Professional Documents
Culture Documents
Respiratory Distress in A Newborn Baby: Slide RD-L
Uploaded by
Alhamid DusOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Distress in A Newborn Baby: Slide RD-L
Uploaded by
Alhamid DusCopyright:
Available Formats
NNF Teaching Aids:Newborn Care
Respiratory distress in a newborn baby
Slide RD-l Introduction
Respiratory distress in a newborn is a challenging problem. It accounts for significant morbidity and mortality. It occurs in 4 to 6 percent of neonates. Many of the conditions causing respiratory distress are preventable. Early recognition and prompt management are required. A few may need ventilatory support but this treatment is often not available and when available may be expensive.
Slide RD-2 Tachypnea vs respiratory distress
It is important to recognise the difference between tachypnea and respiratory distress. Tachypnea alone means an increased respiratory rate of >60/min in a quiet resting baby. Respiratory rate should not be counted immediately after feeds. It should be counted in a calm child retractions and grunting. The usual manifestations of respiratory distress would include tachypnea, retractions and grunting. Central cyanosis, lethargy and poor feeding may also appear. for full one minute. Distress indicates more severe form of respiratory disease and it is associated with
Slide RD-3 Causes of respiratory distress
Pulmonary disease is the most common cause of respiratory distress. But non pulmonary problems can also manifest with respiratory distress. These include cardiac (congenital heart disease, myocardial dysfunction) neurologic (asphyxia, intracranial bleed) and metabolic (hypoglycemia, acidosis).
NNF Teaching Aids:Newborn Care
Slide RD-4, 5 Causes of respiratory distress
Respiratory distress in a newborn could be caused either by surgical or medical conditions. The common medical conditions are Respiratory distress syndrome (RDS), Meconium aspiration syndrome (MAS), Transient tachypnea of newborn (TTNB), pneumonia, aspiration, pulmonary hypertension, delayed adaptation, asphyxia and acidosis. Surgical conditions would include Pneumothorax, Diaphragmatic hernia, Tracheo esophageal fistula (aspiration), Pierre Robin Syndrome (upper airway obstruction due to glossoptosis), Choanal atresia and Lobar emphysema.
Slide RD-6 History
While stabilizing a baby with severe respiratory distress, it is important to get a good history. We need to know the gestation and if the baby is premature it is important to know if antenatal steroids have been given or not. A history to determine the source of infection would include history of premature rupture of membranes (PROM), if onset of distress is early. Again in early onset distress one should find out the Apgar score and history of meconium stained liquor. The importance of determining the time of onset of distress needs to be emphasized, as this may vary depending upon the etiology . It is important to know about the feeding problems. Feeding problems could be present in a severely distressed baby. If feeding problems are present such as choking or aspiration during a feed, one could think of aspiration pneumonia as a possibility.
Slide RD-7 Examination
To assess the severity of the distress the scoring system given in Table 1 could be used. Clinical monitoring is most important. An increasing score is more important than just an increase in rate. It is also important to distinguish between tachypnea and respiratory distress. Tachypnea is usually characteristic of a disease like transient tachypnea of newborn. Cardiac conditions and acidosis also usually manifest with tachypnea but could progress on to distress.
NNF Teaching Aids:Newborn Care
Slide RD-8 Assessment of respiratory distress
Table 1: Score for respiratory distress
Score 0 Resp. rate Central cyanosis Retractions Grunting Air Entry <60 None None None Good 1 60-80 None with 40% FiO2 Mild Minimal Decreased 2 >80 Need >40% FiO2 Severe Obvious Very poor
A score of greater than 6 would indicate severe respiratory distress.
Slide RD-9 Chest examination
Examination of the chest could be helpful in diagnosing the etiology. In MAS, the chest is hyperinflated. Air entry is usually decreased in severe RDS. Mediastinal shift could occur in pneumothorax or diaphragmatic hernia. Distant heart sounds could give a clue to the diagnosis of pneumothorax.
