Professional Documents
Culture Documents
Complications of IV Therapy
Uploaded by
Lorilei Rose JuntillaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Complications of IV Therapy
Uploaded by
Lorilei Rose JuntillaCopyright:
Available Formats
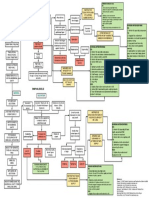
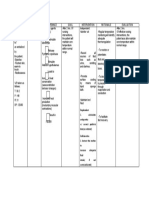
INFILTRATION Causes Dislodgement of the intravenous cannula from the vein which results in infusion of fluid into the
surrounding tissues. Clinical Manifestations Swelling, blanching, and coolness of surrounding skin and tissue. Discomfort, depending on nature of solution. Fluid flowing more slowly or ceasing. Absence of blood backflow in intravenous catheter and tubing. Nursing Interventions: 1.) Stop the infusion immediately and remove the intravenous needle or catheter. 2.) Restart the intravenous in the other arm. 3.) If infiltration is moderate to severe, apply warm, moist compresses and elevate the limb. 4.) If a vasoconstrictor agent (eg, norepinephrine bitartrate, dopamine) or vesicant has infiltrated, initiate emergency local treatment as directed. Serious tissue injury, necrosis, and sloughing may result if actions are not taken. 5.) Document interventions and assessments. Preventive Measures Make sure that the intravenous and the distal tubing are secured sufficiently with tape to prevent movement. Splint the patients arm or hand as necessary. Check the intravenous site frequently for complications.
THROMBOPHLEBITIS Causes Injury to vein during venipuncture, largebore needle or catheter use, or prolonged needle or catheter use. Clinical Manifestations Preventive Measures
Tenderness at first, Anchor the needle or catheter securely at then pain along the the insertion site. vein. Change the insertion site every 72hours Swelling, warmth, in adult patients (it may not be feasible to and redness at remove short-term catheters in neonates infusion sites; the and pediatric patients every 72 hours; Irritation to vein due vein may appear as however, they should be removed to rapid infusions or a red streak above immediately if contamination or
irritating solutions the insertion site. (eg, hypertonic glucose solutions, cytotoxic agents, strong acids or alkalis, potassium, and others); smaller veins are more susceptible. Clot formation at the end of the needle or catheter due to slow infusion rate. More commonly seen with synthetic catheters than steel needles. Nursing Interventions:
complications are suspected). Peripheral (short-term) catheters placed during an emergency where aseptic techniques could have been compromised should be removed no later than 48 hours. Use large veins for irritating fluid because of higher blood flow, which rapidly dilutes the irritant. Sufficiently dilute irritating agents before infusion.
1.) Apply cold compresses immediately to relieve pain and inflammation. 2.) Follow the moist, warm compresses to stimulate circulation and promote absorption. 3.) Document interventions and assessment.
BACTEREMIA Causes Underlying phlebitis. Clinical Manifestations Elevated temperature, chills Preventive Measures Follow the same measures as outlines for thrombophlebitis. Use strict sterile technique when inserting the intravenous or changing the intravenous dressing. Solutions should never hang longer than 24 hours. Change the insertion site every 72 hours in an adult patient and within 48 hours if catheter was placed in an emergent situation.
Contaminated Nausea, vomiting equipment or Elevated white infused solutions blood cell (WBC) Prolonged count placement of an intravenous device Malaise, increased (catheter or needle, pulse tubing, solution Backache, container) headache
Nonsterile intravenous insertion or dressing change. Crosscontamination by the patient with other infected areas if the body. A critically ill or immunosuppressed patient is at greatest risk of bacteremia.
May progress to Change continuous intravenous septic shock with administration sets no more frequently than profound every 72 hours and intermittent intravenous hypotension administration sets every 24 hours. Possible signs of Change intravenous dressing on a routine local infection at basis and immediately if it becomes intravenous compromised. insertion site (eg, a.) Gauze dressing that prevents redness, pain, foul visualization of the site should be drainage) changed every 48 hours. b.) Transparent semipermeable dressing on peripheral short-term site should be changed at site change or if the dressing loses its integrity. c.) Transparent semipermeable dressing on central line sites should be changed at least every 7 days. Maintain skin integrity of the infusion set.
