Professional Documents
Culture Documents
BPSD Final For Notes
Uploaded by
WorldEventsForumOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BPSD Final For Notes
Uploaded by
WorldEventsForumCopyright:
Available Formats
4/18/2013
Behavioral Disturbances of DEMENTIA: Interventions to Reduce the Use of Psychotropic Medications
MICHELE THOMAS
Pharmacy Services Manager Virginia Department of Behavioral Health, Developmental Services
ANDREW HECK
Clinical Director Piedmont Geriatric Hospital, Virginia Department of Behavioral Health, Developmental Services
(c) 2013 by the authors, on behalf of the Virginia Geriatric Mental Health Partnership & made possible through a grant from the Virginia Center on Aging's Geriatric Training Education Initiative and supported by the Riverside Center for Excellence in Aging and Lifelong Health, the Virginia Geriatric Mental Health Partnership, and the VCU's Department of Gerontology.
4/18/2013
ABBREVIATION
DETAIL
ADE Adverse Drug Effects ADL Activities of Daily Living ALF Assisted Living Facility BPSD Behavioral and Psychological Symptoms of Dementia CMS Centers for Medicare & Medicaid Services GDR Gradual Dose Reduction LTC Long Term Care LTCF Long Term Care Facility Sx Symptoms
ABBREVIATIONS
4/18/2013
By the end of the presentation, participants will:
Be able to more clearly describe Behavioral and Psychological Symptoms of Dementia, (problematic behaviors, [BPSD or BPSD Sxs]) and possible triggers;
Learn about appropriate use of antipsychotic medications in individuals diagnosed with problematic behaviors in dementia Become familiar with nonpharmacological strategies for preventing and/or reducing problematic behaviors;
Objectives
4/18/2013
Ms. Take (MT)
The patient is an 84 year old white female newly admitted to a LTC setting exhibiting the following signs and symptoms: two to three year history of increasing forgetfulness Increased wandering and elopement attempts distractibility repetitive requests calling out for her husband intrusiveness resistance to personal care language deficits.
Patient Intake & History
Over the next few weeks at the LTCF, MT declined. She: no longer recognized her husband exhibited repetitive behaviors verbalized suspicious statements about husbands whereabouts exhibited increased restlessness, and began experiencing persistent nighttime wakefulness.
Case of Ms. Take (MT)
4/18/2013
Common BPSD/Behaviors in Dementia
Aggression/Agitation Apathy Delusions Anxiety Psychomotor Disturbance
Up to 80%
72%
9-63%
48%
46%
Hallucinations
Physical Aggresion
Irritability/Lability
Sleep/Wake Distburbance
Depression/Dysphoria
4-41%
31-42%
42%
42%
38%
Disinhibition
Sundowning
Hypersexuality
Obsessive/Compulsive
36%
18%
3%
2%
Jeste D, et al. Neuropsychopharmacology. 2008;33:957 Spalletta G, et al. Am J Geriatr Psychiatry. 2010;18:1026
4/18/2013
Early(~0-3yrs) Mild-Mod(~3-5yrs) Severe(~6yrs)
Mood
100 80
Cognition
Behavior / Function Agitation
% patients
60 40 20
Depression Social withdrawal
Diurnal rhythm Irritability Wandering Aggression
Anxiety Mood change Paranoia Accusatory behavior
-20 10 0
Suicidal ideation
-40 -30
Hallucinations Socially unacceptable behavior Delusions Sexually inappropriate behavior
10 20 30
months before dementia diagnosis / months after dementia diagnosis
Estimated Timeline of BPSD in Dementia
Jost BC, Grossberg GT. J Am Geriatr Soc. 1996;44:1078-1081 Brodaty et al. 2003. J. Clin Psychiatry 64:36. http://www.ucc.ie/en/
4/18/2013
POLL Appropriate Antipsychotic Treatment targets include the following: (Check all that apply)
A. B. C. D. Distressing hallucinations Physically aggressive behavior Delusional jealousy Anger over accepting assistance with ADLs
POLL: CMS Approved Indications for LTC Facilities
4/18/2013
BPSD Clusters & Antipsychotic Medications
PSYCHOMOTOR AGITATION *AGGRESSION
Physically aggressive Verbally aggressive Aggressive resistance to care Pacing Restlessness Repetitive actions Dressing/undressing Sleep disturbance
MANIA
Euphoria Pressured Speech Irritable
*PSYCHOSIS APATHY
Withdrawn Lacks interest Amotivation Hallucinations Delusions Misidentifications Suspiciousness
DEPRESSION
Sad Tearful Hopeless Low self esteem Anxiety Guilt
Bugden. Antipsychotics and Dementia: Part of the Solution or Part of the Problem, Dementia Care Conf. 2012
4/18/2013
Apathy Calling out e.g., screaming
Most common BPSD NOT amenable to medication/ antipsychotic medication
Hiding/hoarding Nocturnal restlessness Repetitive activities e.g., pulling on locked doors, etc. Wandering Unsociability Poor self care Uncooperativeness without aggressive behavior Verbal expressions or behaviors that do not represent a danger Nervousness / fidgeting / Mild anxiety Impaired memory
Bugden. Antipsychotics and Dementia: Part of the Solution or Part of the Problem, Dementia Care Conf. 2012
4/18/2013
No FDA-approved medications to treat dementia-related behavioral disturbances Medications utilized today, prescribed off-label:
Typical & atypical antipsychotics Benzodiazepines Anticonvulsants Cholinesterase inhibitors NMDA receptor antagonist Selective serotonin reuptake inhibitors (SSRIs)
BPSD and Psychotropics
Lawrence RM et al, Psychiatric Bulletin. 2002;26:230
10
4/18/2013
2005: FDA issued warning: 1.6 1.7 fold increase in mortality in response to analysis of 17 placebo-controlled studies. 2010: Nearly 1/3 of elderly patients with dementia residing in nursing homes are on atypical antipsychotics for BPSD even though..
