Professional Documents
Culture Documents
Transportasi Gas Respirasi
Uploaded by
Nidia Sali PratiwiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Transportasi Gas Respirasi
Uploaded by
Nidia Sali PratiwiCopyright:
Available Formats
1
Oxygen Transport
Total Body Oxygen Stores
Oxygen in the Lung (~500 ml O
2
).
Oxygen in the Blood (~850 ml O
2
).
Oxygen in the Cells (very little except
Mb-bound).
3
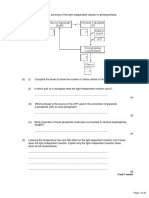
At the Lung Level
At the Tissue Level
Oxygen Is Carried in Blood in 2
Forms
Bound to hemoglobin in red blood cells.
Dissolved in plasma. Normally
insignificant.
7
Hemoglobin
Each heme molecule is capable of binding
with 1 O
2
molecule and each globin
molecule is capable of binding with 1 CO
2
molecule.
So, each molecule of Hb can bind to either 4
molecules of O
2
and 1 molecule of CO
2
100 ml of blood has about 15 gm of Hb, at Hct
= 0.45
8
Binding of O
2
to 4 heme sites given by:
4 2 2 3 2
3 2 2 2 2
2 2 2 2
2 2
) ( ) (
) ( ) (
) (
O Hb O O Hb
O Hb O O Hb
O Hb O HbO
HbO O Hb
+
+
+
+
Equilibrium constants for different reactions
different
Binding of first O
2
relatively low affinity
2nd, 3rd and 4th - much higher affinity
9
Oxygen as Oxyhemoglobin
Each gram of Hb can store about 1.34 ml
of O
2
:
1 L of blood (150 gm of Hb) can store
about 208 ml of O
2
Oxygen Capacity of
Hb.
With normal cardiac output, about 1040 ml
of O
2
can be carried in blood per minute. (4
times of the metabolic demands).
10
11
Oxygen in Dissolved Form
The amount of O
2
carried in blood in dissolved
form obeys Henrys law which states that
C
O2
= o
O2
*P
O2
.
o
O2
is the solubility coefficient of O
2
in plasma:
o
O2
= 1.35E-6 M/mmHg
= 0.03ml of O
2
/(L of plasma*mmHg)
Normal arterial plasma with P
O2
of 100 mmHg
contains 3 ml of O
2
/L of plasma and RBC water.
During a normal cardiac cycle, about 15 ml of O
2
is carried in plasma per minute, where the normal
metabolic demand is about 250 ml O
2
per minute.
12
O
2
Saturation.
Units: percent.
Fraction or percentage of all the
hemoglobin binding sites that are
currently occupied by oxygen.
14
100
Hb of capacity O
Hb with combined O
) saturation (% S
2
2
HbO2
=
Oxygen Saturation of Hb
Four (5-6?) Things Change
Oxyhemoglobin Affinity
1. Hydrogen Ion Concentration, [H
+
]
2. Carbon Dioxide Partial Pressure, PCO
2
3. Temperature
4. [2,3-DPG]
5. Special Case: Carbon Monoxide
6. Hemoglobin variants
16
17
Factors Affecting Hb-O
2
Affinity:
Summary
Hydrogen Ion:
Increased H
+
(decreased pH) increases H
+
binding to
Hb and reduces O
2
affinity (HbO
2
+H
+
HbH
+
+O
2
).
Carbon Dioxide (Bohr effect):
Increased P
CO2
increases CO
2
binding to Hb and
reduces O
2
affinity (increased O
2
delivery to tissue).
Increased P
CO2
increases H
+
and reduces O
2
affinity
(fixed acid Bohr effect).
Temperature and 2,3-DPG (diphosphoglycerate):
Increased temperature and 2,3-DPG reduces O
2
affinity.
Effect of CO & Anemia on Hb-O
2
Affinity
Normal blood with Hb=15 gm/dl, anemia with Hb=7.5 gm/dl,
and normal blood with 50% HbCO (carboxyhemoglobin).