Nursing Interventions: 1.) Discontinue infusion and intravenous cannula. 2.) Intravenous device should be removed and the tip cut off with sterile scissors, placed in a dry sterile container, and immediately sent to the laboratory for analysis. 3.) Check vital signs; reassure the patient. 4.) Obtain WBC count, as directed, and assess for the other sites of infection (urine, sputum, wound). 5.) Start appropriate antibiotic therapy immediately after receiving orders. 6.) Document interventions and assessments.
CIRCULATORY OVERLOAD Clinical Causes Manifestations Delivery excessive amounts of Increased pulse of Increased BP
Preventive Measures and Know whether patient has existing heart or kidney condition. Be particularly vigilant in the high-risk patient. CVP,
intravenous fluid (greater risk exists for elderly patients, infants, or patients with cardiac or renal insufficiency)
venous distension (engorged jugular Closely monitor the infusion flow rate. Keep accurate intake and output records. veins) Headache, anxiety Shortness of breath, tachypnea, coughing Pulmonary crackles Chest pain (if history of coronary artery disease) Splint the arm or hand if the intravenous flow rate fluctuates too widely with movement.
Nursing Interventions: 1.) Slow infusion to a keep-open rate and notify the health care provider. 2.) Monitor closely for worsening condition. 3.) Raise the patients head to facilitate breathing.
AIR EMBOLISM Causes A greater risk exists in central venous lines, when air enters catheter during tubing changes (air sucked in during inspiration due to negative intrathoracic pressure) Clinical Manifestations Preventive Measures
Drop in BP, Clear all air from tubing before infusion to elevated heart rate patient. Cyanosis, tachypnea Rise in CVP Change solution containers before they run dry.
Ensure that all connections are secure. Always use luerlock connections on Changes in mental central lines. status, loss of consciousness Use precipitate and air-eliminating filters unless contraindicated. Air in tubing delivered by Change intravenous tubing during intravenous push or expiration. infused by infusion pump. Nursing Interventions: 1.) Immediately turn the patient on his left side and lower the head of the bed; in this
2.) 3.) 4.) 5.)
position, air will rise to right atrium. Notify the health care provider immediately. Administer oxygen as needed. Reassure the patient. Document interventions and assessments.
MECHANICAL FAILURE (SLUGGISH INTRAVENOUS FLOW) Causes Clinical Manifestations Preventive Measures Needle lying against Check the intravenous often for the side of the vein, Sluggish intravenous patency and kinking. cutting off fluid flow flow Secure the intravenous well with tape Clot at the end of the Alarm of flow and an arm board, if necessary. catheter or needle regulator sounding Infiltration of May be signs of local intravenous cannula irritationswelling, coolness of skin Kinking of the tubing or catheter Nursing Interventions: 1.) Remove tape and check for kinking of tubing or catheter. 2.) Pull back the cannula because it may be lying against wall of vein, vein valve, or vein bifurcation. 3.) Elevate or lower needle to prevent occlusion of bevel. 4.) Move the patients arm to new position. 5.) Lower the solution container to below the level of patients heart and observe for blood backflow. 6.) If an electronic flow-rate regulator is in use, check its integrity. 7.) If none of the preceding steps produces the desired flow, remove the needle or catheter and restart infusion.
HEMORRHAGE Causes Clinical Manifestations Preventive Measures Cap all central lines with luer-lock adapters and connect luer-lock tubing to the capnot directly to the line. Tape all catheters securelyuse
Loose connection of Oozing or trickling of tubing or injection port blood from intravenous site or Inadvertent removal of catheter peripheral or central
catheter Hematoma Anticoagulant therapy
transparent dressing when possible for peripheral and central catheters. Tape the remaining catheter lumens and tubing in a loop so tension is not directly on the catheter. Keep pressure on sites where catheters have been removed (a minimum of 10 minutes for a patient taking anticoagulants).