Slide RD-10 Approach in preterm
In a preterm baby, early onset respiratory distress which is progressive is invariably due to RDS. However, if distress is transient, asphyxia, hypoglycemia and hypothermia could contribute. Other causes of distress which occur in term babies could also occur in preterm babies, but the most common and important cause in pre term babies is RDS. Pneumonia could present at anytime after birth.
Slide RD-11 Approach in term
In term babies etiology could differ depending on the time of onset of distress. If the baby has tachypnea beginning at birth the causes could be TTNB or secondary to polycythemia. If the distress begins early but is more severe it may be due to MAS, pneumonia, asphyxia or malformations.
NNF Teaching Aids:Newborn Care
If the distress occurs at the end of first week or later the cause would be most probably pneumonia. Presence of a cleft palate, history of a choking episode could indicate aspiration pneumonia. If however the baby has hepatomegaly or is in shock one needs to think of a cardiac cause. On the other hand if the baby is dehydrated and in shock, a possibility of metabolic acidosis needs to be considered.
Slide RD-12 Suspect surgical cause
We need to suspect surgical conditions if there are any obvious malformations (cleft palate, micrognathia) or if there is a scaphoid abdomen (diaphragmatic hernia) . Presence of frothing or history suggestive of aspiration may give a clue to the presence of a tracheo-esophageal fistula (TEF). Worsening of condition during resuscitation at birth by bag and mask ventilation -think of diaphragmatic hernia.
The common malformations/surgical conditions which could present in the neonatal period include TEF, diaphragmatic hernia, lobar emphysema, choanal atresia and cleft palate. It is important to recognize these conditions early as immediate referral and appropriate management would improve prognosis. A baby with suspected TEF should not be fed and a baby with suspected diaphragmatic hernia should not be resuscitated with bag and mask.
Slide RD- 13,14 Investigations
Investigations would obviously depend on the possible etiology. If PROM is present one should look for polymorphs in the gastric aspirate. The first gastric aspirate should be used for this test and the aspirate should be clear. Shake test is a simple bedside test and should be done in preterm babies with respiratory distress. The gastric aspirate (0.5 ml) is mixed with 0.5 ml of absolute alcohol in test tube. This is shaken for 15 sec. and allowed to stand for 15 minutes. A negative shake test i.e. no bubbles or bubbles covering less than 1/3 rd of the rim indicates a high risk of developing RDS and the presence of bubbles at more than 2/3 of the rim indicates lung maturity and decreased risk of developing RDS. Sepsis screen is indicated if infection is suspected. The most important investigation in a neonate with respiratory distress is a chest X-
NNF Teaching Aids:Newborn Care
ray( refer RD-20 ). An arterial blood gas if available is a good adjunct to plan and monitor respiratory therapy.
Slide RD-15 Principles of management
Supportive therapy is most crucial in all neonates with respiratory distress and the same principles apply, whatever the cause. Monitoring is needed in all babies with respiratory distress. Clinical monitoring is most important as sophisticated equipment may not be available. The scoring system could be utilised to monitor babies. An increasing score would indicate worsening distress. All babies with significant distress should be kept on IV fluids ; blood pressure and blood sugar should be maintained. Other measures include oxygen therapy and if available ventilatory support or CPAP (continuous positive airway pressure). Specific therapy is now available for RDS i.e. surfactant, but even with this ventilatory support will be needed.
Slide RD-16, 17 Oxygen therapy
All babies with worsening or severe respiratory distress, with or without cyanosis should get oxygen. Oxygen should be warm and humidified . It can be provided through nasal catheters or preferably through oxygen hood. The flow rate should be 2-5 L/min (40-70% O2) . Oxygen should be used with caution especially in preterm babies. Respect oxygen -it has both good and toxic effects and use it only if needed. Use lower concentration of oxygen to relieve cyanosis or distress. Pulse oximetry is a simple non-invasive method for measuring oxygen saturation. Ideally all neonates with respiratory distress should be monitored using a pulse oximeter and oxygen should be administered if saturations are less than 90%. Aim is to maintain saturation between 90-93% to avoid hyperoxia.
