Professional Documents
Culture Documents
Cancer Epidemiol Biomarkers Prev 2008 Scheurer 1277 81
Uploaded by
valuatOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cancer Epidemiol Biomarkers Prev 2008 Scheurer 1277 81
Uploaded by
valuatCopyright:
Available Formats
Long-term Anti-inflammatory and Antihistamine Medication Use and Adult Glioma Risk
Michael E. Scheurer, Randa El-Zein, Patricia A. Thompson, et al. Cancer Epidemiol Biomarkers Prev 2008;17:1277-1281.
Updated version
Access the most recent version of this article at: http://cebp.aacrjournals.org/content/17/5/1277
Cited Articles Citing articles
This article cites by 27 articles, 11 of which you can access for free at: http://cebp.aacrjournals.org/content/17/5/1277.full.html#ref-list-1 This article has been cited by 11 HighWire-hosted articles. Access the articles at: http://cebp.aacrjournals.org/content/17/5/1277.full.html#related-urls
E-mail alerts Reprints and Subscriptions Permissions
Sign up to receive free email-alerts related to this article or journal. To order reprints of this article or to subscribe to the journal, contact the AACR Publications Department at pubs@aacr.org. To request permission to re-use all or part of this article, contact the AACR Publications Department at permissions@aacr.org.
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
1277
Short Communication
Long-term Anti-inflammatory and Antihistamine Medication Use and Adult Glioma Risk
Michael E. Scheurer,1 Randa El-Zein,1 Patricia A. Thompson,5 Kenneth D. Aldape,2 Victor A. Levin,3 Mark R. Gilbert,3 Jeffrey S. Weinberg,4 and Melissa L. Bondy1
Departments of 1Epidemiology, 2Pathology, 3Neuro-Oncology, and 4Neurosurgery, University of Texas M. D. Anderson Cancer Center, Houston, Texas; and 5Cancer Prevention and Control Program, Arizona Cancer Center, University of Arizona, Tucson, Arizona
Abstract
A personal history of asthma or allergy has been associated with a reduced risk for adult malignant gliomas. Recent reports on the use of nonsteroidal antiinflammatory drugs (NSAID) and the presence of risk alleles in asthma susceptibility genes showed similar inverse associations. To further explore the relationship between immune mediators and gliomas, we examined the use of NSAID and antihistamines, history of asthma or allergy, and infection in 325 glioma cases and 600 frequency-matched controls from the metropolitan area of Houston, TX (2001-2006). The regular use of NSAID was associated with a 33% reduction in the risk for glioma, suggestive of possible antitumor activity. Surprisingly, regular long-term antihistamine use among those reporting a history of asthma or allergies was significantly associated with a 3.5-fold increase in the risk for glioma. Similar to previous reports, cases in our study were less likely to have reported asthma, allergy, or a history of a number of viral infections (chickenpox or shingles, oral herpes, and mononucleosis) than controls. We therefore speculate that the observed positive association with antihistamine use may reflect an alteration of protective immune factors in susceptible individuals. Our results lend additional support for an important but unknown link between malignant brain tumors and immune mediators. (Cancer Epidemiol Biomarkers Prev 2008;17(5):1277 81)
Introduction
Malignant gliomas are the most common primary brain tumor in adults, yet little is known about their etiology. Epidemiologic studies suggest a lower risk for gliomas among people reporting a history of allergies and asthma (1-10). Schwartzbaum et al. (11) reported that asthma susceptibility gene polymorphisms in IL4RA and IL13 were associated with a decreased risk for adult gliomas; however, they were unable to show significance in a larger analysis (12). Another report suggested a reduced risk for glioma with the use of nonsteroidal antiinflammatory drugs (NSAID; ref. 13). These studies lend support for a yet unexplained association between immune factors and glioma risk. Antihistamines, a class of commonly used allergy drugs, have not been well examined in relation to adult gliomas. Studies on the effects of antihistamine use on the risk for pediatric brain tumors largely pursue a direct carcinogenic action of antihistamines as nitrosatable exposures in the brain; however, results have been inconclusive (14-17). A 2-year feeding study (National Toxicology Program, CAS No. 147-24-0, NTP Study TER82067) reported increased incidences of gliomas in male Fischer 344/N rats after administration of diphenhydramine hydrochloride, the most common antihistamine. These drugs act to alleviate symptoms associated with histamine release after exposure to allergens. We speculated that antihistamine use would be more common among persons prone to allergy and more likely to be associated with a decrease in risk, as has been report in previous studies (6, 7, 10). We used data from a case-control study on adult glioma in greater Houston, TX, to examine the relationships between these medications and glioma risk.
