Professional Documents
Culture Documents
Multiple Measures of Magnesium Status Are Comparable in Mild Asthma and Control Subjects
Uploaded by
Sukma EffendyOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Multiple Measures of Magnesium Status Are Comparable in Mild Asthma and Control Subjects
Uploaded by
Sukma EffendyCopyright:
Available Formats
Journal of Asthma, 43:783788, 2006 Copyright C 2006 Informa Healthcare ISSN: 0277-0903 print / 1532-4303 online DOI: 10.
1080/02770900601031870
ORIGINAL ARTICLE
Multiple Measures of Magnesium Status Are Comparable in Mild Asthma and Control Subjects
ALEXANDRA G. KAZAKS, PH.D.,1, JANET Y. URIU-ADAMS, PH.D.,1 TIMOTHY E. ALBERTSON, M.D., M.P.H., PH.D.,2 AND JUDITH S. STERN, SC.D.3
1 Department of Nutrition, University of California, Davis, California, USA Department of Internal Medicine, Division of Pulmonary and Critical Care Medicine, University of California, Davis School of Medicine, Davis, California, USA 3 Department of Nutrition, Department of Internal Medicine, Division of Endocrinology, Clinical Nutrition and Vascular Biology, University of California, Davis, California, USA 2
Magnesium (Mg) may be a signicant factor in asthma management. There is debate about how to best assess Mg status. We evaluated multiple indices of Mg status and lung function in 52 people with mild to moderate asthma and 47 controls. Mg measures included serum total, ionized and erythrocyte Mg, intravenous Mg load retention and dietary recall. Methacholine challenge and pulmonary function tests were used to assess diagnosis and severity of asthma. Mg status was similar in asthma and controls, and was not correlated to lung function. Total serum Mg closely reected ionized Mg and offers a useful clinical diagnostic monitor. Keywords asthma, magnesium status, serum magnesium
BACKGROUND Asthma is a signicant public health burden that affects about 19.8 million people in the United States and 300 million people worldwide (1, 2). Asthma symptoms are instigated by numerous and diverse endogenous and environmental triggers. Episodes can vary from mild chest tightness, shortness of breath, coughing or wheezing, to life-threatening respiratory failure. Epidemiologic studies suggest that environmental factors, including diet, may be implicated in asthma occurrence and severity. Magnesium (Mg) is a dietary element that may impact asthma (3). Higher intakes of dietary Mg are associated with decreased risk of asthma and wheezing (4), better lung function, and reduced bronchial reactivity (4, 5). Certain population groups, including people with asthma, may not be obtaining adequate dietary Mg and, as a result, may have a compromised Mg status (4). When compared to controls, people with asthma have been reported to have reduced levels of serum and erythrocyte Mg (6, 7). However, others have found no difference in Mg status between asthma and control subjects (8, 9). Despite the importance of Mg to nutrition and health, assessment of Mg status in humans is challenging. Current markers are limited with regard to their being sensitive and specic appraisals of total body Mg (10). Because the amount of Mg present in serum represents less than 1% of the total body stores, it is unclear whether serum Mg is an accurate indicator of Mg status.
Corresponding author: Alexandra G. Kazaks, Ph.D., Department of Nutrition, University of California, Davis, 1 Shields Avenue, Davis, CA 95616; E-mail: agkazaks@ucdavis.edu
Serum Mg exists as fractions that are either ionized, complexed, or bound to serum protein (11). Ionized Mg, the physiologically active form, may be a better index of overall Mg status, and a more sensitive index of deciency, than total serum Mg (12). Other researchers have suggested that intracellular compartments, such as leukocytes and erythrocytes, may more adequately reect Mg stores in patients with asthma. One group showed that 40% of the people with asthma and 11% of controls were decient in Mg, as measured with a Mg loading test; Mg retention was inversely correlated with erythrocyte Mg concentration (13). However, Basso et al. found that, in women receiving Mg supplements, sequential erythrocyte Mg measurements were not useful for monitoring Mg intake and status (14). While the most accurate evaluations of Mg status may be bone and muscle biopsies (10), they are extraordinarily invasive methods of obtaining information about Mg status from people who are not already undergoing such procedures. Using an IV Mg loading test, Cohen, et al. in 1990 reported that increased Mg retention was correlated with decreased bone Mg (15). The principle of the IV Mg loading test is that normal individuals will excrete 80 to 100% of the amount of Mg administered within 24 hours. In contrast, the Mg-depleted individual will retain a large amount of the infused Mg to restore underlying tissue decits. The diagnosis of Mg depletion is based on the percent of Mg retained after an IV infusion. Rob and colleagues established that a one-hour IV Mg loading test could accurately measure Mg decits (16). The aim of this study was to evaluate whether Mg status was different in subjects with mild to moderate asthma compared to healthy control subjects. To obtain a comprehensive estimation of Mg status, we measured ve currently used indices of Mg status: ionized Mg in serum (iMg), total serum Mg (S-Mg), erythrocyte Mg (R-Mg), and intravenous Mg
783
784 load testing (IV Mg). Twenty-four hour dietary recall was used to determine Mg intake from food and water. Numerous studies have investigated the relationship between Mg and pulmonary function in severe asthma populations. In this investigation, we studied asthma subjects with mild to moderate asthma. To compare Mg status with airway narrowing, we used pulmonary function tests (PFT) to assess airow and methacholine challenge testing (MCCT) to gauge bronchial hyperreactivity. MCCT results are expressed as PC20 FEV1 , which is the concentration of drug that causes a 20% fall in forced expiratory volume in 1 second (FEV1 ) when compared to baseline (17, 18). It was hypothesized that Mg status and lung function would be lower in the subjects with asthma when compared to healthy controls, and that Mg status would be related to lung function. We also evaluated whether there were interrelationships between indices of Mg status that would be useful for identifying sensitive and specic indicators of Mg status. METHODS Participants Eighteen men and 36 women aged 21 to 55 years, who fullled diagnostic criteria for mild to moderate asthma according to National Asthma Education and Prevention Program (19) guidelines, and who used only beta-agonists or inhaled corticosteroids (ICS) for asthma treatment, participated in the study. We recruited 17 male and 30 female controls, who