Professional Documents
Culture Documents
Cystic Thyroid
Uploaded by
abhishekbmc0 ratings0% found this document useful (0 votes)
66 views4 pagesthyroid
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentthyroid
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
66 views4 pagesCystic Thyroid
Uploaded by
abhishekbmcthyroid
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 4
Hindawi Publishing Corporation
Case Reports in Endocrinology
Volume 2012, Article ID 732715, 4 pages
doi:10.1155/2012/732715
Case Report
Unusual Presentation of Cystic Papillary Thyroid Carcinoma
Vijayraj S. Patil, Abhishek Vijayakumar, and Neelamma Natikar
Department of General Surgery, Victoria Hospital, Bangalore Medical College and Research Institute, Bangalore 560002, India
Correspondence should be addressed to Abhishek Vijayakumar, abhishekbmc@yahoo.co.in
Received 13 September 2012; Accepted 1 October 2012
Academic Editors: C. Capella and O. Isozaki
Copyright 2012 Vijayraj S. Patil et al. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Papillary thyroid carcinoma is the most common thyroid malignancy, accounting for 80% of all thyroid cancers. The most
common presentation of thyroid cancer is an asymptomatic thyroid mass or a nodule. Usually as thyroid enlarges, it extends
in to mediastinum. Papillary thyroid carcinoma presentation as multiple true cystic swelling extending from neck to anterior chest
wall in subcutaneous plane is not present in the literature. We present a rare case of cystic papillary thyroid carcinoma which is
presented as subcutaneous swelling with sinus formation.
1. Introduction
Papillary thyroid carcinoma is the most common thyroid
malignancy, accounting for 80% of all thyroid cancers [1].
The most common clinical presentation is a solitary thyroid
nodule. A pure cystic nodule, although rare (<2% of all
nodules), is highly unlikely to be malignant [2].
Cystic neck masses appearing in the anterior or posterior
triangles of the neck are usually benign. However, they may
occasionally have a sinister origin and should be investigated
rigorously [3]. Solitary cervical cystic mass is an uncommon
presentation of papillary thyroid carcinoma (PTC). Usually
as thyroid enlarges, it extends in to mediastinum due to its
anatomic location under investing layer of the deep cervical
fascia.
We report a case of papillary thyroid carcinoma pre-
sented as a multiple true cystic swelling in neck extending
over the chest in subcutaneous plane with a discharging sinus
a very unusual presentation. Papillary thyroid carcinoma
presented as multiple true cystic swelling extending from
neck to breast is not present in literature. The case was
diagnosed after surgery by histopathological examination.
2. Case Report
A 60-year-old female patient was presented with swelling
in front of the neck since 12 yrs, initially small in size
started in thyroid region and gradually increased to present
size (25 15 cm) with watery discharge form swelling of 6
months duration (Figure 1).
On examination there were multiple cystic swellings
extending from thyroid cartilage to mid sternum. There
were about 1215 cysts with features of intercommunication.
The whole swelling moved with deglutition and there was
no independent mobility of cysts. A sinus was present on
right side of neck with active serous discharge (Figure 2).
Cervical lymph nodes were not enlarged. On indirect lar-
yngoscopy, no abnormality was detected. Thyroid prole
was within normal limits. Neck and chest X-ray showed
increased soft tissue density seen in neck region extending
up to upper sternal region and indenting trachea. Fine
Needle Aspiration Cytology of the swelling showed features
suggestive of nodular goitre. Ultrasound of the neck showed
multiple anechoic areas with areas of calcication and
internal septae in the neck extending from carotid level to
midsternal level. Lesion seemed to be arising from thyroid
tissue showing minimal vascularity suggestive of multicystic
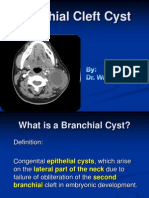
goitre or lymphangioma. On computer tomography there
were multiple uid attenuation coalescent cystic lesions in
subcutaneous plane of neck and proximal thorax. There
were no inhomogenous enhancing areas within the cyst.
Thyroid gland could not be visualized seperately from
cysts. There was no inltration of surrounding structures
or lymphadenopathy. The cystic lesions seem to be arising
from thyroid gland and only part of left lobe of thyroid
was visible (Figure 3). Patient was subjected for surgery.
2 Case Reports in Endocrinology
Figure 1: Preoperative photo multiple cysts in neck and chest with
sinus (arrow).
Figure 2: Transillumination of swelling.
Under general anesthesia Kochers horizontal incision taken
over the swelling and in middle incision extended vertically
downwards over right breast as T incision and aps raised.