Most episodes of BPSD appear as single episode (~86%) and the average duration of each episode lasts between ~9 to 19 months
BLACK BOX WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS and SUICIDALITY *Antipsychotic drugs have increased risk of death*
Jablow V. Trial. 2008;44:12 Recupero PR et al. J Psychiatric Pract. 2007;13:143
11
4/18/2013
HHS Initiative: National Partnership to Improve Dementia Care CMSs initial goal to reduce unnecessary antipsychotic medication use in all care settings.
Goal:
Using personcentered and individualized interventions for behavioral health in nursing homes
By improving dementia care
Unnecessary medication use will decrease.
Antipsychotics are the initial focus of the partnership, however attention to other potentially harmful medications is also part of this initiative.
483.25(l) Unnecessary Drugs Each residents drug regimen must be free from unnecessary drugs (F329)
12
4/18/2013
National prevalence rate of antipsychotic medication use in long-stay residents
Initiative: Reduce the national rate by 15%
This number includes all residents in NHs EXCEPT persons diagnosed with Schizophrenia, Tourettes Syndrome or Huntingtons disease .
23.9%
2012 GOAL . 2013 GOALs? Reevaluate based on 2012 4th quarter findings
First Year Goals
13
4/18/2013
Effective interventions follow thorough assessments aimed at the problems specific cause Management of BPSD must be comprehensive and systematic Successful BPSD management blends reactive and proactive strategies
Treatment of BPSD should begin with nonpharmacological approaches keeping in mind five care goals for the patient with dementia:
to experience pleasure to feel safe
to experience minimal stress with adequate positive stimulation to experience a sense of control
to feel comfortable
BPSD: Need for Alternative Approaches in Treatment
Buhr GT, White HK. Difficult behaviors in long-term care patients with dementia. J Am Med Dir Assoc. 2006;7(3):181. Ryden MB, Feldt KS. Goal-directed care: caring for aggressive nursing home residents with dementia. J Gerontol Nurs. 1992;18(11):35-42.
14
4/18/2013
Why is this behavior a problem?
Is it: only problematic for the resident? endangering/irritating/ upsetting to other residents/family members/visitors/staff? interfering with care?
Focus resources towards behaviors that are dangerous or cause marked distress to the resident or others
First Question in Identifying & Describing BPSD Behaviors
15
4/18/2013
PRIORITY RISK AREAS
OAMING? MMINENT PHYSICAL RISK (fire, falls, frailty?) UICIDE? INSHIP RELATIONSHIP ABUSE/NEGLECT? ELF NEGLECT, SUBSTANCE ABUSE, SAFE DRIVING? Risk Assessment: Taking Inventory
16
4/18/2013
Static
Presence of delusions Impaired communication Frontotemporal dementia Certain forms of traumatic brain damage
Depression Low serotonin levels Psychosis; esp. Irritability
command hallucinations and thought disorganization
Dynamic
BPSD Example: Aggression Risk Factors
Heck, A. Aggressive behavior in the elderly: prevention and management. Cross Country Education Seminar, 2006.
17
4/18/2013
Will want to know the following about the BPSD:
Type Frequency Intensity Duration
Functional analysis of behavior:
an examination of what a behaviors purpose (i.e., function) serves for the individual
Answers the what, where, when and how questions Basic functional analyses can be performed by anyone clinically familiar with the resident
Clarifying the BPSD
18
4/18/2013
Behavior Description
what specific behavior(s) occurred?
Behavior Prediction
did the behavior(s) primarily occur during specific time periods?
Behavior Functions
What functions did the behavior(s) appear to serve for the person?
if >1 behavior, did any ever occur together?
were there periods when the behavior(s) consistently did not occur?
What were the consequences that were typically provided when the behavior(s) occurred?
when behavior(s) were occurring, were there setting events or stimuli which were consistently related to their occurrence?
With answers to these questions, along with any baseline data gathered, clinicians may begin to draw conclusions about the cause(s) and treatment of the problematic behavior
Clarifying the BPSD (cont.)
