Professional Documents
Culture Documents
Obat KB
Uploaded by
Firma Nurdinia DewiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Obat KB
Uploaded by
Firma Nurdinia DewiCopyright:
Available Formats
Gynecological Endocrinology, August 2009; 25(8): 543545
CASE REPORT
Oral stomatitis induced by endogenous progesterone: Case report
ELIANA M. MINICUCCI1, ALINE B. CARRENHO1, SILKE A. T. WEBER2, FERNANDA M. BOMBINI1, RENATA A. M. A. RIBEIRO1, MARIANGELA E. A. MARQUES3, & DANIEL A. RIBEIRO4
Department of Dermatology and Radiotherapy, 2Department of Otorhinolaryngology and Ophthalmology, 3Department of Pathology, Botucatu Medical School, Sao Paulo State University, UNESP, Sao Paulo, Brazil, and 4Department of Biosciences, Federal University of Sao Paulo, UNIFESP, Santos, Sao Paulo, Brazil (Received 21 February 2008; revised 12 April 2009; accepted 27 April 2009)
1
Abstract Oral stomatitis induced by endogenous progesterone is a rare clinical condition which may be associated with cutaneous involvement. That is probably due to the peak of progesterone production during the luteal phase of the menstrual cycle. In the present case report, a 21-year-old patient displayed recurrent ulcerative lesions located on the buccal mucosa or the upper lip, on a monthly basis since the age of 15. Such lesions would always manifest themselves on the second day until the end of the menstrual cycle.
Keywords: Oral stomatitis, progesterone
Introduction Hypersensitivity induced by female sexual hormones is a rare clinical condition in which the patient develops a hypersensitivity reaction to endogenous progesterone. Such pathological condition occurs in patients ranging from 16 to 48 years of age with a predominance of young people [1]. Clinical manifestation is triggered every month during the luteal phase of the menstrual cycle, when the peak of progesterone production is reached. The clinical manifestations are variable [2] and include urticaria [3,4], erythema multiforme like-reaction [5], and eczema [6]. However, after the menstrual cycle, lesions disappear spontaneously. To date, a large number of studies have addressed clinical manifestations, especially on the skin, induced by endogenous progesterone. To the best of our knowledge, there are a few case reports addressing lesions specically in the oral mucosa [2]. Therefore, such a circumstance justies this case report as well as others; and, by taking into consideration, the current article describes a case report of oral stomatitis induced by endogenous progesterone.
Case report A 21-year-old Caucasian woman was referred to the Department of Dermatology, at the Ambulatory Care Center of Stomatology at Botucatu Medical School Sao Paulo State University (UNESP), Brazil complaining of ulcerative lesions in the perioral region, buccal mucosa, and upper lip (Figures 1 and 2). The patient reported that those lesions were painful. She also added that they had rst appeared when she was 15 years old, on a monthly basis. However, the general conditions of health were good. Under clinical examination, no skin abnormalities were found. No drugs were used for minimizing the symptomatology. To exclude herpes as putative diagnosis, Tzancks test was performed [7]. The result was negative; and, as a consequence, incisional biopsy was performed. Microscopically, the lesion had sub- and intraepithelial vesicles associated with necrosis in the basal layer (Figure 3). Moderate inammatory inltrate consisting of lymphocytes, neutrophils and eosinophils was present, with some of the inammatory cells located in the perivascular region (Figure 3). Skin testing
Correspondence: Daniel Araki Ribeiro, DDS, PhD, Departamento de Biocie ncias, Universidade Federal de Sa o Paulo UNIFESP, Av. Ana Costa 95, 11060001 Santos, SP, Brazil. Tel: 55-1332218058. Fax: 55-1332232592. E-mail: daribeiro@unifesp.br ISSN 0951-3590 print/ISSN 1473-0766 online 2009 Informa UK Ltd. DOI: 10.1080/09513590903015585
544