Fluid in cyst was clear light brown color. Some cysts were
intercommunicated and cysts were found arising from right
lobe and isthmus of thyroid (Figure 4). On the right side
cysts were adherent to internal jugular vein [IJV] (Figure 5)
and common carotid artery (Figure 6). Internal jugular vein
was ligated and divided. Cysts were separated from right
carotid artery. Total thyroidectomy done along with excision
of all cysts and skin around sinus. Postoperative period was
uneventful (Figure 7). On histopathological examination of
specimen papillary carcinoma of thyroid was found and
sinus tract was free of tumor cells. Patient underwent
an radioactive iodine ablative postoperatively and is on
suppressive dose of thyroxine since then.
3. Discussion
The most common benign cervical cysts are branchial cleft
cysts, dermoid cysts, teratoma, epidermoid cysts, and cystic
hygromas. Due to the increasing incidence of oropharyngeal
carcinoma, cystic masses of the neck can also be metastases
from an oropharyngeal or tonsillar tumour [4]. Rarely,
PTC is presented as a cystic neck mass without palpable
lesion in the thyroid gland [5]. The origin of these cysts
Figure 3: Computer tomaographic image showing multiple cysts
arising from right lobe of thyroid.
Figure 4: Intraoperative photo showing multiple cysts.
is controversial. Some authors think that it represents a
malignant transformation of ectopic thyroid tissue others
believe they represent a secondary metastatic spread from
occult thyroid lesion to the lymph node which underwent
central liquefaction with cystic formation [6].
Papillary thyroid carcinoma is a slowly growing neo-
plasm which explains the relatively long duration in our
patient. The long duration of such cysts in young aged
patients can lead to incorrect provisional diagnosis of benign
cysts [7]. Papillary thyroid carcinoma with extrathyroidal
extension (ETE) occurs in 4% to 16% of cases and carries
with it an increased risk of disease recurrence and death [8].
Common ETEs include involvement of recurrent laryngeal
nerve, larynx, trachea, and esophagus. Involvement of skin
with sinus formation is rare, only few cases are reported [9].
High-resolution sonography is widely used to detect and
characterize thyroid nodules. Sonographic features that are
found to be associated with an increased risk of malignancy
include a predominantly solid composition, hypoechogenic-
ity, absence of a hypoechoic halo, presence of microcalcica-
tions, irregular margins, and intranodular vascularity [10].
On sonography, papillary thyroid carcinoma appears most
commonly as hypoechoic solid lesions with a smooth or
irregular contour, intrinsic vascularity, and lacks a hypoe-
choic halo. Also in a study on papillary thyroid carcinoma
by Jun et al. [11], it was shown that only 5% of lesions
were purely cystic and that 69% of all papillary thyroid
carcinomas had marked intrinsic hypervascularity: ow in
Case Reports in Endocrinology 3
Figure 5: Cyst adherent to Internal jugular vein (arrow).
Figure 6: Picture showing right carotid artery (arrow) and trachea
on removal of cysts and total thyroidectomy.
the central part of the tumor that was greater than that of the
surrounding parenchyma; 22% had perinodal vascularity.
Chan et al. [12] reported that all predominantly cystic pap-
illary thyroid carcinomas in their study had some intrinsic
blood ow. Lymph node metastases are common in patients
with papillary thyroid carcinoma, and approximately 50%
of patients have cervical lymph node metastases at the
time of their initial presentation [13]. In up to 20% of all
patients, lymph node metastases may even be the sole or
initial manifestation of disease (occult primary tumor) [14].
Approximately 40% (reported range, 2150%) of all lymph
node metastases from papillary thyroid carcinomas have
the tendency to completely cavitate a lymph node by cystic
degeneration and thus may mimic an apparently benign
cervical cyst [15].
Sonographic features of cystic papillary thyroid carci-
noma or metastatic cystic nodes include multiple or solitary
cyst with internal septation, internal nodules, and punctuate
calcication. Histologically, the internal septations were
either caused by solid, papillary structures on brovascular
stalks, by connective tissue laments, or by the remaining
streaks of lymphoid tissue (residual after the liquefaction
Figure 7: Postoperative photo.
necrosis or accompanying intranodal hemorrhage). The pap-
illary structures on brovascular stalks are especially known
to be typical for papillary thyroid carcinomas and are
associated with psammoma bodies and paucity of colloid in
the primary tumors [16]. The sonographic visible internal
nodules were either caused by partly organized colloid or
thyroid tumor cells forming follicles with subsequent colloid
production, by (partly) organized intranodal hemorrhage
and debris, or by clusters of remaining lymphoid tissue
surrounded by carcinomatous elements.
