Professional Documents
Culture Documents
Irritable Bowel Syndrome
Uploaded by
Rakesh S IndiaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Irritable Bowel Syndrome
Uploaded by
Rakesh S IndiaCopyright:
Available Formats
Continuing Medical Education
Irritable Bowel Syndrome
Martin Schlup
Correspondence to: martin.schlup@stonebow.otago.ac.nz A good set of bowels is worth more than any quantity of brain Josh Billing (Henry WheelerShaw 18181885)
Martin Schlup is a Senior Lecturer in
Medicine at the University of Otago and a Gastroenterologist, Otago District Health Board, Dunedin. He has specific interests in aspects of colonic disease, gastrointestinal endoscopy and the quality of endoscopy. Martin was born and trained in Switzerland and has been in his current position since 1986.
Introduction
If there was a popularity hit list of various bodily organs, bowels wouldnt rate very highly. Patients not infrequently commiserate with my job as a gastroenterologist dealing with parts of the body one doesnt talk about. And yet the gut is a marvellous organ: its big the size of a football field if stretched out and has the bodys largest absorptive surface area exposed to foreign material. It is a major player of the immune system and has a neural wiring system that in size and complexity matches the spinal cord. The gut has the dual function of selective absorption of nutrients and protection against ingested injurious components such as viruses, bacteria and toxins. The gut is exposed to a huge antigenic load it has been estimated that over a lifetime we ingest about 2500kg of food antigens1 without this eliciting a systemic immune response. The gut, particularly the colon, is a repository for bacteria with about 1013 organisms, the highest cell density recorded for any
ecosystem.2 Some 60% of faecal residue passed is made up of bacteria. Several mechanisms help to maintain the integrity and function of the intestine: Mechanical, such as peristalsis, epithelial barrier function including the important role of tight junctions, mucus layer, and Non mechanical processes, such as the commensal gut flora, innate and adaptive immune responses and neuroregulatory processes. These complex interactions that modulate the guts response to external and internal stimuli occur mostly autonomically at the level of the gut. There is both afferent and efferent communication with the brain where conscious perception occurs the brain-gut axis. Most of these interactions remain largely unperceived the two exceptions being ingestion and excretion. It is perhaps surprising that disturbances of these interactions are not more common when they do occur we tend to call them functional gastrointestinal problems with one subgroup being IBS.
What is IBS?
IBS occurs worldwide with similar incidences in developed and developing countries, but is more common in women. It affects about 1520% of the population, but not all affected people will seek medical assistance. Abnormalities of GI sensation, motility, autonomic function, bacterial flora and the immune system have been described as possible
mechanisms leading to the symptoms of IBS.3 A more holistic view of IBS is to regard it as a complex of symptoms without a single cause, that reflects an integrated response to a variety of complex interactions combining biological and psychosocial factors. Or, put more succinctly, IBS is a disorder of the braingut interactions with both physical and psycho-social components.4,5 IBS is one of many different functional somatic syndromes (FSS), which are characterised by patterns of persistent bodily complaints, for which adequate examination does not reveal sufficiently structural or other specified pathology.6 Medically unexplained symptoms are common in general practice; studies have shown that in up to 50% of patients presenting with physical symptoms the cause remains unknown. In our own unit we recently reviewed our OP activities over the last 15 years and found that some 3040% of patients attending OP present with medically unexplained gastrointestinal symptoms.7 IBS is one of the three most common FSS, the others being Chronic fatigue syndrome and Fibromyalgia, with overlaps between FSS being quite common; be it between different functional gastrointestinal problems such as IBS/functional dyspepsia and/or functional abdominal pain or between gastrointestinal and nongastrointestinal FSS. IBS is often associated with chronic fatigue and/or fibromyalgia symptoms. Although FSS are often associated with anxiety, depression and somati-
354
Volume 34 Number 5, October 2007
sation they cannot be viewed simply as a psychological reaction or over reaction to bodily complaints nor as masked or somatised depressive or anxiety problems.
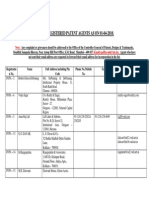
Table 1.