were matched to asthma subjects with regard to age and body mass index (BMI). Exclusion criteria at the screening visit were: abnormal kidney function, other lung disease, use of Mg-containing products that provided more than 50 mg of Mg per day within the past 3 months, alcohol or substance abuse, uncontrolled hypertension, cardiovascular disease, diabetes, immunodeciency or infection with HIV, current use of theophylline or leukotriene antagonists, smoking, psychiatric disorders that make participation difcult, pregnancy or breast feeding, history of emergency room care or hospitalization in the last 6 months, or use of prednisone in the past 3 months. Subjects were recruited with yers and newspaper advertisements from the general public in the Sacramento, California, area. Written informed consent was obtained from all participants, and the University of California, Davis, Institutional Review Board approved the study protocol. STUDY DESIGN Procedures At the screening visit, all subjects underwent a health interview and a physical exam. Measurements of height and weight were taken. Weight was measured at each succeeding visit. A fasting venous blood sample was analyzed for Chem 7 and CBC panels. To determine lung function, all subjects were given spirometry testing. Only those subjects who had a forced expiratory volume in 1 second (FEV1 ), percent predicted (% pred) >60% continued in the study. At the second visit, all subjects were given a methacholine challenge test to determine bronchial hyperresponsiveness. A positive MCCT (PC20 < 8 mg/mL methacholine) for asthma subjects and a negative MCCT for controls was necessary for continued participation. At visit three, fasting serum was col-
A. G. KAZAKS ET AL.
lected from all subjects and analyzed for Mg concentration (S-Mg, R-Mg, and iMg). All subjects were given an IV Mg load test (0.1 mmol Mg/kg) (16) and asked to collect urine for the following 24-hour period. On two separate occasions, all subjects were asked to recall what they ate in the previous 24 hours to determine dietary Mg intake. Asthma subjects were recruited for a six-month study of Mg supplementation; however, the data presented here only include their baseline values compared to controls. Subject Assessments Body weight. Body weight was measured in light clothing, without shoes, using a balance scale. Height was measured using a wall mounted stadiometer. Body mass index was calculated as weight/height2 (kg/m2 ). Spirometric tests. Spirometry was performed with the Koko Pneumotach and Koko Spirometry Software (PDS/Ferraris, Lousville, CO., USA) after a bronchodilatorfree period of at least 8 hours. Flow-volumes including FEV1 (forced expiratory volume in 1 second), forced vital capacity (FVC), FEF2575% (forced expiratory ow rate between 25 and 75% of FEV, a midow rate that is usually increased with airway obstruction), and PEFR (peak expiratory ow rate) were measured according to American Thoracic Society (ATS) criteria (19). NHANES III spirometry reference standards were used for percent predicted values (20). Methacholine challenge test. Bronchial hyperresponsiveness to methacholine was assessed with a Koko Digidoser (PDS/Ferraris, Lousville, CO, USA) and was expressed as the cumulative concentration of methacholine required to provoke a 20% decreased in FEV1 (PC-20) according to ATS guidelines (17, 18). The subjects were asked not to use shortacting beta agonists for at least 8 hours prior, long-acting bronchodilators for 48 hours prior, and antihistamines or ICS for 72 hours prior to the test. The test was rescheduled if the subject had a current respiratory tract infection. Ionized Mg. Fasting serum was analyzed in duplicate using a Nova CRT magnesium ion selective electrode (Nova Biomedical, Waltham, MA, USA). Total serum, erythrocyte, urine and drinking water Mg. Total Mg in serum, erythrocytes, urine, and drinking water was analyzed using sequential ICP-AES (Trace Scan; Thermo Electron Corp, Willmington, MA, USA). National Bureau of Standards bovine liver samples (NBS 1577b; Gaithersburg, MD, USA) were included with each run to ensure accuracy. Mg from erythrocytes was acid precipitated and analyzed according to the method described by Clegg (21). Serum Mg concentration was analyzed in the supernate of serum samples acidied with 1 N HNO3 and centrifuged at 3,000 rpm for 12 minutes. Urine was kept refrigerated or chilled with ice packs during the 24-hour collection. A sample was acidied with 0.2 milliliters (mL) of concentrated HCl per 50 mL of urine. For analysis, the acidied urine was diluted with 0.1 N HNO3 , vortexed, and analyzed for Mg concentration. IV Mg load test. Subjects were infused with a sterile Mg solution (0.1 mmol Mg/kg body weight as Mg sulfate
MEASURING MAGNESIUM STATUS IN ASTHMA in 500 mL isotonic saline) for one hour and were asked to collect urine for the following 24-hr period. Subjects were informed of Mg-rich foods that were to be avoided during the collection period. The percent Mg retention was used to assess total body Mg status (16). Dietary Mg intake. Participants were twice asked to recall food and water intake during the previous 24 hours. The records were reviewed by a registered dietitian and were analyzed using Food Processor software (ESHA Research, Inc., Salem, OR, USA). Subjects provided samples of drinking water (bottled, tap) for Mg analysis. Results from a subjects water sample analysis were used when they exceed 10 mg/L, which is the default value for the Food Processor program. Mg intake was presented as average daily total and energy adjusted intake and as a percentage of the Mg Recommended Daily Allowance (RDA) goal for age and gender. Statistics. Results were expressed as mean SE. Data were analyzed using Student t-tests. Correlations were assessed with simple and multiple linear regressions. Analyses were conducted with Statview Version 5.0.1 (SAS Institute, Cary, NC, USA). P values .05 were considered signicant. RESULTS Demographic, BMI, and Pulmonary Function Data There were no signicant differences in age and BMI between asthma and control subjects (Table 1). The pulmonary function test results were reported as percent predicted using NHANES III reference standards (20). The values for FEV1 , FEV1 /FVC, and FEF2575% were signicantly lower in the subjects with asthma compared with controls, whereas FVC and PEFR were similar between groups. The MCCT to assess bronchial reactivity was categorized as stages 1 through 6 according to the dose concentration required to provoke a 20% decreased in FEV1 (the doses were: saline, 0.5, 1, 2, 4, and 8 mg/mL methacholine). All control subjects had a negative MCCT. Subjects with asthma had a mean positive response at stage 4 which corresponds to a dose of 2 mg/mL methacholine.