NNF Teaching Aids:Newborn Care
Slide RD-18 Respiratory distress syndrome (RDS)
If a preterm baby has respiratory distress within the first 6 hrs of birth and is cyanosed or needs oxygen to maintain oxygen saturation the diagnosis is RDS unless proved otherwise. X-ray findings would be a reticulo-granular pattern in mild disease and a "white out" picture in severe disease.
Slide RD-19
X-ray showing air bronchogram and hazy lung suggestive of HMD.
Slide RD-20 Pathogenesis
The basic problem in a preterm baby with RDS is surfactant deficiency. Surfactant is needed to decrease alveolar surface tension and keep them open. In a preterm baby, absence of surfactant leads to alveolar collapse during expiration. This affects gas exchange and the baby goes into respiratory failure.
Slide RD-21 Predisposing factors
Predisposing factors include -prematurity, asphyxia and maternal diabetes. Prolonged rupture of membranes (PROM) and intrauterine growth retardation are believed to enhance lung maturity. Drugs such as antenatal steroids enhance lung maturity and can prevent the neonate from developing RDS.
Slide RD-22 Antenatal corticosteroids
Antenatal corticosteroid therapy is a simple and effective therapy that prevents RDS and saves neonatal lives. Antenatal steroids will prevent the occurrence and severity of RDS in preterm babies between 24 and 34 weeks of gestation. Optimal effect of antenatal steroids is seen if delivery occurs after 24 hours of the initiation of therapy. Effect lasts for 7 days. Cases of preterm premature rupture of membrane (PPROM) at less than 32 weeks of gestation (in the absence of clinical chorioamnionitis), maternal hypertension and diabetes are not contra indications for administering antenatal steroids, if delivery is anticipated below 34 weeks of gestation. Dose recommended is Inj
NNF Teaching Aids:Newborn Care
Betamethasone 12 mg 1M every 24 hrs x 2 doses; or Inj Dexamethasone 6 mg 1M every 12 hrs x 4 doses. Multiple courses of antenatal steroids are not beneficial and hence are not recommended Preterm babies below 1 kg and 28 wks gestation should be referred to a suitable Level II NICU after stabilization.
Slide RD-23, 24 Surfactant therapy
It is important to emphasize that surfactant therapy should be instituted only if there are facilities for ventilation. The efficacy of surfactant in reducing the duration of ventilation is proven. The main deterrent to its use is the cost factor. Prophylactic surfactant use is recommended for any neonate< 28 weeks and < 1000 gms. This is not yet a routine practice in India. Rescue therapy is using surfactant in a symptomatic neonate. This could be used in any neonate suspected / diagnosed to have RDS.
Slide RD-25 Meconium aspiration syndrome (MAS)
Babies born through meconium stained liquor could have MAS and aspiration may occur in-utero, during delivery or immediately after birth. Thick meconium could block air passages and cause atelectasis and air leak syndromes.
Slide RD-26
The baby with MAS is usually post-term or small-for-date. There may be meconium staining of the umbilical cord, nails and skin. The chest may be hyperinflated and onset of distress is usually within the first 4-6 hours.
Slide RD- 27
X-ray shows fluffy shadows involving both lungs with hyperinflation as evidenced by pushed down diaphragm.
Slide RD-28 MAS prevention
Immediate management of a baby born through meconium stained liquor is extremely important. Oropharynx should be suctioned before delivery of
NNF Teaching Aids:Newborn Care
shoulders and all babies born through meconium stained liquor who are not vigorous at birth should be intubated and intratracheal suction should be done. However, vigorous and active babies need not undergo intratracheal suctioning. A vigorous baby is defined as one who is breathing, has good muscle tone and heart rate above 100 beats per minute.
Slide RD-29 Transient tachypnea of newborn (TTNB)
Transient tachypnea of the newborn is a benign condition usually seen in term babies born by cesarean section. These babies are well and have only tachypnea with rates as high as 80-100/min. The breathing is shallow and rapid without any significant chest retractions. It occurs because of delayed clearance of lung fluid. Management is supportive and prognosis is excellent.
Slide RD-30
X ray shows clear lung fields with prominent right interlobar fissure with borderline cardiomegaly suggestive of transient tachypnoea of newborn (TTNB).
