Professional Documents
Culture Documents
Papilledema Vignette
Uploaded by
Robert Montgomery0 ratings0% found this document useful (0 votes)
27 views6 pagesPapilledema
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentPapilledema
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views6 pagesPapilledema Vignette
Uploaded by
Robert MontgomeryPapilledema
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Papilledema
Golnaz J avey, M.D.
and
J effrey J . Zuravleff, M.D.
Papilledema specifically refers to optic nerve head swelling secondary to
increased intracranial pressure (IICP). Optic nerve swelling from etiologies other than
IICP is characterized as optic disc edema. Any process which leads to IICP can
likewise cause papilledema. The most common etiologies include tumors of the brain,
spinal cord, intracranial hemorrhage, hydrocephalus, craniosynostosis, cavernous and
dural sinus thrombosis, pseudotumor cerebri (benign intracranial hypertension), head
injury and intracranial infection such as abscess or meningitis.
Most cases of papilledema are bilateral, although the optic nerve appearance can
be asymmetric. Any reported unilateral papilledema should be viewed skeptically and is
more likely optic disc edema. Papilledema is relatively uncommon in infants due to the
lack of fusion of skull bones.
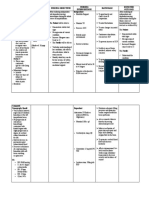
Diagnosis of papilledema is made by direct or indirect ophthalmoscopic
examination of the optic nerves. Hyperemia of the nerve head, blurring of the optic disc
margins, peripapillary flame-shaped hemorrhages, dilation of the capillaries on the
surface of the nerve, and absence of spontaneous venous pulsation are all clinical signs of
papilledema (Figures 1-4) (7).
It must be remembered that not all individuals have
spontaneous venous pulsations so that their absence alone does not indicate IICP. Nerve
fiber layer hemorrhages are the most common finding and often indicate an acute
process. In severe IICP, circumferential retinal folds known as Patons lines may develop
(Figure 4-6) (2, 8)
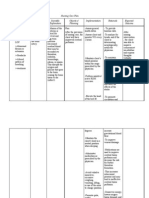
Chronic papilledema leads to nerve fiber layer atrophy (Figure 6) (6); this
thinning of the nerve fiber bundles, can be best appreciated by examination through the
red- free filter of a direct ophthalmoscope or by slit lamp biomicroscopy. The time
required for papilledema to evolve into optic atrophy depends on severity, and duration of
the IICP.
In chronic papilledema, the compromised blood egress through the central retinal
vein leads to formation of optociliary shunt vessels. These compensatory shunt vessels
indicate the retinal venous blood is bypassing the obstructed retinal vein via the choroidal
venous circulation (4).
Patients with papilledema often complain of headaches, worse upon awakening,
nausea, and vomiting. In early stages of papilledema patients may have no visual
complaints or only be aware of enlargement of the physiologic blind spot. As
papilledema worsens, patients may experience transient obscurations of vision believed
to be secondary to fluctuating ICP, nerve compression and/or or nerve ischemia (3).
Patients with papilledema secondary to an intracranial mass may also have homonymous
visual field defects from lesions in the intracranial visual pathway.
J avey and Zuravleff Page -2- Papilledema
Differential diagnosis of papilledema includes pseudopapilledema (Figure 7)
(anomalous elevated optic disc) and optic nerve edema caused by direct nerve
compression, inflammation, vascular, or infiltrative diseases. The finding of papilledema
in a patient without known intracranial disease, should lead to prompt neuro-imaging and
lumbar puncture.
Treatment of papilledema is directed at the underlying disorder causing IICP.
Papilledema generally resolves 6-8 weeks after ICP is normalized (1). Surgical
intervention is employed when patients present with vision threatening compressive optic
neuropathy or when primary treatment failed to lower the IICP. Cerebrospinal fluid
diversion by ventriculoperitoneal shunt is the most common method for reducing ICP and
optic nerve compression. Optic nerve sheath decompression has been effectively used to
acutely reduce the CSF pressure in the subarachnoid space of the optic nerve; a surgical
window of the nerve sheath allows the CSF to flow into the orbital soft tissues. The
technique is usually employed in severely elevated ICP such as pseudotumor cerebri.
Papilledema may improve in less than a week following optic nerve sheath
decompression surgery (5).
However, the long term effectiveness of this procedure in
reducing IICP is poor.
References:
1. Bettman J W J r, Daroff RB, Sanders MD, et al. Papilledema and symptomatic
intracranial hypertension in systemic lupus erythematosus, Arch Ophthalmol 1968;
80:180-193.
2. Bird AC, Sanders MD. Choroidal folds in association with papilloedema. Br J
Ophthalmol 1973;57:89-97.
3. Cogan DG. Blackouts not obviously due to carotid occlusion. Arch Ophthalmol
1961; 66:180-187.
4. Eggers HM, Sanders MD. Acquired optociliary shunt vessels in papilloedema. Br J
Ophthalmol 1980;64:267-271.
5. Hamed LM, Tse DT, Glaser J S, Frazier Byrne S, Schatz NJ . Neuroimaging of the
optic nerve after fenestration for management of pseudotumor cerebri. Arch Ophthalmol
1992; 110:636-639.
6. Hedges TR III, Legge RH, Peli E, et al. Retinal nerve fiber layer changes and visual
field loss in idiopathic intracranial hypertension. Ophthalmology 1995; 102: 1242-1247.
7. Neetens A, Smets RM. Papilledema. Neuroophthalmology 1989; 9:81-101.
8. Nettleship E. Peculiar lines in the choroid in a case of post-papillitic atrophy. Trans
Ophthalmol Soc UK 1884; 4: 167-8.