Rome III Criteria
Recurrent abdominal pain/discomfort at least three days per month in the last three months associated with two or more of the following: Improvement with defecation Onset associated with a change in bowel frequency Onset associated with a change in form
Alarm symptoms
Age over 50 on first presentation Short history Weight loss Nocturnal symptoms Rectal bleeding Recent antibiotic use
How to diagnose IBS
IBS is a positive, clinically based diagnosis and not a diagnosis made as a last resort after other pathologies have been excluded, a view that is still widely promulgated. A thorough history and physical examination allow establishing the diagnosis of IBS on first consultation: patients are usually young females presenting with a combination of abdominal pain/discomfort and variable bowel motions. Detailed history often elicits a long history of various abdominal complaints. Fatigue and lack of appetite but weight gain are frequently present. The Rome III criteria (Table 1) are very helpful in establishing a positive diagnosis of IBS8 while presence of alarm symptoms generally precludes a diagnosis of IBS and warrants appropriate investigations. IBS can be subdivided according to stool frequency: IBS with constipation hard stools >25% loose stools <25% of the time IBS with diarrhoea hard stools <25% loose stools >25% of the time Mixed IBS the most common form of IBS. This division is particularly useful for the longer term management of the patient.
The physical examination is generally unremarkable ill-defined abdominal tenderness is common. Point tenderness along the costal margin exaggerated by tensing the abdominal wall muscles suggests the painful rib syndrome.9 Features suggesting a non-visceral abdominal pain are summarised in Table 2.10 History and physical examination should be complemented by some baseline blood tests that should include a test for coeliac disease. Sigmoidoscopy is particularly useful in patients with diarrhoea to exclude inflammatory bowel disease. More extensive and repetitive investigations create uncertainty that is detrimental to the successful management of patients with IBS; it has the effect of reinforcing concerns about a potential physical cause of the problem.
Management
Treatment of patients with IBS starts at the first consultation taking the time to take a thorough history, to
Table 2. Features of Non-Visceral abdominal pain
Onset
Often insidious History of injury or repetitive trauma or uncommon activity not uncommon
Pain Position Modulating factors
Sharp component with dull persisting ache, which may radiate, on the affected side Aggravated or relieved by certain positions, changes in posture, lifting, coughing or sneezing Relief by local heat application or pressure Generally no association with food intake or bowel action
perform the physical examination and to explain the nature of IBS and the basis for this diagnosis. Physicians seem to have considerable discomfort in managing these patients, who are often referred to as difficult or heartsink patients.11 The frequent attendance of these patients results in high health care costs12 often attributed to the patients demanding further investigations. And yet, the somatising effect of medically unexplained symptoms is as much a result of the clinician seeking an elusive cause as the patient wanting an explanation.13 We often feel ill equipped to deal with such patients and continue to look for a medical cause for the patients symptoms resulting in a spiral of unnecessary interventions. The Hippocratic oath, first do no harm seems to be replaced by a new mantra: first of all: dont miss a medical diagnosis.14 Maybe we need to be less concerned about cause and be more concerned with care.15 The interaction between patient and doctor is therefore a crucial part in the management of patients with medically unexplained symptoms. A constructive approach is to establish the diagnosis of IBS on initial consultation with confidence, but at the same time acknowledging concerns and anxieties about more serious pathology. These need to be discussed and explained as to why they are not the cause of the patients symptoms. Some baseline tests are useful in alleviating
Volume 34 Number 5, October 2007
355
Continuing Medical Education Con
Continuing Medical Education
