Professional Documents
Culture Documents
Lung Abscess in Children
Uploaded by
Caballero X CaballeroOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lung Abscess in Children
Uploaded by
Caballero X CaballeroCopyright:
Available Formats
Journal of Pediatric Infectious Diseases 4 (2009) 2735 27
DOI 10.3233/JPI-2009-0148
IOS Press
Review Article
Lung abscess in children
Haya Alsubie and Dominic A. Fitzgerald
Department of Respiratory Medicine, The Childrens Hospital at Westmead, Sydney, NSW, Australia
Received 25 July 2008
Revised 30 July 2008
Accepted 4 September 2008
Abstract. Lung abscess is an uncommon but challenging condition to manage. Predisposing factors including pulmonary
aspiration and impaired mucociliary defense mechanisms increase the likelihood of developing a secondary lung abscess.
Aspirating anaerobic organisms from the mouth leading to pneumonia and a secondary lung abscess is more likely to be
seen in children with neuro-cognitive impairment. The more likely anaerobic organisms include Peptostreptococcus species,
Fusobacterium nucleatum and Prevotella melaninogenica. These organisms may be difcult to isolate without specic anaerobic
transport vials and culture media. The rise of interventional radiology, higher positive culture results, better targeted antibiotic
regimes and a greater awareness of hospital acquired pathogens have been signicant is decreasing the length of hospitalization
for children with lung abscesses. The morbidity and mortality for lung abscess in children is vastly superior to that in adult
patients because of the lack of co-morbidities in the pediatric population.
Keywords: Lung abscess, pathophysiology, microbiology, anaerobes, interventional radiology, antibiotic therapy
1. Introduction
Lung abscess is an uncommon but important pedi-
atric problem. It is believed to be less common in chil-
dren than adults, although the literature is accordingly
relatively sparse. Lung abscesses may be classied as
primary or secondary, depending upon the existence
of predisposing conditions. Similarly, lung abscesses
may be single or multiple. Those that are secondary
are far more likely to be caused by anaerobic bacteria.
Typically, in children as in adults, it is the existence
of underlying conditions, which will inuence the ap-
proach to management, and the prognosis of a patient
who presents with a lung abscess [13].
Correspondence: Dr. Dominic A. Fitzgerald, Department of Res-
piratory Medicine, The Childrens Hospital at Westmead, Locked
Bag 4001, Westmead, Sydney, NSW, Australia, 2145. Tel.: +61 2
9845 3397; Fax: +61 2 9845 3396; E-mail: dominif2@chw.edu.au
2. Denition
A lung abscess is a thick-walled cavity that contains
purulent material resulting fromsuppuration and necro-
sis of the lung parenchyma [14]. The lung abscess
may be primary or secondary. A primary lung abscess
occurs in a previously well child with normal lungs,
usually as a complication of pneumonia, and will usu-
ally reach a full recovery without any sequalae. A sec-
ondary lung abscess occurs in a child with an under-
lying airway or lung abnormality, which may be con-
genital (cystic brosis, immunodeciency or structural
malformation) or acquired (achalasia or a neurodevel-
opmental abnormality) [13].
3. Epidemiology
It has been suggested that lung abscesses were more
common in previous years [1] before the ability of pre-
1305-7707/09/$17.00 2009 IOS Press and the authors. All rights reserved
28 H. Alsubie and D.A. Fitzgerald / Lung abscess in children
Table 1
Factors predisposing to secondary lung abscesses may be seen in
children at increased risk of pulmonary aspiration such as those with
the following predisposing factors
Immunocompromised host:
Chemotherapy
Immunosuppressive treatment (corticosteroids)
Nutritional deciencies
Localized structural lung abnormalities:
Congenital cystic adenomatoid malformation
Bronchogenic cyst
Tracheo-esophageal stula (H-type)
Generalized suppurative lung disease:
Cystic brosis
Hematogenous spread
Neurodevelopmental abnormalities:
Poorly coordinated swallowing
Neuromuscular condition such as myotonic dystrophy and
Duchenne muscular dystrophy
Esophageal motility problems:
Following tracheo-esophageal atresia repair
Esophageal strictures
Achalasia
venting aspiration of infected uid at the time of ton-
sillectomy, the widespread availability of antibiotics
to treat chest infections and the more recent evolution
of better lung imaging to enable earlier treatment of
pneumonia before complications, such as lung abscess
and pneumonia arose [1]. Figures from Canada in the
1980s put the incidence of children hospitalized with
a lung abscess at 0.7 per 100,000 [5]. Lung abscess
may occur at any age but is thought to be less common
in the neonatal period [1]. However, this may change
with the increasing shift of neonatal care to support in-
fants at the extreme of viability and the resulting inva-
sive techniques (e.g. central venous lines for parenteral
nutrition) to support these technology dependent chil-
dren, often with signicant neurocognitive and physical
disabilities [1,2,6].
4. Predisposing factors
A lung abscess may arise fromaspiration of infected
uid, aspiration of non-infected uid which triggers a
chemical irritation (e.g. acidic gastric uids), a primary
bacterial lung infection, hematogenous spread of bacte-
ria (e.g. bacterial endocarditis of the right sided cham-
bers of the heart) or contiguous spread of infection from
a neighboring organ [1,3]. Pulmonary aspiration may
be the central factor in the evolution of a lung abscess.
Whether this occurs acutely in a previously well child
who has inhaled brackish, infected water or in a debil-
itated child with recurrent aspiration of upper airway
secretions and saliva or gastric contents, aspiration is a
common initial step in the progression frompneumoni-
tis to pneumonia to lung abscess. Specically, predis-
posing factors in well children in adolescence include
anesthesia, head injury with impaired cognition, exces-
sive sedation or alcohol ingestion, poor dental hygiene
together with poor gingival status that may be seen in
children receiving anticonvulsants [13]. The signi-
cance of the introduction of oral ora into the lung is
that the bacteria are predominantly anaerobic and this
will alter the antibiotic approach [3,6]. It is worth not-
ing that lung abscess is rare in neonates and also may
be associated with predisposing factors such as lung
cyst, pneumonia, cognitive impairment or the presence
of central venous lines. Again, the early symptoms and
signs may be non-specic [13].