785
TABLE 2.Indices of magnesium status in controls and subjects with asthma.
Control Asthma
iMg (mmol/L) S-Mg (mmol/L) R-Mg (mmol/L) IV Mg load retention (%) Avg diet Mg (mg) % Diet Mg Goal Diet Mg/Kcal
0.58 0.01 0.77 0.01 2.8 0.1 19 5 326 15 94 5 0.16 0.01
0.57 0.01 0.76 0.01 2.8 0.1 24 4 306 17 89 5 0.15 0.01
Mean SE. iMg = ionized magnesium; S-Mg = total serum magnesium; R-Mg = erythrocyte magnesium; Avg diet Mg = average dietary magnesium; % Diet Mg Goal = percentage of RDA for age and gender; Diet Mg/Kcal = ratio of magnesium intake per kilocalorie intake.
Mg Status and Pulmonary Function There were no signicant differences in any biochemical or dietary measure of Mg status between asthma and control subjects (Table 2). iMg and R-Mg levels in all subjects were within normal reference ranges, but 6/52 asthma subjects and 4/47 controls had S-Mg of <0.70 mmol/L and can be described as Mg decient (Elin 1987). When S-Mg data were divided into tertiles (low <0.64 mmol/L; high >0.80 mmol/L), there were no signicant differences between the low and high tertiles of Mg serum concentration and any lung function parameter, both when groups were analyzed separately or together. Mg Status Measurement Inter-Relationships There was a strong positive relationship between S-Mg and iMg (r = 0.64; p < 0.0001) in all subjects (Figure 1). Even after adjusting for BMI, age, and gender, the relationship between S-Mg and iMg was still highly signicant. We also found a positive association between S-Mg and R-Mg (r = 0.26; p = 0.011) within the whole population (Figure 2), although the relationship weakened when analyzed separately in asthma (r = 0.25; p = 0.078) and controls (r = 0.26; p = 0.073). iMg was positively associated with R-Mg in all subjects (r = 0.29; p = 0.004) (Figure 3). When measured only in the asthma subjects, the association remained signicant (r = 0.30; p = 0.031) and approached signicance in controls (r = 0.30; p = 0.057). IV retention was not related to iMg, S-Mg, or R-Mg. IV Mg retention was negatively correlated with % diet Mg goal in all subjects, but this association remained signicant only in the asthma group when measured separately (r = 0.38; p = 0.006). DISCUSSION The aim of this study was to use multiple indices to assess Mg status and to correlate Mg status with lung function in subjects with mild to moderate asthma and healthy control subjects. We also evaluated the interrelationships of the Mg indices to determine which marker, or combination of markers, would provide the most accurate assessment of Mg status. As expected, we found that lung function measured by spirometric testing was signicantly lower in people with asthma; however, our hypothesis that Mg status would be lower in subjects with asthma was not conrmed. There was no signicant difference in any of the ve Mg parameters measured between asthma and control subjects. These
TABLE 1.Characteristics of control and asthma subjects.
Control Asthma
N Gender (males/females) Age (years) BMI (kg/m2 ) FEV1 % pred FVC % pred FEV1 / FVC % pred FEF 2575% % pred PEFR MCCT stage
47 17/30 37 1 27 1 96 2 98 2 97 1 91 3 90 2 na
52 16/36 37 1 28 1 89 2 96 2 92 1 73 3 84 3 42
Mean SE. P 0.05. P 0.001. Methacholine challenge test results were categorized as stages 1 through 6 according to the dose concentration required to provoke a 20% decreased in FEV1. All control subjects had a negative MCCT. BMI = body mass index; % pred = % of predicted value; FEV% = forced expiratory 1 volume in 1 second; FVC = forced vital capacity; FEF 2575% = forced expiratory ow rate between 25 and 75% of FEV; PEFR = peak expiratory ow rate; MCCT = methacholine challenge test.
786
A. G. KAZAKS ET AL.
FIGURE 1.Relationship between S-Mg and iMg (n = 52 asthma and n = 47 control subjects, r = 0.64, p = 0.0001).
ndings are in agreement with some studies that showed no difference in R-Mg or S-Mg (8, 9, 22, 23). These aforementioned results are in contrast with other studies that reported that Mg status was lower in people with asthma (6, 7, 13, 24). Altura and colleagues reported that iMg, but not S-Mg, was lower than the expected normal range in asthma patients (25).
The lack of correlation between pulmonary function and Mg status is in contrast with studies that reported a negative correlation between airway reactivity and R-Mg (7, 26), and between S-Mg and severity of asthma (27). Our results are similar to other research that showed no correlation between Mg status and FEV1 or PEFR (6, 24), The reasons for the inconsistency in results may be due to differences in age,
FIGURE 2.Relationship between S-Mg and R-Mg (n = 52 asthma and n = 47 control subjects, r = 0.26; p = 0.011).