19
4/18/2013
ealth and medical conditions nvironment pproach esident factors
An ordered strategy for examining common sources of a behavior problem
The HEAR method
20
4/18/2013
B12/Folic Acid Deficiency Infection (UTI/Pneumonia)
Most common and potentially dangerous causes of BPSD Sxs
Hunger/Thirst
MEDICAL
Nocturia Hypercalcemia Pain Hypothyroidism Constipation
Digoxin
MEDICATIONS/DRUG INDUCED DELIRIUM
Anticholinergic agents
Benzodiazepines Opioids
Antihistamines
Health and Medical Conditions: BPSD Common Causes and Trigger Factors
Bugden. Antipsychotics and Dementia: Part of the Solution or Part of the Problem, Dementia Care Conf. 2012
21
4/18/2013
POLL Delirium is a state of acute cognitive impairment caused by a medical problem. Three primary cardinal features of delirium are:
A. Acute/onset is days to weeks B. Transient in severity often fluctuating throughout the day for short periods of time C. Reversible state of confusion D. Most often irreversible state of confusion
POLL: Delirium
22
4/18/2013
The likelihood of developing delirium increases with age Three primary features to look for:
1. 2. 3. ACUTE TRANSIENT (lasts only for a short time) and REVERSIBLE state of confusion.
Delirium diagnosis is often missed in up to 70% of cases
This is especially concerning, since up to 60 % of elderly individuals experience a delirium prior to or during a hospitalization
Delirium is Always an Acute Medical Emergency
Delirium
http://www.nlm.nih.gov/medlineplus/ency/article/000740.htm
23
4/18/2013
DRUGS, DRUGS, DRUGS! EYES, EARS POOR HEARING AND VISION = RISK FACTORS L OW O STATES (MI, CHF, COPD, acute respiratory distress syndrome) I NFECTION, IMMOBILZATION RETENTION (URINE/STOOL), RESTRAINTS ICTALSEIZURES CAN CAUSE DELIRIUM UNDERHYDRATION, UNDERNUTRITION METABOLIC ABNORMALITIES (s)UBDURAL, SLEEP DEPRIVATION
2
Common Causes of Delirium
24
4/18/2013
MT
84 year old white female newly admitted to LTC setting exhibiting signs & symptoms of: wandering elopement attempts distractibility at mealtime repetitive requests for husband intrusiveness resistance to personal care, and language deficits.
MTs Husband Staff talked with MTs husband. He noted she appeared more worried, apprehensive, fearful and she no longer recognized him during their daily visits
MTs current medications Docusate 100mg bid constipation. Oxybutynin 10mg XL daily incontinence.
Adherence Prior to admission, Mr. Take reported that his wifes dose of oxybutynin had been increased from 5mg to 10mg but, he also stated that his wife rarely took her medications, let alone on a regular basis...
Case Update: Ms. Take
25
4/18/2013
MT became more and more challenging exhibiting increasing exit seeking behaviors; daytime restlessness and pacing increased to where it became extremely difficult for staff to redirect her
Ms. Take
She had periods of feeling exhausted, appearing overly sedated or subdued; this resulted in frequent daytime napping. MT also began exhibiting increased distractibility and began refusing to eat. As a result, MT had an eight pound weight loss.
MT: 30 Day Update
26
4/18/2013
Orthopedic issues / arthritis: feet (e.g., poorly fitting shoes), shoulder, back, knee, etc
Is there Dehydration/ Nutritional issues?
Constipation, urinary retention / incontinence?
Musculoskeletal: Joint pain?
Is there Pain?
Eyes: Corneal abrasion?
HPE, Vital Signs, Labs as warranted
Is there Infection/ Illness?
Sensory deficits?
Skin: Bed sores/ skin lesions?
Is the resident experiencing ADEs?
Evaluation: Are there any Physical Causes or Medication Adverse Effects (ADE)?
27
4/18/2013
**DELIRIUM**
PE Labs: CBC, electrolytes & U/A Delirium Assessment performed: MT was Positive Acute onset Sxs, fluctuating in course, and
VS: +orthostatic hypotension; +restlessness, +poor attention
U/A >> BUN relative to SCr >> Sp. Gravity>> 3+ leuks & WBCs in urine
a change in cognition,
(increasing difficulty in focusing attention).
Findings: ANTICHOLINERGIC TOXICITY
"Compliance Toxicitydue to increase in oxybutynin dose with resultant anticholinergic load/toxicity
oxybutynin dose > oral intake > urinary retention >> bladder infection.
MT: Evaluation/Findings
28
4/18/2013
Definition:
ANY ASPECTS OF AN INDIVIDUALS SURROUNDINGS THAT INFLUENCE BPSD
Both cognitively impaired and cognitively intact individuals can be very sensitive to even minor environmental irritants or changes Irritant/change + behavioral dyscontrol = potentially harmful reaction! Environmental changes are recommended in most circumstances
No adverse effects Easy to implement
HEAR: Environmental Factors
29
4/18/2013
Common examples:
Physical elements
Highly patterned wallpaper Mirrors
Noise and activity level
Loud call bells/paging systems Constant Television Programs (e.g., Soap Operas, CNN)
Space issues
Frequent room changes/redesign Relocation (within or between facilities) Lack of adequate physical space
Environmental Factors cont.
30
4/18/2013
Liberally attempt different environmental changes (being sensitive to the amount of change the residents can tolerate)
Try using soothing sounds (ocean waves, babbling brooks, even white noise)
Scheduled walking or exercise programs have demonstrated effectiveness in preventing and addressing BPSD
Exposure to bright light can also be effective (avoid in patients with a history of Bipolar Disorder)
Environmental Factors cont.