In the child with ongoing pulmonary aspiration, it is
the impaired mucociliary defense mechanisms, which
increase the likelihood of pulmonary morbidity and
mortality [6]. These may occur for a variety of reasons,
which begin with pooled oral secretions and poorly co-
ordinated swallow mechanisms. Contributing to this
may include: gingival infection, neuromuscular weak-
ness, structural proximal airway abnormalities (e.g.
cleft larynx), vocal cord palsy, tracheo-bronchomalacia
and signicant thoracic scoliosis [2,3,6]. Converse-
ly, there may be signicant gastro-esophageal reux
of acidic stomach contents and pulmonary aspiration
of these uids. Indeed, it is often gastro-esophageal
reux, which is the focus of investigations and inter-
ventions such as gastrostomy tube insertion and fun-
doplication of the stomach. The role of fundoplication
may have been over-emphasized previously as there is
now a trend toward inserting gastrostomy tubes with-
out fundoplication in the absence of documented evi-
dence of reux [6]. This is a reasonable approach, but
it is important to consider the possibility of inducing
gastro-esophageal reux following gastrostomy feeds
at higher volumes (e.g. bolus feeds as opposed to lower
volumes given as continuous overnight feeds) [6].
Additional factors to consider in a previously well
child include the case of a bacterial pneumonia which
often follows an otherwise unremarkable viral upper
respiratory tract infection [1,2,4]. The presumed bac-
terial infection may or may not have been treated along
the course of progressing to a lung abscess. Alterna-
tively, the child may have developed bacterial endo-
carditis, more commonly on an abnormal heart valve
or in a structurally abnormal heart, which has sent off
septic emboli to the lungs (Table 1) [1,2,57].
H. Alsubie and D.A. Fitzgerald / Lung abscess in children 29
Table 2
Common pathogens in lung abscesses
Classication Pathogen
Aerobic Gram-positive cocci Streptoococcus pneumoniae
Staphylococccus aureus
Aerobic Gram-negative Pseudomonas aeruginosa
bacilli Klebsiella pneumoniae
Anaerobic cocci Peptostreptococcus,
Microaerophilic streptococci
Anaerobic Gram-negative Bacteroides species
bacilli Prevotella, Fusobacterium
species
Fungus Candida albicans, Aspergillus
species
5. Pathophysiology
Once the lungs are soiled, an inammatory cascade
is triggered giving rise to the chemical pneumonitis,
which predisposes to infection. Aspiration pneumoni-
tis is an acute lung injury, which occurs after the in-
halation of regurgitated gastric contents [7]. Aspira-
tion pneumonitis, was originally described as Mendel-
sons syndrome from the adult obstetric literature [8],
is a chemical injury caused by the inhalation of sterile
gastric contents which is seen as distinct from aspira-
tion pneumonia which is an infectious process resulting
from the inhalation of oropharyngeal secretions which
are colonized by pathogenic bacteria [7]. There is con-
siderable overlap between these conditions and it may
be difcult to distinguish them in the clinical setting.
Nonetheless, both may contribute to the subsequent de-
velopment of the relatively uncommon complication of
lung abscess (Table 2).
Aspiration pneumonitis is seen in children with a
marked disturbance of consciousness which may be
seen in conditions including: status epilepticus, hypox-
ic and metabolic encephalopathies, catastrophic cere-
brovascular events, cerebral trauma as well as patients
with severe neurocognitiveimpairment of uncertaineti-
ology, often referred to as having cerebral palsy [4,6,
7]. It is a recognized complication of general anesthe-
sia for any operative procedure and may occur despite
all appropriate anesthetic precautions [6,7]. Again, in
the adult literature, a correlation between the level of
impaired consciousness as measured by the Glasgow
Coma Scale and the risk of aspiration was demonstrat-
ed [9]. It has been suggested that a gastric aspirate pH
of less than 2.5 and a volume of greater than 0.3 mL
per kilogramof body weight are required for the devel-
opment of aspiration pneumonitis in adults [7]. There
is no corresponding data for children. However, the
stomach contents contain other irritants besides gas-
tric acid and so it is possible to cause an inammatory
response without highly acidic uid [710].
It is likely that the number of episodes of aspira-
tion, the volume of aspirated material and any impair-
ment of mucociliary clearance mechanisms contribute
to the development of a lung abscess [1,2,6,7]. The
time course for progression from aspiration to pneu-
monia and abscess is not rapid. Indeed, the course is
somewhat insidious, especially in childrenwith chronic
low-grade cough related to impaired mucociliary clear-
ance. Interestingly, it takes days before the symptoms
and signs develop even after a known aspiration event
has occurred, because the bodys host defense mecha-
nisms may decrease perfusion to an area of aspiration
and thereby reduce the inux of defense mediators and
the egress of infective material [57]. Animal work
has demonstrated that there is a biphasic response after
acid aspiration [10].
A lung abscess may arise from embolic phenomena
such as right-sided bacterial endocarditis, more likely
in children with right-sided heart valve abnormalities
and post-surgery or the placement of a central venous
line [2,6,7]. Rarely, children with septicemia may have
foci in the lung from hematogenous spread or from
thrombophlebitis with septic emboli. In addition, lo-
cal extension from pharyngeal abscesses or abdominal
collections is also seen [7].
In the case of a single small lung abscess, the changes
in ventilation and perfusion may be minimal. As the
abscess grows there may be more signicant changes
in ventilation and perfusion, resulting in hypoxemia
and tachypnea. With the evolution of pleuritic pain
from pleural inammation, there may be a restrictive
component to lung function due to the loss of lung
volume and reduced lung compliance [1].
6. Clinical presentation
The presentation of lung abscess may be insidious,
typically evolving over two weeks in a child with fever
and cough. Other features may include chest pain, dys-
pnea, sputum production and hemoptysis (Table 3) [1,
2,5]. The physical ndings may range from no de-
tectable abnormality in the chest to signs of consolida-
tion (Table 4). Not infrequently, the diagnosis is made
on a chest radiograph as an investigation in a child with
a persisting cough where a well-circumscribed shadow
is seen containingan air-uid level [2]. This is more of-
ten the case in children with a primary lung abscess [1,
2,11].