these anxieties; predicting that these tests will likely be normal further helps to reassure the patient. Patients often experience our explanations that examination and baseline investigations are normal as rejecting the reality of their symptoms; we need to convey to the patients the reality and legitimacy of their symptoms.16 Lifestyle advice is another important part of the management of IBS patients. Dietary concerns need to be reviewed and dietary excesses need to be addressed; a trial of a lactose free diet for one to two weeks can help to exclude lactase deficiency as a cause for the patients symptoms. Many patients will already have trialled various dietary modifications; food intolerance has not been shown to be associated with IBS. Food intolerance is often diagnosed on the basis of skin tests that are notoriously unreliable in this context. I dont believe in initiating a gluten free diet until a diagnosis of coeliac disease has been established even though many patients with or without IBS opt to restrict gluten intake. Regular mealtimes with more frequent and small meals can be useful; not infrequently patients with IBS eat very irregularly and at times large meals. Although drug therapy is often the preferred way of treating or being treated for IBS, its results are often disappointing. Drug therapy should be a last rather than an initial approach to the management of IBS patients. Systematic reviews on the efficacy and safety of pharmacological agents for IBS have recently been published17,18 a brief summary follows: Antispasmodics/smooth muscle relaxants may be of limited benefit in patients in whom pain is the predominant symptom. Their efficacy is not well documented in controlled trials. Loperamide may have a place in IBS with diarrhoea particularly where there is an added problem of faecal incontinence. Both these drugs can be used on demand rather than on a regular basis. Bulking agents and laxatives may be a useful adjunct in IBS with constipation. Regular intake with sufficient fluid intake is crucial in achieving a good result. Tricyclic antidepressants have been shown in a meta-analysis to offer advantage over placebo.19 These work best in patients who have abdominal pain and diarrhoea or mixed IBS. The dose of the drug is well below the antidepressant dose I usually use amitryptiline starting at 10mg at night and building up to a maximum of 50mg. Patients need to persevere with the medication for at least four weeks; they need to be warned about early side effects such as fatigue and dry mouth that tend to settle over time. If effective they should be continued for a minimum of six months. Selective serotonin reuptake inhibitors (SSRI) have fewer side effects than tricyclic antidepressants, which makes them more attractive to patients who have IBS. Few trials, often including small numbers only, have addressed their efficacy. Generally a beneficial effect in favour of SSRIs is found: SSRIs seem to promote a sense of wellbeing, possibly some improvement in pain (SSRIs do have a mild analgesic effect) and may be more useful in patients with constipation. These beneficial effects seem to be independent of improvement in any concurrent depression. SSRIs may also reduce the reporting of multiple bodily symptoms or somatisation.4 The serotonin type 3 (5HT3) antagonist, alosetron, has been shown to improve diarrhoea in female IBS patients with the latest study showing improvement for all doses of alosetron at 12 weeks.20 However, concerns about ischemic colitis and severe constipation have prompted withdrawal of the drug in most countries.
Key Points
IBS is a syndrome of medically unexplained symptoms resulting from a variety of biological and psychosocial factors The diagnosis can be made on the basis of a typical history it is not a diagnosis of exclusion Baseline investigations are useful in addressing patients concerns about serious medical condition but extended and repeat investigations have no place Thorough explanations need to address patients concerns and anxieties Lifestyle and dietary advice should be used before drug therapy Fibre may have a role in IBS with constipation, Loperamide in IBS with diarrhoea SSRIs improve global symptoms without altering bowel symptoms Tricyclic antidepressants may benefit patients with pain and diarrhoea Antispasmodics are of limited value Serotonin antagonists (diarrhoea) and agonists (constipation) are effective but have potentially serious adverse effects Psycho- and hypnotherapy if available are useful and beneficial
The serotonin type 4 (5HT4) agonist tegaserod may improve constipation in woman with IBS. Concerns about an increase in myocardial ischemia and strokes have led to a restriction in its use. Psychological treatments such as cognitive behaviour therapy and hypnotherapy have been evaluated in
356
Volume 34 Number 5, October 2007
Continuing Medical Education
randomised controlled trials21 and show improved coping although they are not necessarily associated with improving bowel symptoms. These treatments are not easily accessible in New Zealand.
Competing interests
None declared.