31
4/18/2013
Providing space to freely wander
Brief gentle hand massages
Empirically supported interventions to prevent/ manage agitation
Individualized music
Use of gliding rockers
Aromatherapy
Environmental Factors cont.
Landreville P et al. Intl Psychogeriatrics 2006;18 Rayner A et al. Am Fam Physician 2006; 73 Camp C et al. In Lichtenberg D et al., Handbook of dementia 2003; NY: Wiley & Sons
32
4/18/2013
69 year old male with Alzheimers disease Has refused to leave room in past month; swings out at staff who try to get him to come out for meals, activities Often observed to walk up to doorway, look at floor beyond threshold, and retreat into room Staff discovered janitorial staff had recently changed to a shinier wax for the hallway floors (looks slick?) Mr. Faller Timing of change coincided with the emergence of Mr. Fallers behaviors Less shiny wax used, Mr. Faller was able to leave the room with minimal difficulty soon afterward
Case Example: Mr. Faller
33
4/18/2013
Definition:
THE METHOD(S) BY WHICH INDIVIDUALS ARE ADDRESSED BY THEIR CAREGIVERS THAT CAN INFLUENCE BPSD
Can include physical, verbal, nonverbal, schedule/routine issues, etc.
Common examples
Violations of personal space
Caregiver attitude/reactions
Stance and positioning issues
Verbal approaches
Physical touch (esp. during ADLs)
Erratic or unpredictable daily structure
HEAR: Approach Factors
34
4/18/2013
Emphasize lack of intentionality of resident behaviors Educate about signs and symptoms of dementia
Staff training
Teach communication skills (below) Train on proper physical approach to physical contact-based tasks (e.g., ADLs) Use short phrases that express one major idea at a time Use closed-ended rather than open-ended questions
PREVENTION/ MANAGEMENT STRATEGIES:
Communication
Focus on the emotion rather than the content of what is being said (validation) Give directions one step at a time Use distraction rather than logic/reason to calm resident behavior (most often in later dementia stages) Keep predictable schedule (esp. mealtimes and sleep) Use familiar staff whenever possible
Structure
Approach Factors cont.
35
4/18/2013
Resident with 6-year diagnosis of Alzheimers disease Memory unit in ALF: For the past three weeks, every morning Ms. Hurley has been observed to throw her toast from her tray across the room Resident had not previously expressed a dislike for toast, and family said she used to like it
Ms. Hurley
After starting to observe Ms. Hurley from beginning of meal forward, staff noticed that she struggled to apply the sealed butter and jelly packets (sequencing problems) Staff started serving the toast with butter and jelly already spread on it, behavior ceased directly. Example of catastrophic reaction
Case Example: Ms. Hurley
36
4/18/2013
Definition:
THE NEEDS, WANTS, DESIRES, OR HABITS OF AN INDIVIDUAL THAT INFLUENCE BEHAVIORAL PROBLEMS
Can also be considered psychological factors These constitute a broad array of potential contributing causes for BPSD
Learned patterns of behavior and/or thinking History of trauma Mood states Emotional discomfort Lack of socialization Boredom Lack of autonomy/privacy/intimacy Distress/feeling abandoned Fear of danger Misinterpretation paranoia
HEAR: Resident Factors
37
4/18/2013
PSYCHOTHERAPY (for some residents)
Individuals with early-state dementia may benefit from some forms of psychotherapy Gather collateral informationfamily and others
Has your loved one ever shown behavior like this before? Is there anything about these circumstances that may be bringing up bad memories for your loved one?
Pass along information and observations to therapist
HEAR: Resident Factors (cont.)
38
4/18/2013
BEHAVIOR PLANNING
Some residents may benefit from more involved contingency management plans (AKA behavior plans) Works across different levels of cognitive ability Typically developed by a MH consultant, implemented by facility staff (with staff training) Aimed at bringing about desirable behaviors while discouraging or eliminating harmful behaviors
HEAR: Resident Factors (cont.)
39
4/18/2013
81 year old woman in psychiatric hospital Cursing and swinging arms Personality disorder and early dementia Plan: could earn treats (coffee, strolls, etc.) every 2 hours if no cursing or striking out Needed frequent reminders of treat opportunities Problematic behavior dropped 66% in 2 months After thinning reinforcement schedule, behavior stopped completely
Mrs. Sweet
Case Example: Mrs. Sweet
40
4/18/2013
Identification and attribution of behaviors
Prevalence of BPSD has been found to vary across cultures
Is behavior culturally normative? (e.g., loudly and constantly praying, high hostility in interpersonal interactions) Is environment or approach having a disproportionate impact due to cultural factors? (e.g., physical touch during ADL care)
Diagnosis
Were instruments geared toward individuals [national or ethnic] culture? (e.g., normative data, language) Was level of education accounted for?