30 H. Alsubie and D.A. Fitzgerald / Lung abscess in children
Table 3
Symptoms reported in several series for children with a lung abscess
Parameters Ho et al. [2] Tan et al. [18] Chan et al. [24] Yen et al. [25]
(n = 23) (n =23) (n =27) (n = 23)
Fever 83% 84% 100% 91%
Cough 65% 53% 67% 87%
Dyspnea 36% 35% 19% 35%
Table 4
Clinical signs elicited in children with primary and secondary lung abscess fromthe Childrens
Hospital at Westmead (19852001) [2]
Parameters Primary lung abscess Secondary lung abscess
(n = 29) (n =14)
Tachypnea 100% 71%
Dull percussion note or reduced air entry 44% 79%
Fever 44% 50%
Localized crepitations 33% 36%
In contrast, a child with a secondary lung abscess is
more likely to have underlyingmedical problems. Such
problems may include recurrent pulmonary aspiration
of saliva and upper airway secretions, debilitation, sig-
nicant neuron-cognitive disability, dysphagia, naso-
gastric tube feeding, seizure disorders, altered levels
of consciousness, congenital or acquired immunode-
ciency states and congenital abnormalities of proximal
airway structures [11]. In vulnerable individuals, the
presence of poor oral hygiene predisposes to aspiration
pneumonia, lung abscess and empyema with anaerobic
organisms [7].
7. Microbiology
The pathogens causing a lung abscess may be classi-
ed as being aerobic, anaerobic or fungal. More com-
monly isolated pathogens are listed in Table 1. In addi-
tion to Staphylococcus aureus, one should also consider
group B Streptococcus, Escherichia coli and Klebsiella
pneumoniae in young infants [1]. However, with age,
the likelihood of predisposing factors to lung abscess
increases and therefore the likelihood of an anaerobic
pathogen increases. From the work in the 1970s, us-
ing trans-tracheal aspiration, studies demonstrated that
anaerobic bacteria accounted for 6080% of lung ab-
scess, with Peptostreptococcus species, Fusobacterium
nucleatumand Prevotella melaninogenica predominat-
ing [1215]. These bacteria matched known oral ora,
which had been implicated by Dr David Smith at Duke
University in the pre-antibiotic era of the 1920s [15].
In children with aspiration pneumonia, the likelihood
of yielding an anaerobic organism was reported to be
as high as 90% in trans-tracheal aspirates evaluated in
a cohort of 74 children with aspiration pneumonia: 52
with pneumonitis, 12 with necrotizing pneumonia and
10 with a lung abscess [12]. Interestingly, an average
of 4.9 organisms per aspirate was isolated (2.7 anaer-
obes and 2.2 aerobes) in that study. It is not uncommon
to isolate multiple organisms from lung abscesses and
more commonly in secondary lung abscesses [1217].
This is not only related to how the specimen is col-
lected, percutaneous or trans-tracheal versus purulent
sputum or unprotected bronchial brushings where con-
tamination with oral ora may occur [1214]. Anaer-
obes are more common in patients who are predisposed
to aspiration, such as with dental caries, seizure dis-
orders and impaired co-ordination of swallowing [13
16]. In a cohort of adults presenting with acute lung
abscess in South Africa in the early 1990s, 29 of 34
patients had predisposing factors for lung abscess (i.e.
secondary lung abscess). In these subjects, anaerobes
accountedfor 74%of the bacterial yield, and apart from
those subjects with tuberculosis, the bacterial cultures
obtained consisted of anaerobes alone in 52% and of
aerobes alone in only 22% [17]. In a pediatric sample
of patients presenting with an acute lung abscess from
Zimbabwe in 1992, more aerobic organisms were cul-
tured, especially S. aureus, reecting different risk fac-
tors for lung abscess (e.g. post-viral lower respiratory
tract infection) and the higher proportion of primary
lung abscesses seen [17].
Importantly, the key issues are to consider the likeli-
hood of anaerobic pathogens, to attempt to obtain un-
contaminated purulent material fromthe abscess cavity,
culture the pus in appropriate anaerobic media and treat
accordingly. The sensitivity of some obligate anaer-
obes to die when exposed to air will undermine attempts
to isolate causal anaerobic bacteria and so a liquid spec-
H. Alsubie and D.A. Fitzgerald / Lung abscess in children 31
imen of pus is best injected directly after aspiration into
an oxygen-free (anaerobic) transport vial [11].
8. Imaging
The basic diagnostic test for lung abscess is the chest
radiography, which typically demonstrates an air-uid
level within a spherical area of consolidation (Fig. 1).
The possibility of lung abscess is greater in the de-
pendent areas of lung, which are more prone to reect
pulmonary aspiration, specically the posterior upper
lobe or the superior lower lobe [11]. In one series of
45 lung abscesses in subjects aged from 1 month to 28
years, the distribution was as follows: right upper lobe
(36%), right lower lobe (33%), right middle lobe (24%)
and left upper lobe (9%). Eleven of the 45 subjects had
involvement of more than one lobe and in 16% of all
cases; a pleural effusion was demonstrated [18]. This
important data was gathered from one large US centre
over nearly 14 years (19821993). The data present-
ed, when contrasted with current practice, highlights
how the role of interventional radiology has come to
the fore in the role of management of lung abscess, the
role of computerized tomography(CT) guided imaging
has improved and the duration of inpatient stay has re-
duced. Today, not withstanding concerns about the use
of ionizing radiation, low dose, contrast-enhanced CT
scans are usually considered to be the investigation of
choice to distinguish lung abscess from an empyema,
necrotizing pneumonia with a pneumatocele, seques-
tration or underlying congenital abnormality such as
bronchogenic cyst [24]. This is particularly relevant
if image guided drainage is considered to distinguish
between necrotizing pneumonia and lung abscess [4].
The characteristic appearance of a lung abscess on
a CT image is shown in Figs 2a and 2b. In particular,
the thick-walled cavity contains mobile, central uid
occurring in the midst of an area of consolidated lung.
An air-uid level is often apparent on the CT scan,
even when it may not be evident on the plain chest
radiograph [19]. Magnetic resonance imaging scans
offer no diagnostic advantage over CT scans and are
not routinely used in most centers for investigation and
treatment of lung abscess as the resolution provided is,
at present in clinical practice, not as helpful as the CT
imaging [19].
Fig. 1. Chest radiograph of a lung abscess in the right upper lobe.
8.1. The role and type of interventional approach
The traditional mode of therapy has involved intra-
venous antibiotic treatment with a lengthy hospital stay
followed by several weeks of enteral antibiotics [1,3,
20]. The alternative was surgery, usually with a lobec-
tomy or segmentectomy where possible [1,5]. Howev-
er, this was not a simple procedure and came with sig-
nicant morbidity and some mortality, particularly in
patients with predisposing conditions for a secondary
lung abscess [1]. Consequently, the involvement of
interventional procedures in the management of lung
abscess became established [4].
