Professional Documents
Culture Documents
Clinical Progres
Uploaded by
icorrrCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clinical Progres
Uploaded by
icorrrCopyright:
Available Formats
CLINICAL PROGRESS
The roles of tissue hypoxia, blood sugar control, corticosteroid administration, and the use
of aPC in clinical outcomes have been recently subjected to clinical trials. A recent study
by Rivers et al. (!" demonstrated improved survival #ith early restoration of oxygen
transport in septic patients. $trategies for increasing oxygen delivery are discussed in
Chapters % and &'. (an den )erghe et al. (%" studied the benefit of intensive control of
blood sugar in critically ill patients. *ith intensive control of blood sugar in a group of
primarily post+operative cardiac surgery patients, mortality #as improved. The mechanism
producing benefit is not clear. ,o#+dose corticosteroids #ere sho#n to reduce mortality
in highly selected patients. These findings suggest that adrenal insufficiency may
be a part of the organ failure syndrome. Perhaps, corticosteroids are vital for the
counter+inflammatory response ('". The importance of the coagulation cascade in producing
-$./ is suggested by the aPC trial. 0n a randomi1ed controlled trial, a survival
benefit #as observed in patients #ith sepsis #ho received aPC ('2".
FUTURE CONSIDERATIONS
)asic science research has made remar3able strides in determining the path#ays at
the cellular, protein, and gene levels, #hich regulate both the initial and the secondary
inflammatory responses to infection, toxin, or ischemia. $everal lines of investigation
are #or3ing their #ay to#ard clinical trials. 4o#ever, none of the organi1ing hypotheses
alone ade5uately explains the clinical phenomena observed in critically ill patients.
Rather, they are conceptual frame#or3s that serve #ell to organi1e research data at a
reductionist level, but, #hen applied to complex clinical situations, the shortcomings of
a single unifying hypothesis are stri3ingly apparent. .ne difficulty is the concept of
sepsis and -./ as a single disease entity. )y the !66!7!66% Consensus Conference criteria,
both an 89+year+old #ith fecal peritonitis and an 8+month+old #ith otitis media can
be said to have :sepsis; (<". $hould both be entered in the same clinical trial= >et clinical
trials in :sepsis; patients are by nature beset #ith extreme selection bias problems. 0dentification
of a statistically identifiable benefit hidden in a sea of patients #ho #ill get #ell
#ithout the intervention, and patients #ho #ill sic3en and die #ith or #ithout the intervention,
poses formidable difficulties. Clearly, identifying the appropriate patient population
for trials, as #ell as for each of the therapies #e already possess, #ill be essential to
improving care. A %99! conference re+examined the definitions of sepsis, and proposed
a model of categori1ing response to infectious challenge modeled on the T?- staging
system used by oncologists (<" and designated as the P0R. model. 0n this formulation,
P is patient disposition and reflects genetic susceptibility to infection and inflammation@
0 is infection and includes site, extent, and organism(s" responsible@ R is response and
5uantifies the characteristics of the patient response to infection (by measurement of
mediators and mar3ers of inflammation" both #ith regard to an expected time course
and extent based on population studies@ and . represents organ dysfunction. The hope
is to produce a hypothesis+generating schema by staging each patient #ith sepsis/-./
in a #ay that reflects the clinical picture seen daily in 0CAs, leads to more focused use
of current therapies, and produces better designed clinical trials. The difficulties #ith restaging
patients as they progress clinically and 3eeping the model from becoming too cumbersome
for useful application #ill be challenging, but as a first step in clearly defining
patient populations for clinical trials, the model is #orthy of a strong effort.