BPSD: Cultural Considerations for Clinicians
Shah et al Int Psychogeriatr 2004; 16 Herbert P Can J Neurol Sci 2001; 28 Suppl 1
41
4/18/2013
Communication difficulties
Taboo topics
Cultural factors that may complicate the diagnosis of dementia
Stigma attached to mental illness Bias and prejudice of clinicians
Institutional racism Unfamiliarity with sxs of dementia by relatives Sxs of dementia being viewed as a function of old age
CULTURAL CONSIDERATIONS: Diagnosis
Shah, AS. CROSS-CULTURAL ISSUES AND COGNITIVE IMPAIRMENT http://www.rcpsych.ac.uk/pdf/Dementia%20%20Culture.pdf
42
4/18/2013
When is an antipsychotic justified?
Schizophrenia Schizoaffective disorder Delusional disorder Mood disorders (e.g. mania, bipolar disorder, depression with psychotic features, and treatment refractory major depression)
Antipsychotic medication can be used for the following conditions/diagnoses:
Schizophreniform disorder Psychosis NOS Atypical psychosis Brief psychotic disorder Dementing illnesses with associated behavioral symptoms Medical illnesses or delirium with manic or psychotic
Antipsychotic treatment goal[s]: to stabilize and or improve a residents outcome, quality of life and functional capacity
43
4/18/2013
JUSTIFY
H
After
E
After
BPSD Sxs must present a DANGER to the person or others or, cause the patient to experience one of the following:
HEALTH
and medical causes have been ruled out
A
After
ENVIRONMENTAL
R
After
treatment strategies have been tried/ implemented
APPROACH FACTORS
- inconsolable or persistent distress; - a significant decline in function; - substantial difficulty receiving needed care
have been evaluated, (training, communication & structure)
RESIDENT FACTORS
have been evaluated
SELECT
1. Individualize 2. Initiate monotherapy Start low, go slow 3. Titrate dose to effect, Rule of Thumb: 5-10% dose increases q 4-6 wks 4. If effective, continue few weeks few months 5. STOP drug if INEFFECTIVE (appropriately tapering)
Antipsychotic justification in BPSD
Maixner, et al. J Clin Psychiatry. 1999;60(suppl 8):29. Jibson and Tandon. J Psychiatry Res. 1998;32:215.
44
4/18/2013
GDR attempts can be omitted if they are clinically contraindicated.
For behavioral symptoms related to dementia, clinically contraindicated is defined when:
Residents target symptom[s] return or worsen after most recent GDR attempt
AND Physician has documented rationale for why additional GDR attempts would likely impair the residents function
Gradual Dose Reduction : Antipsychotics
Hardesty, JL. Presentation to VHCA, Under the Microscope: The Ever-Increasing Scrutiny of Antipsychotics in LTC, 2012
45
4/18/2013
In clinical record:
Clear documentation of treatment targets / symptoms
Non-pharmacological interventions tried and/or in use
Pharmacological intervention is prescribed:
Lowest effective dose is utilized Time limited duration, (as warranted)
Ongoing monitoring / reporting of efficacy and response
ADEs clearly being monitored for and supported in documentation Tolerability & efficacy assessed every 3 to 7 days
GDR attempts are documented
Reassess for tapering / discontinuation per CMS guidelines
If the drug doesnt help, stop it!
46
4/18/2013
Explore, identify and address the following potential contributors: Conduct risk analysis
Health/medical factors Environmental factors Approach factors Resident factors
Clearly document every step of the way
Immediately address imminent safety issues
Prescribe medications judiciously
Start low and go slow!
Conclusions: Managing BPSD
47
4/18/2013
Michele Thomas, R.Ph., Pharm.D., BCPP michele.thomas@dbhds.virginia.gov Andrew Heck, Psy.D., ABPP andrew.heck@dbhds.virginia.gov
Contact
48
You might also like
- Behavioral Disturbances of DEMENTIADocument48 pagesBehavioral Disturbances of DEMENTIAWorldEventsForumNo ratings yet
- 14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Document9 pages14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Danielcc Lee100% (1)
- Hospice CareDocument2 pagesHospice CareSamuel YoungNo ratings yet
- Lecture #7, Points On The Continuum - Ambulatory Care, Home Care, Hospice and Palliative CareDocument17 pagesLecture #7, Points On The Continuum - Ambulatory Care, Home Care, Hospice and Palliative CareKathleen LaNo ratings yet
- Antipsychotics HandoutDocument25 pagesAntipsychotics HandoutTeddy Kurniady ThaherNo ratings yet