The aspiration of lung abscesses with or without an
external drain under CT guidance for large, peripheral-
ly located abscesses has been used in the pediatric pop-
ulation since the 1980s, with reports of improved suc-
cess rates, reduced morbidity and mortality [2]. Nee-
dle aspiration under image guidance has been used for
many years with success for diagnostic and therapeutic
purposes, but lacks the utility of a small percutaneous
drain (pigtail catheter) which may drain the collection
for several days if required. Originally, the concept
of CT-guided drainage and the insertion of a pigtail
catheter for lung abscess and empyema were consid-
ered when medical therapy had failed or for rapid di-
agnostic and therapeutic benet in patients considered
too unwell for surgery [2123]. With experience, the
practice has broadened to the point where intervention-
al radiology is considered the standard of care where
such expertise is available [2]. This has been suggest-
ed to result in more rapid defervescence of fever and
symptoms, shorter periods of intravenous antibiotics
32 H. Alsubie and D.A. Fitzgerald / Lung abscess in children
(a)
(b)
Fig. 2. (a) Computerized tomography scan image of a lung abscess,
(b) Computerized tomography scan imaging assisting in the place-
ment of a pigtail catheter drain.
and a decreased length of inpatient care [2]. However,
there does remain a role for surgery in selected cases.
In a recent series of 27 cases (eight primary and 19
secondary lung abscesses occurring between 1987 and
2003) from Taiwan, lobectomy was needed in ve of
27 patients (18.5%) [24]. In this series, surgical in-
terventions were required in eight (42%) of 19 of pa-
tients with secondarylung abscess. In the cohort, 10/27
had ultrasound-guidedaspiration of their abscesses and
only one had CT guided aspiration [24].
By way of contrast, at the Childrens Hospital at
Westmead in Sydney, the rise in interventional radiolo-
gy over the past 20 years has resulted in routine use of
CT-guided aspiration for abscesses and, in more recent
years, in the use of CT-guided pigtail drainage catheters
at the time of presentation. This has translated into a
higher proportion of positive cultures overall, with a
Table 5
Antibiotic treatment doses
Intravenous antibiotics Dose [26]
Benzylpenicillin (30 mg/kg up to) 1.2 g 4 to 6 hourly
Di/Flucloxacillin (50 mg/kg up to) 2 g 6 hourly
Cefotaxime 50 mg/kg 8 hourly
Ceftriaxone 50 mg/kg once daily
Clindamicin (10 mg/kg up to) 450 mg 8 hourly
Vancomycin (10 mg/kg up to) 500 mg 6 hourly
Metronidazole (12.5 mg/kg up to) 500 mg 8 to 12 hourly
Meropenem (20 mg/kg up to) 1 g 8 hourly
Derived from the Childrens Hospital at Westmead Handbook [26].
higher prevalence anaerobes, a reduced proportion of
S. aureus and Haemophilus inuenzae type b (since the
introduction of routine immunization in 1992) and a
shorter length of hospital stay than reported in previ-
ous series [2]. Most interestingly, for the 19 patients
managed exclusively in our institution (mean age 8.3
years; range 20 days to 19.5 years) between 1985 and
2000 with a primary lung abscess (n = 9), the average
length of stay in our institution was 12.4 days [95%
condence interval (CI) 8.4, 16.5] and for those with
secondary lung abscess (n =10) it was 25.1 days (95%
CI 14.6, 35.6), giving an overall average of 19.1 days
(95% CI 13.0, 25.2) [2]. Subsequently, over the past 5
years, the length of hospital stay has decreased in our
institution. Current practice at the Childrens Hospital
at Westmead in Sydney sees children presenting with
primary lung abscess managed routinely undergoing
placement of a CT-guided pigtail catheter at presenta-
tion, with 23 days of drainage, intravenous antibiotics
and discharge within 7 days on a course of oral (enteral
for those managed with gastrostomy feeds and medi-
cations) antibiotic therapy to complete a month of total
antimicrobial therapy guided by culture results [1,2,6,
13,20].
9. Antibiotics
The choice of antibiotics (Table 5) varies somewhat
between institutions and is guided by a number of fac-
tors, including the ability to isolate organisms through
aspiration and drainage of the abscess, whether the ab-
scess is believed to be a primary or secondary phe-
nomenon, the likelihood of penicillin resistance, cost
and local practices [1,2,6,13,20,25,26]. At our in-
stitution, we initially prefer to use a third-generation
cephalosporin and ucloxacillin (or clindamicin) un-
til the aspirated lung abscess uid culture results are
available to rationalize therapy.
H. Alsubie and D.A. Fitzgerald / Lung abscess in children 33
For primary lung abscess, antibiotic choice should
cover likely organisms including S. aureus, Streptococ-
cus pneumoniae and other streptococcal species and
gram-negative bacilli that are normally found in the up-
per respiratory tract. Therefore, the use of ucloxacillin
and cefotaxime/ceftriaxone would be appropriate start-
ing points. With the increasing threat of multiply resis-
tant S. aureus (MRSA), the role of vancomycinis likely
to increase. For patients at risk of a hospital acquired in-
fection with Klebsiella spp. or Enterobacter spp., these
are resistant to penicillin and there is an increasing risk
of antibiotic resistance to third and fourth generation
cephalosporins owing to the production of plasmid-
mediated extended-spectrum beta-lactamases. Conse-
quently, most isolates are sensitive to uoroquinolones,
trimethoprim/ sulfamethoxazole, aminoglycosides and
carbapenems (e.g. meropenem) and a combination of
a carbapemem (or uoroquinolone) with an aminogly-
coside may be appropriate [20].
For patients at risk of secondary lung abscess through
aspiration, it is important to cover anaerobes normally
found in the upper airway, with clindamicin provid-
ing coverage against these organisms as well as S. au-
reus. Alternatives could include benzylpenicillin and
metronidazole. For an immunocompromised host, an-
tibiotic coverage is broader and likely to include con-
sideration of fungal pathogen. Once the child has de-
fervesced, an oral antibiotic would replace the intra-
venous therapy and the child would be discharged on
an oral antibiotic to complete a four-week course of
treatment [1,2,13,20,25,26].