VENOUS THROMBOSIS Clinical Causes Manifestations Infusion irritating solutions
Preventive Measures
of Slowing of Ensure proper dilution of irritating substances. intravenous infusion or inability to draw Ensure superior vena cava catheter tip blood from the placement for irritating solutions. Infection along central line catheter may preclude this Swelling and pain in syndrome the area of catheter or in the extremity Clot formation proximal to the around the intravenous line. catheter (This clot will eventually occlude the vein.) Nursing Interventions: 1.) Stop fluids immediately and notify health care provider. 2.) Reassure the patient and institute appropriate therapy: a.) Anticoagulants b.) Heat c.) Elevation of affected extremities d.) Antibiotics
You might also like
- Coronary Care Unit/ Cardiac Care Unit: Patient MonitorsDocument3 pagesCoronary Care Unit/ Cardiac Care Unit: Patient MonitorsPhoebe Kyles Camma100% (1)
- MastoiditisDocument37 pagesMastoiditisAkanksha EkkaNo ratings yet
- Nursing Care of Head InjuryDocument1 pageNursing Care of Head InjuryRaveen mayiNo ratings yet
- 21 BurnsDocument16 pages21 BurnsPriyaNo ratings yet
- Nsi PostureDocument2 pagesNsi PostureD. GandhirajNo ratings yet
- Devices Used in ICU: Critical Care NursingDocument95 pagesDevices Used in ICU: Critical Care NursinghendranatjNo ratings yet
- Hip Fracture Case Study: 39-Year-Old Male with EpilepsyDocument9 pagesHip Fracture Case Study: 39-Year-Old Male with EpilepsyufuNo ratings yet
- Effectiveness of Planned Teaching Programme On Knowledge Regarding Needle Stick Injury Among The Staff NursesDocument3 pagesEffectiveness of Planned Teaching Programme On Knowledge Regarding Needle Stick Injury Among The Staff NursesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Drug StudyDocument41 pagesDrug StudyVecky TolentinoNo ratings yet
- Care of CVP LineDocument36 pagesCare of CVP LineArchana GaonkarNo ratings yet
- Nutritional Assessment and Care PlanDocument1 pageNutritional Assessment and Care PlanMar OrdanzaNo ratings yet
- Procedure - Gastric LavageDocument2 pagesProcedure - Gastric LavageJose Paul RaderNo ratings yet
- Physical Exam LessonDocument10 pagesPhysical Exam Lessonapi-259554593No ratings yet
- Perforated PeritonitisDocument5 pagesPerforated PeritonitisDeepak singh ratheeNo ratings yet
- Assessment and Management of Patients With Hearing and Balance Disorders WebDocument36 pagesAssessment and Management of Patients With Hearing and Balance Disorders Webmalinda0% (1)
- Oxygen Terapi Dan PrinsipelDocument16 pagesOxygen Terapi Dan PrinsipelAmrita KaurNo ratings yet
- ANTENATAL CARE Translate GooglingDocument26 pagesANTENATAL CARE Translate GooglingLutfi ari206100% (2)
- SinusitisDocument37 pagesSinusitismalathiNo ratings yet
- Fundamental of NursingDocument1 pageFundamental of Nursingioana_ciobincanNo ratings yet
- Nursing Care Plan Nephrotic SyndromeDocument2 pagesNursing Care Plan Nephrotic SyndromeJames Pachejo100% (1)
- Stomal Therapy GuideDocument2 pagesStomal Therapy Guideসায়ন্তন দত্ত100% (1)
- Gastroschisis & OmphaloceleDocument1 pageGastroschisis & OmphaloceleMaecy PasionNo ratings yet
- A Case Presentation On Cerebrovascular Accident/Stroke: TH NDDocument30 pagesA Case Presentation On Cerebrovascular Accident/Stroke: TH NDBeckyNo ratings yet
- Drug StudyDocument13 pagesDrug StudyAlisse Sales De-PazNo ratings yet
- Tracheostomy CareDocument1 pageTracheostomy CareShreyas WalvekarNo ratings yet
- Nicu Lesson PlanDocument11 pagesNicu Lesson PlanSAYMABANUNo ratings yet