References
1. Perdue MH. Mucosal immunity and inflammation III. The mucosal antigen barrier: cross talk with mucosal cytokines. Am. J. Physiol. 1999; 277:G1-G5. Backhead F, Ley R, Sonnenburg JL, et al. Host-bacterial mutualism in the human intestine. Science 2005; 307:1915-20. Spiller R. Clinical update: irritable bowel syndrome. Lancet 2007; 369:1586-88. Hayee B, Forgacs I. Psychological approach to managing irritable bowel syndrome. BMJ 2007; 334:1105-9. Drossmann D. The Functional Gastrointestinal Disorders and the Rome III criteria. Gastroenterology 2006; 130:1377-90 Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet 2007; 369:94655. What does the Gastroenterologist do all day A Dunedin perspective. Trainee Intern Health Care Evaluation Project, Dept. of Preventive and Social Medicine, Dunedin School of Medicine, University of Otago. Longstreth GF, Thompson WG, Chey WQD, et al. Functional bowel disorders. Gastroenterology 2006; 130:1480-91. Scott EM, Scott BB. Painful rib syndrome a review of 76 cases. Gut 1993; 34:1006-8 Sharpstone D, Colin-Jones DG. Chronic, non-visceral abdominal pain. Gut 1994; 35:8336. Rosendal M, Fink P, Flemming B. Somatization, heartsink patients, or functional somatic symptoms? Scan J Prim Health Care 2005; 23:310. Leong SA, Barghout V, Birnbaum HG, et al. The economic consequences of irritable bowel syndrome. Arch Intern Med 2003; 163:92935. Ring A, Dowrick CF, Humphries GM, et al. The somatising effect of clinical consultation: what patients and doctors say and do not say when patients present medically unexplained physical symptoms. Soc Sci Med 2005; 61:150515. Bensing JM, Verhaak PFM, Somatisation: a joint responsibility of doctor and patient. Lancet 2006; 367:452-3. McWhinney IR, Epstein RM, Freeman TR. Rethinking somatisation. Ann Intern Med 1997; 126:747-50. Salmon P, Peters S, Stanley I. Patients perceptions of medical explanations for somatisation disorders: qualitative analysis. BMJ 1999; 318:372-6. Tack J, Fried M, Houghton LA, et al. Systematic review: the efficacy of treatments for irritable bowel syndrome a European perspective. Aliment Pharmacol Ther 2006; 24:183-205. Heading R, Bardhan K, Hollerbach S, et al. Systematic review: the safety and tolerability of pharmacological agents for treatment of irritable bowel syndrome a European perspective. Aliment Pharmacol Ther 2006; 24:207-236. Jackson JL, OMalley PG, Tomkins G, et al. Treatment of functional gastrointestinal disorders with antidepressant medications: a meta-analysis. Am J Med 2000; 325:991-1000. Krause R, Ameen V, Gordon SH, et al. A randomized, doubleblind, placebo-controlled study to assess efficacy and safety of 0.5 mg and 1 mg Alosetron in women with severe diarrheapredominant IBS. Am J Gastroenterol. 2007; 102:1709-19. Lackner JM, Mesmer C, Morley S, et al. Psychological treatments for irritable bowel syndrome: a systematic review and meta analysis. J Consult Clin Psychol 2004; 72:1100-13.
2. 3. 4. 5. 6. 7.
8. 9. 10. 11.
12.
13.
14. 15. 16.
17.
18.
19.
20.
21.
Volume 34 Number 5, October 2007
357
You might also like
- A Victim No More: Overcoming Irritable Bowel Syndrome: Safe, Effective Therapies for Relief from Bowel ComplaintsFrom EverandA Victim No More: Overcoming Irritable Bowel Syndrome: Safe, Effective Therapies for Relief from Bowel ComplaintsNo ratings yet
- For GI DisturbanceDocument17 pagesFor GI Disturbanceraquel maniegoNo ratings yet
- Good DigestionDocument140 pagesGood DigestionMonica VillavicencioNo ratings yet
- Irritable Bowel SyndromDocument7 pagesIrritable Bowel SyndromJosni VargheseNo ratings yet
- Functional Gastrointestinal DisordersDocument6 pagesFunctional Gastrointestinal DisordersMarwan M.No ratings yet
- Acute GastritisDocument43 pagesAcute GastritisANCHAL SHARMANo ratings yet