- Rns Can Work in A Variety of Healthcare Settings, IncludingDocument6 pagesRns Can Work in A Variety of Healthcare Settings, IncludingpriyagerardNo ratings yet
- Unit 2-Community Health Nursing Roles (Autosaved)Document57 pagesUnit 2-Community Health Nursing Roles (Autosaved)Krista KloseNo ratings yet
- Op-Ed Part 2Document1 pageOp-Ed Part 2api-530416054No ratings yet
- Screening Test Sensitivity vs SpecificityDocument7 pagesScreening Test Sensitivity vs SpecificityKinuPatel100% (2)
- Nurs403 Practice Summary Paper NeuburgDocument14 pagesNurs403 Practice Summary Paper Neuburgapi-452041818No ratings yet
- Nursing Dissertation, Nursing Essay, Nursing Project, Nursing Assignment, Nursing Homework, Nursing Writing, Nursing Outline, Nursing Abstract, Nursing DissertationDocument10 pagesNursing Dissertation, Nursing Essay, Nursing Project, Nursing Assignment, Nursing Homework, Nursing Writing, Nursing Outline, Nursing Abstract, Nursing DissertationiWanttutor.com100% (1)
- Nursing PhilosophyDocument1 pageNursing PhilosophyNene DikeNo ratings yet
- Nurse Compentency ChecklistDocument17 pagesNurse Compentency ChecklistMary ElizabethNo ratings yet
- Professional Development PlanDocument9 pagesProfessional Development Planapi-533828062No ratings yet
- Nursing Diagnosis List for Basic Human NeedsDocument28 pagesNursing Diagnosis List for Basic Human NeedsAmit MartinNo ratings yet
- Medication Reconcillation in Home Care Getting Started KitDocument74 pagesMedication Reconcillation in Home Care Getting Started Kitjopet8180No ratings yet
- Home Health NursingDocument16 pagesHome Health NursingSathish Rajamani100% (1)
- Nursing PhilosDocument8 pagesNursing Philosapi-527531404No ratings yet
- Depressive DisordersDocument9 pagesDepressive Disorderslengkong100% (1)
- Palliative CareDocument23 pagesPalliative CareCharles Frank100% (1)
- Utilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffDocument6 pagesUtilizing Bedside Shift Report To Improve The Effectiveness of Shift HandoffselviNo ratings yet
- Utilization Review RNDocument2 pagesUtilization Review RNapi-121451258No ratings yet
- Home Health Nursing Care: Everything You Need to KnowDocument78 pagesHome Health Nursing Care: Everything You Need to KnowJake Arizapa100% (1)
- Medication Administration Error 3Document16 pagesMedication Administration Error 3Priya bhattiNo ratings yet
- Palliative Care - End of Life Care - Northern HealthDocument8 pagesPalliative Care - End of Life Care - Northern HealthDiklatpimempat AngkatanlimabelasNo ratings yet
- Clinical ExemplarDocument4 pagesClinical Exemplarapi-272451466No ratings yet
- Self-Assessment of Nursing Standards of PracticeDocument14 pagesSelf-Assessment of Nursing Standards of Practiceapi-236260255100% (1)
- Professional Development PowerpointDocument12 pagesProfessional Development Powerpointapi-400385739No ratings yet
- The Nursing Process - PowerpointDocument39 pagesThe Nursing Process - PowerpointAslam BalteeNo ratings yet
- End of Life Care Checklist PDFDocument16 pagesEnd of Life Care Checklist PDFBenny TrisaktyariNo ratings yet
- Bsn-Rs-Careplan 2Document9 pagesBsn-Rs-Careplan 2api-520841770No ratings yet
- Problems Related To Abuse Neglect and Violence Among Vulnerable GroupsDocument53 pagesProblems Related To Abuse Neglect and Violence Among Vulnerable GroupsSumam NeveenNo ratings yet
- Career Clarity for Nurses: Navigating Nursing Through Challenging TimesFrom EverandCareer Clarity for Nurses: Navigating Nursing Through Challenging TimesRating: 1 out of 5 stars1/5 (1)
- Benzo PowerpointDocument21 pagesBenzo Powerpointapi-300457344No ratings yet
- Understanding Key Concepts of Health Education and PromotionDocument59 pagesUnderstanding Key Concepts of Health Education and PromotionAshri Nur IstiqomahNo ratings yet
- Check List For PT ETOH Alcohol UseDocument12 pagesCheck List For PT ETOH Alcohol Usesen ANo ratings yet
- Do You Agree or Disagree With McCarthyDocument3 pagesDo You Agree or Disagree With McCarthyBinu Kumar100% (3)
- The Constraints in Providing Primary Care To Elder Patients With Chronic Disease Causes A More Challenging Physical and Social EnvironmentDocument10 pagesThe Constraints in Providing Primary Care To Elder Patients With Chronic Disease Causes A More Challenging Physical and Social EnvironmentTony MuselaNo ratings yet