According to consensus guidelines on the management
of thyroid nodules detected on sonography, with a specic
focus on which nodule should undergo sonographically
guided FNA by Society of Radiologists in Ultrasound (SRU)
[10]. Predominantly cystic nodules (>75% cystic) without
microcalcications have a very low likelihood of malignancy.
Similarly, lack of internal ow on color Doppler imaging
suggests a lower likelihood of malignancy. As a result, the
consensus statement did not recommend FNA for cystic or
almost completely cystic nodules [10]. FNAC is less sensitive
in the diagnosis of cystic neck masses compared with solid
masses having a false negative rate ranging from 50% to 67%
[17]. In a study by Muller et al. [18], FNAC had false negative
rate of 45% in diagnosing cystic papillary thyroid carcinoma.
This high level of false negativity is due to sampling error and
not cytological misdiagnosis. Ultrasound guided FNAC that
can obtain material from the wall and solid part of the cyst
increases the accuracy of FNAC [19].
Wunderbaldinger et al. [20] showed 80% of cystic
nodes in papillary thyroid carcinoma the aspirated uid
as brownish viscous and had elevated thyroglobulin levels.
Som et al. [21] and King et al. [22]who hypothesized that
high intranodal concentration of thyroglobulin reect areas
of high attenuation on CT and inhomogeneous intracystic
signal changes on MR imaging, respectively. Therefore, the
uid from these cystic lesions should be sent for thyroglob-
ulin analysis whenever an unclear cystic mass in the neck is
present or when the diagnosis of such a mass is in question.
Excisional biopsy is essential to detect papillary thyroid
carcinoma in patients with negative FNAC. If clinical or
radiological suspicion of malignancy is present, frozen
section analysis of the specimen may help to proceed for a
total thyroidectomy with modied radical neck dissection at
the same setting.
4 Case Reports in Endocrinology
Adequate surgery by removing the cyst, all of the thyroid
tissue and accessible involved lymph nodes is essential for
better prognosis. Postoperative radioiodine ablation of thy-
roid remnant with suppressive thyroxine dose is advocated
to reduce recurrences. Followup with serial thyroglobulin
estimation can help early recurrences or metastasis.
Papillary thyroid carcinoma (PTC) clinically behaves in
an indolent fashion and carries an excellent prognosis >90%
survival at 20 years. ETE has a 54% 15 year survival and 29%
30 year survival [8].
4. Conclusion
Papillary thyroid carcinoma is the most common of thyroid
malignancies. Though most present with solitary thyroid
nodule or as lymph node mass. Unusual presentation
like solitary cystic nodal mass or multiple cystic mass in
neck must be considered. Rarely can it present with sinus
formation in long standing cases. Ultrasonography can help
in dierentiating benign from malignant cystic lesions of
neck. Though FNAC is not very accurate in diagnosis of
cystic lesions. Aspirated uid thyroglobulin and thyroid
transcription factor levels may help to dierentiate cystic
thyroid carcinomas from benign cystic lesions. Complete
cyst excision with total thyroidectomy and node dissection
provides good prognosis even in setting of extrathyroidal
extension.
References
[1] A. Scott, S. A. Hundahl, I. D. Fleming, A. M. Fremgen, and H.
R. Menck, A national cancer data base report on 53, 856 cases
of thyroid carcinoma treated in the U.S., 19851995, Cancer,
vol. 83, no. 12, pp. 263822948, 1998.
[2] H. I. Benito, R. A. S anchez, P. M. Rodrguez et al., Simple
thyroid cyst, Revista Espanola de Medicina Nuclear, vol. 20,
no. 1, pp. 3235, 2001.
[3] H. Seven, A. Gurkan, U. Cinar, C. Vural, and S. Turgut, Inci-
dence of occult thyroid carcinoma metastases in lateral cervi-
cal cysts, American Journal of Otolaryngology, vol. 25, no. 1,
pp. 1117, 2004.
[4] T. Nakagawa, T. Takashima, and K. Tomiyama, Dierential
diagnosis of a lateral cervical cyst and solitary cystic lymph
node metastasis of occult thyroid papillary carcinoma, Jour-
nal of Laryngology and Otology, vol. 115, no. 3, pp. 240242,
2001.
[5] J. N. Attie, M. Setzin, and I. Klein, Thyroid carcinoma pre-
senting as an enlarged cervical lymph node, American Journal
of Surgery, vol. 166, no. 4, pp. 428430, 1993.