Materials and Methods
Subjects. Cases (z18 years) were newly diagnosed between January 2001 and January 2006 with a glioma (International Classification of Diseases for Oncology, 3rd Edition, codes 9380-9481) and resided in the following Texas counties: Austin, Brazoria, Chambers, Colorado, Fort Bend, Galveston, Harris, Jefferson, Liberty, Montgomery, Orange, San Jacinto, Walker, Waller, and Wharton. Cases were interviewed before radiotherapy or chemotherapy but typically after surgery. Proxies were interviewed for subjects unable to participate because of disability or death. For all cases, diagnosis was confirmed by a neuropathologist at the M. D. Anderson Cancer Center. Controls, frequency-matched
Received 9/21/07; revised 3/3/08; accepted 3/4/08. Grant support: National Cancer Institute grant CA 070917 (M.L. Bondy). Note: Current address for M.E. Scheurer: Dan L. Duncan Center, Baylor College of Medicine, Houston, Texas. Requests for reprints: Melissa L. Bondy, Department of Epidemiology, University of Texas M. D. Anderson Cancer Center, Unit 1340, P.O. Box 301439, Houston, TX 77230-1439. Phone: 713-794-5264; Fax: 713-792-9568. E-mail: mbondy@mdanderson.org Copyright D 2008 American Association for Cancer Research. doi:10.1158/1055-9965.EPI-07-2621
Cancer Epidemiol Biomarkers Prev 2008;17(5). May 2008
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
1278
Medication Use and Glioma Risk
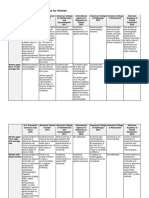
Table 1. Demographic and inflammation-related characteristics of study subjects, Harris County Adult Glioma Study, 2001-2006
Controls (n = 600) Age (y)c Mean (SE) Genderc [n (%)] Male Female Racec [n (%)] White African-American Hispanic Other Education [n (%)] <High school High school/some college College degree Advanced degree Ever cigarette use [n (%)] Ever alcohol use [n (%)] Family history of cancer [n (%)] Family history of brain tumor [n (%)] Inflammation-related events History of asthma or allergy [n (%)] History of chickenpox [n (%)] History of shingles [n (%)] History of oral herpes [n (%)] History of mononucleosis [n (%)] History of migraine headaches [n (%)] Previous head injury [n (%)] Previous stroke [n (%)] 50.1 (0.54) 311 (52) 289 (48) 476 41 71 12 21 250 170 159 453 546 468 48 202 515 51 76 65 50 184 18 (79) (7) (12) (2) (4) (42) (28) (26) (76) (91) (78) (8) (34) (86) (9) (13) (11) (8) (31) (3) Cases (n = 325) 50.6 (0.74) 188 (58) 137 (42) 264 17 37 7 16 173 75 57 235 249 261 51 44 239 17 10 13 4 115 6 (81) (5) (11) (2) (5) (54) (23) (18) (73) (77) (80) (16) (14) (74) (5) (3) (4) (1) (36) (2) P value* 0.53 0.08 0.80
0.001
0.32 <0.001 0.412 <0.001 <0.001 0.001 0.069 <0.001 0.001 <0.001 0.104 0.292
*P values derived from m2 tests for categorical variables and t tests for continuous variables; comparison of cases to controls. cMatching variables.
to cases by age, gender, and ethnicity, were Englishspeaking residents of the same Texas counties, obtained through standard random-digit dialing (18, 19). Interested eligible controls were contacted by study personnel to obtain consent and arrange an interview. Overall response rates were 77% for cases and 53% for controls. Interviews. Structured in-person or telephone interviews using questionnaires and show cards were conducted with consenting cases (or proxies) and controls. Neither cases nor controls were told of the study hypotheses during the interview. In-person interviews were conducted for 46% of cases and 5% of controls; telephone interviews were conducted for 54% of cases and 95% of controls. Subjects answered questions about demographic characteristics, personal and family medical history, and occupational and environmental exposures. The inflammation-related questions of interest consisted of all infectious diseases, self-report of asthma or any allergy, and conditions associated with inflammation in the brain (stroke, migraine headaches, and brain injury). Information on all medications taken during the previous 10 years was also obtained. The two medications of interest for the analysis were antiinflammatory agents (NSAID) linked with reduced risk for other cancers and antihistamines taken for allergies, which have been shown to confer a reduced risk for gliomas. Subjects were shown or read aloud a list of these drugs (generic and brand names). Response rates to the medication questions among cases and controls did not differ significantly for in-person or telephone interviews. Cases reported similar use for in-person (15% antihistamines, 21% NSAID) and telephone (13% antihistamines,
23% NSAID) interviews. Controls reported slightly higher use for in-person (20% antihistamines, 44% NSAID) compared with telephone (15% antihistamines, 31% NSAID) interviews; however, this was most evident for NSAID use. Participants were asked whether they had taken these drugs on a regular basis for 6 months or more before diagnosis (cases) or time of interview (controls). If the respondent reported regular use, the interviewer asked the specific name of the drug(s) and the duration of regular use; dosage was not obtained. Data Analysis. Unconditional logistic regression was used to estimate odds ratios and 95% confidence intervals (95% CI). Variables that were significantly related to case status in univariate analysis were evaluated for inclusion in the final logistic model, which was adjusted for age, gender, and race. Reference categories were those who reported no regular medication use. Proxy-reported data did not appreciably alter our findings and were not excluded from our analysis. To be considered a confounder, the characteristics in Table 1 had to be associated with the outcome in the unexposed, associated with the exposure among the controls, and must have changed the point estimate by more than 10% after adjustment. None of the variables were found to be confounders by this method. All analyses were done using Stata version 8.2. All P values are two-sided with a 0.05 level of significance.