- The Complete Guide to Irritable Bowel Syndrome: Symptoms, Risks, Prevention, Medicines & Home RemediesFrom EverandThe Complete Guide to Irritable Bowel Syndrome: Symptoms, Risks, Prevention, Medicines & Home RemediesNo ratings yet
- Beam Deflection FormulaeDocument2 pagesBeam Deflection Formulae7575757575100% (6)
- Diet IBS PDFDocument31 pagesDiet IBS PDFIesanu MaraNo ratings yet
- SAE Product Engineering Mini CatalogDocument60 pagesSAE Product Engineering Mini CatalogRakesh S IndiaNo ratings yet
- FMEA RCM Course Foundations of Effective FMEA RS 470 CourseNotes Rev9 1 PDFDocument358 pagesFMEA RCM Course Foundations of Effective FMEA RS 470 CourseNotes Rev9 1 PDFRakesh S India100% (2)
- Failure Modes and Effects Analysis: R.R. MohrDocument37 pagesFailure Modes and Effects Analysis: R.R. Mohrmh70100% (8)
- Medically Unexplained Symptoms Assessment and ManagementDocument6 pagesMedically Unexplained Symptoms Assessment and ManagementMatheus AzevedoNo ratings yet
- SEC 5 Bearing, Sprocket & Roller ChainDocument41 pagesSEC 5 Bearing, Sprocket & Roller ChainRakesh S IndiaNo ratings yet
- SEC 5 Bearing, Sprocket & Roller ChainDocument41 pagesSEC 5 Bearing, Sprocket & Roller ChainRakesh S IndiaNo ratings yet
- Inflammatory Bowel Disease & Irritable Bowel Syndrome Understanding, Distinguishing and AddressingDocument20 pagesInflammatory Bowel Disease & Irritable Bowel Syndrome Understanding, Distinguishing and AddressingVas RaNo ratings yet
- Oet RT2Document16 pagesOet RT2Ryu Tse100% (3)
- DIN STD List PDFDocument4 pagesDIN STD List PDFRakesh S IndiaNo ratings yet
- Irritable Bowel Syndrome (IBS) or Excessive Mast Cells? Research SummaryFrom EverandIrritable Bowel Syndrome (IBS) or Excessive Mast Cells? Research SummaryNo ratings yet
- Integration of Mental Health Into Primary Health CareDocument15 pagesIntegration of Mental Health Into Primary Health CareBenson Nyirenda Jnr100% (1)
- Irritable Bowel Syndrome: Heal Your Gut Naturally in 90 Days!From EverandIrritable Bowel Syndrome: Heal Your Gut Naturally in 90 Days!No ratings yet
- Brain-Gut Interactions And Somatization in Irritable Bowel Syndrome (IBS)From EverandBrain-Gut Interactions And Somatization in Irritable Bowel Syndrome (IBS)No ratings yet
- Dr. S.P. RaiDocument12 pagesDr. S.P. RaiSachin MundeNo ratings yet
- Irritable Bowel SyndromDocument2 pagesIrritable Bowel SyndromCésar AndraskiNo ratings yet
- Quigley Ibs LectureDocument6 pagesQuigley Ibs Lecturegbass_9No ratings yet
- Iritable Bowel SyndromeDocument6 pagesIritable Bowel SyndromefitrianugrahNo ratings yet
- Beyond Bowels: Understanding Co-existing Symptoms in IBSDocument8 pagesBeyond Bowels: Understanding Co-existing Symptoms in IBSparthibanemails5779No ratings yet
- Guide to Living With IBSDocument12 pagesGuide to Living With IBSMuhammad Imam Fitrah HariantoNo ratings yet
- Irritable Bowel DiseaseDocument15 pagesIrritable Bowel DiseaseSupriya chhetryNo ratings yet
- Case Study 3Document16 pagesCase Study 3api-27097296550% (2)
- TraditionallyDocument13 pagesTraditionally02 APH Komang AnggariniNo ratings yet
- Irritable Bowel SyndromeDocument7 pagesIrritable Bowel SyndromeJudith GraalNo ratings yet
- Colonul Iritabil, C. I., in Literatura Engleza Functionale Gastrointestinale Frecvent Intalnite in Practica MedicalaDocument49 pagesColonul Iritabil, C. I., in Literatura Engleza Functionale Gastrointestinale Frecvent Intalnite in Practica MedicalaAndreea MarinNo ratings yet
- IBS CaseDocument8 pagesIBS CaseStarr NewmanNo ratings yet
- Irritable Bowel Syndrome: Histology ReportDocument6 pagesIrritable Bowel Syndrome: Histology ReportHussein Al-khafajiNo ratings yet
- IBS Pathophysiology & ManagementDocument18 pagesIBS Pathophysiology & ManagementUsman Ali AkbarNo ratings yet