E. M. Minicucci et al. followed a consultation with her gynecologist, in which it was prescribed Tamoxifen (Nolvadex), an antiestrogen agent, at a dosage of 20 mg/day for 2 months as described elsewhere [8]. The patient reported that her clinical symptoms began to decline gradually over a few weeks, and no recurrences were detected up to now (8 months after initial diagnosis). Discussion Autoimmune reaction triggered by endogenous progesterone is a rare clinical condition. The picture is characterized by recurrent cutaneous lesions during the luteal phase of the menstrual cycle, when the levels of endogenous progesterone are increased. Patients have reported cyclic lesions mainly in the skin. Such lesions appear before menstruation and remain even after the menstrual cycle is over [2]. In this case report, we have been able to report the instance of a woman with oral manifestations induced by endogenous progesterone. The lesions occurred in the perioral region, buccal mucosa, and upper lip with symptomatology. The early clinical pattern seemed to be a herpes infection, but Tzancks test presented a negative result. Moghadam et al. [8] have postulated that lesions induced by endogenous progesterone disappear 1 week after the menstrual cycle. Other authors have assumed hypersensitivity to be induced by endogenous progesterone, such as anaphylaxis during the menstrual cycle [9]. All symptoms disappear after some days [10,11]. Skin testing with estrogen (1 mg/ml) and Depo-Provera (1 mg/ml), a derivative of progesterone, was performed and no reaction in skin areas developed after 48-h evaluation. There is no relationship between oral stomatitis induced by progesterone and positive response in this test. Therefore, nal diagnosis was perfomed taking into consideration the clinical history only. The underlying mechanisms by which endogenous progesterone becomes antigenic remain unknown so far. It has been suggested that abnormalities in the composition of the hormone are present in women able to develop such autoimmune reaction [11]. The occurrence of antibodies against endogenous progesterone has been demonstrated in patients presenting history of oral ulcers since their rst menstruation [12]. Another possibility is a crossreaction between endogenous progesterone and circulating antibodies produced by putative antigen present in the body, such as in the case of a viral infection [11,12]. Growing evidence suggests that synthetic progesterone may stimulate antibodies against endogenous progesterone in contraceptive users [13]. Therapy is the use of anti-estrogenic drugs, such as Tamoxifen [14], estrogens (Premarin), which are
with estrogen (1 mg/ml) and Depo-Provera (1 mg/ ml), a derivative of progesterone, was performed and no reaction in skin areas developed after 48-h evaluation. Taken as a whole, these ndings supported the nal diagnosis of oral stomatitis induced by endogenous progesterone. After that, the patient
Figure 1. Clinical aspects of lesions in the upper lip.
Figure 2. Clinical aspects of lesions in the buccal mucosa.
Figure 3. Photomicrography of the lesion (H.E. stain, 640 magnication).
Stomatitis and progesterone able to interrupt the ovulation process as well as the production of endogenous progesterone [2,3]. Nevertheless, several patients do not undergo any therapy [15]. In this case, the patient received Tamoxifen (Nolvadex) after establishing the nal diagnosis, at a dosage of 20 mg/day for 2 months as described elsewhere [8]. The patient reported that her clinical symptoms began to decline gradually over a few weeks, and no recurrences were detected up to now (8 months after initial diagnosis). As a conclusion, oral stomatitis induced by endogenous progesterone is a rare disease. Histological conrmation of the clinical diagnosis is not essential in most cases. Gynecologists, dentists and/ or endocrinologists should be aware of such concerns. Declaration of interest: The authors report no conicts of interest. The authors alone are responsible for the content and writing of the article.
545
4. 5.
6. 7.
8.
9.
10. 11.
12.
References
1. Basomba A, Guerrero M, Campos A, Villalmanzo JG. Grave anaphylactic-like reaction in the course of menstruation: a case report. Allergy 1987;42:477479. 2. Berger H. Ulcerative stomatitis caused by endogenous progesterone. Ann Intern Med 1955;42:205208. 3. Cheesman KI, Gaynor LV, Chatterton RT Jr, Radvany RM. Identication of a 17 hydroxyporgesterone-binding immuno-
13.
14.
15.
