Professional Documents
Culture Documents
Anaerobic Infections: Bacteroides Prevotella Porphyromonas Fusobacterium Bilophila and Sutterella SPP
Uploaded by
dilawarj_2Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anaerobic Infections: Bacteroides Prevotella Porphyromonas Fusobacterium Bilophila and Sutterella SPP
Uploaded by
dilawarj_2Copyright:
Available Formats
ANAEROBIC INFECTIONS
LEARNING OBJECTIVES: At the end of the lecture, students should be able to: Describe about the anaerobic bacteria. Describe the classification of anaerobes. Describe the pathogenesis of anaerobic infections. ANAEROBIC INFECTIONS: Anaerobic infections are caused by anaerobic bacteria. ANAEROBIC BACTERIA: Anaerobic bacteria do not grow on solid media in room air (10% carbon dioxide and 18% oxygen). OBLIGATE ANAEROBE Lack superoxide dismutase and/or catalase toxic radicals formed by oxidative enzymes kill organisms AERO-TOLERANT ANAEROBES survive in presence of oxygen Do not use oxygen for energy requirements FACULTATIVE ANAEROBES can grow in the presence as well as in the absence of air. ANAEROBIC BACTERIA: Gram-negative rods: Bacteroides Prevotella Porphyromonas Fusobacterium Bilophila and Sutterella spp. Gram-positive cocci (primarily Peptostreptococcus spp.) Gram-positive spore-forming (Clostridium spp.) and nonspore-forming bacilli (Actinomyces, Propionibacterium, Eubacterium, Lactobacillus and Bidobacterium spp.) Gram-negative cocci (mainly Veillonella spp.)
ANAEROBES OF CLINICAL IMPORTANCE: CLOSTRIDIA C tetani; C perfringens; C difficile; C botulinum BACTEROIDES B fragilis; Prevotella Porphyromonas ACTINOMYCES FUSOBACTERIUM ANAEROBIC STREPTOCOCCI: Pathogenesis of anaerobic infections: Contamination of site with spores Factors which promote anaerobiasis crush injuries with interruption of blood supply, contaminaton with foreign bodies (dirt), tissue damage Germination of spores Toxin release Binding of toxin to receptor Resulting effect produces symptom(s) of disease.
Clostridium perfringens:
Large rectangular Gram positive bacillus Spores seldom seen in vivo or in vitro non motile Produces several toxins alpha (lecithinase), beta, epsilon ...... enterotoxin Causes a spectrum of human diseases -- Gas gangrene Bacteraemia Myonecrosis food poisoning enteritis necrotica (pig bel)
Gas gangrene:
As capillary permeability increases, the accumulation of fluid increases, and venous return eventually is curtailed.
As more tissue becomes involved, the clostridia multiply within the increasing area of dead tissue, releasing more toxins into the local tissue and the systemic circulation.
Diagnosis Myonecrosis clinical Gram stain of exudate - typical organisms no pus cells Culture -growth of C perfringens (and/or other clostridia associated with this clinical condition) Food poisoning abdominal pain, diarrhoea and vomiting 8-18 hours after a suspect meal. Self limiting Enteritis necroticans severe abdominal pain, bloody diarrhoea , shock and peritonitis (C perfringens type C)
Treatment and prevention: Myonecrosis Proper wound debridement and ensure adequate blood supply Penicillin antitoxin and hyperbaric oxygen - no proven value Food poisoning Proper preparation and storage of food self limiting disease -antibiotics not indicated Enteritis necroticans Proper cooking of food immunization of susceptible population
Clostridium tetani:
Small motile spore forming gram positive bacillus with round terminal spores Causes tetanus Pathogenesis: produces tetanospasmin during stationary phase which is released when cell lysis occurs heavy chain binds to ganglioside on neuronal membranes toxin internalized and moves from peripheral to central nervous system by retrograde axonal transport crosses synapse and localized within vesicles acts by blocking release of inhibitory neurotransmittors (eg GABA) TETANUS Clinical syndromes due to unregulated excitatory synaptic activity resulting in spastic paralysis Generalised tetanus Neonatal tetanus localized tetanus
Prevention and treatment: Active immunization with tetanus toxoid Wound toilet and active/passive immunization of risk injuries management of wound tetanus toxoid Anti-tetanus serum (ARS -horse serum) or Human Tetanus ImmunoGlobulin (HTIG) Penicillin or Metronidazole Management of patient with tetanus reduce stimuli respiratory and CVS support
Clostridium difficile:
Associated with human disease in mid-1970s Found in human GIT in small numbers With antibiotic use, increase in number in GIT Clindamycin, ampicillin, cephalosporins. Produces 2 entero toxins Toxin A -enterotoxin & Toxin B cytotoxin Diagnosis: Detection of toxins in stools, culture of organism Clinical Pseudomembranous colitis Treatment omit antibiotic if possible oral vancomycin or metronidazole Pseudomembranous colitis
Clostridium botulinum:
Fastidious spore forming anaerobic gram positive bacillus Produces 8 antigenically distinct toxins Human disease described with types A, B & E Heavy chain binds to ganglioside receptor Toxin internalized and prevents release of acetyl choline from vesicles Clinical Food borne botulism (weakness, dizziness, ocular palsy and progressive flaccid paralysis) infant botulism (floppy baby) wound botulism ANAEROBIC GRAM NEGATIVE BACILLI Bacteroides, Prevotolla, Porphyromonas and Fusobacterium Present in GI tract -form large component of normal flora >80% of human infections associated with B fragilis virulence factors - capsule, LPS, agglutinins and enzymes Clinical - Endogenous infections Intra-abdominal pyogenic infections pleuro-pulmonary infctions genital infection ACTINOMYCES: Strict anaerobic Gram positive bacilli typically arranged in hyphae which fragment into short bacilli Normal flora of upper respiratory tract, GI tract and female genital tract. Low virulence produce disease when mucosal barrier is breached (eg: following dental trauma or surgery) ENDOGENOUS Establishes chronic infection that spreads through normal anatomical barriers.