10. Clinical course
If intravenous antibiotics alone are used, the fever
may resolve in seven to ten days and the illness resolves
within a further two weeks [1,5]. It is our experience
that the use of interventional radiology has since ap-
proximately halved the length of hospitalization from
our gures from 1985 to 2000 of 12.4 days for a pri-
mary lung abscess and 25 days for a secondary lung
abscess [2]. The use of percutaneous aspiration or pig-
tail catheter drainage (Fig. 3) shortens the course of
the illness considerably and probably has an associated
cost saving allowing for the costs of anesthesia and in-
terventional procedures given the costs of intravenous
therapies and hospital bed days [2]. More importantly,
a shorter hospital stay is better for the children and their
families [1,2].
Fig. 3. Transcutaneous drain in situ in treatment of a lung abscess
(Photo courtesy of Dr David Lord).
The rate of resolution of the abscess cavity lags be-
hind the clinical resolution of the abscess. In fact,
whilst children would routinely receive another 3weeks
of oral antibiotics after discharge, the abscess cavity
on the chest radiograph may persist for months to even
years after appropriate therapy [1]. Pulmonary function
typically returns to baseline [5].
10.1. Complications
In the pre-antibiotic era, a lung abscess was fatal in
30% to 40% of cases [1]. In contrast, whilst deaths
due to lung abscess still occur in children, they are be-
lieved to be infrequent for primary lung abscess but
more common in secondary lung abscess. Deaths are
more commonly reported in cases of secondary lung
abscess where host factors (e.g. malnutrition in patients
in the developing world; immunodeciencies or malig-
nancies) are more likely to determine the outcome in
cases [1]. In our experience, there have been no deaths
from lung abscess in the last 20 years [2], yet in a sim-
ilar time period from Taiwan there were 5/27 (18.5%)
of patients who died due to the severity of their under-
lying conditions [21]. The series fromTaiwan reported
34 H. Alsubie and D.A. Fitzgerald / Lung abscess in children
Table 6
Complications of lung abscess
Spontaneously rupture into adjacent compartment
Empyema, pyothorax or pneumothorax
The connection between the abscess cavity and the pleural space
Bronchopleural stula
Hematogenous spread leading to multiple abscesses
Anesthesia complication:
Aspiration, reaction, post-op nausea and fever
Radiation exposure:
Computerized tomography scans, chest radiographs
Reaction to antibiotics:
Fever, rash or anaphylaxis
Site scar
a complication rate of 41%, which included respiratory
failure (6/27), pneumothorax (3/27), shock (1/27), os-
teomyelitis (1/27) and colon perforation (1/27). In ad-
dition, four surviving patients had sequelae (2/27 with
bronchiectasis and 2/27 with lung brosis) [24].
Spontaneous complications described include over-
expansion of the abscess with lung compression and
mediastinal shift, tension pneumothorax after abscess
wall rupture into the pleural space and spontaneous
rupture of the abscess with seeding to other parts of the
lung [1].
Complications leading to signicant morbidity may
also occur and are more likely to result from interven-
tions than to the underlying disease process [1]. These
may include abscess rupture and intrabronchial spread
of pus at the time of evaluation with bronchoscopy,
bleeding and subcutaneous emphysema from transtra-
cheal needle aspiration. Transcutaneous drainage may
be associated with pneumothorax or the development
of a broncho-pleural stula will require insertion of a
pleural drain for a number of days with the likely result
of spontaneous closure without surgical intervention [3,
4]. Lobectomy has been associated with empyema and
pleural effusion (Table 6) [1]. In western centers, the
standard management of empyema includes the use of
imaging and removal of pus fromthe pleural space with
interventional radiology or surgical intervention with
video-associated thoracoscopic surgery [22]. There is
no xed length of antibiotic therapy, but most clini-
cians would provide for a total of four to six weeks of
antibiotic treatment, with the initial 510 days being
delivered intravenously to coincide with drainage, and
the balance orally as an outpatient [23].
10.2. Long term outcome
The prognosis for children with primary lung abscess
is overwhelmingly favorable. In adults, the morbidity
with lung abscess is reported as being 1520% [24],
whereas in children the mortality is signicantly lower,
probably of the order of less than 5% and occurs pre-
dominantlyin those with a secondarylung abscess [21].
It is the co-morbidity of the predisposing conditions in
both adults and children that contributes to the worse
prognosis and higher mortality rate. Consequently, al-
most all immunologically competent children with a
primary lung abscess would be expected to recover,
whereas those with predisposing conditions, predom-
inantly immunocompromised states, would expect to
fare signicantly worse [1,2,18,21,24,25].
References
[1] M.I. Asher and A.M. Leversha, Lung abscesses, in: Kendigs
Disorders of the Respiratory Tract in Children, (6th ed.), V.
Chernick, T.F. Boat and E.L. Kendig, eds, Philadelphia: WB
Saunders, 1998, pp. 552560.
[2] P. Patradoon-Ho and D.A. Fitzgerald, Lung abscess in chil-
dren, Paediatr Resp Rev 8 (2007), 7784.
[3] P.S. Puligandla and J.M. Laberge, Respiratory infections:
pneumonia, lung abscess, and empyema, Semin Pediatr Surg
17 (2008), 4252.
[4] F.A. Hoffer, D.A. Bloom, A.A. Colin and S.J. Fishman, Lung
abscess versus necrotizing pneumonia: implications for inter-
ventional therapy, Pediatr Radiol 29 (1999), 8791.
[5] M.I. Asher, S. Spier, M. Beland, A.L. Coates and P.H. Beaudry,
Primary lung abscess in childhood: the long term outcome of
conservative management, Am J Dis Child 136 (1982), 492
496.
[6] D.A. Fitzgerald, J. Follett and P.P. van Asperen, Lung disease
and sleep problems in children with cerebral palsy, Pediatr
Respir Reviews (in press).
[7] P.E. Marik, Aspiration pneumonitis and aspiration pneumonia,
N Engl J Med 344 (2001), 665671.
[8] C.L. Mendelson, The aspiration of stomach contents into the
lungs during obstetric anaesthesia, Am J Obstet Gynecol 52
(1946), 191205.
[9] F. Adnet and F. Baud, Relation between Glasgow Coma Scale
and aspiration pneumonia, Lancet 348 (1996), 123124.
[10] T.P. Kennedy, K.J. Johnson, R.G. Kunkel, P.A. Ward, P.R.
Knight and J.S. Finch, Acute acid aspiration lung injury in the
rat: biphasic pathogenesis, Anesth Analg 69 (1989), 8792.
[11] I. Brook, Anaerobic pulmonary infections in children, Pediatr
Emerg Care 20 (2004), 636640.
[12] I. Brook and S.M. Finegold, Bacteriology of aspiration pneu-
monia in children, Pediatrics 65 (1980), 11151120.