MEASURING MAGNESIUM STATUS IN ASTHMA
787
FIGURE 3.Relationship between iMg and R-Mg (n = 52 asthma and n = 47 control subjects, r = 0.29; p = 0.004).
gender, BMI, and severity of asthma among subjects. All of our subjects were matched for gender and BMI, and a MCCT was used to help conrm presence or absence of asthma. The asthma subjects all had mild to moderate asthma that was controlled only with inhaled beta agonists or ICS. They may have been controlled well enough that variation in Mg status did not have an obvious effect on lung function. Thus, our results cannot be extended to more severe asthma. Since there is considerable debate about which is the most accurate test to assess Mg status, we evaluated multiple Mg measurements to determine how the markers relate to each other, and the usefulness of one measure to predict others. We found that S-Mg was highly correlated to iMg in all subjects, or when analyzed separately within asthma and control groups. We also found positive, albeit weaker, associations between S-Mg and R-Mg. While iMg may be indicative of Mg status, ion-selective electrodes are not widely used. In contrast, measurement of S-Mg is a common test for Mg evaluation, and our research supports its use as an efcient indicator of Mg status in groups that have similar age, gender, BMI, and health status. The IV Mg load test has been suggested to be a sensitive test of Mg status (16, 28). However, we did not nd any correlation between percent Mg retention and any other index of Mg status except dietary intake. The % diet Mg goal was negatively correlated with %IV Mg retention in all subjects, but this association was signicant only in the asthma group when measured separately. It is unknown whether people with asthma are more sensitive to dietary Mg uctuations. The IV Mg load test described by Rob (16) that was used in this study varies from other tests in that it does not include a 24-hour urine collection before the Mg infusion, and the Mg load is infused in one hour. This type of loading test may not be comparable to other, longer infusion test protocols.
The standard deviation about the %IV retention means was greater than planned for, and it affected our ability to detect differences between groups. Given our sample size of 52 asthma subjects and 47 controls, a post hoc analysis showed that we could detect a difference of 13 percentage points with 80% power. Our sample means were separated by a 5 percentage point difference; therefore, our ability to detect differences between groups was limited. Further studies with larger sample sizes are needed to dene the relationship between %IV Mg retention asthma and other measures of Mg status in individuals with mile to moderate asthma. CONCLUSIONS In summary, this study demonstrated that, in this matched population of people with mild to moderate asthma and healthy controls, there was no difference in Mg status as assessed by ve Mg indices, and no effect of Mg on pulmonary function. No association between the IV Mg test and any other measure of Mg status, except dietary intake, was found. Since IV Mg retention was inuenced by dietary intake in asthma, but not in controls, people with asthma may respond to dietary Mg intervention. Total Mg in serum closely reected iMg values suggesting that S-Mg can be used in place of other more expensive or complicated tests as a useful clinical diagnostic monitor. ABBREVIATIONS American Thoracic Society body mass index forced expiratory volume in 1 second forced vital capacity inhaled corticosteroids ionized magnesium
ATS BMI FEV1 FVC ICS iMg
788 IV Mg MCCT Mg NHANES NHLBI PFT R-Mg S-Mg intravenous magnesium load methacholine challenge testing magnesium National Health and Nutrition Examination Survey National Heart, Lung, and Blood Institute pulmonary function tests erythrocyte magnesium total serum magnesium
A. G. KAZAKS ET AL.
12. Altura BT, Burack JL, Cracco RQ, Galland L, Handwerker SM, Markell MS, et al. Clinical studies with the NOVA ISE for IMg2+. Scand J Clin Lab Invest 1994; Suppl. 217:5367. 13. Hashimoto Y, Nishimura Y, Maeda H, Yokoyama M. Assessment of magnesium status in patients with bronchial asthma. J Asthma 2000; 37(6):489 496. 14. Basso LE, Ubbink JB, Delport R. Erythrocyte magnesium concentration as an index of magnesium status: a perspective from a magnesium supplementation study. Clin Chim Acta 2000; 291(1):18. 15. Cohen L, Laor A. Correlation between bone magnesium concentration and magnesium retention in the intravenous magnesium load test. Magnes Res 1990; 3(4):271274. 16. Rob PM, Dick K, Bley N, Seyfert T, Brinckmann C, Hollriegel V, et al. Can one really measure magnesium deciency using the short-term magnesium loading test? J Intern Med 1999; 246(4):373378. 17. Hunter CJ, Brightling CE, Woltmann G, Wardlaw AJ, Pavord ID. A comparison of the validity of different diagnostic tests in adults with asthma. Chest 2002; 121(4):10511057. 18. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This ofcial statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 2000; 161(1):309329. 19. NHLBI. NAEPP Expert Panel Report: Guidelines for the Diagnosis and Management of AsthmaUpdate on Selected Topics; 2002. 20. Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 1999; 159(1):179187. 21. Clegg M. Biol Trace Element Res 1981; 3:107115. 22. Picado C, Deulofeu R, Lleonart R, Agusti M, Mullol J, Quinto L, et al. Dietary micronutrients/antioxidants and their relationship with bronchial asthma severity. Allergy 2001; 56(1):4349. 23. Falkner D, Glauser J, Allen M. Serum magnesium levels in asthmatic patients during acute exacerbations of asthma. Am J Emerg Med 1992; 10(1):13. 24. Oladipo OO, Chukwu CC, Ajala MO, Adewole TA, Afonja OA. Plasma magnesium in adult asthmatics at the Lagos University Teaching Hospital, Nigeria. East Afr Med J 2003; 80(9):488491. 25. Altura BT, Altura BM. Measurement of ionized magnesium in whole blood, plasma, and serum with a new ion-selective electrode in healthy and diseased human subjects. Magnes Trace Elem 1991; 10(24):9098. 26. Dominguez LJ, Barbagallo M, Di Lorenzo G, Drago A, Scola S, Morici G, et al. Bronchial reactivity and intracellular magnesium: a possible mechanism for the bronchodilating effects of magnesium in asthma. Clin Sci (Lond) 1998; 95(2):137142. 27. Alamoudi OS. Hypomagnesaemia in chronic, stable asthmatics: prevalence, correlation with severity and hospitalization. Eur Respir J 2000; 16(3):427 431. 28. Gullestad L, Midtvedt K, Dolva LO, Norseth J, Kjekshus J. The magnesium loading test: reference values in healthy subjects. Scand J Clin Lab Invest 1994; 54(1):2331.