[6] C. F. Loughran, Case report: cystic lymph node metastasis
from occult thyroid carcinoma: a sonographic mimic of a
branchial cleft cyst, Clinical Radiology, vol. 43, no. 3, pp. 213
214, 1991.
[7] J. M. Monchik, G. De Petris, and C. De Crea, Occult papillary
carcinoma of the thyroid presenting as a cervical cyst, Surgery,
vol. 129, no. 4, pp. 429432, 2001.
[8] P. E. Andersen, J. Kinsella, T. R. Loree, A. R. Shaha, and J. P.
Shah, Dierentiated carcinoma of the thyroid with extrathy-
roidal extension, American Journal of Surgery, vol. 170, no. 5,
pp. 467470, 1995.
[9] K. Harish, Thyroid carcinoma with discharging sinusa
rarity: a case report, Journal of Medical Case Reports, vol. 2,
article 64, 2008.
[10] M. C. Frates, C. B. Benson, J. W. Charboneau et al., Manage-
ment of thyroid nodules detected at US: society of Radiologists
in Ultrasound consensus conference statement, Ultrasound
Quarterly, vol. 22, no. 4, pp. 231238, 2006.
[11] P. Jun, L. C. Chow, and R. B. Jerey, The sonographic features
of papillary thyroid carcinomas: pictorial essay, Ultrasound
Quarterly, vol. 21, no. 1, pp. 3945, 2005.
[12] B. K. Chan, T. S. Desser, I. R. McDougall, R. J. Weigel, and R.
B. Jerey Jr., Common and uncommon sonographic features
of papillary thyroid carcinoma, Journal of Ultrasound in
Medicine, vol. 22, no. 10, pp. 10831090, 2003.
[13] J. K. Hoang, W. K. Lee, M. Lee, D. Johnson, and S. Farrell, US
features of thyroid malignancy: pearls and pitfalls, Radio-
graphics, vol. 27, no. 3, pp. 847860, 2007.
[14] N. Al-Brahim and S. L. Asa, Papillary thyroid carcinoma: an
overview, Archives of Pathology and Laboratory Medicine, vol.
130, no. 7, pp. 10571062, 2006.
[15] H. J. Tae, D. J. Lim, K. H. Baek et al., Diagnostic value of
ultrasonography to distinguish between benign and malignant
lesions in the management of thyroid nodules, Thyroid, vol.
17, no. 5, pp. 461466, 2007.
[16] O. Beahrs, P. Kiernan, and J. J. Hubert, Cancer of the thyroid
gland, in Cancer of the Head and Neck, J. Suen and E. Myers,
Eds., pp. 599632, Churchill Livingstone, New York, NY, USA,
1981.
[17] H. S. Chi, L. F. Wang, F. Y. Chiang, W. R. Kuo, and K. W. Lee,
Branchial cleft cyst as the initial impression of a metastatic
thyroid papillary carcinoma: two case reports, Kaohsiung
Journal of Medical Sciences, vol. 23, no. 12, pp. 634638, 2007.
[18] N. Muller, P. L. Cooperberg, K. C. H. Suen, and S. C. Thorson,
Needle aspiration biopsy in cystic papillary carcinoma of the
thyroid, American Journal of Roentgenology, vol. 144, no. 2,
pp. 251253, 1985.
[19] D. S. Cooper, G. M. Doherty, B. R. Haugen et al., Revised
American thyroid association management guidelines for
patients with thyroid nodules and dierentiated thyroid can-
cer, Thyroid, vol. 19, no. 11, pp. 11671214, 2009.
[20] P. Wunderbaldinger, M. G. Harisinghani, P. F. Hahn et al.,
Cystic lymph node metastases in papillary thyroid carci-
noma, American Journal of Roentgenology, vol. 178, no. 3, pp.
693697, 2002.
[21] P. M. Som, M. Brandwein, M. Lidov, W. Lawson, and H. F.
Biller, The varied presentations of papillary thyroid carci-
noma cervical nodal disease: CT and MR ndings, American
Journal of Neuroradiology, vol. 15, no. 6, pp. 11231128, 1994.
[22] A. D. King, A. T. Ahuja, E. W. H. To, G. M. K. Tse, and
C. Metreweli, Staging papillary carcinoma of the thyroid:
magnetic resonance imaging vs ultrasound of the neck,
Clinical Radiology, vol. 55, no. 3, pp. 222226, 2000.