Results
We obtained complete interviews from 325 cases, including 33 (4%) proxy reports, and 600 controls.
Cancer Epidemiol Biomarkers Prev 2008;17(5). May 2008
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
Cancer Epidemiology, Biomarkers & Prevention
1279
Table 2. Adjusted odds ratios for the use of antihistamines and anti-inflammatory agents among glioma cases and controls, Harris County Adult Glioma Study, 2001-2006
Controls (n = 600) Antihistamine use Yes No Anti-inflammatory use Yes No History of asthma or allergy Yes No History of chickenpox Yes No History of oral herpes Yes No History of mononucleosis Yes No History of migraine headaches Yes No Previous head injury Yes No 92 508 188 412 202 398 515 85 76 524 65 535 50 550 184 416 Cases (n = 325) 42 278 72 248 44 276 236 84 10 310 13 307 4 316 115 205 Odds ratio (95% CI) 1.37 (0.87, 2.14) Reference 0.67 (0.47, 0.96) Reference 0.34 (0.23, 0.51) Reference 0.52 (0.36, 0.75) Reference 0.28 (0.14, 0.57) Reference 0.40 (0.21, 0.76) Reference 0.19 (0.07, 0.54) Reference 1.41 (1.03, 1.93) Reference
NOTE: The odds ratios were derived from unconditional logistic regression models, adjusting for age, gender, and race, and controlling for all other covariates.
Controls, on average, were more highly educated, reported a history of alcohol use, and were more likely to report a positive history of the inflammation-related variables than cases (Table 1). After controlling for all other covariates in the multivariable model (listed in Table 2), the use of NSAID was associated with a 33% reduction in risk (odds ratio, 0.67; 95% CI: 0.47, 0.96), whereas the use of antihistamines was associated with a 37% increase in the risk for glioma (odds ratio, 1.37; 95% CI: 0.87, 2.14; Table 2). However, when antihistamine use was examined only among those reporting a history of asthma or allergies, a 3.56-fold increase in risk was seen for those who reported the longest (z10 years) regular antihistamine use (Table 3). History of inflammation-related events was asked of all participants (Table 1), including asthma or allergy, chickenpox or shingles, oral herpes, mononucleosis, migraine headaches, head injury, and stroke. Adjusted odds ratios for each inflammation-related event and
medication use are presented in Table 2. A history of asthma or allergy was associated with a 66% reduction in the risk for glioma (odds ratio, 0.34; 95% CI: 0.23, 0.51). A history of chickenpox was associated with a 48% reduction in the risk for glioma (odds ratio, 0.52; 95% CI: 0.36, 0.75). A history of self-reported oral herpes was also associated with a decrease in the risk for glioma (odds ratio, 0.28; 95% CI: 0.14, 0.57); however, the number of exposed cases was low. Similarly, self-reported mononucleosis resulted in a 60% reduction in the risk for glioma (odds ratio, 0.40; 95% CI: 0.21, 0.76). Although the number of subjects reporting a history of migraine headache was low (50 controls and 4 cases), a significant reduction in risk (81%) was observed and the upper limit of the confidence interval remained well below 1.0 (odds ratio, 0.19; 95% CI: 0.07, 0.54). Previous head injury also showed a significant increase in risk (odds ratio, 1.41; 95% CI: 1.03, 1.93), although this could be because of recall bias.
Table 3. Adjusted odds ratios for the use of antihistamines stratified by history of asthma or allergies among glioma cases and controls, Harris County Adult Glioma Study, 2001-2006
Antihistamine use No asthma or allergy history No use <10 y z10 y Any use Any asthma or allergy history No use <10 y z10 y Any use Controls (n = 600) 362 21 15 36 146 32 24 56 Cases (n = 325) 259 14 8 22 23 8 13 21 Odds ratio (95% CI) Reference 0.91 (0.45, 1.84) 0.70 (0.29, 1.69) 0.82 (0.47, 1.44) Reference 1.73 (0.69, 4.29) 3.56 (1.56, 8.14) 2.54 (1.28, 5.03)
NOTE: The odds ratios were derived from unconditional logistic regression models, adjusting for age, gender, and race.
