Professional Documents
Culture Documents
Occular Complications Following Dental Local Anesthesia
Uploaded by
Bunga Erlita RosaliaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Occular Complications Following Dental Local Anesthesia
Uploaded by
Bunga Erlita RosaliaCopyright:
Available Formats
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
Journal section: Oral Surgery Publication Types: Review
doi:10.4317/medoral.17078 http://dx.doi.org/doi:10.4317/medoral.17078
Occular complications following dental local anesthesia
Jose-Maria Aguado-Gil 1, Cristina Barona-Dorado 2, Juan-Carlos Lillo-Rodrguez 3, David-Sebastian De la Fuente-Gonzlez 4, Jose-Maria Martnez-Gonzlez 5
DDSSpmSyImpyUv Dentist. Masters degree in Dental Sciences. Student in the Masters program in Oral Surgery and Implantology at the University Hospital of Madrid 2 Associate Professor of Oral Surgery. School of Dentistry. Complutense University of Madrid 3 Dentist. Assistant Director of the Masters program in Oral Surgery and Implantology. University Hospital of Madrid 4 Dentist. Collaborating Professor. School of Dentistry. Complutense University of Madrid 5 Professor of Maxillofacial Surgery. School of Dentistry. Complutense University of Madrid. Head of the Department of Oral Surgery and Implantology. University Hospital of Madrid
1
Correspondence: School of Dentistry Pza Ramn y Cajal s/n Madrid, Spain hospimar@hotmail.com
Aguado-Gil JM, Barona-Dorado C, Lillo-Rodrguez JC, De la FuenteGonzlez DS, Martnez-Gonzlez JM. Occular complications following dental local anesthesia. Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
http://www.medicinaoral.com/medoralfree01/v16i5/medoralv16i5p688.pdf Article Number: 17078 http://www.medicinaoral.com/ Medicina Oral S. L. C.I.F. B 96689336 - pISSN 1698-4447 - eISSN: 1698-6946 eMail: medicina@medicinaoral.com Indexed in: Science Citation Index Expanded Journal Citation Reports Index Medicus, MEDLINE, PubMed Scopus, Embase and Emcare Indice Mdico Espaol
Received: 27/04/2010 Accepted: 21/05/2010
Abstract
Objective: To determine the frequency of appearance and the factors most commonly associated with ocular complications following dental local anesthesia, also establishing the location and type of anesthesia used. Study Design: An indexed search in the Pubmed and Compludoc databases was carried out with the keywords oral anesthesia, ocular, ophthalmologic, damage, complications, injection. We established a limitation that the literature had to have been published after the year 1970. A total of 19 articles were obtained, forming a total sample of 37 patients. The patients sex, age, nerve anesthetized, type of anesthetic used, ophthalmological complication present, recovery time, treatment and side effects were analyzed. Results: There is a higher involvement of females (77%). The average age was 34.2 years. There was no preference for an anesthetic technique. Diplopia was the most common complication (65%), which coincides with the data from other authors. Almost all of the complications were of a temporary nature, with an average recovery time of 68 minutes. Conclusions: This is one of the few studies of its kind in dental literature, it thus being difficult to make precise conclusions. Ophthalmological complications are seldom a problem, diplopia being the most common among them. The authors appear to indicate an intravascular injection of the anesthetic as the cause of the problem, and therefore, it should be avoided in order to prevent accidents at the ocular level. Key words: Accidents, ophthalmology, dental anesthesia.
e688
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
Introduction
For many years, dental literature describes signs and symptoms at the ophthalmic level following injection of anesthesia into the oral cavity, both in regional techniques at a superior level, due to the proximity with the orbital region, as well as in the mandibular blocking of the inferior dental nerve. The main complications that may occur in regards to intraoral anesthesia may include: temporary diplopia, transitory unilateral amaurosis, strabismus due to paralysis of the extrinsic muscles of the eye, and palpebral ptosis. To date, the mechanism that produces such complications is unclear, although the authors suggest an intravascular injection of the anesthetic, which would follow a retrograde path towards the infraorbital artery or the middle meningeal artery. Despite being described as a local type of complication of anesthesia, the ocular alterations are quite uncommon, representing approximately 0.1% of the complications. The purpose of this study was to determine the ocular complications the appear most frequently following administration of dental local anesthesia, seeking to determine the relationship with a certain common factor or variable, as well as the presence of such complications according to the anesthetic technique and type of anesthetic used, and finally, to determine the duration of the ocular complications.
tion present in each case was recorded. The accompanying signs present were also noted. 4. Technique: the p patients were distinguished according to whether the anesthesia was administered on the inferior dental nerve (IDN) or on the posterior superior alveolar nerve (PSAN). 5. Anesthetic: yp both the type of anesthetic and its concentration (in %) has been described, as well as the vasoconstrictor used and in what proportion. 6. Recovery time: expressed in minutes or hours. 7. Treatment carried out by the professional at the time that the ocular alteration occurs. 8. Side effects: if any complications remain after the time for recovering sensitivity after anesthesia.