You might also like
- Salivary Gland Cancer: From Diagnosis to Tailored TreatmentFrom EverandSalivary Gland Cancer: From Diagnosis to Tailored TreatmentLisa LicitraNo ratings yet
- Thyroglossal CystsDocument4 pagesThyroglossal CystsCondurache Ilie-AndreiNo ratings yet
- Simultaneous Papillary Carcinoma in Thyroglossal Duct Cyst and ThyroidDocument5 pagesSimultaneous Papillary Carcinoma in Thyroglossal Duct Cyst and ThyroidOncologiaGonzalezBrenes Gonzalez BrenesNo ratings yet
- Kista Pada LeherDocument4 pagesKista Pada LeherKhairuman FitrahNo ratings yet
- Progressive Dyspnea in Patient With Large Mediastinal Mass: Casereport Open AccessDocument5 pagesProgressive Dyspnea in Patient With Large Mediastinal Mass: Casereport Open AccessFendry KolondamNo ratings yet
- B1 PDFDocument6 pagesB1 PDFDr. Arvind YadavNo ratings yet
- Normal Mediastinal Anatomy, Pathologies and Diagnostic MethodsDocument9 pagesNormal Mediastinal Anatomy, Pathologies and Diagnostic MethodsJuma AwarNo ratings yet
- Thyroglossal Duct Cyst StudyDocument7 pagesThyroglossal Duct Cyst StudyAurel OctavianNo ratings yet
- Thyroid MetsDocument3 pagesThyroid MetsQusai Al JarrahNo ratings yet
- Title: Latent Primary Papillary Micro Tumor in Thyroglossal Duct Cyst Wall - A Rare Case Report With Review of LiteratureDocument9 pagesTitle: Latent Primary Papillary Micro Tumor in Thyroglossal Duct Cyst Wall - A Rare Case Report With Review of LiteratureRathinaKumarNo ratings yet
- Large CystDocument4 pagesLarge CystKin DacikinukNo ratings yet
- Additional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandDocument7 pagesAdditional Article Information: Keywords: Adenoid Cystic Carcinoma, Cribriform Pattern, Parotid GlandRizal TabootiNo ratings yet
- Urology Case Reports: Abdullah, Junping XingDocument3 pagesUrology Case Reports: Abdullah, Junping XingHardiTariqHammaNo ratings yet
- Adenoid Cystic Carcinoma of Hard Palate: A Case ReportDocument5 pagesAdenoid Cystic Carcinoma of Hard Palate: A Case ReportHemant GuptaNo ratings yet
- International Journal of Surgery Case Reports: Case Report - Open AccessDocument3 pagesInternational Journal of Surgery Case Reports: Case Report - Open AccesscagcmdNo ratings yet
- 2009 Tumores DiafragmaDocument9 pages2009 Tumores DiafragmaJavier VegaNo ratings yet
- Rare Case of Aggressive Malignant Phyllodes Tumor with Rapid MetastasisDocument16 pagesRare Case of Aggressive Malignant Phyllodes Tumor with Rapid MetastasisunknownNo ratings yet
- MnahiDocument29 pagesMnahiRara SafikaNo ratings yet
- Ismail 2010Document4 pagesIsmail 2010Oscar GarciaNo ratings yet
- Art 1Document15 pagesArt 1Nizam Ul MulkNo ratings yet
- 2012 Article 202Document12 pages2012 Article 202cronoss21No ratings yet
- Angiomatous Leiomyoma of The Urachus: A Rare Entity Masquerading As Extraluminal Gastrointestinal Stromal TumorDocument4 pagesAngiomatous Leiomyoma of The Urachus: A Rare Entity Masquerading As Extraluminal Gastrointestinal Stromal Tumordella elvira rosaNo ratings yet
- Rare Case of Zosteriform Metastases from Hard Palate CancerDocument4 pagesRare Case of Zosteriform Metastases from Hard Palate CancerShiva PNo ratings yet
- Cerebellopontine Angle Epidermoid CYST: Case ReportDocument3 pagesCerebellopontine Angle Epidermoid CYST: Case ReportTamajyoti GhoshNo ratings yet
- Primary Adenocarcinoma of Rete Testis Report of A Rare NeoplasmDocument4 pagesPrimary Adenocarcinoma of Rete Testis Report of A Rare NeoplasmDio Mafazi FabriantaNo ratings yet
- Thyroid UltrasoundDocument9 pagesThyroid UltrasoundMoh SuriyawalNo ratings yet