- Nursing Credentials and CertificationsDocument8 pagesNursing Credentials and CertificationsmhaymunezNo ratings yet
- Talking Therapy: Knowledge and Power in American Psychiatric NursingFrom EverandTalking Therapy: Knowledge and Power in American Psychiatric NursingNo ratings yet
- FinalintegrativereviewDocument17 pagesFinalintegrativereviewapi-346349076No ratings yet
- Ethical Dilemmas in Nursing PDFDocument5 pagesEthical Dilemmas in Nursing PDFtitiNo ratings yet
- Scope of Nursing Practice DefinitionDocument26 pagesScope of Nursing Practice DefinitionJurinia VicenteNo ratings yet
- Nurses' Guide to Critically Reading ResearchDocument8 pagesNurses' Guide to Critically Reading ResearchAndrew BarbourNo ratings yet
- Vascular Disorder Case StudyDocument3 pagesVascular Disorder Case StudyAaron Wallace100% (1)
- Observation Summary 2Document5 pagesObservation Summary 2api-493028287No ratings yet
- Nurse's Role as Part of an Interprofessional Healthcare TeamDocument11 pagesNurse's Role as Part of an Interprofessional Healthcare TeamOmi EdNo ratings yet
- Teaching Plan For DiabetesDocument4 pagesTeaching Plan For DiabetesanrefNo ratings yet
- Program Graduate Competency ReflectionDocument11 pagesProgram Graduate Competency Reflectionapi-458433381No ratings yet
- Case 1Document28 pagesCase 1John Joshua Lacson Medicine100% (1)
- Psychiatric MedicinesDocument12 pagesPsychiatric MedicinesMr. Psycho Sam0% (1)
- Managing Alcohol WithdrawalDocument36 pagesManaging Alcohol WithdrawalnadyaNo ratings yet
- Pilot Project ReportDocument26 pagesPilot Project ReportInclusionNorthNo ratings yet
- Nrs 110 Lecture 1 Care Plan WorkshopDocument45 pagesNrs 110 Lecture 1 Care Plan Workshopalphabennydelta4468100% (2)
- 696 Clinical Learning Agreement - Plan EvaluationDocument16 pages696 Clinical Learning Agreement - Plan Evaluationapi-456551916No ratings yet
- Chapter 24 Management of Patients With Chronic Pulmonary DisordersDocument3 pagesChapter 24 Management of Patients With Chronic Pulmonary DisordersPeej Reyes100% (1)
- Documentation and Nurse Practitioner RoleDocument5 pagesDocumentation and Nurse Practitioner RoleEnerolisa ParedesNo ratings yet
- HOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREDocument7 pagesHOSPICE CARE: A TEAM APPROACH TO COMPASSIONATE END-OF-LIFE CAREJason SteelNo ratings yet
- Virginia Dementia State Plan DRAFTDocument36 pagesVirginia Dementia State Plan DRAFTWorldEventsForumNo ratings yet
- HAI2015 BookDocument155 pagesHAI2015 BookWorldEventsForumNo ratings yet
- Human Amyloid Imaging 2015 Book DraftDocument151 pagesHuman Amyloid Imaging 2015 Book DraftWorldEventsForumNo ratings yet
- MCI 2014 Public Forum DevousDocument24 pagesMCI 2014 Public Forum DevousWorldEventsForumNo ratings yet
- Rentz MCI Public Forum TalkDocument27 pagesRentz MCI Public Forum TalkWorldEventsForumNo ratings yet
- Human Amyloid Imaging 2015 Book DraftDocument151 pagesHuman Amyloid Imaging 2015 Book DraftWorldEventsForumNo ratings yet
- Clinical Implications of Concordant and Discordant Beta-Amyloid and Neurodegenerative Abnormalities in Mild Cognitive ImpairmentDocument26 pagesClinical Implications of Concordant and Discordant Beta-Amyloid and Neurodegenerative Abnormalities in Mild Cognitive ImpairmentWorldEventsForumNo ratings yet
- MCI Petersen Miami FinalDocument60 pagesMCI Petersen Miami FinalWorldEventsForumNo ratings yet
- Wolk ForumDocument25 pagesWolk ForumWorldEventsForumNo ratings yet
- Mormino MCI Symposium Web FinalDocument31 pagesMormino MCI Symposium Web FinalWorldEventsForumNo ratings yet
- MCI Talk-Park Web FinalDocument38 pagesMCI Talk-Park Web FinalWorldEventsForumNo ratings yet
- Landau MCI 2014 - Final SlidesDocument22 pagesLandau MCI 2014 - Final SlidesWorldEventsForumNo ratings yet
- Wolk SymposiumDocument27 pagesWolk SymposiumWorldEventsForumNo ratings yet
- Fleisher MCI Amyloid 2014 - LatestDocument26 pagesFleisher MCI Amyloid 2014 - LatestWorldEventsForumNo ratings yet
- Rentz - MCI 2014 Symposium SlidesDocument29 pagesRentz - MCI 2014 Symposium SlidesWorldEventsForumNo ratings yet
- LoewensteinMCI Jan16,2014Document30 pagesLoewensteinMCI Jan16,2014WorldEventsForumNo ratings yet
- Jack Mci LatestDocument44 pagesJack Mci LatestWorldEventsForumNo ratings yet
- Case 1: - 62yo Right Handed Man, Manager For An Engineering FirmDocument24 pagesCase 1: - 62yo Right Handed Man, Manager For An Engineering FirmWorldEventsForumNo ratings yet