Exercise
Increase temperature
Increased PCO
2
and
Decreased pH (acidosis)
2,3-DPG
2,3-DPG is a glycolytic intermediate
accumulates to uniquely high levels in RBCs
-Increased 2,3-DPG right shift
-Decreased 2,3-DPG left shift
Increased 2,3-DPG associated with
hypoxia.
Conditions with Increased 2,3-DPG
acclimatization to high altitudes.
chronic lung disease; emphysema.
anemia.
hyperthyroidism.
right to left shunt.
congenital heart disease.
pulmonary vascular disease.
23
Carbon Dioxide
Transport
24
At the Tissue Level
25
At the Lung Level
26
Carbon Dioxide Transport
CO
2
is transported in blood in dissolved form, as
bicarbonate ions, and as protein-bound carbamino
compound.
Protein-bound CO
2
(carbamino compounds):
Amount of CO
2
stored as carbamino compounds
is about 21 ml/L (4% of the total art CO
2
).
27
Carbon Dioxide Transport
A majority amount of CO
2
is transported in the
form of bicarbonate ions (HCO
3
-
):
Amount of CO
2
in HCO
3
-
form at P
CO2
=40
mmHg is about 420 ml/L (90% of the total
arterial CO
2
).
-
HCO H CO H O H CO
3 3 2
CA
2 2
+
+
+
28
Carbon Dioxide Transport
Haldane Effect: Increasing O
2
-saturation reduces
CO
2
content and shifts the CO
2
dissociation
curve to right. This is because, increasing P
O2
leads to :
Decrease in the formation of carbamino compound.
Release of H+ ions from the hemoglobin and resulting
in dehydration of HCO
3
-
.
29
Carbon Dioxide Dissociation Curve
Over the normal physiological range (P
CO2
= 30 to 55 mmHg
and P
O2
= 40 to 100 mmHg), the CO
2
equilibrium curve is
nearly linear. But, O
2
equilibrium curve is highly nonlinear.
Bicarbonate in RBCs.
Carbonic anhydrase is present in RBCs
CO
2
forms carbonic acid which
dissociates to H
+
and HCO
3
-
Released H
+
is buffered by histidine
residues (imidazole group)
CO H O H CO H HCO
2 2 2 3 3
+ +
+ Carbonic Anhydrase
Percent of the total PaCO
2
: 70%
Carbamino Compounds in RBCs.
Approximately 30% of RBC contents is Hb
CO
2
forms carbamino hemoglobin
Released H
+
is buffered by histidine
residues (imidazole group)
Percent of the total PaCO
2
: 23 %
CO
2
Formation in Plasma
Carbamino compounds
CO
2
binds the amine groups of plasma
proteins to form carbamino compounds.
R NH CO R NH COO H + +
+
2 2
34
Carbon Dioxide Transport
Three forms of storage, transport & kinetics of CO
2
in blood
Chloride Shift (Hamburger Shift)
Newly formed HCO
3
-
passes out of RBC
Cl
-
diffuses into RBC to maintain
electroneutrality
Chloride shift is rapid
Complete before the RBCs exit capillary
36
Tissue-Gas Exchange: Summary
Gas exchange processes in the peripheral organs
are essentially opposite those in the lungs.
O
2
is released from the capillary blood to the
tissues and diffuses to the mitochondria where O
2
is converted to CO
2
and energy (ATP) through
cellular metabolism.
CO
2
diffuses from the tissues to the blood stream
and is transported to the lungs for elimination.