globulin in the serum of a woman with periodic rashes. J Clin Endocrinol Metab 1985;55:597599. Kasperska-Zajac A, Brzoza Z, Rogala B. Sex hormones and urtica ria. J Dermatol Sci 2008;52:7986. Walling HW, Scupham RK. Autoimmune progesterone dermatitis. Case report with histologic overlap of erythema multiforme and urticaria. Int J Dermatol 2008;47:380382. Farah FS, Shbaklu Z. Autoimmune progesterone urtica ria. J Allergy Clin Immunol 1971;48:257261. Ozcan A, Senol M, Saglam H, Seyhan M, Durmaz R, Aktas E, Ozerol IH. Comparison of the Tzanck test and polymerase chain reaction in the diagnosis of cutaneous herpes simplex and varicella zoster virus infections. Int J Dermatol 2007;46:11771179. Moghadam BKH, Hersini S, Baker BF. Autoimmune progesterone dermatitis and stomatitis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998;85:537541. Bemanian MH, Gharagozlou M, Farashahi MH, Nabavi M, Shirkhoda Z. Autoimmune progesterone anaphylaxis. Iran J Allergy Asthma Immunol 2007;6:9799. Hart R. Autoimmune progesterone dermatitis. Arch Dermatol 1977;113:426430. Herzberg AJ, Strohmeyer CR, Cirillo-Hyland VA. Autoimmune progesterone dermatitis. J Am Acad Dermatol 1995;32: 333335. Jenkins J, Geng A, Robinson-Bostom L. Autoimmune progesterone dermatitis associated with infertility treatment. J Am Acad Dermatol 2008;58:353355. Stephens CJM, Wojnarowska FT, Willkinson JD. Autoimmune progesterone dermatitis responding to tamoxifen. Br J Dermatol 1989;121:135137. Cocuroccia B, Gisondi P, Gubinelli E, Girolomoni G. Autoimmune progesterone dermatitis. Gynecol Endocrinol 2006;22:5456. Teelucksingh S, Edwards CRW. Autoimmune progesterone dermatitis. J Intern Med 1990;121:135137.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Modified Quad HelixDocument5 pagesModified Quad HelixFirma Nurdinia DewiNo ratings yet
- 3Mix-MP in Endodontics - An overview of the triple antibiotic pasteDocument10 pages3Mix-MP in Endodontics - An overview of the triple antibiotic pasteFirma Nurdinia DewiNo ratings yet
- Critical and Unexpected Findings Reporting Policy 1Document8 pagesCritical and Unexpected Findings Reporting Policy 1Firma Nurdinia DewiNo ratings yet
- A New Modified Tandem Appliance For Management of Developing Class III MalocclusionDocument5 pagesA New Modified Tandem Appliance For Management of Developing Class III MalocclusionFirma Nurdinia DewiNo ratings yet
- Dentinogenesis GigiDocument5 pagesDentinogenesis GigiFirma Nurdinia DewiNo ratings yet
- KonservasiDocument7 pagesKonservasiFirma Nurdinia DewiNo ratings yet
- Compound Compleks OdontomaDocument6 pagesCompound Compleks OdontomaFirma Nurdinia DewiNo ratings yet
- Klas 3 KoreksiDocument8 pagesKlas 3 KoreksiFirma Nurdinia DewiNo ratings yet
- Catlan's ApplianceDocument5 pagesCatlan's ApplianceFirma Nurdinia DewiNo ratings yet
- Dentinogenesis GigiDocument5 pagesDentinogenesis GigiFirma Nurdinia DewiNo ratings yet
- 3 MixDocument8 pages3 MixFirma Nurdinia DewiNo ratings yet
- Non-Surgical Treatment of Periapical Lesion Using Calcium Hydroxide-A Case ReportDocument4 pagesNon-Surgical Treatment of Periapical Lesion Using Calcium Hydroxide-A Case ReportNadya PurwantyNo ratings yet
- Compound Compleks OdontomaDocument6 pagesCompound Compleks OdontomaFirma Nurdinia DewiNo ratings yet
- 3 MixDocument6 pages3 MixFirma Nurdinia DewiNo ratings yet
- 3 MixDocument4 pages3 MixFirma Nurdinia DewiNo ratings yet
- 3mix MPDocument6 pages3mix MPFirma Nurdinia DewiNo ratings yet
- OrthiDocument16 pagesOrthiFirma Nurdinia DewiNo ratings yet
- KonservasiDocument7 pagesKonservasiFirma Nurdinia DewiNo ratings yet
- 1 1 8-25 PDFDocument18 pages1 1 8-25 PDFYunisca SeptianiNo ratings yet
- Periodontal Host Modulation With Antiproteinase Anti Inflammatory and Bone Sparing AgentsDocument26 pagesPeriodontal Host Modulation With Antiproteinase Anti Inflammatory and Bone Sparing AgentsVrushali BhoirNo ratings yet
- 3 MixDocument8 pages3 MixFirma Nurdinia DewiNo ratings yet
- OrthodonticDocument3 pagesOrthodonticFirma Nurdinia DewiNo ratings yet
- v04 n04 01Document17 pagesv04 n04 01Firma Nurdinia DewiNo ratings yet