Slide RD-31, 32, 33 Congenital and postnatal pneumonia
In developing countries, pneumonias account for more than 50 percent cases of respiratory distress in newborn. Primary pneumonias are more common among term or post term infants because of higher incidence of prenatal aspiration due to fetal hypoxia as a result of placental dysfunction. Preterm babies may develop pneumonia postnatally as a consequence of septicemia, aspiration of feeds and ventilation for respiratory failure. Clinical picture is characterized by tachypnea, respiratory distress with subcostal retractions, expiratory grunt and cyanosis. The condition may be heralded by apneic attacks rather than respiratory distress. Cough is rare in a newborn baby. The infant with congenital pneumonia is born with following predisposing factors (PROM> 24 hrs, foul smelling liquor, febrile maternal illness during peripartal period, prolonged/difficult delivery; single unclean or multiple vaginal examination(s) during labor). Respiratory distress is noticed soon after birth or during first 24 hours. Auscultaory signs may be nonspecific. The newborn may die from pneumonia without manifesting distress. Supportive
NNF Teaching Aids:Newborn Care
treatment should be provided. Baby should be nursed in thermo-neutral environment and kept nil orally. Intravenous infusion preferably through peripheral vein should be started. Oxygen should be administered to relieve the cyanosis and gradually weaned off. Specific therapy in the form of antibiotics should be started. In community acquired pneumonia, combination of ampicillin and gentamicin is appropriate while in hospital acquired pneumonia ampicillin and amikacin or a combination of cefotaxime and amikacin are appropriate. Pneumonia may be due to aspirations (TEF), gastro-esophageal reflux or may be of bacterial or viral etiology. Bacterial organisms are usually gram-ve or staphylococci. Parents often bring their children with complaints of noisy breathing. Most often this is due to nose block and could be treated with saline nose drops. However, we should distinguish this from stridor which could be a more serious problem. Other causes of upper airway problems presenting as distress would be bilateral choanal atresia.
Slide RD-34
Neonates who suffer asphyxia at birth may develop respiratory distress. The cause being asphyxia related injury to heart, brain or lungs.
Slide RD-35 Pneumothorax
Pneumothorax in neonates could be spontaneous, but is more often due to MAS or staphylococcal pneumonia. It is important to recognise pneumothorax because quick recognition and prompt treatment could be life saving. The distress is usually sudden in onset and heart sounds become less distinct. Immediate management in hemodynamically unstable neonate is by a needle aspiration and later chest tube drainage.
Slide RD-36
This X-ray shows pneumothorax on left side.
NNF Teaching Aids:Newborn Care
Cardiac disease should be suspected when there is significant distress with cyanosis, tachycardia and hepatomegaly. Tachypnea may be marked but chest retractions are minimal. If the baby presents in shock and distress one should suspect cardiac disease Refer to topic on Danger signs in newborn .
Slide RD-37 Primary pulmonary hypertension in newborn
One should suspect persistent / primary pulmonary hypertension also known as persistent fetal circulation in any neonate having severe respiratory distress and cyanosis. Ruling out a cyanotic congenital heart disease is mandatory in such a situation. Etiology of PPHN could be due to asphyxia, MAS or sepsis. Prognosis is poor and these neonates invariably need ventilatory support.
Slide RD-38 Summary
To sum up, there are many conditions causing respiratory distress. Early recognition of the etiology is important since management is usually complicated and needs level II or level III care. The situations which need referral are RDS, MAS, PPHN, malformations/surgical problems and cardiac disease. Distress due to pneumonia, TTNB and mild distress due to any cause may be managed at the periphery. Progression of distress, whatever the etiology again needs referral.
