- Trans Glomerularpatho FinalDocument16 pagesTrans Glomerularpatho Final2012100% (1)
- Glomerulonephritis Block A TransDocument7 pagesGlomerulonephritis Block A Trans2012No ratings yet
- OS 214 - Renal Module - Imaging of The KUBDocument9 pagesOS 214 - Renal Module - Imaging of The KUB2012No ratings yet
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- GOLD For COPD Pocket GuideDocument30 pagesGOLD For COPD Pocket Guideraul sinatoNo ratings yet
- Respiratory Distress Syndrome 1Document35 pagesRespiratory Distress Syndrome 1Marrah Avila AcuinNo ratings yet
- A 2-Year-Old Child With Cough and Respiratory Distress: Family Medicine and Community HealthDocument2 pagesA 2-Year-Old Child With Cough and Respiratory Distress: Family Medicine and Community HealthElse FashiosNo ratings yet
- Respiratory exam guideDocument10 pagesRespiratory exam guideMarjorie Joy GreciaNo ratings yet
- Effectiveness of oxygen therapy positionsDocument13 pagesEffectiveness of oxygen therapy positionssyafiraainiNo ratings yet
- Contusion Pulmonum: Clinical Features and ManagementDocument10 pagesContusion Pulmonum: Clinical Features and ManagementSyamsuriWahyuNo ratings yet
- Ot - Role of Ot in Pulmonary RehabDocument32 pagesOt - Role of Ot in Pulmonary RehabAlyssa Bituin100% (1)
- Respiratory Exam GuideDocument18 pagesRespiratory Exam GuideIbi Yulia Setyani100% (1)
- The Respiratory System PDFDocument21 pagesThe Respiratory System PDFhechi_zeroNo ratings yet
- NURSING ASSESSMENT OF PATIENT WITH RESPIRATORY DISTRESSDocument4 pagesNURSING ASSESSMENT OF PATIENT WITH RESPIRATORY DISTRESSAlyssa Marie SantosNo ratings yet
- Dutch COPD Physiotherapy Guidelines PDFDocument64 pagesDutch COPD Physiotherapy Guidelines PDFyohanNo ratings yet
- SPIROMETRY GUIDE FOR COPD DIAGNOSISDocument2 pagesSPIROMETRY GUIDE FOR COPD DIAGNOSISGiliana P. García AcevedoNo ratings yet
- Topic Respiratory Distress in NewbornDocument45 pagesTopic Respiratory Distress in NewbornICETNPNo ratings yet
- Symtoms and Signs of The Respiratory SystemDocument33 pagesSymtoms and Signs of The Respiratory SystemmohammedNo ratings yet
- E PneumothoraxDocument12 pagesE PneumothoraxErna MiraniNo ratings yet
- RMO Orientation AIRMEDDocument130 pagesRMO Orientation AIRMEDqueenartemisNo ratings yet
- Pneumothorax: DR G.B.L Samarasekera Consultant Respiratory Physician DGH - GampahaDocument50 pagesPneumothorax: DR G.B.L Samarasekera Consultant Respiratory Physician DGH - GampahappgpcsNo ratings yet
- Modes of Ventilation - NRRCC 2007 PDFDocument59 pagesModes of Ventilation - NRRCC 2007 PDFprofarmah6150No ratings yet
- Client with Difficulty BreathingDocument6 pagesClient with Difficulty BreathingJoji BaitNo ratings yet
- PulmoVista 500 - APPLICATION - Identify Onset of Derecruitment - 032018Document2 pagesPulmoVista 500 - APPLICATION - Identify Onset of Derecruitment - 032018tomNo ratings yet
- Chapter 66 1Document20 pagesChapter 66 1isapatrick8126No ratings yet
- Respiratory System 2Document2 pagesRespiratory System 2Christopher EstevezNo ratings yet
- Fibroza ChisticaDocument65 pagesFibroza ChisticaPatric GutuNo ratings yet
- Asthma: DR Yusuf Adi Gunawan SPPDDocument19 pagesAsthma: DR Yusuf Adi Gunawan SPPDIan GalihNo ratings yet
- RXDXDocument2 pagesRXDXNandaNo ratings yet
- Nursing Management of Respiratory DisordersDocument151 pagesNursing Management of Respiratory DisordersAbirajan100% (2)
- Croup: Dr. Shveta Sethi Narula A.P. MicrobiologyDocument14 pagesCroup: Dr. Shveta Sethi Narula A.P. Microbiology12. Akshit AtwalNo ratings yet
- Types of Nebulizers - Ultrasonic, Vibrating Mesh, & Jet Nebulizers - NebologyDocument7 pagesTypes of Nebulizers - Ultrasonic, Vibrating Mesh, & Jet Nebulizers - NebologyUriel ChavarriaNo ratings yet
- Effectiveness ACBT and PLBT breathing techniques increase COPD oxygen levelsDocument4 pagesEffectiveness ACBT and PLBT breathing techniques increase COPD oxygen levelsI Putu Yoga PrasetyaNo ratings yet
- Anesthesia Workstation Ventilation ModesDocument6 pagesAnesthesia Workstation Ventilation Modesmas agung chandraNo ratings yet