The exchange of O
2
and CO
2
in the blood-tissue
exchange unit depends on P
O2
, P
CO2
, and also on
O
2
and CO
2
saturation curves.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2015 4-H Show & Sale CatalogDocument53 pages2015 4-H Show & Sale CatalogFauquier NowNo ratings yet
- 1 A Finalexam FNH330 June 2015 Final Review QuestionsDocument6 pages1 A Finalexam FNH330 June 2015 Final Review QuestionsChinley HinacayNo ratings yet
- 351 UN 1824 Sodium Hydroxide SolutionDocument8 pages351 UN 1824 Sodium Hydroxide SolutionCharls DeimoyNo ratings yet
- Silly VersesDocument29 pagesSilly Verseskevin daleNo ratings yet
- Environmental Research and Public Health: International Journal ofDocument12 pagesEnvironmental Research and Public Health: International Journal ofKarenNo ratings yet
- Photosynthesis PastPaper QuestionsDocument24 pagesPhotosynthesis PastPaper QuestionsEva SugarNo ratings yet
- Meditran SX Sae 15w 40 API CH 4Document1 pageMeditran SX Sae 15w 40 API CH 4Aam HudsonNo ratings yet
- MCS120 220 Error Ref - GAA30082DAC - RefDocument21 pagesMCS120 220 Error Ref - GAA30082DAC - RefCoil98No ratings yet
- Meng Mammogram JulDocument4 pagesMeng Mammogram JulLivia MillNo ratings yet
- Child Case History FDocument6 pagesChild Case History FSubhas RoyNo ratings yet
- Starters Flash CardsDocument28 pagesStarters Flash CardsNara GarridoNo ratings yet
- Low Voltage Fixed and Automatic Power Factor Correction SystemsDocument6 pagesLow Voltage Fixed and Automatic Power Factor Correction Systemszabiruddin786No ratings yet
- Teleperformance Global Services Private Limited: Full and Final Settlement - December 2023Document3 pagesTeleperformance Global Services Private Limited: Full and Final Settlement - December 2023vishal.upadhyay9279No ratings yet
- Work of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityDocument10 pagesWork of Asha Bhavan Centre - A Nonprofit Indian Organisation For Persons With DisabilityAsha Bhavan CentreNo ratings yet
- EE2401 Power System Operation and ControlDocument93 pagesEE2401 Power System Operation and ControlPrasanth GovindarajNo ratings yet
- Lesson 4: Health and Fitness AdvertisingDocument4 pagesLesson 4: Health and Fitness AdvertisingCatherineNo ratings yet
- Food Safety PosterDocument1 pageFood Safety PosterMP CariappaNo ratings yet
- House of Candy PresentationDocument42 pagesHouse of Candy PresentationRohit JaroudiyaNo ratings yet
- Sikadur 42 HSDocument2 pagesSikadur 42 HSthe pilotNo ratings yet
- Region Iii - Central Luzon Padapada National High SchoolDocument2 pagesRegion Iii - Central Luzon Padapada National High SchoolRotipNo ratings yet
- NASA ISS Expedition 2 Press KitDocument27 pagesNASA ISS Expedition 2 Press KitOrion2015No ratings yet
- Upper Limb OrthosesDocument29 pagesUpper Limb OrthosesMaryam KhalidNo ratings yet
- ATR4518R6v07: Antenna SpecificationsDocument2 pagesATR4518R6v07: Antenna Specificationsanna.bNo ratings yet
- Chef Basics Favorite RecipesDocument58 pagesChef Basics Favorite Recipesbillymac303a100% (2)
- TFU-Risk Assessment RA-11 - Use of Grooving & Threading MachinesDocument1 pageTFU-Risk Assessment RA-11 - Use of Grooving & Threading Machinesarshin wildanNo ratings yet
- Practice Test For Exam 3 Name: Miguel Vivas Score: - /10Document2 pagesPractice Test For Exam 3 Name: Miguel Vivas Score: - /10MIGUEL ANGELNo ratings yet
- Clinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants - UpToDateDocument42 pagesClinical Features, Evaluation, and Diagnosis of Sepsis in Term and Late Preterm Infants - UpToDatedocjime9004No ratings yet
- Minerals and Resources of IndiaDocument11 pagesMinerals and Resources of Indiapartha100% (1)
- Soft Tissue SarcomaDocument19 pagesSoft Tissue SarcomaEkvanDanangNo ratings yet
- Design and Details of Elevated Steel Tank PDFDocument10 pagesDesign and Details of Elevated Steel Tank PDFandysupaNo ratings yet