ACKNOWLEDGMENTS This study was funded in part by RO1 AT00652 from NIH/NCCAM and T32 DK 07355. We express gratitude to the subjects who participated in this study. We also thank Mr. Randev Sandhu for his expertise in subject management, Joel Commisso for mineral analysis, and Janet Peerson for statistical assistance. REFERENCES
1. Masoli M, Fabian D, Holt S, Beasley R. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy 2004; 59(5):469478. 2. Asthmas Impact on the U.S. Population. In: Center for Disease Control; 2005. 3. Mathew R, Altura BM. The role of magnesium in lung diseases: asthma, allergy and pulmonary hypertension. Magnes Trace Elem 1991; 10(24):220 228. 4. Britton J, Pavord I, Richards K, Wisniewski A, Knox A, Lewis S, et al. Dietary magnesium, lung function, wheezing, and airway hyperreactivity in a random adult population sample. Lancet 1994; 344(8919):357362. 5. Soutar A, Seaton A, Brown K. Bronchial reactivity and dietary antioxidants. Thorax 1997; 52(2):166170. 6. Zervas E, Papatheodorou G, Psathakis K, Panagou P, Georgatou N, Loukides S. Reduced intracellular Mg concentrations in patients with acute asthma. Chest 2003; 123(1):113118. 7. Emelyanov A, Fedoseev G, Barnes PJ. Reduced intracellular magnesium concentrations in asthmatic patients. Eur Respir J 1999; 13(1):3840. 8. Fantidis P, Ruiz Cacho J, Marin M, Madero Jarabo R, Solera J, Herrero E. Intracellular (polymorphonuclear) magnesium content in patients with bronchial asthma between attacks. J R Soc Med 1995; 88(8):441445. 9. de Valk HW, Kok PT, Struyvenberg A, van Rijn HJ, Haalboom JR, Kreukniet J, et al. Extracellular and intracellular magnesium concentrations in asthmatic patients. Eur Respir J 1993; 6(8):11221125. 10. Elin RJ. Assessment of magnesium status. Clin Chem 1987; 33(11):1965 1970. 11. Speich M, Bousquet B, Nicolas G. Reference values for ionized, complexed, and protein-bound plasma magnesium in men and women. Clin Chem 1981; 27(2):246248.
You might also like
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderFrom EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 8: UrologyFrom EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyRating: 3 out of 5 stars3/5 (1)
- Effect of Daily Intake of Yoghurt and Bread Enriched With Biologically Active Substances On Blood Lipids and Vitamin A in Adolescents and Young AdultsDocument9 pagesEffect of Daily Intake of Yoghurt and Bread Enriched With Biologically Active Substances On Blood Lipids and Vitamin A in Adolescents and Young AdultsEsmeralda SantillanNo ratings yet
- Respi DiseaseDocument6 pagesRespi Diseaseakuro imaizumiNo ratings yet
- Relationship Between Nutritional Status and The Glomerular Filtration Rate: Results From The MDRD StudyDocument16 pagesRelationship Between Nutritional Status and The Glomerular Filtration Rate: Results From The MDRD Studyannaafia69969No ratings yet
- Valeriaceci Journal Editor 18 Degirmenci 6043Document8 pagesValeriaceci Journal Editor 18 Degirmenci 6043naomigabeNo ratings yet
- P ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 2000)Document6 pagesP ('t':3) Var B Location Settimeout (Function (If (Typeof Window - Iframe 'Undefined') (B.href B.href ) ), 2000)chokylugolNo ratings yet
- Am. J. Epidemiol.-2002-Gilliland-125-31Document7 pagesAm. J. Epidemiol.-2002-Gilliland-125-31dicky wahyudiNo ratings yet
- Walker, 1998 - Magnesium Supplementation Alleviates Premenstrual Symptoms of Fluid RetentionDocument9 pagesWalker, 1998 - Magnesium Supplementation Alleviates Premenstrual Symptoms of Fluid Retentionkatharinabackes43No ratings yet
- Dietary Counselling and Food Fortification in Stable COPD: A Randomised TrialDocument7 pagesDietary Counselling and Food Fortification in Stable COPD: A Randomised TrialJames Cojab SacalNo ratings yet
- Dietary Intake, Blood Pressure and Osteoporosis: Original ArticleDocument5 pagesDietary Intake, Blood Pressure and Osteoporosis: Original ArticleCorin Boice TelloNo ratings yet
- Nutrients 11 01734 v3Document11 pagesNutrients 11 01734 v3Fauziah Furqanah SyamNo ratings yet
- Multiple Micronutrient Supplements During Pregnancy Do Not Reduce Anemia or Improve Iron Status Compared To Iron-Only Supplements in Semirural MexicoDocument14 pagesMultiple Micronutrient Supplements During Pregnancy Do Not Reduce Anemia or Improve Iron Status Compared To Iron-Only Supplements in Semirural MexicoRina ChairunnisaNo ratings yet
- The Effect of Ramadan Fasting On Tuberculin Skin Test and Leukocyte Count Dalam Bhasa InggrisDocument4 pagesThe Effect of Ramadan Fasting On Tuberculin Skin Test and Leukocyte Count Dalam Bhasa InggrisファラハンNo ratings yet
- Colorectal 4Document6 pagesColorectal 4Regina SeptianiNo ratings yet
- Out 11 PDFDocument10 pagesOut 11 PDFBlank SpaceNo ratings yet
- Higher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsDocument7 pagesHigher Selenium Status Is Associated With Adverse Blood Lipid Profile in British AdultsHerly Maulida SurdhawatiNo ratings yet