- A Rare Case of Bilateral Adrenocortical Carcinoma With Metastasis in A Young MaleDocument3 pagesA Rare Case of Bilateral Adrenocortical Carcinoma With Metastasis in A Young MaleDixit VarmaNo ratings yet
- Malignant Parotid Tumors: Introduction and AnatomyDocument1 pageMalignant Parotid Tumors: Introduction and AnatomyCeriaindriasariNo ratings yet
- Surgical Neurology International: Unusual Growth Pattern of A MeningiomaDocument3 pagesSurgical Neurology International: Unusual Growth Pattern of A MeningiomaJamie NicholsNo ratings yet
- Jurnal Patologi AnatomiDocument5 pagesJurnal Patologi Anatomiafiqzakieilhami11No ratings yet
- UrineDocument4 pagesUrineVidhya MuruganNo ratings yet
- Median Raphe Cyst of The Penis: A Case Report and Review of The LiteratureDocument9 pagesMedian Raphe Cyst of The Penis: A Case Report and Review of The LiteratureYi-Ke ZengNo ratings yet
- Congenital Cystic Masses of NeckDocument47 pagesCongenital Cystic Masses of NeckFibrianti SeputriNo ratings yet
- Coincidence of Thymoma and Breast Cancer in A 56 Year Old FemaleDocument7 pagesCoincidence of Thymoma and Breast Cancer in A 56 Year Old FemaleOscar HalumNo ratings yet
- A Case of Malignant Pleural Effusion Secondary To Endometrial Cancer After One Year of HysterectomyDocument5 pagesA Case of Malignant Pleural Effusion Secondary To Endometrial Cancer After One Year of HysterectomyPao Flores.No ratings yet
- CEOTDocument8 pagesCEOTDrSahar PakzadNo ratings yet
- 45syam EtalDocument3 pages45syam EtaleditorijmrhsNo ratings yet
- Benign Paratesticlar Cyst - A Mysterical FindingDocument2 pagesBenign Paratesticlar Cyst - A Mysterical FindingInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Huge Cervical Swelling Hiding A Tonsillated Cyst About 01caseDocument3 pagesHuge Cervical Swelling Hiding A Tonsillated Cyst About 01caseInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 49 Kishor EtalDocument4 pages49 Kishor EtaleditorijmrhsNo ratings yet
- Tonsil TumorDocument4 pagesTonsil TumorafrisiammyNo ratings yet
- Cysts of Pancreas RADIOLOGYDocument20 pagesCysts of Pancreas RADIOLOGYmhany12345No ratings yet
- Ectopic Cervical Thyroid Carcinoma-Review of The Literature With Illustrative Case SeriesDocument8 pagesEctopic Cervical Thyroid Carcinoma-Review of The Literature With Illustrative Case SeriesAnonymous s4yarxNo ratings yet
- Intrathyroidal Lymphoepithelial (Branchial) Cyst: Diagnostic and Management Challenge of A Rare EntityDocument5 pagesIntrathyroidal Lymphoepithelial (Branchial) Cyst: Diagnostic and Management Challenge of A Rare EntityMeliNo ratings yet
- LeiomyomaDocument3 pagesLeiomyomacandiddreamsNo ratings yet
- Case Report Lung Cancer With Skin and Breast MetasDocument6 pagesCase Report Lung Cancer With Skin and Breast Metasreni melindaNo ratings yet
- BranchialCleftCyst GerDocument36 pagesBranchialCleftCyst GerDrsreeram Valluri100% (1)
- Cutaneous MetaDocument3 pagesCutaneous MetatzuskymedNo ratings yet
- Cystic Lymphangioma A Case ReportDocument4 pagesCystic Lymphangioma A Case ReportIJAR JOURNALNo ratings yet
- Meningioma in The Lumbar SpineDocument12 pagesMeningioma in The Lumbar Spinemex487No ratings yet
- Papillary Carcinoma 7-2Document4 pagesPapillary Carcinoma 7-2Amna MurtaxaNo ratings yet
- International Journal of Surgery Case ReportsDocument3 pagesInternational Journal of Surgery Case ReportsYipno Wanhar El MawardiNo ratings yet
- E17 FullDocument5 pagesE17 FullSajit RawatNo ratings yet
- Endometriosis: Different Locations and Faces Seen by CT and MRIDocument31 pagesEndometriosis: Different Locations and Faces Seen by CT and MRIBrenda Ruth PanjaitanNo ratings yet
- D0131011415 PDFDocument2 pagesD0131011415 PDFafm26No ratings yet
- Jurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthDocument7 pagesJurnal Kedokteran Dan Kesehatan Indonesia: Indonesian Journal of Medicine and HealthNio DoodohNo ratings yet
- Cervical Lymph NodeDocument4 pagesCervical Lymph NodeHermawan HmnNo ratings yet
- Imaging of Cystic or Cyst-Like Neck MassesDocument10 pagesImaging of Cystic or Cyst-Like Neck MassesRini RahmawulandariNo ratings yet
- Bronchogenic Malignancy and Metastatic Disease: Hilar MassesDocument4 pagesBronchogenic Malignancy and Metastatic Disease: Hilar MassesTira SariNo ratings yet
- Embolización Angiografica ArtDocument5 pagesEmbolización Angiografica ArtIsamar AlvarezNo ratings yet
- Maxillary FX Pic MDocument58 pagesMaxillary FX Pic MabhishekbmcNo ratings yet
- Delfi Spec LimbProtectionSleeveDocument2 pagesDelfi Spec LimbProtectionSleeveabhishekbmcNo ratings yet
- View Doc 635470672036959908Document6 pagesView Doc 635470672036959908abhishekbmcNo ratings yet
- POSASv2 0 ObserverScale EN1Document1 pagePOSASv2 0 ObserverScale EN1abhishekbmcNo ratings yet
- Hand Burns Treatment Goals and UnknownsDocument42 pagesHand Burns Treatment Goals and UnknownsabhishekbmcNo ratings yet
- 3M Donor SiteDocument6 pages3M Donor SiteabhishekbmcNo ratings yet
- Burns Free Flap Systematic ReviewDocument12 pagesBurns Free Flap Systematic ReviewabhishekbmcNo ratings yet
- Z Plasty - VariationsDocument7 pagesZ Plasty - VariationsabhishekbmcNo ratings yet
- Cuadra AlvaroDocument7 pagesCuadra AlvaroabhishekbmcNo ratings yet
- Gall Stone SpillageDocument6 pagesGall Stone SpillageabhishekbmcNo ratings yet
- Silk DressingDocument13 pagesSilk DressingabhishekbmcNo ratings yet
- Burnout Syndrome Among Dental Students: A Short Version of The "Burnout Clinical Subtype Questionnaire " Adapted For Students (BCSQ-12-SS)Document11 pagesBurnout Syndrome Among Dental Students: A Short Version of The "Burnout Clinical Subtype Questionnaire " Adapted For Students (BCSQ-12-SS)abhishekbmcNo ratings yet
- 220 228Document9 pages220 228abhishekbmcNo ratings yet
- 440 FullDocument8 pages440 FullabhishekbmcNo ratings yet
- Obg Extra EdgeDocument201 pagesObg Extra EdgeabhishekbmcNo ratings yet
- ReviewDocument8 pagesReviewabhishekbmcNo ratings yet
- Tube IleostomyDocument5 pagesTube IleostomyabhishekbmcNo ratings yet
- Aps 39 397Document7 pagesAps 39 397abhishekbmcNo ratings yet
- 3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiDocument6 pages3Fwjfx "Sujdmf &BSMZ %jbhoptjt PG (Bmmcmbeefs $bsdjopnb "O "Mhpsjuin "QqspbdiabhishekbmcNo ratings yet
- 3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftDocument5 pages3ftfbsdi "Sujdmf $pnqbsjtpo PG) JQQPDBNQBM 7Pmvnf Jo %fnfoujb 4vcuzqftabhishekbmcNo ratings yet
- Blunt Trauma PancreasDocument5 pagesBlunt Trauma PancreasabhishekbmcNo ratings yet
- Fournier S GangreneDocument8 pagesFournier S GangreneabhishekbmcNo ratings yet
- Wo ArticleDocument13 pagesWo ArticleabhishekbmcNo ratings yet
- Abdominal X RayDocument64 pagesAbdominal X RayabhishekbmcNo ratings yet
- 2005 Jaime NNDocument10 pages2005 Jaime NNabhishekbmcNo ratings yet
- 300Document36 pages300abhishekbmc100% (1)
- Abdominal X RayDocument64 pagesAbdominal X RayabhishekbmcNo ratings yet
- All India Post Graduate Medical Entrance Exam ForumsDocument57 pagesAll India Post Graduate Medical Entrance Exam ForumsabhishekbmcNo ratings yet
- Fluid and Electrolyte Management PDFDocument10 pagesFluid and Electrolyte Management PDFbalab2311No ratings yet
- Monthly Business ReviewDocument36 pagesMonthly Business Reviewmdipu5_948971128No ratings yet
- Administrations whose CoCs are accepted for CECDocument1 pageAdministrations whose CoCs are accepted for CECGonçalo CruzeiroNo ratings yet