- Liver Biopsy and AbdominalDocument25 pagesLiver Biopsy and AbdominalAfiq Mubasyyir AmranNo ratings yet
- Health Teaching On Influenza A (H1N1) Swine FluDocument4 pagesHealth Teaching On Influenza A (H1N1) Swine FluPmoigkiNo ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- Nursing Careplan - Rectal CancerDocument5 pagesNursing Careplan - Rectal CancerdrugcardrefNo ratings yet
- Ostomy Nursing Care and ManagementDocument5 pagesOstomy Nursing Care and ManagementLara GatbontonNo ratings yet
- Gerontologic Health Promotion ActivityDocument3 pagesGerontologic Health Promotion ActivityCorinne50% (2)
- Nso ErcpDocument3 pagesNso Ercptry dokkNo ratings yet
- CataractDocument24 pagesCataractNeela Kandan100% (1)
- Procedure-Central Venous Access Catheter InsertionDocument18 pagesProcedure-Central Venous Access Catheter Insertionmohamad dildarNo ratings yet
- Abdominal Paracentesis.Document4 pagesAbdominal Paracentesis.Sukh Preet100% (1)
- Hyperthermia NCPDocument1 pageHyperthermia NCPVenus Glaze VerzolaNo ratings yet
- Activity intolerance, fear, infection risks in thalassemiaDocument1 pageActivity intolerance, fear, infection risks in thalassemiaHannah Clarisse Monge IgniNo ratings yet
- Retinopathy of PrematurityDocument15 pagesRetinopathy of Prematuritymarissa ulkhairNo ratings yet
- Pre Post Operative Care of AppendicectomyDocument20 pagesPre Post Operative Care of AppendicectomyAngel DamoNo ratings yet
- Hyperthermia and Risk For AspirationDocument3 pagesHyperthermia and Risk For AspirationAlmyr RimandoNo ratings yet
- CATHETERIZATIONDocument13 pagesCATHETERIZATIONSarah Uy Caronan100% (1)
- Febrile Seizures NCPDocument9 pagesFebrile Seizures NCPNurul IrhamnaNo ratings yet
- NCP Bed SoresDocument3 pagesNCP Bed SoresShe CalliNo ratings yet
- FractureDocument1 pageFractureReechie TeasoonNo ratings yet
- Tracheostomy CareDocument40 pagesTracheostomy CareSreelekhaNo ratings yet
- Helping a Patient with Nutritional Issues Through Family SupportDocument1 pageHelping a Patient with Nutritional Issues Through Family SupportNeelofur Ibran AliNo ratings yet
- Acute Pain (AGE) NCPDocument1 pageAcute Pain (AGE) NCPMike SoySauce LibrojoNo ratings yet
- Pneumo Hemoperitoneum Stab Wound Case StudyDocument7 pagesPneumo Hemoperitoneum Stab Wound Case StudyMari Jasmeen Estrada Noveda100% (1)
- Nursing Care StudyDocument20 pagesNursing Care StudyAnjaliNo ratings yet
- Nursing Care Plan FeverDocument9 pagesNursing Care Plan Feverbharat singhNo ratings yet
- Colostomy Care Procedure StepsDocument5 pagesColostomy Care Procedure StepsEsmareldah Henry SirueNo ratings yet
- Angiography: Presented By: Mulituba, Nairah DDocument9 pagesAngiography: Presented By: Mulituba, Nairah DAkazukin AineNo ratings yet
- Myelography Procedure and Indications ExplainedDocument12 pagesMyelography Procedure and Indications ExplainedDiana CharaNo ratings yet
- Nursing Care Plan for PneumoniaDocument3 pagesNursing Care Plan for PneumoniaFARAH MAE MEDINANo ratings yet
- Era University / Era College of Nursing: Lesson Plan On-Breast GynecomastiaDocument8 pagesEra University / Era College of Nursing: Lesson Plan On-Breast GynecomastiaShreya SinhaNo ratings yet
- Hazards For IV Therapy-1Document9 pagesHazards For IV Therapy-1Arooj HussainNo ratings yet
- IV Therapy SsDocument56 pagesIV Therapy Sssaeed_chohan100% (8)
- Intravenous Therapy Is Treatment That Infuses Intravenous Solutions, Medications, Blood, or BloodDocument5 pagesIntravenous Therapy Is Treatment That Infuses Intravenous Solutions, Medications, Blood, or BloodShehada Marcos BondadNo ratings yet