- Leptin and Energy MetabDocument7 pagesLeptin and Energy MetabNiar MarhaliNo ratings yet
- JournalDocument12 pagesJournalUmi RianaNo ratings yet
- Nutrients: Micronutrient Status in 153 Patients With Anorexia NervosaDocument10 pagesNutrients: Micronutrient Status in 153 Patients With Anorexia NervosaReza Yusna HanastaNo ratings yet
- Journal 8Document6 pagesJournal 8Aceking MarquezNo ratings yet
- Efficacy of Magnesium in Children With Bronchial Asthma: 2 TrendDocument3 pagesEfficacy of Magnesium in Children With Bronchial Asthma: 2 TrendSukma EffendyNo ratings yet
- Magnesium Intake and Colorectal Tumor Risk: A Case-Control Study and Meta-AnalysisDocument10 pagesMagnesium Intake and Colorectal Tumor Risk: A Case-Control Study and Meta-AnalysisRegina SeptianiNo ratings yet
- Rajiv Gandhi University of Health Sciences, Karnataka BangaloreDocument13 pagesRajiv Gandhi University of Health Sciences, Karnataka BangaloreFebri SuryoNo ratings yet
- 1 AntecedentesDocument1 page1 AntecedentesEdgar RomeroNo ratings yet
- Novel Insights On Nutrient Management of Sarcopenia in ElderlyDocument15 pagesNovel Insights On Nutrient Management of Sarcopenia in ElderlyMario Ociel MoyaNo ratings yet
- Antioxidant Effects of Zinc Supplementation in Tunisians With Type 2 Diabetes MellitusDocument6 pagesAntioxidant Effects of Zinc Supplementation in Tunisians With Type 2 Diabetes MellitusgautomsahariaNo ratings yet
- Magnesium Deficiency and Its Lack of Association With Asthma in Taiwanese Elementary School ChildrenDocument7 pagesMagnesium Deficiency and Its Lack of Association With Asthma in Taiwanese Elementary School ChildrenSukma EffendyNo ratings yet
- Graessler 2012Document9 pagesGraessler 2012dora guzmanNo ratings yet
- 2020-2-ABR - Stability and Predictors of Poor 6-Min Walking Test Performance Over 2 Years in Patients With COPDDocument12 pages2020-2-ABR - Stability and Predictors of Poor 6-Min Walking Test Performance Over 2 Years in Patients With COPDRodrigo Martín San AgustínNo ratings yet
- Pharmacokinetic Profile of Oral Magnesium HydroxideDocument6 pagesPharmacokinetic Profile of Oral Magnesium HydroxideRegina Marsha XaveriaNo ratings yet
- Tight GlycemicDocument10 pagesTight GlycemicIsmail Mohammed AbdelgawadNo ratings yet
- Vegetable But Not Animal Protein Intake Is Associated To A Better Physical Performance: A Study On A General Population Sample of AdultsDocument7 pagesVegetable But Not Animal Protein Intake Is Associated To A Better Physical Performance: A Study On A General Population Sample of AdultsEgemen ErsanNo ratings yet
- Changes in Bone Mineral Density in Women With Earlyonset Androgenetik Alopecia and Their Correlations With Hairloss Stages A CrossDocument8 pagesChanges in Bone Mineral Density in Women With Earlyonset Androgenetik Alopecia and Their Correlations With Hairloss Stages A CrossRo KohnNo ratings yet
- Metformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyDocument9 pagesMetformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyIam MaryamNo ratings yet
- 5 Revathi EtalDocument5 pages5 Revathi EtaleditorijmrhsNo ratings yet
- Review of Literature: Chapter - 2Document46 pagesReview of Literature: Chapter - 2InaGargNo ratings yet
- 1 s2.0 S1063458407002324 MainDocument7 pages1 s2.0 S1063458407002324 MainShubhra Ray ChaudhuryNo ratings yet
- Bdavighi 26 Safaeiyan 5481Document7 pagesBdavighi 26 Safaeiyan 5481Maikon MarquêsNo ratings yet
- Decrease in Paco2 With Prone Position Is Predictive of Improved Outcome in Acute Respiratory Distress SyndromeDocument7 pagesDecrease in Paco2 With Prone Position Is Predictive of Improved Outcome in Acute Respiratory Distress SyndromedarwigNo ratings yet
- Journal Stress OksidatifDocument8 pagesJournal Stress OksidatifMiftakhur RohmahNo ratings yet
- Order - 523187 - Main Document With Abstract - TRACKED - REVISEDDocument12 pagesOrder - 523187 - Main Document With Abstract - TRACKED - REVISEDAn MNo ratings yet
- Effects of LifePak Supplementation On Antioxidant Status and LDL-Oxidation in Healthy Non-SmokersDocument12 pagesEffects of LifePak Supplementation On Antioxidant Status and LDL-Oxidation in Healthy Non-SmokersCherry San DiegoNo ratings yet
- Fin 2104Document6 pagesFin 2104Prima Artya KurniawanNo ratings yet
- Gastro Oesophageal RefluxDocument7 pagesGastro Oesophageal Refluxjustifieda13No ratings yet
- Nutrients 12 00932 v2Document16 pagesNutrients 12 00932 v2Mario CoelhoNo ratings yet
- Gastrico Vs TranspiloricaDocument6 pagesGastrico Vs TranspiloricaMagali FloresNo ratings yet
- Obesity in Aspirin-Tolerant and Aspirin-Intolerant AsthmaticsDocument5 pagesObesity in Aspirin-Tolerant and Aspirin-Intolerant Asthmaticsxiongmao2389No ratings yet
- 2018 Article 251 PDFDocument7 pages2018 Article 251 PDFErick AlvarezNo ratings yet
- Effect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenDocument5 pagesEffect of Zinc Supplementation On Insulin Resistance and Metabolic Risk Factors in Obese Korean WomenFahmy2015No ratings yet