Cancer Epidemiol Biomarkers Prev 2008;17(5). May 2008
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
1280
Medication Use and Glioma Risk
Discussion
In our analysis, cases were more likely to report regular long-term use of antihistamines than controls, especially cases reporting a history of allergies or asthma, whereas the inverse was true for NSAID. Schlehofer et al. (6), in their report from a multinational study, found a 30% reduction in the risk for adult glioma with antihistamine use. A recent report in a United Kingdom population showed a slight but nonsignificant reduction in risk associated with ever use of antihistamines by those reporting hay fever, allergic rhinitis, or conjunctivitis (7). A related report from the Nordic-United Kingdom pooled study also found a nonsignificant 22% reduction in the risk of ever antihistamine use in those reporting hay fever (10). These reports could differ from the current findings because of the definition of long-term antihistamine use in the current study or because of differences in use of these drugs between the different study populations. In the report by Wigertz et al. (10), 51% of controls who reported hay fever took antihistamines compared with 48% of cases. In our study, 28% of controls who reported a history of asthma or allergies regularly took antihistamines compared with 48% of cases. Our findings support a positive association for glioma in adults who were long-term users of antihistamines. Although there was a weak correlation (q = 0.2438) between history of asthma or allergies and antihistamine use, the inclusion of an interaction term (P = 0.02) in our model did not significantly alter the main effects for the other terms. Moreover, the addition of asthma or allergies to a main-effects model modified the effect of antihistamine use, and the largest effect in the stratified analysis was seen among those who reported a history of asthma or allergies and long-term use of antihistamines. Studies have reported a protective effect of allergies or asthma on the development of several cancers, including gliomas (20). Fairly consistent risk reductions of 30% to 50% (similar to our current results) have been reported for glioma among those with a history of allergies or asthma in case-control and cohort studies from the United States (1, 3, 9), Europe (5-8, 10), and Australia (2, 4). Wiemels et al. (21) reported that immunoglobulin E levels, a measure of allergic response, were lower in adult glioma cases than controls (odds ratio, 0.37) and that early-onset allergies (before the age of 13 years) were more likely to be related to immunoglobulin E than lateonset allergies. Stronger support for a protective association with asthma is suggested by one study reporting that, compared with controls, cases were less likely to carry polymorphisms in the IL4RA and IL13 genes that increase the risk for asthma and more likely to carry polymorphisms that decrease the risk for asthma (11). However, these findings were not replicated when the authors repeated their analysis in a larger pooled data set (12), and Turner et al. (22) were unable to show differences in brain tumor mortality among a cohort of asthma and hay fever suffers in the United States. In a similar vein, Wrensch et al. (23) reported a 40% to 60% reduction in glioma risk associated with a history of chickenpox or shingles. We showed a 48% reduction in the risk for glioma associated with chickenpox infection. They also found that measured immunoglobulin G antibody levels against varicella-zoster virus were higher
in controls than cases (23). We showed that self-reports of oral herpes lesions (herpes simplex virus) and mononucleosis (Epstein-Barr virus or Cytomegalovirus) were also higher among controls than cases. It is conceivable that the constant reactivation of these herpesviruses may increase immune surveillance and partially account for the decrease in risk associated with a history of infection. The current study adds to a growing body of literature suggesting an increasing role of modulation of the immune system in the prevention or promotion of gliomas. We recognize that additional studies are needed to corroborate our findings for antihistamines. However, these medications cross the blood-brain barrier and can have significant sedative effects. The histamine H1 receptors targeted by these drugs are found on glial cells and have been shown to stimulate proliferation in a receptor-dependent fashion (24). In addition, constitutive activation of H1 receptors triggers numerous inflammation pathways such as nuclear factor nB and arachidonic acid, leading to the production of prostaglandins, leukotrienes, and cytokines (25). These substances, in turn, could drive inflammation even in the presence of antihistamines. Moreover, histamine itself is shown to exhibit both immune-stimulatory and -suppressive behavior when interacting with the H1 receptor (26). This may explain the risk observed in the current study for the use of compounds that interfere with normal H1 receptor activity. Lastly, one report showed that melanoma cells rich in H1 receptors undergo intensive DNA damage and apoptosis in the presence of antihistamines (27). Such mechanisms could be important for glial cells that harbor high concentrations of H1 receptors. To our knowledge, this is the first report to investigate the association between adult glioma and antihistamine use in a U.S. population and to examine the joint effects of allergy or asthma with antihistamine use. A main limitation of the current study is the self-reported nature of the medications. In addition, most of our controls were interviewed by telephone whereas the interview method was split for the cases. This could introduce some information bias; however, response rates to the medication questions were similar in both groups regardless of the interview method. We also did not ask about specific types of allergies, nor did we collect data on dosage or indication for use. In future studies, we will gather detailed data on these aspects of use to allow a better understanding of the underlying mechanisms of antihistamines in glioma risk and to better understand differences in use of these drugs among allergy sufferers in our study population. Another limitation of our study is the inability to adequately account for the time between beginning antihistamine use and the glioma diagnosis. Cases were instructed to report drugs taken before 6 months prior to their diagnosis; however, this could be difficult for them to remember. On the other hand, antihistamines are not usual drugs for the relief of symptoms commonly associated with brain tumor presentation (e.g., seizures, drowsiness, limb weakness, and changes in vision, speech, personality, or memory). Therefore, the initiation of antihistamine use as a result of an undiagnosed glioma is unlikely. Several epidemiologic studies corroborate the involvement of inflammatory factors in glioma development; however, the mechanisms are still poorly
Cancer Epidemiol Biomarkers Prev 2008;17(5). May 2008
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
Cancer Epidemiology, Biomarkers & Prevention
1281
understood because of the difficulty in studying such rare tumors. We are currently working to pool data with other investigators to examine these questions more closely.