Clinical -cervicofacial, abdominal and thoracic. Diagnosis:
Gram stain of sulpher granules Culture - surgery and long term penicillin.
Treatment
------------------------xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx-------------------------------
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 1Document60 pages1aman100% (3)
- Minutes Infection Control Committee Mar 08Document5 pagesMinutes Infection Control Committee Mar 08Czarina Guinto100% (1)
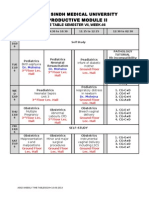
- Semester 07, Week-08 TTDocument1 pageSemester 07, Week-08 TTdilawarj_2No ratings yet
- Flyer-Updates On Dengue FeverDocument1 pageFlyer-Updates On Dengue Feverdilawarj_2No ratings yet
- Dengue Hemorrhagic FeverDocument3 pagesDengue Hemorrhagic Feverdilawarj_2No ratings yet
- Chicken Pox and ShinglesDocument6 pagesChicken Pox and Shinglesdilawarj_2No ratings yet
- Dengue Hemorrhagic FeverDocument3 pagesDengue Hemorrhagic Feverdilawarj_2No ratings yet
- Chicken Pox and ShinglesDocument6 pagesChicken Pox and Shinglesdilawarj_2No ratings yet
- Approach To Patient With RashDocument6 pagesApproach To Patient With Rashdilawarj_2No ratings yet
- Anaerobic InfectionsDocument57 pagesAnaerobic Infectionsentistde0% (1)
- Cleocin HCL Clindamycin Hydrochloride Capsules, USP: Reference ID: 4092165Document14 pagesCleocin HCL Clindamycin Hydrochloride Capsules, USP: Reference ID: 4092165krizelNo ratings yet
- Clostridium Difficile Infection Fidaxomicin Esnm1Document11 pagesClostridium Difficile Infection Fidaxomicin Esnm1Pet UrNo ratings yet
- Clindamycin Gel Is Used ForDocument4 pagesClindamycin Gel Is Used Forgustavo83_prNo ratings yet
- Types of Infectious DiseasesDocument11 pagesTypes of Infectious DiseasesmaricelNo ratings yet
- 2019 MUSE Conference - Educational Presentations - Rev March 19 2019Document52 pages2019 MUSE Conference - Educational Presentations - Rev March 19 2019Michele LambertNo ratings yet
- Mikroba Saluran PencernaanDocument70 pagesMikroba Saluran PencernaanAde Yurga TonaraNo ratings yet
- CeftazidimeDocument16 pagesCeftazidimeNakorn BaisriNo ratings yet
- Magnamycin InjectionDocument8 pagesMagnamycin InjectionHitesh VermaNo ratings yet
- Stewardship Booklet Practical Guide To Antimicrobial Stewardship in HospitalsDocument23 pagesStewardship Booklet Practical Guide To Antimicrobial Stewardship in HospitalsZunisa Rizki100% (4)
- Rationale For Journal SelectionDocument13 pagesRationale For Journal SelectionSusan MolendykNo ratings yet
- HAI Knowledge QuestionnaireDocument3 pagesHAI Knowledge Questionnaireمالك مناصرةNo ratings yet
- Ceftin Prescribing InformationDocument21 pagesCeftin Prescribing InformationbiochemiNo ratings yet
- A 65-Year-Old Man Came To The Emergency Department Via Ambulance - Relatives Accompanied The Patient and Described A 1-Day History of FeverDocument43 pagesA 65-Year-Old Man Came To The Emergency Department Via Ambulance - Relatives Accompanied The Patient and Described A 1-Day History of FeverandriopaNo ratings yet
- Lasting Impact of Clostridium Difficile Infection in in Ammatory Bowel Disease: A Propensity Score Matched AnalysisDocument9 pagesLasting Impact of Clostridium Difficile Infection in in Ammatory Bowel Disease: A Propensity Score Matched AnalysisOana Cristina PetreaNo ratings yet
- Composition: Amoxicillin and Clavulanate Potassium Tablets USPDocument5 pagesComposition: Amoxicillin and Clavulanate Potassium Tablets USPManjeet SinghNo ratings yet
- Clostridium DifficileDocument9 pagesClostridium DifficileRita della ValentiniNo ratings yet
- Cefazolin InjectionDocument15 pagesCefazolin InjectionYaleswari Hayu PertiwiNo ratings yet
- GIDocument196 pagesGIswagmasterNo ratings yet
- DeclomycineDocument14 pagesDeclomycineRamanasarmaNo ratings yet
- Bowel Preparation Colon ResectionDocument28 pagesBowel Preparation Colon ResectioncristiangallardovNo ratings yet
- CefepimeDocument24 pagesCefepimedinniNo ratings yet
- Environmental Hygiene - The Importance of Process, Product and Practice PDFDocument18 pagesEnvironmental Hygiene - The Importance of Process, Product and Practice PDFAnsh KunalNo ratings yet
- C DiffDocument2 pagesC Difftheseus5No ratings yet
- Blaylock Wellness Report: Stomach HealthDocument16 pagesBlaylock Wellness Report: Stomach HealthNabila Rizkika100% (2)
- Diarrhea & ConstipationDocument100 pagesDiarrhea & ConstipationPanee KowNo ratings yet
- S 016 LBLDocument23 pagesS 016 LBLMuhammadAmdadulHoqueNo ratings yet
- Clostridium Difficile in The ICU (2011)Document11 pagesClostridium Difficile in The ICU (2011)drheayNo ratings yet