10
You might also like
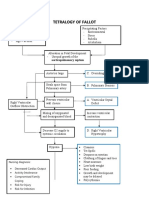
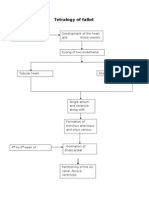
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
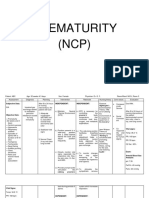
- NCP Proper 1Document6 pagesNCP Proper 1Noreen PinedaNo ratings yet
- Health Info Health Info Medicines Advanced Search Register Login Top of Form User NameDocument24 pagesHealth Info Health Info Medicines Advanced Search Register Login Top of Form User NameAnusha PradhanNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
- Tetralogy of Fallot Nursing Diagnosis and ManagementDocument2 pagesTetralogy of Fallot Nursing Diagnosis and ManagementKarl KiwisNo ratings yet
- Fetal Distress Case DiscussionDocument55 pagesFetal Distress Case DiscussionHafsah G.No ratings yet
- Hydrocephalus NCP - DayanghirangDocument2 pagesHydrocephalus NCP - DayanghirangEdnar DayanghirangNo ratings yet
- Gestational Age AssessmentDocument20 pagesGestational Age Assessmentscr1b1dNo ratings yet
- Birth Asphyxia ManagementDocument26 pagesBirth Asphyxia ManagementElvisNo ratings yet
- Transient Tachypnea of the Newborn (TTNDocument6 pagesTransient Tachypnea of the Newborn (TTNWivan Havilian DjohanNo ratings yet
- GastroschisisDocument19 pagesGastroschisiskunaidongNo ratings yet
- Hyaline Membrane DiseaseDocument31 pagesHyaline Membrane DiseaseWeng RamojalNo ratings yet
- Case (Acute Gastroenteritis) Group 4Document36 pagesCase (Acute Gastroenteritis) Group 4EljhayrosNo ratings yet
- Nursing Assessment, Planning, Implementation and EvaluationDocument2 pagesNursing Assessment, Planning, Implementation and EvaluationDiana MuañaNo ratings yet
- Spina Bifida, Meningocele MyelomeningoceleDocument1 pageSpina Bifida, Meningocele MyelomeningocelesmilingstarsNo ratings yet
- Compiled By: Lorie Noval Paclipan, MPH, RN: Newborn Screening in The PhilippinesDocument94 pagesCompiled By: Lorie Noval Paclipan, MPH, RN: Newborn Screening in The PhilippinesRovenick SinggaNo ratings yet
- Case Simulatio 115Document6 pagesCase Simulatio 115Dudong SasakiNo ratings yet
- 01 Postpartum EndometritisDocument12 pages01 Postpartum EndometritisDimitri Santillán AlarcónNo ratings yet
- Gastroschisis Final PresentationDocument43 pagesGastroschisis Final PresentationlhedavenNo ratings yet
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioNo ratings yet
- Hydrocephalus UpdatesDocument65 pagesHydrocephalus Updatescddinchimm100% (1)
- NCP AnxietyDocument6 pagesNCP AnxietyRaijenne VersolaNo ratings yet
- NCP Drug Study Group 1Document21 pagesNCP Drug Study Group 1Cassandra Grace Muerong Dela CruzNo ratings yet
- Dengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andDocument5 pagesDengue: Dengue Hemorrhagic Fever, Resulting in Bleeding, Low Levels of Blood Platelets andFrance John Evangelista TorresNo ratings yet
- Fluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementDocument32 pagesFluid Volume Deficit and Excess: Types, Causes, Signs and Nursing ManagementAcohCChaoNo ratings yet
- Chronic Tonsillitis Acute Exacerbation Case ReportDocument6 pagesChronic Tonsillitis Acute Exacerbation Case ReportBernadetha AstridNo ratings yet
- Neonatal Jaundice Case Study: Early Diagnosis and Treatment Prevents Brain DamageDocument6 pagesNeonatal Jaundice Case Study: Early Diagnosis and Treatment Prevents Brain DamagemuzamirNo ratings yet
- Prematurity and Lung Surfactant TherapyDocument27 pagesPrematurity and Lung Surfactant TherapyDivine LavaNo ratings yet