You might also like
- Terapi Kombinasi Hipertensi Pada LansiaDocument8 pagesTerapi Kombinasi Hipertensi Pada LansiaicorrrNo ratings yet
- Medication SummaryDocument11 pagesMedication SummaryicorrrNo ratings yet
- Scarlet Fever: by Lori CarpenterDocument8 pagesScarlet Fever: by Lori CarpentericorrrNo ratings yet
- Patofisiologi DifteriDocument11 pagesPatofisiologi DifteriicorrrNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- IMSS Nursing Knowledge ExamDocument11 pagesIMSS Nursing Knowledge ExamScribdTranslationsNo ratings yet
- Vocal Health and HygieneDocument50 pagesVocal Health and HygieneclaugmailNo ratings yet
- The Welfare of Cattle Kept For Beef ProductionDocument150 pagesThe Welfare of Cattle Kept For Beef ProductionIsabel CarrilloNo ratings yet
- The Six-Step Formula for Hypnotic PersuasionDocument24 pagesThe Six-Step Formula for Hypnotic Persuasionmajadb100% (12)
- Synthesis of Novel Amino Acid Derivative of 7-AVCADocument4 pagesSynthesis of Novel Amino Acid Derivative of 7-AVCAIOSRjournal0% (1)
- Forever ARGI+® Stick Packet Product InformationDocument1 pageForever ARGI+® Stick Packet Product InformationArif Zaman SiddiqueNo ratings yet
- Surgical Services Design Guide PDFDocument465 pagesSurgical Services Design Guide PDFCharles TestaNo ratings yet
- AnupanaDocument60 pagesAnupanaVaidya Nur50% (4)
- Semen AnalysisDocument2 pagesSemen AnalysisSabir KamalNo ratings yet
- Ducharme Et Al, 1996Document20 pagesDucharme Et Al, 1996GokushimakNo ratings yet
- Cir 0000000000000899Document25 pagesCir 0000000000000899hanifa ambNo ratings yet
- NCP CompilationDocument11 pagesNCP CompilationRene John FranciscoNo ratings yet
- Mentor Interview Questions TemplateDocument3 pagesMentor Interview Questions Templateapi-381640393No ratings yet
- Mini Question Bank - Vety Sci - For Students PDFDocument106 pagesMini Question Bank - Vety Sci - For Students PDFRakesh Prajapati100% (3)
- Miyawaki Yuki Kuwahara Koei Hari Handbook of Traditional JapDocument23 pagesMiyawaki Yuki Kuwahara Koei Hari Handbook of Traditional Japкостя100% (1)
- Rife RatesDocument17 pagesRife RateszonetrekNo ratings yet
- New 5Document37 pagesNew 5rishi gupta100% (1)
- Gait Analysis: Prerequisite of Normal GaitDocument4 pagesGait Analysis: Prerequisite of Normal GaitKieran Levi100% (1)
- Human Blood CellsDocument3 pagesHuman Blood CellscsamarinaNo ratings yet
- Emergency Welfare FormDocument2 pagesEmergency Welfare FormKristopher HarperNo ratings yet
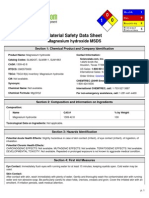
- Msds MgOHDocument5 pagesMsds MgOHCahyaGeriyanaNo ratings yet
- Abdomen ExaminationDocument37 pagesAbdomen ExaminationJaaydevNo ratings yet
- Sing With Distortion - 10 TipsDocument10 pagesSing With Distortion - 10 TipstjoodleNo ratings yet
- ArrhythmiaDocument31 pagesArrhythmiaAbdallah Essam Al-ZireeniNo ratings yet
- EveryDay AyurvedaDocument11 pagesEveryDay AyurvedacvmraviNo ratings yet
- A Devoted SonDocument1 pageA Devoted SonAnkur MaheshwariNo ratings yet
- Footnote To YouthDocument6 pagesFootnote To YouthVanityHughNo ratings yet
- Farm NoteDocument3 pagesFarm NoteSreya Sanil50% (2)
- Bapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IDocument10 pagesBapat Et Al. - 2006 - Quantification of Metabolically Active Biomass Using Methylene Blue Dye Reduction Test (MBRT) Measurement of CFU IJosé Matías ZapiolaNo ratings yet
- Jurnal Manajemen Pelayanan Kesehatan: Artikel PenelitianDocument8 pagesJurnal Manajemen Pelayanan Kesehatan: Artikel PenelitianDiah AdhyaksantiNo ratings yet