- ROT ExamDocument6 pagesROT ExamIan CarodanNo ratings yet
- Part I سنه القمله 2016Document20 pagesPart I سنه القمله 2016Aloah122346No ratings yet
- Covid 19 BookletDocument10 pagesCovid 19 BookletNorhanida HunnybunnyNo ratings yet
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangNo ratings yet
- Leuprolide Vs Triptorelin: The Recent Trends in GNRH Analogues in Precocious PubertyDocument11 pagesLeuprolide Vs Triptorelin: The Recent Trends in GNRH Analogues in Precocious PubertyDianne MarianoNo ratings yet
- Vicorder PWA-PWV Pres 15-04 EnglDocument79 pagesVicorder PWA-PWV Pres 15-04 EnglHatem FaroukNo ratings yet
- Tugas Jurnal PaliatifDocument11 pagesTugas Jurnal PaliatifSiti Wahyuningsih100% (1)
- Engineering Living Therapeutics With Synthetic BiologyDocument20 pagesEngineering Living Therapeutics With Synthetic BiologyGabriel LohnNo ratings yet
- OEC ch25Document10 pagesOEC ch25Phil McLeanNo ratings yet
- EXP 6 - Fecal Coliform Test - StudentDocument8 pagesEXP 6 - Fecal Coliform Test - StudentAbo SmraNo ratings yet
- Coronavirus British English Intermediate b1 b2 GroupDocument4 pagesCoronavirus British English Intermediate b1 b2 GroupAngel AnitaNo ratings yet
- Biology 10Th Edition Raven Test Bank Full Chapter PDFDocument36 pagesBiology 10Th Edition Raven Test Bank Full Chapter PDFlewis.barnes1000100% (12)
- Abdominal ExaminationDocument14 pagesAbdominal ExaminationValeria Guerra CastilloNo ratings yet
- AmavataDocument14 pagesAmavataSamhitha Ayurvedic ChennaiNo ratings yet
- Preparation of Nurses To Disaster ManagementDocument10 pagesPreparation of Nurses To Disaster Managementai nisa hasnasariNo ratings yet
- Nucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresDocument55 pagesNucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresMica BernardoNo ratings yet
- Assessments of Newborn NewDocument15 pagesAssessments of Newborn NewYashoda Satpute100% (1)
- Marking Scheme: Biology Paper 3Document4 pagesMarking Scheme: Biology Paper 3sybejoboNo ratings yet
- Primer: Gastro-Oesophageal Reflux DiseaseDocument23 pagesPrimer: Gastro-Oesophageal Reflux Diseasejcacia17No ratings yet
- E PortfolioDocument3 pagesE Portfolioapi-337945337No ratings yet
- Choosing the Right PaediatricianDocument263 pagesChoosing the Right PaediatricianSuneethaVangala100% (1)
- Everything You Need to Know About Prenatal CareDocument5 pagesEverything You Need to Know About Prenatal Carelaura fernandiaNo ratings yet
- Protozoa Tugas 1Document5 pagesProtozoa Tugas 1De shila syailinda maulidaNo ratings yet
- Answers To Questions:: Analysis of SalivaDocument2 pagesAnswers To Questions:: Analysis of Salivaerisseval14No ratings yet
- CucumberDocument25 pagesCucumberDa Nie LNo ratings yet
- Vocational Rehabilitation Programs for People with DisabilitiesDocument44 pagesVocational Rehabilitation Programs for People with DisabilitiesKannappa Shetty MudiyanuruNo ratings yet
- IV Push MedicationsDocument67 pagesIV Push Medicationsbtalera100% (1)
- Managing obstetric emergenciesDocument9 pagesManaging obstetric emergenciesSnurah Idris100% (1)
- Abortion, Anc, and CS: Focus+ Lecture SeriesDocument24 pagesAbortion, Anc, and CS: Focus+ Lecture SeriesTianah davisNo ratings yet
- Types of Feeding TubesDocument8 pagesTypes of Feeding TubesElda KuizonNo ratings yet
- Double Unders MasteryDocument13 pagesDouble Unders MasterySebastian Hurtado100% (2)