- Kekambuhan Gingivitis Hiperplasi Setelah Gingivektomi: (Recurrent of Hyperplastic Gingivitis After Gingivectomy)Document4 pagesKekambuhan Gingivitis Hiperplasi Setelah Gingivektomi: (Recurrent of Hyperplastic Gingivitis After Gingivectomy)Firman LongtankNo ratings yet
- Obat KBDocument4 pagesObat KBFirma Nurdinia DewiNo ratings yet
- LeukemiaDocument6 pagesLeukemiaFirma Nurdinia DewiNo ratings yet
- PerokokDocument6 pagesPerokokFirma Nurdinia DewiNo ratings yet
- LeukemiaDocument6 pagesLeukemiaFirma Nurdinia DewiNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Diabetes MellitusDocument48 pagesDiabetes Mellitusladylisette67% (3)
- Anaphy Finals ReviewerDocument193 pagesAnaphy Finals Reviewerxuxi dulNo ratings yet
- Congenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeDocument7 pagesCongenital Hypothyroidism: Screening, Diagnosis, Management, and OutcomeIbrahim Abdul KareemNo ratings yet
- 12 Liver-FunctionDocument6 pages12 Liver-FunctionSubhi MishraNo ratings yet
- Causes of Endocrine DisordersDocument8 pagesCauses of Endocrine DisordersKrystel Mae GarciaNo ratings yet
- Adrenal hormones: fight or flight responseDocument49 pagesAdrenal hormones: fight or flight responseNona NanoNo ratings yet
- Molecular ClockworkDocument10 pagesMolecular Clockworkgarsa psikiatriNo ratings yet
- Myocardial InfarctionDocument12 pagesMyocardial InfarctionRifka Meilinda Putri IINo ratings yet
- 821566642727unit-2 - Nutrition and DieteticsDocument12 pages821566642727unit-2 - Nutrition and DieteticsGaganpreet Kaur Fashion DesigningNo ratings yet
- 2562 - PDF OmigatDocument11 pages2562 - PDF OmigatkhansarafidaNo ratings yet
- Garret's Personal Diet Plan!: Meal 1Document2 pagesGarret's Personal Diet Plan!: Meal 1garrettNo ratings yet
- Cushing'S Syndrome and Cushing'S Disease: Your Questions AnsweredDocument9 pagesCushing'S Syndrome and Cushing'S Disease: Your Questions Answeredmawarni siahaanNo ratings yet
- Reproductive SystemDocument49 pagesReproductive SystemAyro Business CenterNo ratings yet
- Body Types MCQDocument9 pagesBody Types MCQDoha DharewaNo ratings yet
- Nutritional BiochemistryDocument17 pagesNutritional BiochemistryVytheeshwaran Vedagiri100% (13)
- Mother and Daughters GuideDocument6 pagesMother and Daughters GuideJane AndersonNo ratings yet
- Energy Circles 1Document34 pagesEnergy Circles 1Satish Agrawal86% (7)
- 4.3 THE MENSTRUAL CYCLE (Form 1 Science)Document25 pages4.3 THE MENSTRUAL CYCLE (Form 1 Science)RATNAJYOUTI A/P KATHIRESAN Moe100% (1)
- Genetic Predisposition in Type 2 Diabetes A PromisingDocument23 pagesGenetic Predisposition in Type 2 Diabetes A PromisingRa,i Al HaddadNo ratings yet
- JaundiceDocument3 pagesJaundiceNyaoNyao MarcellanaNo ratings yet
- Krok 1 - 2006 (General Medicine) - EneutronDocument58 pagesKrok 1 - 2006 (General Medicine) - EneutronHarsh NimavatNo ratings yet
- Biochemistry IDocument10 pagesBiochemistry IKathiravan Murugesan (Kathir An)No ratings yet
- Lecture Notes-Bioreactor Design and Operation-1Document19 pagesLecture Notes-Bioreactor Design and Operation-1LCtey100% (1)
- WORD ROOTDocument11 pagesWORD ROOTta0606hiroNo ratings yet
- NUR11O1 Integrated Human Anatomy and Physiology Department of Biology Institute of Arts and Sciences Far Eastern UniversityDocument4 pagesNUR11O1 Integrated Human Anatomy and Physiology Department of Biology Institute of Arts and Sciences Far Eastern UniversityPrancheska Abigayle Peneyra SantiagoNo ratings yet
- Week 2 Endocrine Anatomy and Physiology Review & Pituitary DisturbancesDocument27 pagesWeek 2 Endocrine Anatomy and Physiology Review & Pituitary DisturbancesZiqri Dimas SandyNo ratings yet
- Role of Micro-Mineral in Infertility in Dairy CattleDocument23 pagesRole of Micro-Mineral in Infertility in Dairy CattlenaturalamirNo ratings yet
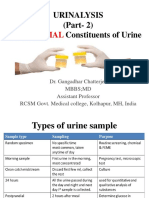
- Urinalysis (Part-2) Constituents of Urine: AbnormalDocument49 pagesUrinalysis (Part-2) Constituents of Urine: AbnormalArnab GhoshNo ratings yet
- Human Digestive SystemDocument19 pagesHuman Digestive SystemCrow LordNo ratings yet
- Mindray Bs 200Document13 pagesMindray Bs 200Roberto AriasNo ratings yet