- Chapter 7 - The Political SelfDocument6 pagesChapter 7 - The Political SelfJohn Rey A. TubieronNo ratings yet
- Symasym BBDocument37 pagesSymasym BBChandraRizkyNo ratings yet
- Cloud Security Training and Awareness Programs For OrganizationsDocument2 pagesCloud Security Training and Awareness Programs For OrganizationsdeeNo ratings yet
- YSUUSYs NiCd Battery RepairDocument6 pagesYSUUSYs NiCd Battery Repairrwesseldyk50% (2)
- Electronics Foundations - Basic CircuitsDocument20 pagesElectronics Foundations - Basic Circuitsccorp0089No ratings yet
- 1 - Gear Seminar ManualDocument125 pages1 - Gear Seminar Manualgustool7100% (1)
- Socio-cultural influences on educationDocument4 pagesSocio-cultural influences on educationofelia acostaNo ratings yet
- OM - Rieter - UNIMix A76Document321 pagesOM - Rieter - UNIMix A76Phineas FerbNo ratings yet
- J-Garlic in CheeseDocument12 pagesJ-Garlic in CheeseMary GinetaNo ratings yet
- Figures of Speech ExplainedDocument5 pagesFigures of Speech ExplainedDarenJayBalboa100% (1)
- PE and Health 12 - Module 7Document19 pagesPE and Health 12 - Module 7Stephen Lorenzo A. DoriaNo ratings yet
- Professional Builder - Agosto 2014Document32 pagesProfessional Builder - Agosto 2014ValNo ratings yet
- AMB4520R0v06: Antenna SpecificationsDocument2 pagesAMB4520R0v06: Antenna SpecificationsЕвгений ГрязевNo ratings yet
- Business Ethics Concepts & Cases: Manuel G. VelasquezDocument19 pagesBusiness Ethics Concepts & Cases: Manuel G. VelasquezRaffi MouradianNo ratings yet
- Pmls 1 Final Exam Reviewer: Clinical Chemistry ContDocument14 pagesPmls 1 Final Exam Reviewer: Clinical Chemistry ContPlant in a PotNo ratings yet
- De Thi HK 2 Tieng Anh 9 de 2Document17 pagesDe Thi HK 2 Tieng Anh 9 de 2Lê Thu HiềnNo ratings yet
- Expt 1 Yarn Formation (Sherley Trash Analyser)Document7 pagesExpt 1 Yarn Formation (Sherley Trash Analyser)Yashdeep Sharma0% (1)
- New Japa Retreat NotebookDocument48 pagesNew Japa Retreat NotebookRob ElingsNo ratings yet
- Frequently Asked Questions: Wiring RulesDocument21 pagesFrequently Asked Questions: Wiring RulesRashdan HarunNo ratings yet
- Nataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaDocument8 pagesNataraja Stotram - A Hymn Without 'CharaNa' and 'ShRi~NgaSiva Krishna100% (1)
- Falling Weight Deflectometer Bowl Parameters As Analysis Tool For Pavement Structural EvaluationsDocument18 pagesFalling Weight Deflectometer Bowl Parameters As Analysis Tool For Pavement Structural EvaluationsEdisson Eduardo Valencia Gomez100% (1)
- F&B Data Analyst Portfolio ProjectDocument12 pagesF&B Data Analyst Portfolio ProjectTom HollandNo ratings yet
- Temptations in MinistryDocument115 pagesTemptations in MinistryJoseph Koech100% (1)
- Preparatory Lights and Perfections: Joseph Smith's Training with the Urim and ThummimDocument9 pagesPreparatory Lights and Perfections: Joseph Smith's Training with the Urim and ThummimslightlyguiltyNo ratings yet
- Manual EDocument12 pagesManual EKrum KashavarovNo ratings yet
- Recent Developments in Ultrasonic NDT Modelling in CIVADocument7 pagesRecent Developments in Ultrasonic NDT Modelling in CIVAcal2_uniNo ratings yet
- Security Testing MatDocument9 pagesSecurity Testing MatLias JassiNo ratings yet
- SAP SD Course Content PDFDocument4 pagesSAP SD Course Content PDFshuku03No ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (41)
- The Stress-Proof Brain: Master Your Emotional Response to Stress Using Mindfulness and NeuroplasticityFrom EverandThe Stress-Proof Brain: Master Your Emotional Response to Stress Using Mindfulness and NeuroplasticityRating: 4.5 out of 5 stars4.5/5 (109)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)