- Irritable Bowel Syndrome: New and Emerging Treatments: Magnus Halland, Yuri A SaitoDocument14 pagesIrritable Bowel Syndrome: New and Emerging Treatments: Magnus Halland, Yuri A SaitoAbeir C. UsmanNo ratings yet
- Diet and IBS, Fibromyalgia, and MigraineDocument40 pagesDiet and IBS, Fibromyalgia, and MigrainedBiswas2011No ratings yet
- Irritable Bowel Syndrome and Other Functional Gastrointestinal DisordersDocument3 pagesIrritable Bowel Syndrome and Other Functional Gastrointestinal DisordersdavpierNo ratings yet
- Nutrients 13 00575Document19 pagesNutrients 13 00575dr.martynchukNo ratings yet
- The Irritable Bowel Syndrome: Edward ZammitDocument7 pagesThe Irritable Bowel Syndrome: Edward ZammitjunliantyNo ratings yet
- Journal Reading: Therapeutic Strategies For Functional Dyspepsia and Irritable Bowel Syndrome Based On PathophysiologyDocument4 pagesJournal Reading: Therapeutic Strategies For Functional Dyspepsia and Irritable Bowel Syndrome Based On PathophysiologyMuhamad IrsyadNo ratings yet
- 561486-564546 - Bland Lynn - Dec 10 2023 1123 Am - Final Project Contribution 1Document11 pages561486-564546 - Bland Lynn - Dec 10 2023 1123 Am - Final Project Contribution 1api-468565768No ratings yet
- Irritable Bowel Syndrome PTH 617 PresentationDocument14 pagesIrritable Bowel Syndrome PTH 617 Presentationapi-621438645No ratings yet
- Irritable Bowel SyndromeDocument3 pagesIrritable Bowel SyndromeRody Mark AraoNo ratings yet
- Ronald Glick, MD, Karl Holtzer, MD, and Greg Thorkelson, MD: Why Do We Need A Different Approach? Beyond These Big ThreeDocument6 pagesRonald Glick, MD, Karl Holtzer, MD, and Greg Thorkelson, MD: Why Do We Need A Different Approach? Beyond These Big ThreewhiteyasminNo ratings yet
- Irritable Bowel Syndrome (IBS)Document2 pagesIrritable Bowel Syndrome (IBS)Lija ManojNo ratings yet
- IBS Physio Presentation (GRP No 4)Document23 pagesIBS Physio Presentation (GRP No 4)Fatima AsifNo ratings yet
- IBD Briggs Beta7Document27 pagesIBD Briggs Beta7Amit Yadav100% (4)
- 4 Constipation and Pregnancy: Garret CullenDocument12 pages4 Constipation and Pregnancy: Garret Cullenj hdezNo ratings yet
- IBS MY PRESENTATIONDocument36 pagesIBS MY PRESENTATIONunderworldgaming161No ratings yet
- Nyeri Abdomen Pada AnakDocument11 pagesNyeri Abdomen Pada AnakIzkaPutriRahmaniaNo ratings yet
- IntestinDocument105 pagesIntestinМарьяна РизничукNo ratings yet
- Irritable Bowel SyndromeDocument11 pagesIrritable Bowel SyndromereboNo ratings yet
- Chronic Pelvic Pain in Adolescents: A Biopsychosocial ApproachDocument4 pagesChronic Pelvic Pain in Adolescents: A Biopsychosocial ApproachMarrietta Sugiarti SadeliNo ratings yet
- Age, Gender, and Women 'S Health and The PatientDocument16 pagesAge, Gender, and Women 'S Health and The Patientmarii de los angelesNo ratings yet
- Irritable Bowel Syndrome: EsophagusDocument4 pagesIrritable Bowel Syndrome: EsophagusbloodyluxNo ratings yet
- Diseases & Disorders IBS (See - Irritable Bowel Syndrome)Document7 pagesDiseases & Disorders IBS (See - Irritable Bowel Syndrome)masteruhkhanNo ratings yet
- Irritablebowelsyndrome: What Treatments Really WorkDocument16 pagesIrritablebowelsyndrome: What Treatments Really WorkTeodora RaindropNo ratings yet
- Ibs 6Document31 pagesIbs 6Hesham IbrahimNo ratings yet
- Irritable Bowel Syndrome: EsophagusDocument4 pagesIrritable Bowel Syndrome: EsophagusGebina Wahyu ArdinaNo ratings yet
- What Causes IBS?Document4 pagesWhat Causes IBS?prima suci angrainiNo ratings yet
- Chronic Abdominal Pain in ChildrenDocument3 pagesChronic Abdominal Pain in ChildrenOmar M AlsalmanNo ratings yet
- Jet 36Document1 pageJet 36api-243067767No ratings yet