Results
Study Design
An indexed search in the Pubmed and Compludoc databases was carried out with the keywords oral anesthesia, ocular, ophthalmologic, damage, complications, injection. As inclusion criteria, we took into consideration that there had to be at least one case described of an ocular alteration following some type of anesthetic procedure carried out in the mouth; and that each and every one of the following variables was taken into account in the description of the case: age and sex of the patient, type and location of the anesthesia, main complication present and accompanying symptoms, duration of the event, treatment applied and whether or not the patient experienced any side effects. The search was limited to articles published after 1970. With these criteria, we obtained a total of 22 articles (Table 1), considering in each and every one of them the variables that are described as follows, forming a total sample of 35 patients (1-19). The method used consisted of a descriptive statistical analysis of the following variables: 1. Sex: male (M) or female (F), in percentage and ratio. 2. Age: the exact age of each patient described in each article was used, after which the different statistical variables within this section were calculated. 3. Ophthalmological pmmpmp complication: the ocular complicae689
Sex: Of the 35 cases selected, 7 affected males (20%) and 28 affected females (80%), which results in a F/M ratio of 4:1. Age: The average age of the patients included in the meta-analysis was 29.5 years old. The mean of the distribution of the data, 32 years, and the mode, which repeats on 3 occasions, is 25 years old. The range of age is from 4 to 73 years old (Fig. 1). The age interval with the highest number of patients was from 20-29 years old. Anesthetic technique: a technique was practiced on the posterior superior alveolar nerve in 19 patients and a direct mandibular block was administered in 15 patients, as well as a case in which both techniques were practiced. Ocular complication: The most common ocular complication was diplopia, present in 23 cases (66%), followed by palpebral ptosis in 12 cases (34%), midriasis in 5 cases (14%), unilateral transitory amaurosis and blurry vision in 4 patients (11%) and Horner syndrome and strabismus, affecting 9% and 6% of the patients, respectively (Fig.2). Other ocular complications, which are not included in the table due to being very uncommon, were ophthalmoplegia, myosis and sudden blackout, all present in a single case (3%), along with permanent amaurosis. In terms of other signs and associated symptoms, the following is worth noting: ischemia or paleness of the area, which was present in 7 of the patients; numbing of the periorbital area and burning of the eye, both present in three patients. Recovery time: The range of recovery time varied from 10 minutes to 24 hours. The average time was 63 minutes. For the calculation, the only case in which recovery from the side effects did not occur was not taken into account, nor was the case of 24 hours, due to being very far from the rest of the results, which would significantly modify the data. Thus, only 33 of the 35 patients were taken into account when calculating the recovery time (Fig. 3).
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
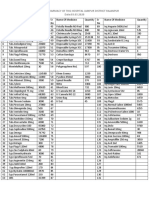
Table 1. Articles and selected cases. Variables analyzed.