Disclosure of Potential Conflicts of Interest
M. Gilbert: Schering Plough commercial research grant and speakers bureau/honoraria. The other employees disclosed no potential conflicts of interest.
Acknowledgments
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked advertisement in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
Brenner AV, Linet MS, Fine HA, et al. History of allergies and autoimmune diseases and risk of brain tumors in adults. Int J Cancer 2002;99:252 9. 2. Cicuttini FM, Hurley SF, Forbes A, et al. Association of adult glioma with medical conditions, family and reproductive history. Int J Cancer 1997;71:203 7. 3. Hochberg F, Toniolo P, Cole P, Salcman M. Nonoccupational risk indicators of glioblastoma in adults. J Neurooncol 1990;8:55 60. 4. Ryan P, Lee MW, North B, McMichael AJ. Risk factors for tumors of the brain and meninges: results from the Adelaide Adult Brain Tumor Study. Int J Cancer 1992;51:20 7. 5. Schlehofer B, Blettner M, Becker N, Martinsohn C, Wahrendorf J. Medical risk factors and the development of brain tumors. Cancer 1992;69:2541 7. 6. Schlehofer B, Blettner M, Preston-Martin S, et al. Role of medical history in brain tumour development. Results from the international adult brain tumour study. Int J Cancer 1999;82:155 60. 7. Schoemaker MJ, Swerdlow AJ, Hepworth SJ, McKinney PA, van Tongeren M, Muir KR. History of allergies and risk of glioma in adults. Int J Cancer 2006;119:2165 72. 8. Schwartzbaum J, Jonsson F, Ahlbom A, et al. Cohort studies of association between self-reported allergic conditions, immunerelated diagnoses and glioma and meningioma risk. Int J Cancer 2003;106:423 8. 9. Wiemels JL, Wiencke JK, Sison JD, Miike R, McMillan A, Wrensch M. History of allergies among adults with glioma and controls. Int J Cancer 2002;98:609 15. 10. Wigertz A, Lonn S, Schwartzbaum J, et al. Allergic conditions and brain tumor risk. Am J Epidemiol 2007;166:941 50. 1.
11. Schwartzbaum J, Ahlbom A, Malmer B, et al. Polymorphisms associated with asthma are inversely related to glioblastoma multiforme. Cancer Res 2005;65:6459 65. 12. Schwartzbaum JA, Ahlbom A, Lonn S, et al. An international casecontrol study of interleukin-4Ra, interleukin-13, and cyclooxygenase2 polymorphisms and glioblastoma risk. Cancer Epidemiol Biomarkers Prev 2007;16:2448 54. 13. Sivak-Sears NR, Schwartzbaum JA, Miike R, Moghadassi M, Wrensch M. Case-control study of use of nonsteroidal antiinflammatory drugs and glioblastoma multiforme. Am J Epidemiol 2004; 159:1131 9. 14. Cardy AH, Little J, McKean-Cowdin R, et al. Maternal medication use and the risk of brain tumors in the offspring: the SEARCH international case-control study. Int J Cancer 2006;118:1302 8. 15. Cordier S, Iglesias MJ, Le Goaster C, Guyot MM, Mandereau L, Hemon D. Incidence and risk factors for childhood brain tumors in the Ile de France. Int J Cancer 1994;59:776 82. 16. McCredie M, Maisonneuve P, Boyle P. Antenatal risk factors for malignant brain tumours in New South Wales children. Int J Cancer 1994;56:6 10. 17. McKean-Cowdin R, Pogoda JM, Lijinsky W, Holly EA, Mueller BA, Preston-Martin S. Maternal prenatal exposure to nitrosatable drugs and childhood brain tumours. Int J Epidemiol 2003;32:211 7. 18. Harlow BL, Davis S. Two one-step methods for household screening and interviewing using random digit dialing. Am J Epidemiol 1988; 127:857 63. 19. Hartge P, Brinton LA, Rosenthal JF, Cahill JI, Hoover RN, Waksberg J. Random digit dialing in selecting a population-based control group. Am J Epidemiol 1984;120:825 33. 20. Wang H, Diepgen TL. Is atopy a protective or a risk factor for cancer? A review of epidemiological studies. Allergy 2005;60:1098 111. 21. Wiemels JL, Wiencke JK, Patoka J, et al. Reduced immunoglobulin E and allergy among adults with glioma compared with controls. Cancer Res 2004;64:8468 73. 22. Turner MC, Chen Y, Krewski D, Ghadirian P, Thun MJ, Calle EE. Cancer mortality among US men and women with asthma and hay fever. Am J Epidemiol 2005;162:212 21. 23. Wrensch M, Weinberg A, Wiencke J, et al. History of chickenpox and shingles and prevalence of antibodies to varicella-zoster virus and three other herpesviruses among adults with glioma and controls. Am J Epidemiol 2005;161:929 38. 24. Hernandez-Angeles A, Soria-Jasso LE, Ortega A, Arias-Montano JA. Histamine H1 receptor activation stimulates mitogenesis in human astrocytoma U373 MG cells. J Neurooncol 2001;55:81 9. 25. Leurs R, Church MK, Taglialatela M. H1-antihistamines: inverse agonism, anti-inflammatory actions and cardiac effects. Clin Exp Allergy 2002;32:489 98. 26. Medina MA, Quesada AR, Nunez CI, Sanchez-Jimenez F. Histamine, polyamines, and cancer. Biochem Pharmacol 1999;57:1341 4. 27. Jangi SM, Diaz-Perez JL, Ochoa-Lizarralde B, et al. H1 histamine receptor antagonists induce genotoxic and caspase-2-dependent apoptosis in human melanoma cells. Carcinogenesis 2006;27: 1787 96.