[13] I. Brook and S.M. Finegold, Bacteriology and therapy of lung
abscess in children, J Pediatr 94 (1979), 1012.
[14] J.G. Bartlett and S.M. Finegold, Anaerobic infections of the
lung and pleural space, AmRev Respir Dis 110 (1974), 5677.
[15] J.G. Bartlett, The role of anaerobic bacteria in lung abscess,
Clin Infect Dis 40 (2005), 923925.
[16] J.M. Hammond, P.D. Potgieter, D. Hanslo, H. Scott and D.
Roditi, The etiology and antimicrobial susceptibility patterns
of microorganisms in acute community-acquired lung abscess,
Chest 108 (1995), 937941.
[17] J.K. Tumwine, Lung abscess in children in Harare, Zimbabwe,
East Afr Med J 69 (1992), 547549.
H. Alsubie and D.A. Fitzgerald / Lung abscess in children 35
[18] T.Q. Tan, D.K. Seilheimer and S.L. Kaplan, Pediatric lung
abscess: clinical management and outcome, Pediatr Infect Dis
J 14 (1995), 5155.
[19] J.F. Johnson, W.E. Shiels, C.B. White and B.D. Williams, Con-
cealed pulmonary abscess: diagnosis by computed tomogra-
phy, Pediatrics 78 (1986), 283286.
[20] E. Bouza and E. Cercenado, Klebsiella and enterobacter: an-
tibiotic resistance and treatment implications, Semin Respir
Infect 17 (2002), 215230.
[21] B. Hirshberg, M. Sklair-Levi, R. Nir-Paz, L. Ben-Sira, V.
Krivoruk and M.R. Kramer, Factors predicting mortality of
patients with lung abscess, Chest 115 (1999), 746750.
[22] S. Sonnappa, G. Cohen, C.M. Owens et al., Comparison of
urokinase and video-assisted thoracoscopic surgery for treat-
ment of childhood empyema, Am J Respir Crit Care Med 174
(2006), 221227.
[23] S. Sonnappa and A. Jaffe, Treatment approaches for empyema
in children, Paediatr Respir Rev 8 (2007), 164170.
[24] P.C. Chan, L.M. Huang, P.S. Wu et al., Clinical management
and outcome of childhood lung abscess: a 16-year experience,
J Microbiol Immunol Infect 38 (2005), 183188.
[25] C.C. Yen, R.B. Tang, S.J. Chen and T.W. Chin, Pediatric
lung abscess: a retrospective review of 23 cases, J Microbiol
Immunol Infect 37 (2004), 4549.
[26] D. Isaacs and H. Kilham, The Childrens Hospital at Westmead
Handbook, Sydney: McGraw Hill, North Ryde, 2004.
You might also like
- VVF Clinical Presentation 1Document24 pagesVVF Clinical Presentation 1georgeloto12No ratings yet
- 05 N107 33940Document33 pages05 N107 33940Mohammed AfzalNo ratings yet
- Chronic Otitis MediaDocument4 pagesChronic Otitis MediaOvyanda Eka MItraNo ratings yet
- PharingitisDocument68 pagesPharingitisSwarantika Aulia RarasatiNo ratings yet
- 02 Bronchial Asthma Circ 2018-2019Document15 pages02 Bronchial Asthma Circ 2018-2019Mooha Alanzy100% (1)
- Pediatric Ist SeminarDocument21 pagesPediatric Ist SeminarAsha jiluNo ratings yet
- A Study of Inguinal Hernia in ChildrenDocument5 pagesA Study of Inguinal Hernia in ChildrenrhmathidayatNo ratings yet
- National Anaemia Prophylaxis Programme Reduces Maternal MortalityDocument15 pagesNational Anaemia Prophylaxis Programme Reduces Maternal MortalityAnkit TalujaNo ratings yet
- Salbutamol Sulphate Inhaler for Asthma ReliefDocument5 pagesSalbutamol Sulphate Inhaler for Asthma ReliefRajib MandalNo ratings yet
- Managing Diarrhea in Under-5sDocument15 pagesManaging Diarrhea in Under-5skuruvagadda sagarNo ratings yet
- MethergineDocument3 pagesMethergineJohn AlanoNo ratings yet
- The Pathophysiology of PPROMDocument2 pagesThe Pathophysiology of PPROMNano KaNo ratings yet
- Lesson Plan On DNSDocument10 pagesLesson Plan On DNSFeel AmazedNo ratings yet
- Nursing Care PneumoniaDocument26 pagesNursing Care PneumoniaIsaac Kipkemoi100% (1)
- Case Presentation HydrocephalusDocument48 pagesCase Presentation HydrocephalusSu Osman50% (2)
- Hookworm Diseases: (Ancylostomiasis /Miner'S Disease/Egyptian Chlorisis)Document21 pagesHookworm Diseases: (Ancylostomiasis /Miner'S Disease/Egyptian Chlorisis)Mel Izhra N. Margate100% (1)
- Aerosol Therapy TMK 1Document34 pagesAerosol Therapy TMK 1Inna DoroshkevychNo ratings yet
- Case Study of HypospadiaDocument19 pagesCase Study of Hypospadialicservernoida100% (2)
- Case PresentationDocument46 pagesCase PresentationAileen DometitaNo ratings yet
- Patient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDocument93 pagesPatient Scenario, Chapter 45, Nursing Care of A Family When A Child Has A Gastrointestinal DisorderDay MedsNo ratings yet
- Chronic Kidney DiseaseDocument7 pagesChronic Kidney DiseaseLardel Balbiran LafortezaNo ratings yet
- Pleural Effusion: Presented By:-Gayathri Gopakumar BSC - Nursing 2 YearDocument30 pagesPleural Effusion: Presented By:-Gayathri Gopakumar BSC - Nursing 2 YearGAYATHRI GOPAKUMARNo ratings yet
- Pyeloplasty (Anderson-Hynes)Document12 pagesPyeloplasty (Anderson-Hynes)HardiTariqHammaNo ratings yet
- Pediatric - 18.04.20-Child Guidance ClinicDocument29 pagesPediatric - 18.04.20-Child Guidance ClinicAjeeshNo ratings yet
- Acute Rheumatic Fever Causes, Symptoms and TreatmentDocument49 pagesAcute Rheumatic Fever Causes, Symptoms and Treatmentbereket gashuNo ratings yet
- SUCADENUMDocument9 pagesSUCADENUMmayliaNo ratings yet