- What Is The Process of IBS Treatment in PakistanDocument3 pagesWhat Is The Process of IBS Treatment in PakistanMuhammad Shahrukh KhanNo ratings yet
- Production Technology Ch07Document15 pagesProduction Technology Ch07Nimmagadda BharathNo ratings yet
- Tolerance TableDocument2 pagesTolerance TablePrabhanjan BhatNo ratings yet
- Biofuel - INNOVATION - Researchers Find Way To Turn Algae Into Fuel, Energy News, ET EnergyWorld PDFDocument6 pagesBiofuel - INNOVATION - Researchers Find Way To Turn Algae Into Fuel, Energy News, ET EnergyWorld PDFRakesh S IndiaNo ratings yet
- Biofuel - INNOVATION - Researchers Find Way To Turn Algae Into Fuel, Energy News, ET EnergyWorld PDFDocument6 pagesBiofuel - INNOVATION - Researchers Find Way To Turn Algae Into Fuel, Energy News, ET EnergyWorld PDFRakesh S IndiaNo ratings yet
- PDFDocument26 pagesPDFJelena MalaNo ratings yet
- General Design Rules For MachiningDocument30 pagesGeneral Design Rules For MachiningSarath Chandra82% (11)
- Honeywell MagneticSensorsDocument13 pagesHoneywell MagneticSensorsRakesh S IndiaNo ratings yet
- List PatentAgent April 2010Document188 pagesList PatentAgent April 2010Gnanesh Shetty BharathipuraNo ratings yet
- Rolling and Sliding Bearings PDFDocument55 pagesRolling and Sliding Bearings PDFRakesh S IndiaNo ratings yet
- Honeywell MagneticSensorsDocument13 pagesHoneywell MagneticSensorsRakesh S IndiaNo ratings yet
- 7 of The Top 10 Most Polluted Cities in The World Are in India - The Economic TimesDocument2 pages7 of The Top 10 Most Polluted Cities in The World Are in India - The Economic TimesRakesh S IndiaNo ratings yet
- Grind-hardening Process Reduces Environmental ImpactDocument6 pagesGrind-hardening Process Reduces Environmental ImpactRakesh S IndiaNo ratings yet
- Hall and VR Speed SensorsDocument3 pagesHall and VR Speed SensorsAmir BshNo ratings yet
- List PatentAgent April 2010Document188 pagesList PatentAgent April 2010Gnanesh Shetty BharathipuraNo ratings yet
- 'RHV 6lolfrq 9dooh/: +dyh (QRXJK 0hfkdqlfdo (Qjlqhhuv"Document6 pages'RHV 6lolfrq 9dooh/: +dyh (QRXJK 0hfkdqlfdo (Qjlqhhuv"Rakesh S IndiaNo ratings yet
- Mechanical Components GuideDocument36 pagesMechanical Components GuideRakesh S IndiaNo ratings yet
- Stackup Analysis - Topics For TrainingDocument1 pageStackup Analysis - Topics For TrainingRakesh S IndiaNo ratings yet
- Hall Effect Crankshaft Sensors: Similar But BetterDocument4 pagesHall Effect Crankshaft Sensors: Similar But BetterRakesh S IndiaNo ratings yet
- Jigs and FixturesDocument187 pagesJigs and FixturesRakesh S IndiaNo ratings yet
- Introduction to Stress and Strain ConceptsDocument48 pagesIntroduction to Stress and Strain ConceptsRakesh S IndiaNo ratings yet
- Chapter 1 Introduction 1 Chapter 5 General Rules 51: Preface VII Acknowledgements VIIIDocument2 pagesChapter 1 Introduction 1 Chapter 5 General Rules 51: Preface VII Acknowledgements VIIIRakesh S IndiaNo ratings yet
- General Design Rules For MachiningDocument30 pagesGeneral Design Rules For MachiningSarath Chandra82% (11)
- Time Planner EverydayDocument2 pagesTime Planner EverydayRakesh S IndiaNo ratings yet
- CBT approach to medically unexplained symptomsDocument7 pagesCBT approach to medically unexplained symptomsaastha jainNo ratings yet
- Actual Neurosis and PTSD The Impact of The OtherDocument16 pagesActual Neurosis and PTSD The Impact of The OtherLuana SouzaNo ratings yet
- Print 10Document4 pagesPrint 10FARAH MOHAMMEDNo ratings yet
- Somatoform Symptom Disorder: A Diagnostic Dilemma!: BMJ Case Reports November 2019Document5 pagesSomatoform Symptom Disorder: A Diagnostic Dilemma!: BMJ Case Reports November 2019HKNo ratings yet
- Somatic Symptom Disorder: Lesley A. Allen and Robert L. WoolfolkDocument26 pagesSomatic Symptom Disorder: Lesley A. Allen and Robert L. WoolfolksimbawulaNo ratings yet