Cancer Epidemiol Biomarkers Prev 2008;17(5). May 2008
Downloaded from cebp.aacrjournals.org on June 24, 2013. 2008 American Association for Cancer Research.
You might also like
- Nej MC 082208Document2 pagesNej MC 082208anggiNo ratings yet
- Immunotherapeutic Strategies for the Treatment of GliomaFrom EverandImmunotherapeutic Strategies for the Treatment of GliomaNo ratings yet
- Managing Health in the Genomic Era: A Guide to Family Health History and Disease RiskFrom EverandManaging Health in the Genomic Era: A Guide to Family Health History and Disease RiskNo ratings yet
- Follicular Lymphoma: Current Management and Novel ApproachesFrom EverandFollicular Lymphoma: Current Management and Novel ApproachesNathan H. FowlerNo ratings yet
- Thursday, 13 June 2013 347: Scientific AbstractsDocument2 pagesThursday, 13 June 2013 347: Scientific Abstractstika_876267153No ratings yet
- Common Vaccines and The Risk of Incident Dementia A Population-Based Cohort Study - PubMedDocument2 pagesCommon Vaccines and The Risk of Incident Dementia A Population-Based Cohort Study - PubMedAle FurvisNo ratings yet
- Lung CancerDocument2 pagesLung Cancerkaustuv2uNo ratings yet
- DK CRP B-8 HarmDocument20 pagesDK CRP B-8 HarmCennikon PakpahanNo ratings yet
- Dapus 2-Feigin2005Document9 pagesDapus 2-Feigin2005sri noviyanty yusufNo ratings yet
- Clinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareFrom EverandClinical Updates in the Management of Severe Asthma: New Strategies for Individualizing Long-term CareNo ratings yet
- Targeted Therapies for Lung CancerFrom EverandTargeted Therapies for Lung CancerRavi SalgiaNo ratings yet
- Agostini 2016 - The Prevention of EpilepsyDocument2 pagesAgostini 2016 - The Prevention of EpilepsyMark CheongNo ratings yet
- Colen 2017Document7 pagesColen 2017yalocim666No ratings yet
- Impulse Oscillometry Versus Spirometry in A Long-Term Study of Controller Therapy For Pediatric AsthmaDocument9 pagesImpulse Oscillometry Versus Spirometry in A Long-Term Study of Controller Therapy For Pediatric Asthmadewi trisnawatiNo ratings yet
- Management of Infections in the Immunocompromised HostFrom EverandManagement of Infections in the Immunocompromised HostBrahm H. SegalNo ratings yet
- Chang Ve Ark. 2013 Occupational Noise Exposure and Incident Hypertension in Men A ProspectiveDocument8 pagesChang Ve Ark. 2013 Occupational Noise Exposure and Incident Hypertension in Men A ProspectivefzehragumussNo ratings yet
- AERD Genetics Protocol v6Document5 pagesAERD Genetics Protocol v6Jason WongNo ratings yet
- The Basics of Cancer ImmunotherapyFrom EverandThe Basics of Cancer ImmunotherapyHaidong DongNo ratings yet
- ARA II y Cancer EditorialDocument2 pagesARA II y Cancer EditorialFabiana MuriasNo ratings yet
- NIH Public Access: Author ManuscriptDocument13 pagesNIH Public Access: Author ManuscriptGeorge UngureanuNo ratings yet
- RefaratDocument8 pagesRefaratGrace SesaNo ratings yet
- Characterizing Opioid Use in A US Population With MigraineDocument12 pagesCharacterizing Opioid Use in A US Population With MigraineVagner PinheiroNo ratings yet
- Tumor MicroenvironmentFrom EverandTumor MicroenvironmentPeter P. LeeNo ratings yet
- FFFGVDocument10 pagesFFFGVyundaNo ratings yet
- Histopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationFrom EverandHistopathology of Preclinical Toxicity Studies: Interpretation and Relevance in Drug Safety EvaluationNo ratings yet
- Between the Lines of Genetic Code: Genetic Interactions in Understanding Disease and Complex PhenotypesFrom EverandBetween the Lines of Genetic Code: Genetic Interactions in Understanding Disease and Complex PhenotypesLeonid PadyukovNo ratings yet
- Chimerism: A Clinical GuideFrom EverandChimerism: A Clinical GuideNicole L. DraperNo ratings yet
- The Paradox of the Immune System: Protection, Chronic Inflammation, Autoimmune Disease, Cancer, and PandemicsFrom EverandThe Paradox of the Immune System: Protection, Chronic Inflammation, Autoimmune Disease, Cancer, and PandemicsNo ratings yet