AUTHOR Rood JP (1) (1972) Campbell RL (2) (1979) Petrelli EA (3) (1980) Norris L (4) (1982) Goldenberg AS (5) (1983) Kronman JH (6) (1984) Clarke JR (7) (1987) Goldenberg A (8) (1990) Dryden JA (9) (1993) Marinho R (10) (1995) Van der Bijl P (11) (1996) Spierer A (12) (1999)
NO. CASES 1 1 1 1 1 1 1 1 1 1 1 2
SEX F F F F F F F F F M F F M F F M F F F F F F M F F F F M F M F F M F F
AGE 24 34 42 17 58 37 10 31 33 25 14 5 4 65 29 53 49 60 25 24 32 22 35 40 73 65 40 45 33 73 20 21 25 30 28
OCCULAR COMPLICATION Ptosis, diplopia Ptosis, myosis Diplopia Diplopia Diplopia, strabismus and unilateral transitory amaurosis Diplopia Unilateral transitory amaurosis and diplopia Diplopia, blurred vision Diplopia and ptosis Diplopia Diplopia Diplopia, strabismus Ptosis Palpebral ptosis, Enophthalmos, Myosis Palpebral ptosis, Enophthalmus, Myosis Palpebral ptosis, Enophthalmus, Myosis Diplopia, ptosis, mydriasis Diplopia, ptosis, mydriasis Diplopia, ptosis, mydriasis Diplopia Diplopia Diplopia Diplopia Diplopia Diplopia Diplopia Diplopia Unilateral transitory amaurosis, mydriasis, ptosis, diplopia Blurred vision Permanent amaurosis, midriasis Blurred vision Blurred vision Burning sensation in the eye Unilateral transitory amaurosis Diplopia
TECHNIQUE IDN IDN PSAN IDN IDN PSAN PSAN PSAN IDN PSAN IDN IDN IDN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN PSAN IDN IDN IDN, PSAN IDN IDN IDN IDN IDN
TIME (min.) 45 120 90 20 20 50 30 180 90 180 1440 15 20 50 20 40 45 30 60 30 45 60 90 120 120 50 30 30 45 Perm 15 15 20 45 120
Pearrocha M (13) (2000)
14
Wilkie GJ (14) (2000) Webber B (15) (2001) Rishiraj B (16) (2005) Ngeow WC (17) (2006) Uckan S (18) (2006) Scott JK (19) (2007)
1 1 1 2 2 1
e690
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
Age
10 8 6 4 2 0 0�9� 10�19� 20�29� 30�39� 40�49� 50�59� 60�69� 70�79� years years years years years years years years
Fig. 1. Distribution of the patients according to their age group.
Primary�occular�complication
70% 60% 50% 40% 30% 20% 10% 0% DP PT MD AUT VB SH EST
Fig. 2. Percentage of patients according to the ocular complication presented. Diplopia (DP), Ptosis (PT), Mydriasis (MD), Unilateral Transitory Amaurosis (AUT), Blurred Vision (VB), Horner Syndrome (SH), Strabismus (EST).
Recovery�time
25 20 15 10 5 0 10�60�minutes 90�120�minutes 3�5�hours 24�hours
Fig. 3. Distribution of the patients according to their recovery time after the ocular complication.
Discussion
As aforementioned, ocular complications are an uncommon problem. Although there were authors that suggested a frequency of 0.1%, if a calculation is made based on the studies by Meyer (1999), who estimated ten years ago that there were 30 million cases in which anesthesia
e691
was administered in Germany each year, we would be talking about one case of an ocular accident for every 500 million or 1 billion cases in which patients are administered anesthesia, which clearly indicates that these alterations are very uncommon. However, that does not mean that they do not occur, which requires researching the causes that may lead to these events, as well as their mechanism of production. Although the latter is not yet clear, all of the authors appear to suggest an intravascular injection of the anesthetic in the cases of troncular anesthesia of the inferior dental nerve, which would follow a retrograde mechanism until reaching the medium meningeal artery, through which it would connect with the lacrimal artery. In the case of anesthesia of the superior posterior alveolar nerve, this refers to diffusion to the orbit from the infratemporal and pterygopalatine fossa (13). This may be based, above all, on the troncular blocks of the maxillary nerve through the posterior palatine duct, as in the study by Sved et al. (20), carried out on 101 patients on whom this anesthetic technique was applied, up to 39% of the cases presented some type of ocular alteration, although they only speak of 8% of the cases in which an aspiration of blood in the anesthetic carpule was noted. In terms of the sex of the patients, in our study, 77% of the cases affected females, which represents a large difference with respect to males. This data coincides with the data obtained by Pearrocha et al. (13), in the study which we also took into account for our meta-analysis. Due to not having more articles which consider more than 2 or 3 cases, there is no study that contradicts these results, but in general, we can affirm that there is a higher inclination towards females. With respect to age, the average age obtained was 34.2 years old, as well as a more common presentation in the 3rd and 4th decades of life. According to the studies conducted by Pearrocha et al. (13), they obtained a higher average age (44 years old); although they concur that this phenomenon occurs most frequently during the 3rd decade of life. The average age of the patients of our study is influenced by the 2 cases that occurred at the dental pediatric level, although we also take into account the cases of patients over the age of 65, thus making our data rather objective. In regards to the ocular complication most frequently described, the results are similar, with these authors indicating diplopia due to the paralysis of the extrinsic muscles of the eye as the most common complication that occurs at the ophthalmological level. Our data is also corroborated by Sved et al. (20), who spoke in their aforementioned study of diplopia as the most common complication, following by strabismus and ptosis. Palpebral ptosis, present in 3 cases studied by Pearrocha et al. (13) as a syndrome similar to Horner, which concurs with our observation that it is the second most