- Fleisher MCI Amyloid 2014 - LatestDocument26 pagesFleisher MCI Amyloid 2014 - LatestWorldEventsForumNo ratings yet
- Wolk WorkshopDocument43 pagesWolk WorkshopWorldEventsForumNo ratings yet
- Wolk ForumDocument25 pagesWolk ForumWorldEventsForumNo ratings yet
- Dodge Symposium MCI 2014 V7 LatestDocument34 pagesDodge Symposium MCI 2014 V7 LatestWorldEventsForumNo ratings yet
- Salloway MCI Miami Keynote 1-14rev - LatestDocument25 pagesSalloway MCI Miami Keynote 1-14rev - LatestWorldEventsForumNo ratings yet
- Snitz Symposium LatestDocument40 pagesSnitz Symposium LatestWorldEventsForumNo ratings yet
- MCI Educational Forum 1-14revDocument19 pagesMCI Educational Forum 1-14revWorldEventsForumNo ratings yet
- Wolk SymposiumDocument27 pagesWolk SymposiumWorldEventsForumNo ratings yet
- Landau MCI 2014 - Final SlidesDocument22 pagesLandau MCI 2014 - Final SlidesWorldEventsForumNo ratings yet
- Wolk WorkshopDocument43 pagesWolk WorkshopWorldEventsForumNo ratings yet
- MIAMI MCI MTG Schmittetal FinalDocument17 pagesMIAMI MCI MTG Schmittetal FinalWorldEventsForumNo ratings yet
- Wolk ForumDocument25 pagesWolk ForumWorldEventsForumNo ratings yet
- Alfred AdlerDocument20 pagesAlfred AdlerChristian Arby BantanNo ratings yet
- Developmental Dysplasia of The HipDocument16 pagesDevelopmental Dysplasia of The Hipjonathan_alvaNo ratings yet
- Cfda-Nrega Monitoring and Evaluation ReportDocument87 pagesCfda-Nrega Monitoring and Evaluation ReportAnand SugandheNo ratings yet
- Virgin Media CaseDocument18 pagesVirgin Media CaseRiaz AttrashNo ratings yet
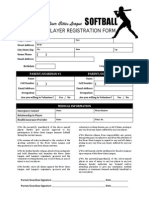
- RCL Softball Registration FormDocument1 pageRCL Softball Registration FormRyan Avery LotherNo ratings yet
- Acne TreatmentDocument2 pagesAcne TreatmentBps Azizah CangkringanNo ratings yet
- Principles of Tooth PreparationsDocument14 pagesPrinciples of Tooth PreparationsMarrion Jules Sequitin MendozaNo ratings yet
- ReferDocument189 pagesReferrameshNo ratings yet
- FC Script-1lv8zpiDocument149 pagesFC Script-1lv8zpiPaulo CamiloNo ratings yet
- Employers Cited For MIOSHA Violations at Holland Warehouse Totaling $357,000 in Proposed PenaltiesDocument3 pagesEmployers Cited For MIOSHA Violations at Holland Warehouse Totaling $357,000 in Proposed PenaltiesMichigan NewsNo ratings yet
- Hamilton County Infant Mortality RatesDocument3 pagesHamilton County Infant Mortality RatesWCPO 9 NewsNo ratings yet
- School Form 1 (SF 1)Document6 pagesSchool Form 1 (SF 1)ᜇᜓᜇᜓᜅ᜔ ᜄᜌᜓᜐNo ratings yet
- PHARMACEUTICAL INORGANIC CHEMISTRY: Radiopharmaceuticals: December 2017Document7 pagesPHARMACEUTICAL INORGANIC CHEMISTRY: Radiopharmaceuticals: December 2017pankaj dagurNo ratings yet
- LiposarcomaDocument9 pagesLiposarcomaKenneth ColeNo ratings yet
- Social WorkDocument13 pagesSocial WorkAyas uddinNo ratings yet
- Performing a Surgical ScrubDocument15 pagesPerforming a Surgical ScrubSavita HanamsagarNo ratings yet
- Clinical Pediatrics - Lectures or TutorialDocument210 pagesClinical Pediatrics - Lectures or TutorialVirender VermaNo ratings yet
- Fournier Gangrene-A Flesh Eating DiseaseDocument35 pagesFournier Gangrene-A Flesh Eating DiseaseDr Diana EnachescuNo ratings yet
- PredicineCARE WhitepaperDocument6 pagesPredicineCARE WhitepapersagarkarvandeNo ratings yet
- 1866 Famine's Devastating Impact on OdishaDocument8 pages1866 Famine's Devastating Impact on OdishaWizatrix SamNo ratings yet
- Diabetes Treatment Report ProposalDocument4 pagesDiabetes Treatment Report ProposalrollyNo ratings yet
- OSH5005EP Chapter 5 PDFDocument23 pagesOSH5005EP Chapter 5 PDFEva HuiNo ratings yet
- 5 Rubbing Compound 3MDocument12 pages5 Rubbing Compound 3MSharath Gowda VGNo ratings yet
- JournalDocument6 pagesJournalkhaiz_142989No ratings yet
- Guideline MNBDocument26 pagesGuideline MNBSasmit RoyNo ratings yet
- De Leon v. MaunladDocument4 pagesDe Leon v. MaunladTibsNo ratings yet
- Updated Intake Packet 2020Document21 pagesUpdated Intake Packet 2020Allison GomoNo ratings yet
- Villa RotographDocument302 pagesVilla RotographJiggsNo ratings yet
- TDS PE91 (Sama DGN Euxyl PE9010) ENGDocument3 pagesTDS PE91 (Sama DGN Euxyl PE9010) ENGDhea 'Chiu' SamanthaNo ratings yet
- Checklist For AmbulanceDocument5 pagesChecklist For AmbulanceMRPSH Quality100% (1)