- National Health Programmes For Children in IndiaDocument79 pagesNational Health Programmes For Children in IndiashahnazNo ratings yet
- Childhood Lymphoma Types, Stages, and TreatmentDocument42 pagesChildhood Lymphoma Types, Stages, and TreatmentPriyaNo ratings yet
- Hookworm Disease: Ancylostoma Duodenale-Are Anthropophilic Human Hookworms Transmitted From Infected SoilDocument5 pagesHookworm Disease: Ancylostoma Duodenale-Are Anthropophilic Human Hookworms Transmitted From Infected SoilBrix Valdriz100% (1)
- Understanding Diarrhea: Causes, Symptoms, Prevention and ManagementDocument12 pagesUnderstanding Diarrhea: Causes, Symptoms, Prevention and ManagementSoumya RajeswariNo ratings yet
- Displacement of The UterusDocument32 pagesDisplacement of The UterusRaja100% (1)
- Rheumatic FeverDocument3 pagesRheumatic FeverKennette LimNo ratings yet
- ContractedDocument15 pagesContractedswapnil3250No ratings yet
- National Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaDocument53 pagesNational Guidelines On Management of Dengue Fever & Dengue Haemorrhagic Fever in Children and Adolescents - Sri LankaNational Dengue Control Unit,Sri Lanka100% (1)
- Abnormal LabourDocument7 pagesAbnormal LabourSaman SarKo0% (1)
- Acute Respiratory FailureDocument19 pagesAcute Respiratory Failurek uche100% (1)
- Diarrhea: DefinitionDocument13 pagesDiarrhea: Definitionudaybujji100% (1)
- The Pathophysiology of LabyrinthitisDocument2 pagesThe Pathophysiology of LabyrinthitisSurya Michael ChanceNo ratings yet
- Neurological AssessmentDocument5 pagesNeurological AssessmentVIDYANo ratings yet
- ChemotherapyDocument11 pagesChemotherapyRekha G.No ratings yet
- K6 - Tetanus PEDIATRICDocument23 pagesK6 - Tetanus PEDIATRICbanuperiahNo ratings yet
- Assessments of NewbornDocument8 pagesAssessments of NewbornYashoda SatputeNo ratings yet
- Hypospadias and Epispadias 1Document35 pagesHypospadias and Epispadias 1Corey100% (1)
- HydronephrosisDocument6 pagesHydronephrosisJamaluddin Ahmad A.MNo ratings yet
- Ob Nursing Care Plan For Maternal Database Maternal and NewbornDocument2 pagesOb Nursing Care Plan For Maternal Database Maternal and Newbornapi-403051801No ratings yet
- Respiratory Disorder Note BSC 3rd YearDocument41 pagesRespiratory Disorder Note BSC 3rd YearNancyNo ratings yet
- Immediate Physiological Changes in New BornDocument7 pagesImmediate Physiological Changes in New BornLahunWanniangNo ratings yet
- Care PlanDocument4 pagesCare PlangopscharanNo ratings yet
- PBBN 1St Yr Child Health Nursing CBIMNCIDocument29 pagesPBBN 1St Yr Child Health Nursing CBIMNCIcopy smart100% (1)
- Nephrotic SyndromeeDocument28 pagesNephrotic SyndromeeRiteka SinghNo ratings yet
- ILEOSTOMYDocument11 pagesILEOSTOMYShine Khay100% (1)
- Respiratory Distress SyndromeDocument41 pagesRespiratory Distress Syndromef.abrahamNo ratings yet
- Chronic Kidney Disease: Presented By, Mariya Antony 3 Year BSC Nursing ST - Thomas College of Nursing ChethipuzhaDocument62 pagesChronic Kidney Disease: Presented By, Mariya Antony 3 Year BSC Nursing ST - Thomas College of Nursing ChethipuzhaSamuel LalNo ratings yet
- Fetal DistressDocument37 pagesFetal DistressRp NdaNo ratings yet
- Drugs Study For PneumoniaDocument5 pagesDrugs Study For PneumoniaLucelle ArellanoNo ratings yet
- CcroupDocument53 pagesCcroupOlivia BernadiNo ratings yet
- Pelvic Inflammatory DiseaseDocument3 pagesPelvic Inflammatory DiseaseokaciaNo ratings yet
- Presented By: Gayramara Arben John ZDocument36 pagesPresented By: Gayramara Arben John ZgoykicoshenNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesFrom EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNo ratings yet
- Connatal Localized Neuroblastoma: The Case To Delay TreatmentDocument7 pagesConnatal Localized Neuroblastoma: The Case To Delay TreatmentCaballero X CaballeroNo ratings yet
- Reporte Anual UsaDocument184 pagesReporte Anual UsaCaballero X CaballeroNo ratings yet
- Disorders of CTLA 4 Expression, How They Lead To.6Document8 pagesDisorders of CTLA 4 Expression, How They Lead To.6Caballero X CaballeroNo ratings yet
- The Third Intergroup Rhabdomyosarcoma StudyDocument21 pagesThe Third Intergroup Rhabdomyosarcoma StudyCaballero X CaballeroNo ratings yet
- Current Concepts in Pediatric Philadelphia Chromosome-Positive Acute Lymphoblastic LeukemiaDocument21 pagesCurrent Concepts in Pediatric Philadelphia Chromosome-Positive Acute Lymphoblastic LeukemiaCaballero X CaballeroNo ratings yet
- Lessons From Ctla-4 Deficiency and Checkpoint Inhibition: SciencedirectDocument6 pagesLessons From Ctla-4 Deficiency and Checkpoint Inhibition: SciencedirectCaballero X CaballeroNo ratings yet
- Blood 745174Document11 pagesBlood 745174Caballero X CaballeroNo ratings yet
- Wagner Bohn2006Document6 pagesWagner Bohn2006Caballero X CaballeroNo ratings yet
- Managing Tumor Lysis Syndrome.2Document4 pagesManaging Tumor Lysis Syndrome.2Caballero X CaballeroNo ratings yet
- J 1365-2141 2010 08143 XDocument9 pagesJ 1365-2141 2010 08143 XekanovicaNo ratings yet