- A Case Report On Multifetal PregnancyDocument5 pagesA Case Report On Multifetal PregnancyThreecee VelezNo ratings yet
- Precipitate LaborDocument1 pagePrecipitate LaborJeli AlgasNo ratings yet
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Nutrition for pregnant and lactating womenDocument3 pagesNutrition for pregnant and lactating womenmo'niqueNo ratings yet
- Pneumonia in Children: Symptoms, Causes, TreatmentDocument4 pagesPneumonia in Children: Symptoms, Causes, TreatmentkuterinbatNo ratings yet
- Pneumonia Case StudyDocument8 pagesPneumonia Case StudyChristopher John AgueloNo ratings yet
- Beta ThalaDocument2 pagesBeta ThalaAngie LamoNo ratings yet
- PneumoniaDocument1 pagePneumoniaAyen FornollesNo ratings yet
- Jaundice NeonatalDocument26 pagesJaundice Neonatalhunk2662No ratings yet
- Neonatal Respiratory Distress SyndromenhschoicesDocument6 pagesNeonatal Respiratory Distress SyndromenhschoicessehatkanNo ratings yet
- Umbilical Cord ProlapseDocument6 pagesUmbilical Cord ProlapseCeth BeltranNo ratings yet
- Transient Tachypnea of The NewbornDocument6 pagesTransient Tachypnea of The NewbornTarquin TomadaNo ratings yet
- Nursing Diagnosis for Family AssessmentDocument106 pagesNursing Diagnosis for Family AssessmentShaira Ann CalambaNo ratings yet
- Premature Rupture of MembraneDocument7 pagesPremature Rupture of MembranedrommygreatNo ratings yet
- Hirschsprung's DiseaseDocument3 pagesHirschsprung's DiseaserjalavazoNo ratings yet
- Active Management of Normal LabourDocument16 pagesActive Management of Normal LabourjincyneeleshNo ratings yet
- Neonatal Sepsis Case StudyDocument6 pagesNeonatal Sepsis Case StudyCatherine PradoNo ratings yet
- Fraktur NCP Surgery PDFDocument4 pagesFraktur NCP Surgery PDFMuklis Al Fadlika100% (1)
- Pediatric Pneumonia Nursing Care PlanDocument2 pagesPediatric Pneumonia Nursing Care PlanLizaMarieNo ratings yet
- Aklan State University Nursing Readings on Pyloric StenosisDocument5 pagesAklan State University Nursing Readings on Pyloric Stenosisensoooooooooo100% (1)
- Rheumatic FeverDocument3 pagesRheumatic FeverKennette LimNo ratings yet
- Ectopic Pregnancy - PathophysiologyDocument1 pageEctopic Pregnancy - PathophysiologyMarimiel PagulayanNo ratings yet
- Case Study: Acute GlomerulonephritisDocument19 pagesCase Study: Acute GlomerulonephritisKuruma Maricar SorianoNo ratings yet
- Pathophysiology: Risk FactorsDocument4 pagesPathophysiology: Risk FactorsEdson John DemayoNo ratings yet
- PPH Introduction 1Document95 pagesPPH Introduction 1regine maeNo ratings yet
- Meconium Aspiration Syndrome: DR Bob KlajoDocument17 pagesMeconium Aspiration Syndrome: DR Bob KlajoBob John100% (1)
- Case Study OligoDocument7 pagesCase Study OligomutiaNo ratings yet
- Hepatitis overview and nursing careDocument18 pagesHepatitis overview and nursing careAnne B. BuenvenidaNo ratings yet
- High-Risk Pregnancy Factors & CareDocument19 pagesHigh-Risk Pregnancy Factors & CareRoger Jr PumarenNo ratings yet
- Neonatal Respiratory Distress Syndrome (RDS) Causes, Symptoms & TreatmentDocument11 pagesNeonatal Respiratory Distress Syndrome (RDS) Causes, Symptoms & TreatmentHina MasoodNo ratings yet
- Diagnosing and Treating Apnea of PrematurityDocument8 pagesDiagnosing and Treating Apnea of PrematuritypatriaindraNo ratings yet
- AI Search Iterative DeepeningDocument4 pagesAI Search Iterative DeepeningNirjal DhamalaNo ratings yet
- Veolia Moray Outfalls Repair WorksDocument8 pagesVeolia Moray Outfalls Repair WorksGalih PutraNo ratings yet