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
common complication. The aforementioned mechanism of the possible retrograde passing or diffusion of the anesthetic will most commonly affect the III, IV and VI par than the optical nerve, due to its path closest to the place of injection, which generates the paralysis that causes double vision. With respect to the nerve anesthetized, our data reveals a very slight difference in terms of the anesthetic technique on the inferior dental nerve and on the posterior alveolar nerve, with a slight inclination towards the latter. These data are contrasted by that shown by Pearrocha et al. (13), who exclusively name the superior periapical anesthesia on the posterior alveolar nerve. Whereas there are authors that recommend the retrograde path of anesthetic by intravascular injection on the inferior dental artery, up to the medium meningeal artery and the connecting of this artery with the lacrimal artery, an anastomosis always appears between both, which enables the relationship between the arterial plexus of the medium meningeal and the ophthalmic artery (4, 11-12); others (3,7) suggest a connection at the pterygomaxillary fossa, where the anesthetic would penetrate into the pterygoid venus plexus, being distributed to the ophthalmic vein at its connection in the orbital fissure. With the data that we have obtained in this study, we are unable to establish some clear conclusions on whether the mechanism of production is the first or the second, or whether both may be involved in the development of ocular complications. However, this does not concur with that described by authors such as Dryden et al. (9), in whose case they refer an infiltration with negative aspiration after using a Gow-Gates technique. This only serves to show the lack of unanimity in these mechanisms of producing the complications. The anesthetic most often used was articain 2% with epinephrine 1:100,000, used on 35% of the patients. Despite this, this data does not appear entirely conclusive, as anesthesia has been practiced with many types of anesthetics (lidocain, mepivacain, procain, etc.) with ocular alterations present in the use of all of them. In addition, we must keep in mind that articain is currently one of the most commonly used anesthetics. Our study also coincided that the total of the ocular complications corresponds with that of the study conducted by Pearrocha et al. (13), knowing the dedication of this group to the field of oral surgery, where the use of this anesthetic is even more frequent due to its higher plasma half-life and duration of the anesthetic effect. The usual recovery time of these accidents was 70 minutes, although more than 60% of the patients recovered within the first hour. This concordance in our results is also evident in the study by Pearrocha et al. (13). As has already been explained in the results, the only case of a permanent complication was not taken into account. With respect to the this case, Rhisiraj et al. (16)
e692
state that it had to do with a patient who suffered a serious systemic alteration (andocarditis of the mitral valve due to S. salivarius, awaiting substitution), which may have played a role in producing this episode, as the only case of permanent amaurosis or that of any other type of permanent alteration after injection of local anesthesia was found in dental science publications. In the majority of the cases of diplopia, the affected eye was covered for the duration of the symptom in order to prevent the patient from suffering the strain of double vision. Despite all of this, in the majority of the cases, dental treatment was continued with the mere observation and care of the patient. In certain cases, the patient was advised to visit the ophthalmologist if the symptoms were not relieved within a few hours, although the symptoms were always relieved within this time, except in the case of permanent blindness, in which ocular massage was even attempted. The main limitation of our study was not having more articles in which various cases of ocular complications are contemplated so that we could establish a broader and more in-depth comparison of the results, which would have enabled us to make specific and clear conclusions. We believe that it would be interesting for the authors to publish this type of experience encountered in the dental clinic, in order to conduct an exhaustive study on the mechanisms of production of the ocular complications, enabling the researchers to establish some protocols for preventing them, which, in turn, would result in better quality and comfort in treating our patients, given that oral anesthesia is probably the most common procedure practiced by stomatologists and dentists in their daily work, and these complications may lead to uncomfortable and unpleasant situations when treating the patients. The best way of avoiding the appearance of complications, both ocular as well as clinical, is to examine the patient and use a careful and correct technique, especially being careful to avoid intravascular injection of the anesthetic. In the event that such a complication does occur, the most important step is to calm the patient. In cases of diplopia, it is recommended to cover the patients affected eye in order to prevent the unpleasant sensation of double vision (21).