- Blood Sugar Lowering Effect of Zinc and Multi Vitamin/ Mineral Supplementation Is Dependent On Initial Fasting Blood GlucoseDocument14 pagesBlood Sugar Lowering Effect of Zinc and Multi Vitamin/ Mineral Supplementation Is Dependent On Initial Fasting Blood GlucoseNorries Jonell CaballarNo ratings yet
- The Effects of Rosiglitazone and Metformin On Oxidative Stress and Homocysteine Levels in Lean Patients With Polycystic Ovary SyndromeDocument8 pagesThe Effects of Rosiglitazone and Metformin On Oxidative Stress and Homocysteine Levels in Lean Patients With Polycystic Ovary SyndromeElena VisterniceanNo ratings yet
- Dietary Fat and Coronary Heart Disease - Summary of Evidence From Prospective Cohort and Random Is Ed Controlled TrialsDocument29 pagesDietary Fat and Coronary Heart Disease - Summary of Evidence From Prospective Cohort and Random Is Ed Controlled Trialsa_rogall7926No ratings yet
- Peanut Consumption and Cardiovascular RiskDocument6 pagesPeanut Consumption and Cardiovascular RiskWahyuningsih HamidNo ratings yet
- Hepatology - April 1993 - Mendenhall - A Study of Oral Nutritional Support With Oxandrolone in Malnourished Patients WithDocument13 pagesHepatology - April 1993 - Mendenhall - A Study of Oral Nutritional Support With Oxandrolone in Malnourished Patients WithkentryzbustamanteNo ratings yet
- Review Article Effect of The Dietary Fat Quality On Insulin SensitivityDocument9 pagesReview Article Effect of The Dietary Fat Quality On Insulin SensitivityGilberto BicalhoNo ratings yet
- DisasterDocument29 pagesDisasteramiNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 19: MiscellaneousFrom EverandComplementary and Alternative Medical Lab Testing Part 19: MiscellaneousNo ratings yet
- Histopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationFrom EverandHistopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationNo ratings yet
- A6 MMWR Update On IGRA in Diagnosis of TB 2010Document28 pagesA6 MMWR Update On IGRA in Diagnosis of TB 2010Rhea DerijeNo ratings yet
- Tanpa JudulDocument689 pagesTanpa JudulSukma Effendy100% (3)
- Cpns Soal2Document25 pagesCpns Soal2Sukma EffendyNo ratings yet
- 2010 Research Quantitative Analysis of Urine Based Assay For Detection of LAM in Patient With TB PDFDocument3 pages2010 Research Quantitative Analysis of Urine Based Assay For Detection of LAM in Patient With TB PDFSukma EffendyNo ratings yet
- 2010 Systematic Review Interferon Gamma Release Assays For Tuberculosis Screening of Healthcare WorkersDocument9 pages2010 Systematic Review Interferon Gamma Release Assays For Tuberculosis Screening of Healthcare WorkersSukma EffendyNo ratings yet
- 1999, JCP REVIEW The Molecular Basis of Disorders of Red Cell EnzymesDocument4 pages1999, JCP REVIEW The Molecular Basis of Disorders of Red Cell EnzymesSukma EffendyNo ratings yet
- MRSA Recommendations: Members of The Task ForceDocument13 pagesMRSA Recommendations: Members of The Task ForceNasrullah Samejo 2No ratings yet
- 032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsDocument59 pages032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsSukma EffendyNo ratings yet
- 032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsDocument59 pages032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsSukma EffendyNo ratings yet
- MRSA Infections: Jama Patient PageDocument1 pageMRSA Infections: Jama Patient PageSukma EffendyNo ratings yet
- Building A Smart Laboratory: An Introduction To The Integrated LabDocument36 pagesBuilding A Smart Laboratory: An Introduction To The Integrated LabSukma EffendyNo ratings yet
- 032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsDocument59 pages032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsSukma EffendyNo ratings yet
- 032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsDocument59 pages032-Roubort-Advantages and Integration of Multi-Vendor LIS EnvironmentsSukma EffendyNo ratings yet
- 02 RX Monaco (RX5000)Document1 page02 RX Monaco (RX5000)Sukma EffendyNo ratings yet
- An Overview of The Pulmonary SystemDocument9 pagesAn Overview of The Pulmonary SystemSukma EffendyNo ratings yet
- Study of Lipid Peroxide and Lipid Profile in Diabetes Mellitus PDFDocument5 pagesStudy of Lipid Peroxide and Lipid Profile in Diabetes Mellitus PDFSukma EffendyNo ratings yet
- In Flight ArabicDocument12 pagesIn Flight ArabicSukma EffendyNo ratings yet
- Surveys Manual Glossary PDFDocument57 pagesSurveys Manual Glossary PDFSukma EffendyNo ratings yet
- National Geographic 2010-05Document164 pagesNational Geographic 2010-05arsivlik12100% (1)
- Anemia MonographDocument140 pagesAnemia MonographZaveri Hemant GirishkumarNo ratings yet
- In Flight ArabicDocument12 pagesIn Flight ArabicSukma EffendyNo ratings yet
- DM Lipid Profile With LDL PDFDocument1 pageDM Lipid Profile With LDL PDFSukma EffendyNo ratings yet