- $Ojxqdvrevhuydflrqhvvreuhodklvwruldghoolqirpdgh+Rgjnlq: $uwtfxorghuhylvlyqDocument5 pages$Ojxqdvrevhuydflrqhvvreuhodklvwruldghoolqirpdgh+Rgjnlq: $uwtfxorghuhylvlyqCaballero X CaballeroNo ratings yet
- NHL MTX BFM 95 Blood2004Document12 pagesNHL MTX BFM 95 Blood2004Caballero X CaballeroNo ratings yet
- GemcitabineDocument6 pagesGemcitabineCaballero X CaballeroNo ratings yet
- Siopel 4 Protocol 1Document156 pagesSiopel 4 Protocol 1Caballero X CaballeroNo ratings yet
- Fiebre y Neutropenia 2Document8 pagesFiebre y Neutropenia 2Caballero X CaballeroNo ratings yet
- Pediatric GuidelinesDocument334 pagesPediatric GuidelinesCaballero X CaballeroNo ratings yet
- BFM B 90Document9 pagesBFM B 90Caballero X CaballeroNo ratings yet
- Neutropenia 2018 PDFDocument13 pagesNeutropenia 2018 PDFPaula SuárezNo ratings yet
- Siopel 6Document137 pagesSiopel 6Caballero X CaballeroNo ratings yet
- BFM B 90Document9 pagesBFM B 90Caballero X CaballeroNo ratings yet
- NHL MTX BFM 95 Blood2004Document12 pagesNHL MTX BFM 95 Blood2004Caballero X CaballeroNo ratings yet
- Pinda FynDocument7 pagesPinda FynCaballero X CaballeroNo ratings yet
- Rabdo OrbitarioDocument6 pagesRabdo OrbitarioCaballero X CaballeroNo ratings yet
- Pediatr Clin Na 2013 BronquiolitisDocument16 pagesPediatr Clin Na 2013 BronquiolitisCaballero X CaballeroNo ratings yet
- Congenital Diaphragmatic HerniaDocument15 pagesCongenital Diaphragmatic HerniaErico Marcel Cieza MoraNo ratings yet
- 1 s2.0 S002571251830172XDocument11 pages1 s2.0 S002571251830172XAndiie ResminNo ratings yet
- Pyothorax Treatment & StagesDocument22 pagesPyothorax Treatment & StagesAnkan Dey100% (1)
- Pediatric TB Case PresentationDocument167 pagesPediatric TB Case PresentationJannen CasasNo ratings yet
- Antibiotics in Childhood Pneumonia ReviewDocument7 pagesAntibiotics in Childhood Pneumonia ReviewTainah__100% (1)
- Thoracentesis NotesDocument39 pagesThoracentesis NotesWing YenNo ratings yet
- 1.who Shall Be Considered As Having Community-Acquired Pneumonia?Document6 pages1.who Shall Be Considered As Having Community-Acquired Pneumonia?Kristine Jade OdtujanNo ratings yet
- Antibiotics Indicated for Bacterial Aspiration PneumoniaDocument4 pagesAntibiotics Indicated for Bacterial Aspiration PneumoniaangelicaNo ratings yet
- NCP - Or-Rotation 2Document12 pagesNCP - Or-Rotation 2Vian RiveraNo ratings yet
- Parapneumonic Effusion - Case Study Adult IDocument59 pagesParapneumonic Effusion - Case Study Adult IJunior Future-Gastroenterologist Henry100% (1)
- A 19 Year Old Man With Gunshot WoundsDocument8 pagesA 19 Year Old Man With Gunshot WoundsAkhmadZainurRidlaNo ratings yet
- USG Efusi Pleura PDFDocument7 pagesUSG Efusi Pleura PDFEnvhy AmaliaNo ratings yet
- Pneumonia DR M ManiDocument69 pagesPneumonia DR M ManimaniNo ratings yet
- Empyema: By-Komal JaiswalDocument29 pagesEmpyema: By-Komal JaiswalOlga GoryachevaNo ratings yet
- IDSA Guidelines for Managing Community-Acquired Pneumonia in ChildrenDocument14 pagesIDSA Guidelines for Managing Community-Acquired Pneumonia in ChildrenAaron Nureña JaraNo ratings yet
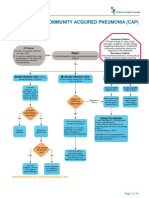
- Complicated Community Acquired Pneumonia Clinical PathwayDocument14 pagesComplicated Community Acquired Pneumonia Clinical PathwayFaisalMuhamadNo ratings yet
- CR Piopneumothoraks Nicky FIXdDocument62 pagesCR Piopneumothoraks Nicky FIXdPutri RahmawatiNo ratings yet
- Chronic Pulmonary Aspergillosis An Updated On Diagnosis and TreatmentDocument13 pagesChronic Pulmonary Aspergillosis An Updated On Diagnosis and TreatmentCahrun CarterNo ratings yet
- CopdDocument89 pagesCopdVijayalaxmi KathareNo ratings yet
- CIM by Shahid Zafar LNCONDocument3 pagesCIM by Shahid Zafar LNCONJalil KhanzzNo ratings yet
- Childhood Pneumonia Diagnosis and TreatmentDocument65 pagesChildhood Pneumonia Diagnosis and TreatmentYemata HailuNo ratings yet
- Liver Abscess Diagnosis and TreatmentDocument12 pagesLiver Abscess Diagnosis and TreatmentSimon Messi SiringoringoNo ratings yet
- Neumonia Pediatrics in Review 2008Document16 pagesNeumonia Pediatrics in Review 2008ERNESTO RODRIGUEZ SARASTY.No ratings yet
- Gilbert 1993Document14 pagesGilbert 1993Teja LaksanaNo ratings yet
- Eloesser Flap Thoracostomy WindowDocument20 pagesEloesser Flap Thoracostomy WindowJEFFRI JEFFRINo ratings yet
- Fibrinolitik On Pleural EffusionDocument19 pagesFibrinolitik On Pleural Effusionpande andikaNo ratings yet
- Investigate CAP Severity & CausesDocument27 pagesInvestigate CAP Severity & CausesRoshana Mallawaarachchi0% (1)
- Manage Child Cough, Breathing IssuesDocument18 pagesManage Child Cough, Breathing IssuesNithu NithuNo ratings yet
- EmpyemaDocument17 pagesEmpyemaNoviaCandraDwipaNo ratings yet
- Abses Hati Diagnosis dan PenangananDocument12 pagesAbses Hati Diagnosis dan PenangananSimon Messi SiringoringoNo ratings yet
- Dexamethasone For Parapneumonic Pleural Effusion A RandomizedDocument13 pagesDexamethasone For Parapneumonic Pleural Effusion A RandomizedCahrun CarterNo ratings yet