References
References with links to Crossref - DOI
1. Rood JP. Ocular complication of inferior dental nerve block. A case report. Br Dent J. 1972;132:23-4. 2. Campbell RL, Mercuri LG, Van Sickels J. Cervical sympathetic block following intraoral local anesthesia. Oral Surg Oral Med Oral Pathol. 1979;47:223-6. 3. Petrelli EA, Steller RE. Medial rectus muscle palsy after dental anesthesia. Am J Ophthalmol. 1980;90:422-4. 4. Norris L. Eye complications following Gow-Gates block technique. Dent Anaesth Sedat. 1982;11:59-60. 5. Goldenberg AS. Diplopia resulting from a mandibular injection. J Endod. 1983;9:261-2.
Med Oral Patol Oral Cir Bucal. 2011 Aug 1;16 (5):e688-93.
Occular alterations in anesthesia
6. Kronman JH, Kabani S. The neuronal basis for diplopia following local anesthetic injections. Oral Surg Oral Med Oral Pathol. 1984;58:533-4. 7. Clarke JR, Clarke DJ. Hysterical blindness during dental anaesthesia. Br Dent J. 1987;162:267. 8. Goldenberg AS. Transient diplopia from a posterior alveolar injection. J Endod. 1990;16:550-1. 9. Dryden JA. An unusual complication resulting from a Gow-Gates mandibular block. Compendium. 1993;14:94,96,98. 10. Marinho RO. Abducent nerve palsy following dental local analgesia. Br Dent J. 1995;179:69-70. 11. Van der Bijl P, Lamb TL. Prolonged diplopia following a mandibular block injection. Anesth Prog. 1996;43:116-7. 12. Spierer A, Spierer S. Transient extraocular muscle palsy resulting from inferior alveolar nerve block in children. J Clin Pediatr Dent. 1999;24:29-30. 13. Pearrocha-Diago M, Sanchis-Bielsa JM. Ophthalmologic complications after intraoral local anesthesia with articaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:21-4. 14. Wilkie GJ. Temporary uniocular blindness and ophthalmoplegia associated with a mandibular block injection. A case report. Aust Dent J. 2000;45:131-3. 15. Webber B, Orlansky H, Lipton C, Stevens M. Complications of an intra-arterial injection from an inferior alveolar nerve block. J Am Dent Assoc. 2001;132:1702-4. 16. Rishiraj B, Epstein JB, Fine D, Nabi S, Wade NK. Permanent vision loss in one eye following administration of local anesthesia for a dental extraction. Int J Oral Maxillofac Surg. 2005;34:220-3. 17. Ngeow WC, Shim CK, Chai WL. Transient loss of power of accommodation in 1 eye following inferior alveolar nerve block: report of 2 cases. J Can Dent Assoc. 2006;72:927-31. 18. Uckan S, Cilasun U, Erkman O. Rare ocular and cutaneous complication of inferior alveolar nerve block. J Oral Maxillofac Surg. 2006;64:719-21. 19. Scott JK, Moxham BJ, Downie IP. Upper lip blanching and diplopia associated with local anaesthesia of the inferior alveolar nerve. Br Dent J. 2007;202:32-3. 20. Sved AM, Wong JD, Donkor P, Horan J, Rix L, Curtin J, et al. Complications associated with maxillary nerve block anaesthesia via the greater palatine canal. Aust Dent J. 1992;37:340-5. 21. Crean SJ, Powis A. Neurological complications of local anaesthetics in dentistry. Dent Update. 1999;26:344-9.