- Validated Sandwich ELISA For The Quantification of Von Willebrand Fact - PDF - 3236 PDFDocument9 pagesValidated Sandwich ELISA For The Quantification of Von Willebrand Fact - PDF - 3236 PDFSukma EffendyNo ratings yet
- DM Lipid Profile With LDL PDFDocument1 pageDM Lipid Profile With LDL PDFSukma EffendyNo ratings yet
- A Study of Oxidative Stress, Antioxidant Status and Lipid Profile in Diabetic Patient in The Western Region of Nepal PDFDocument7 pagesA Study of Oxidative Stress, Antioxidant Status and Lipid Profile in Diabetic Patient in The Western Region of Nepal PDFSukma EffendyNo ratings yet
- Serial NumberDocument1 pageSerial NumberSukma EffendyNo ratings yet
- Detection of Mycobacterium Tuberculosis in Blood Using The Xpert MTBRIF AssayDocument28 pagesDetection of Mycobacterium Tuberculosis in Blood Using The Xpert MTBRIF AssaySukma EffendyNo ratings yet
- Vascular Permeability ICAM-1: Role in Inflammation and in The Regulation ofDocument3 pagesVascular Permeability ICAM-1: Role in Inflammation and in The Regulation ofSukma EffendyNo ratings yet
- Detection of VWF PDFDocument11 pagesDetection of VWF PDFSukma EffendyNo ratings yet
- Evaluation of The GeneXpert MTBRIF Assay For Rapid Diagnosis TB ElimDocument5 pagesEvaluation of The GeneXpert MTBRIF Assay For Rapid Diagnosis TB ElimSukma EffendyNo ratings yet
- Compare PEFR Value Obtained From PFM and SpirometrDocument3 pagesCompare PEFR Value Obtained From PFM and SpirometrAfifah Solehah HamdanNo ratings yet
- SN Chugh - Bedside Medicine Without TearsDocument454 pagesSN Chugh - Bedside Medicine Without Tearsnb280100% (11)
- CMO 09 s2007Document55 pagesCMO 09 s2007XtiaRNo ratings yet
- Mannitol Clinical PREADocument9 pagesMannitol Clinical PREAjoelrequenaNo ratings yet
- Anatomy Final Exam Notes PDFDocument45 pagesAnatomy Final Exam Notes PDFLydia LalalandNo ratings yet
- C O P D: Hronic Bstructive Ulmonary IseaseDocument53 pagesC O P D: Hronic Bstructive Ulmonary IseaseLe KhoaNo ratings yet
- Prognostic Factors in Sarcoidosis: Mini ReviewDocument4 pagesPrognostic Factors in Sarcoidosis: Mini ReviewRicky SetiawanNo ratings yet
- BMR 191803 PDFDocument10 pagesBMR 191803 PDFArchita AgarwalNo ratings yet
- MIR Spirolab 3 - User ManualDocument77 pagesMIR Spirolab 3 - User ManualMirza CoricNo ratings yet
- An Overview of Asthma Management - UpToDateDocument83 pagesAn Overview of Asthma Management - UpToDatedocjime9004No ratings yet
- Lung VolumesDocument4 pagesLung VolumesLdv1 1No ratings yet
- Clinical Screening Form - AgriSafe NetworkDocument4 pagesClinical Screening Form - AgriSafe NetworkAgriSafeNo ratings yet
- ENDO Catalog CompactDocument44 pagesENDO Catalog Compactputeri rahmadaniNo ratings yet
- Copd Quick Reference Guide IcgpDocument28 pagesCopd Quick Reference Guide IcgpeimearNo ratings yet
- Noninvasiveventilationin Amyotrophiclateral Sclerosis: Jessica A. Cooksey,, Amen SergewDocument12 pagesNoninvasiveventilationin Amyotrophiclateral Sclerosis: Jessica A. Cooksey,, Amen SergewGeraldine HernándezNo ratings yet
- PHD Public Health Doctoral Thesis UpdateDocument163 pagesPHD Public Health Doctoral Thesis UpdateLianne Grace De VeraNo ratings yet
- Seca P8000 User ManualDocument50 pagesSeca P8000 User ManualJhancarlos JuanmacalderonNo ratings yet
- Multiple Choice Questions On Occupational Health and Safety (S. K. HALDAR) (Z-Library)Document440 pagesMultiple Choice Questions On Occupational Health and Safety (S. K. HALDAR) (Z-Library)gabriel castilloNo ratings yet
- Viasys Vmax Encore Technical Reference ManualDocument86 pagesViasys Vmax Encore Technical Reference ManualSilvio Guerrero100% (1)
- COPD Case PresentationDocument66 pagesCOPD Case PresentationAzima Abdelrhaman100% (4)
- Internal MedicineDocument277 pagesInternal MedicineAhmad Abu ArkoubNo ratings yet
- Block 4 Lung PathDocument31 pagesBlock 4 Lung PathShalini ShanmugalingamNo ratings yet
- Dräger Evita Infinity® V500 Elite: Advanced and Comprehensive Ventilation TherapyDocument4 pagesDräger Evita Infinity® V500 Elite: Advanced and Comprehensive Ventilation TherapyABHINANDAN SHARMANo ratings yet
- Wandfluh - Explanations Hydraulic ValvesDocument9 pagesWandfluh - Explanations Hydraulic ValvesHanzoNo ratings yet
- ACOG Practice Bulletin - Number 90 - Asthma in PregnancyDocument8 pagesACOG Practice Bulletin - Number 90 - Asthma in PregnancyDecha SaechoenNo ratings yet
- Interpretasi Hasil Faal Paru DR - DanielDocument33 pagesInterpretasi Hasil Faal Paru DR - DanielAyahnya RafliNo ratings yet
- See Radiology Like Never Before.: KDR AU-DDR SystemDocument6 pagesSee Radiology Like Never Before.: KDR AU-DDR SystemFanof EcdNo ratings yet
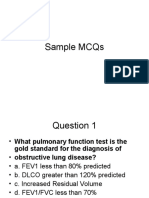
- Sample MCQs (Respiratory)Document12 pagesSample MCQs (Respiratory)Evan O'FlahertyNo ratings yet
- Astm Bronsic Diagnostic Si Management PDFDocument50 pagesAstm Bronsic Diagnostic Si Management PDFAlina GheNo ratings yet
- A Study On Chronic Obstructive Pulmonary DiseasesDocument12 pagesA Study On Chronic Obstructive Pulmonary DiseasesHamid RazaNo ratings yet