- 128 Research Papers Supporting The Vaccine Autism LinkDocument96 pages128 Research Papers Supporting The Vaccine Autism LinkEllaNo ratings yet
- Multifaceted Role of IL-1 in Cancer and InflammationFrom EverandMultifaceted Role of IL-1 in Cancer and InflammationManisha SinghRating: 5 out of 5 stars5/5 (1)
- A Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimDocument14 pagesA Systematic Literature Review of The Efficacy, Effectiveness, and Safety of FilgrastimNo NameNo ratings yet
- Environmental EpidemiologyDocument5 pagesEnvironmental EpidemiologyKarthik VkNo ratings yet
- Eso AmiodaronDocument5 pagesEso AmiodaronNurhasna Sushmita SariNo ratings yet
- Mechanisms and Regulation of The Gene-Expression Response To SepsisDocument11 pagesMechanisms and Regulation of The Gene-Expression Response To SepsisNagy MonikaNo ratings yet
- Management of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)From EverandManagement of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)No ratings yet
- Statins For COPD: A Challenge To Conventional Beliefs?: ReferencesDocument3 pagesStatins For COPD: A Challenge To Conventional Beliefs?: ReferencesshayNo ratings yet
- Tumor Immune Microenvironment in Cancer Progression and Cancer TherapyFrom EverandTumor Immune Microenvironment in Cancer Progression and Cancer TherapyPawel KalinskiNo ratings yet
- The Value of BCG and TNF in AutoimmunityFrom EverandThe Value of BCG and TNF in AutoimmunityDenise FaustmanNo ratings yet
- Timed Up and Go - Diagnóstico de DemênciaDocument6 pagesTimed Up and Go - Diagnóstico de DemênciaMarta SilvaNo ratings yet
- Parcial 1 - TP 4. Chagas BENEFITDocument12 pagesParcial 1 - TP 4. Chagas BENEFITVictoria ChristieNo ratings yet
- Rivers Auty2020Document25 pagesRivers Auty2020Nadia SaiNo ratings yet
- Nihms866890 UPLOAD 3Document21 pagesNihms866890 UPLOAD 3Peter GardinerNo ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofAlmuizzu NurjannahNo ratings yet
- Pi Is 0002939412004783Document8 pagesPi Is 0002939412004783masmedicaNo ratings yet
- Stem Cell-Based Therapy for Lung DiseaseFrom EverandStem Cell-Based Therapy for Lung DiseaseJanette K. BurgessNo ratings yet
- Mutagen SensitivityDocument4 pagesMutagen SensitivityVasishta NadellaNo ratings yet
- Journal Homepage: - : IntroductionDocument6 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Immune Hematology: Diagnosis and Management of Autoimmune CytopeniasFrom EverandImmune Hematology: Diagnosis and Management of Autoimmune CytopeniasJenny M. DespotovicNo ratings yet
- Brain Tumors in ChildrenFrom EverandBrain Tumors in ChildrenAmar GajjarNo ratings yet
- 2012 Health Disparity Asthma CourseDocument63 pages2012 Health Disparity Asthma CoursethomasNo ratings yet
- Winter/Spring Term Class List: The Super Saturday ProgramDocument11 pagesWinter/Spring Term Class List: The Super Saturday ProgramvaluatNo ratings yet
- Tar Hollow State Park CampgroundDocument1 pageTar Hollow State Park CampgroundvaluatNo ratings yet
- Bimcom: User ManualDocument33 pagesBimcom: User ManualvaluatNo ratings yet
- SpecEd WorkMemDocument1 pageSpecEd WorkMemvaluatNo ratings yet
- WISC IV Handout PDFDocument121 pagesWISC IV Handout PDFvaluat100% (1)
- The T-Cell ArmyDocument14 pagesThe T-Cell ArmyvaluatNo ratings yet
- Ravens SPM Answer SheetDocument1 pageRavens SPM Answer SheetvaluatNo ratings yet
- Numerical Solutions To PDEs With Financial ApplicationsDocument41 pagesNumerical Solutions To PDEs With Financial ApplicationsvaluatNo ratings yet
- 57 TH Short Course ScheduleDocument10 pages57 TH Short Course SchedulevaluatNo ratings yet
- Breast Cancer Screening GuidelinesDocument4 pagesBreast Cancer Screening GuidelinesvaluatNo ratings yet
- TuringSpecialIssue (Nature2012) PDFDocument2 pagesTuringSpecialIssue (Nature2012) PDFvaluatNo ratings yet
- Laplace Transforms and The American StraddleDocument10 pagesLaplace Transforms and The American StraddlevaluatNo ratings yet
- Irreversible Investments and Ambiguity Aversion: Sebastian JaimungalDocument36 pagesIrreversible Investments and Ambiguity Aversion: Sebastian JaimungalvaluatNo ratings yet