e693
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Peripheral Vascular Disease Arteries NHSDocument10 pagesPeripheral Vascular Disease Arteries NHSAdahl HetheringtonNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Patient Referral PDFDocument6 pagesPatient Referral PDFBunga Erlita RosaliaNo ratings yet
- Manage Odontogenic Infections Stages Severity AntibioticsDocument50 pagesManage Odontogenic Infections Stages Severity AntibioticsBunga Erlita RosaliaNo ratings yet
- Acupoint Sensitization, Acupuncture Analgesia, Acupucnture On Visceral Functional Disorders and Its MechanismDocument138 pagesAcupoint Sensitization, Acupuncture Analgesia, Acupucnture On Visceral Functional Disorders and Its MechanismElizabeth Neil100% (1)
- Principles and Practice of Gynecologic Oncology: Handbook ForDocument288 pagesPrinciples and Practice of Gynecologic Oncology: Handbook ForPeter Osundwa KitekiNo ratings yet
- Test 2Document15 pagesTest 2Ding DialyzerNo ratings yet
- Comparative Health Information Management 4th Edition Peden Solutions Manual DownloadDocument15 pagesComparative Health Information Management 4th Edition Peden Solutions Manual DownloadVickie Montejo100% (28)
- Flexible Partial DentureDocument5 pagesFlexible Partial DentureDeasireeNo ratings yet
- NCP OsteoarthritisDocument4 pagesNCP OsteoarthritisKyle Margaret Flores100% (1)
- National Guidelines For Screening of Hypothyroidism During PregnancyDocument48 pagesNational Guidelines For Screening of Hypothyroidism During PregnancyManish Chandra PrabhakarNo ratings yet
- Dry Socket-Risk FactorDocument17 pagesDry Socket-Risk FactorBunga Erlita RosaliaNo ratings yet
- Interceptiveorthodontics 111013083234 Phpapp02Document62 pagesInterceptiveorthodontics 111013083234 Phpapp02Bunga Erlita RosaliaNo ratings yet
- Diagnosisandtreamentplanninginfpd 131209082046 Phpapp01Document104 pagesDiagnosisandtreamentplanninginfpd 131209082046 Phpapp01Bunga Erlita RosaliaNo ratings yet
- Local Anaesthetic: A Guide For Parents and ClientsDocument0 pagesLocal Anaesthetic: A Guide For Parents and ClientsBunga Erlita RosaliaNo ratings yet
- Spread of Odontogenic InfectionDocument2 pagesSpread of Odontogenic InfectionBunga Erlita RosaliaNo ratings yet
- Terminology: Bridge (FPD)Document14 pagesTerminology: Bridge (FPD)Bunga Erlita RosaliaNo ratings yet
- FPD Lecture 2009-2Document16 pagesFPD Lecture 2009-2Nikola DerebanNo ratings yet
- Cases Journal: Swallowed Dental Bridge Causing Ileal Perforation: A Case ReportDocument3 pagesCases Journal: Swallowed Dental Bridge Causing Ileal Perforation: A Case ReportBunga Erlita RosaliaNo ratings yet
- Spread of Odontogenic InfectionDocument2 pagesSpread of Odontogenic InfectionBunga Erlita RosaliaNo ratings yet
- Introducing Dental Local Anaesthesia Using A Standardized Cognitive Behavioural TechniqueDocument15 pagesIntroducing Dental Local Anaesthesia Using A Standardized Cognitive Behavioural TechniqueBunga Erlita RosaliaNo ratings yet
- Final Handout For SplintingDocument7 pagesFinal Handout For SplintingBunga Erlita RosaliaNo ratings yet
- Severe Odonto Genic Infections Part 1Document11 pagesSevere Odonto Genic Infections Part 1Bunga Erlita RosaliaNo ratings yet
- Syncope ShockDocument39 pagesSyncope ShockBunga Erlita RosaliaNo ratings yet
- 2011 Abstracts 57 No - 6 - Dec JanDocument3 pages2011 Abstracts 57 No - 6 - Dec JancoklatstrawberryNo ratings yet
- Pa Tho Genesis and Management of Dry SocketDocument4 pagesPa Tho Genesis and Management of Dry SocketNina AbdulNo ratings yet
- Contraindications To Vasoconstrictors in Dentistry: Part IIDocument5 pagesContraindications To Vasoconstrictors in Dentistry: Part IIBunga Erlita RosaliaNo ratings yet
- Local Anesthesia: Local and Systemic ComplicationsDocument6 pagesLocal Anesthesia: Local and Systemic ComplicationsBunga Erlita RosaliaNo ratings yet
- Guideline On Use of Local Anesthesia For Pediatric Dental PatientsDocument7 pagesGuideline On Use of Local Anesthesia For Pediatric Dental PatientsyoelianibudisidhartaNo ratings yet