- IS 2848 - Specition For PRT SensorDocument25 pagesIS 2848 - Specition For PRT SensorDiptee PatingeNo ratings yet
- Biotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Document20 pagesBiotechnology Eligibility Test (BET) For DBT-JRF Award (2010-11)Nandakumar HaorongbamNo ratings yet
- Eating and HealingDocument19 pagesEating and HealingMariana CoriaNo ratings yet
- Audi A3 Quick Reference Guide: Adjusting Front SeatsDocument4 pagesAudi A3 Quick Reference Guide: Adjusting Front SeatsgordonjairoNo ratings yet
- Past Paper Booklet - QPDocument506 pagesPast Paper Booklet - QPMukeshNo ratings yet
- Basics of Duct DesignDocument2 pagesBasics of Duct DesignRiza BahrullohNo ratings yet
- Conceptual Framework For Group Processing of Lyric Analysis Interventions in Music Therapy Mental Health PracticeDocument9 pagesConceptual Framework For Group Processing of Lyric Analysis Interventions in Music Therapy Mental Health Practiceantonella nastasiaNo ratings yet
- Publications FireSafetyDesign SDocument369 pagesPublications FireSafetyDesign SJayachandra Reddy AnnavaramNo ratings yet
- Nysc Editorial ManifestoDocument2 pagesNysc Editorial ManifestoSolomon Samuel AdetokunboNo ratings yet
- Module 2 What It Means To Be AI FirstDocument85 pagesModule 2 What It Means To Be AI FirstSantiago Ariel Bustos YagueNo ratings yet
- Hilton 5-29 Case SolutionDocument4 pagesHilton 5-29 Case SolutionPebbles RobblesNo ratings yet
- Women Safety AppDocument18 pagesWomen Safety AppVinod BawaneNo ratings yet
- Divide Fractions by Fractions Lesson PlanDocument12 pagesDivide Fractions by Fractions Lesson PlanEunice TrinidadNo ratings yet
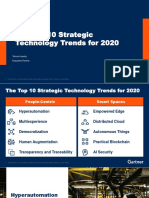
- The Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerDocument31 pagesThe Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerCarlos Stuars Echeandia CastilloNo ratings yet
- Wei Et Al 2016Document7 pagesWei Et Al 2016Aline HunoNo ratings yet
- SRC400C Rough-Terrain Crane 40 Ton Lifting CapacityDocument1 pageSRC400C Rough-Terrain Crane 40 Ton Lifting CapacityStephen LowNo ratings yet
- Marriage Gift PolicyDocument4 pagesMarriage Gift PolicyGanesh Gaikwad100% (3)
- Principal Component Analysis of Protein DynamicsDocument5 pagesPrincipal Component Analysis of Protein DynamicsmnstnNo ratings yet
- Design of Steel Structures Handout 2012-2013Document3 pagesDesign of Steel Structures Handout 2012-2013Tushar Gupta100% (1)
- Government of The Punjab Primary & Secondary Healthcare DepartmentDocument3 pagesGovernment of The Punjab Primary & Secondary Healthcare DepartmentYasir GhafoorNo ratings yet
- Type of PoemDocument10 pagesType of PoemYovita SpookieNo ratings yet
- EGMM - Training Partner MOUDocument32 pagesEGMM - Training Partner MOUShaik HussainNo ratings yet
- UTC awarded contracts with low competitionDocument2 pagesUTC awarded contracts with low competitioncefuneslpezNo ratings yet
- Marketing of Agriculture InputsDocument18 pagesMarketing of Agriculture InputsChanakyaNo ratings yet
- Skype Sex - Date of Birth - Nationality: Curriculum VitaeDocument4 pagesSkype Sex - Date of Birth - Nationality: Curriculum VitaeSasa DjurasNo ratings yet
- Ejemplo FFT Con ArduinoDocument2 pagesEjemplo FFT Con ArduinoAns Shel Cardenas YllanesNo ratings yet
- EasyLogic PM2000 Series - METSEPM2130Document4 pagesEasyLogic PM2000 Series - METSEPM2130ٍJordan SportNo ratings yet
- Speech TravellingDocument4 pagesSpeech Travellingshafidah ZainiNo ratings yet