- FullDocument6 pagesFullvaluatNo ratings yet
- 08-Genomic Integrity and CancerDocument42 pages08-Genomic Integrity and CancervaluatNo ratings yet
- Test Bank ECGs Made Easy 5th Edition Barbara J AehlertDocument10 pagesTest Bank ECGs Made Easy 5th Edition Barbara J AehlertErnest67% (3)
- Clinical Evaluation FormDocument1 pageClinical Evaluation FormAndalNo ratings yet
- Parasitology Lecture 16 - Blood Flukes PDFDocument4 pagesParasitology Lecture 16 - Blood Flukes PDFmiguel cuevasNo ratings yet
- Drug StudyDocument2 pagesDrug Studyluvbel100% (2)
- Ebook Gabbes Obstetrics Essentials Normal Problem Pregnancies PDF Full Chapter PDFDocument67 pagesEbook Gabbes Obstetrics Essentials Normal Problem Pregnancies PDF Full Chapter PDFandre.davis379100% (27)
- GTD Case StudyDocument9 pagesGTD Case StudyZnarf Izlah Sadanreb100% (1)
- Mirikizumab As Induction and Maintenance Therapy For UlcerativeDocument15 pagesMirikizumab As Induction and Maintenance Therapy For Ulcerativesreebhahun satishNo ratings yet
- Artifacts in CytopathologyDocument25 pagesArtifacts in Cytopathologysamuel adagaNo ratings yet
- Cerebral Palsy - Critical Elements of CareDocument25 pagesCerebral Palsy - Critical Elements of CaremarkoNo ratings yet
- NSG ProcessDocument6 pagesNSG ProcessJay-Dee Evangelista PacionNo ratings yet
- Hospital List 2019Document9 pagesHospital List 2019singhjpNo ratings yet
- "The Man Who Mistook His Wife For Hat" Is ADocument9 pages"The Man Who Mistook His Wife For Hat" Is AIADT Psy50% (2)
- A Review of The New GLP-1 Receptor Agonist/basal Insulin Fixed-Ratio Combination ProductsDocument11 pagesA Review of The New GLP-1 Receptor Agonist/basal Insulin Fixed-Ratio Combination Productsarief hakikiNo ratings yet
- NARPAA E-Class Module 3 - Historical Definitions of AutismDocument19 pagesNARPAA E-Class Module 3 - Historical Definitions of AutismnarpaaNo ratings yet
- Argumentative Essay: Why The COVID-19 Vaccine Should Be MandatedDocument10 pagesArgumentative Essay: Why The COVID-19 Vaccine Should Be MandatedJulia Brok100% (1)
- Urine TherapyDocument43 pagesUrine TherapyBashu Poudel100% (3)
- Lab Report 15438869 20231127064225Document1 pageLab Report 15438869 20231127064225carilloabhe21No ratings yet
- Ats Menjawab Soal Unas November 2021 EditedDocument26 pagesAts Menjawab Soal Unas November 2021 Editedanton suponoNo ratings yet
- Clinical Approach To A Patient With Dysphagia: Medicine UpdateDocument3 pagesClinical Approach To A Patient With Dysphagia: Medicine UpdateAnonymous XFDJfsGviNo ratings yet
- Ptosis Definition of Eyelid Ptosis: Abnormally Low Position of The Upper Eyelid Margin Caused by PoorDocument6 pagesPtosis Definition of Eyelid Ptosis: Abnormally Low Position of The Upper Eyelid Margin Caused by PoortiamaharaniNo ratings yet
- Maternal and Child Health Programmes: MCH ServicesDocument10 pagesMaternal and Child Health Programmes: MCH ServicesRosebel LaguraNo ratings yet
- 3.2 Dr. Taufin SpOT - Operating RoomDocument29 pages3.2 Dr. Taufin SpOT - Operating RoomTaqwatin Ma'rifahNo ratings yet
- GUIAS UCI para La Alimentación de Paciente CriticoDocument33 pagesGUIAS UCI para La Alimentación de Paciente CriticoFredy UmbarilaNo ratings yet
- MCN 2Document11 pagesMCN 2karenkaren09No ratings yet
- Vestibular Function TestsDocument11 pagesVestibular Function TestsM. Arief Purnanta0% (1)
- HemostasisDocument5 pagesHemostasisPadmavathi C100% (1)
- Vaccines and Vaccination History and Emerging IssuesDocument15 pagesVaccines and Vaccination History and Emerging IssuesMěđ SimoNo ratings yet
- Kenyaemr V17.3.1 Release Notes: Integration With Eid, Adt & Differential Upload DescriptionDocument3 pagesKenyaemr V17.3.1 Release Notes: Integration With Eid, Adt & Differential Upload DescriptionMigori Art DataNo ratings yet
- D Dimer Test in VTEDocument35 pagesD Dimer Test in VTEscribmedNo ratings yet
- Pathological Condition in Buffalo GenitalsDocument3 pagesPathological Condition in Buffalo GenitalsgnpobsNo ratings yet