- Management Of: Hypovolaemic ShockDocument58 pagesManagement Of: Hypovolaemic ShockZawawi Ibnu RosyidNo ratings yet
- Pa Tho Genesis and Management of Dry SocketDocument4 pagesPa Tho Genesis and Management of Dry SocketNina AbdulNo ratings yet
- Local Anesthesia: Local and Systemic ComplicationsDocument6 pagesLocal Anesthesia: Local and Systemic ComplicationsBunga Erlita RosaliaNo ratings yet
- Zinc Deficiency and Clinical Practice PDFDocument6 pagesZinc Deficiency and Clinical Practice PDFBunga Erlita RosaliaNo ratings yet
- Effects of Zinc-Deficiency On Oral and Periodontal Diseases in RatsDocument6 pagesEffects of Zinc-Deficiency On Oral and Periodontal Diseases in RatsBunga Erlita RosaliaNo ratings yet
- Gambaran Radiografik Pasca Pencabutan Gigi PDFDocument1 pageGambaran Radiografik Pasca Pencabutan Gigi PDFBunga Erlita RosaliaNo ratings yet
- Causes and prevention of ledging and blockages in root canalsDocument19 pagesCauses and prevention of ledging and blockages in root canalsBunga Erlita RosaliaNo ratings yet
- Chapter 5 - Oral Surgery PDFDocument49 pagesChapter 5 - Oral Surgery PDFBunga Erlita RosaliaNo ratings yet
- The Residency Towers: 15 - 16 SeptemberDocument10 pagesThe Residency Towers: 15 - 16 SeptembervamshidhNo ratings yet
- Cosmos PresentationDocument27 pagesCosmos Presentationmaher.suliemanNo ratings yet
- Asperger's Syndrome Definition and CharacteristicsDocument2 pagesAsperger's Syndrome Definition and CharacteristicsSamakab MohamedNo ratings yet
- Diagnosis of cow milk allergy in infants and childrenDocument2 pagesDiagnosis of cow milk allergy in infants and childrenMaya FikriNo ratings yet
- For Printing Grand Case Group1Document37 pagesFor Printing Grand Case Group1Joco Bordeos AripNo ratings yet
- Available Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Document2 pagesAvailable Medicine at Pharmacy of THQ Hospital Jampur District Rajanpur Date:03.03.2020Kashif AhmadNo ratings yet
- Amniotic Fluid EmbolismDocument10 pagesAmniotic Fluid EmbolismRebecca ApeladoNo ratings yet
- KNGF Guideline For Physical Therapy Cardiac Rehabilitation FlowchartDocument3 pagesKNGF Guideline For Physical Therapy Cardiac Rehabilitation FlowchartXulkanain ZENo ratings yet
- JOSPT Anthony Delitto (2012)Document57 pagesJOSPT Anthony Delitto (2012)Bruno RechNo ratings yet
- Western Medical SystemDocument9 pagesWestern Medical Systemlorelyn panisNo ratings yet
- PsyHx and MSEDocument25 pagesPsyHx and MSERazel AnneNo ratings yet
- Questionsheet 1: Disease / Immunology A2.15Document6 pagesQuestionsheet 1: Disease / Immunology A2.15Nabindra RuwaliNo ratings yet
- Evaluascdc Hiv MethodDocument11 pagesEvaluascdc Hiv MethodmasaruddinNo ratings yet
- A Day in Occupational Therapy Analice BurdDocument5 pagesA Day in Occupational Therapy Analice Burdapi-518311936No ratings yet
- Melatonin Agonists A Brief Clinical ReviewDocument6 pagesMelatonin Agonists A Brief Clinical ReviewgeoaislaNo ratings yet
- Grade 10 Disaster Management Project Pocket Guide On First AidDocument6 pagesGrade 10 Disaster Management Project Pocket Guide On First AidSweta JainNo ratings yet
- National Minimum Prevention MPPI GuideDocument20 pagesNational Minimum Prevention MPPI GuideEmmanuel Umo EffiongNo ratings yet
- Brosur - Ageloc Youth enDocument20 pagesBrosur - Ageloc Youth enLidya ZhuangNo ratings yet
- Navrekar - LWM PPT For Workshop 16 JulyDocument40 pagesNavrekar - LWM PPT For Workshop 16 JulyQudratullah ShaikNo ratings yet
- Vitamin K: Adjunct To Vitamin DDocument7 pagesVitamin K: Adjunct To Vitamin DBeena WalvekarNo ratings yet
- A Mathematical Model For Analysis of The Cell Cycle in Human TumoursDocument24 pagesA Mathematical Model For Analysis of The Cell Cycle in Human TumoursObetz ClNo ratings yet
- 10 Best Homeopathic Medicines For AcneDocument13 pages10 Best Homeopathic Medicines For AcneAyeshik ChakrabortyNo ratings yet
- Nephrotic SyndromeDocument61 pagesNephrotic SyndromeRanah Julia Garchitorena AyoNo ratings yet