Figure 1. Courtesy of Mr. David B. Bennett, CRA.
Papilledema with blurring of disc margins.
Figure 2. Courtesy of Mr. David B. Bennett, CRA.
Papilledema with blurring of disc margins and dilation of surface capillaries.
Figures 3. Courtesy of Mr. David B. Bennett, CRA.
Papilledema with blurring of disc margins, disc hyperemia, and peripapillary flame
shaped hemorrhages.
Figure 4. Courtesy of Mr. David B. Bennett, CRA.
Papilledema with peripapillary flame shaped hemorrhages. Note the
circumferential retinal folds also known as Patons lines.
Figure 5. Courtesy of Mr. David B. Bennett, CRA
Papilledema with blurry disc margins and Patons lines.
Figure 6. Courtesy of Mr. David B. Bennett, CRA
Chronic papilledema with neurofibrolayer atrophy and Patons lines.
Note the extensive retinal exudates in the maculo-papillary bundle.
Figure 7. Courtesy of Mr. David B. Bennett, CRA
Pseudopapilledema. Optic nerve head drusen causing elevation and blurring of the
optic nerve head.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Multidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateDocument2 pagesMultidrug-Resistant Tuberculosis (MDR-TB) : 2012 UpdateRobert MontgomeryNo ratings yet
- The Extended FAST Exam: ObjectivesDocument16 pagesThe Extended FAST Exam: ObjectivesRobert MontgomeryNo ratings yet
- Interprofessional Education PDFDocument3 pagesInterprofessional Education PDFRobert MontgomeryNo ratings yet
- Nephrotic Syndrome IDocument12 pagesNephrotic Syndrome IRobert MontgomeryNo ratings yet
- Asphyxia: Forensic Medicine Rs Bhayangkara Porong Fakultas Kedokteran Universitas Muhammadiyah MalangDocument7 pagesAsphyxia: Forensic Medicine Rs Bhayangkara Porong Fakultas Kedokteran Universitas Muhammadiyah MalangRobert MontgomeryNo ratings yet
- Daftar Pustaka EdiarDocument1 pageDaftar Pustaka EdiarRobert MontgomeryNo ratings yet
- Papilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusDocument8 pagesPapilloedema: - Circulation of Cerebrospinal Fluid - Causes of Raised Intracranial Pressure - HydrocephalusRobert MontgomeryNo ratings yet
- Managing Acute Pain in The Developing WorldDocument8 pagesManaging Acute Pain in The Developing WorldRobert MontgomeryNo ratings yet
- Papilloedema and Optic AtrophyDocument27 pagesPapilloedema and Optic AtrophyRobert MontgomeryNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- DocxDocument53 pagesDocxkuro hanabusaNo ratings yet
- P1Document12 pagesP1Roykedona Lisa TrixieNo ratings yet
- Approach To ComaDocument33 pagesApproach To ComaDương Đình ThuậnNo ratings yet
- Pediatrics Nclex Review PointersDocument14 pagesPediatrics Nclex Review PointersCathryn Dominique Tan100% (1)
- Testing The Impact of Protocolized Care Of.5Document9 pagesTesting The Impact of Protocolized Care Of.5Nelson Da VegaNo ratings yet
- Meningitis Pada AnakDocument14 pagesMeningitis Pada AnakRayhanun MardhatillahNo ratings yet
- Pentagon NLE Review NotesDocument33 pagesPentagon NLE Review NotesChieChay Dub93% (123)
- 11NCP Ineffective Tissue Perfusion 2018 Revised 3.12.18Document2 pages11NCP Ineffective Tissue Perfusion 2018 Revised 3.12.18Aubrey SungaNo ratings yet
- Chapter 257: Head Trauma: Introduction and EpidemiologyDocument35 pagesChapter 257: Head Trauma: Introduction and EpidemiologyIustitia Septuaginta SambenNo ratings yet
- NNGN3780 ClinicalDocument26 pagesNNGN3780 ClinicalErica Dianne VelasquezNo ratings yet
- Maternal NursingDocument29 pagesMaternal NursingRose JoyNo ratings yet
- HER CCB in Crisis HypertensionDocument22 pagesHER CCB in Crisis HypertensionHandi Wijaya HasanNo ratings yet
- ATLS Practice Test 2 Answers & ExplanationsDocument8 pagesATLS Practice Test 2 Answers & ExplanationsCarl Sars50% (2)
- Approach To An Unconscious PatientDocument62 pagesApproach To An Unconscious Patientangiolikkia80% (5)
- NCLEX PracticeDocument18 pagesNCLEX Practiceandrew504777No ratings yet
- Neuropathology PDFDocument205 pagesNeuropathology PDFNarendraNo ratings yet
- Review Questions With RationaleDocument40 pagesReview Questions With RationaleHoward Corcuera100% (2)
- Evaluation and Management of Elevated Intracranial Pressure in AdultsDocument28 pagesEvaluation and Management of Elevated Intracranial Pressure in AdultssandykumalaNo ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- ATLS Chapter Review QuestionsDocument36 pagesATLS Chapter Review QuestionsKen Evans89% (57)
- Head Injury Management: Ahimbisibwe Alaphael Lecturer DR - JulietDocument33 pagesHead Injury Management: Ahimbisibwe Alaphael Lecturer DR - JulietNinaNo ratings yet
- Share Neuro SummaryDocument152 pagesShare Neuro SummaryAnonymous o0SCsnwNo ratings yet
- Chapter 14 Neurologic Disorders Study Guide Outline #2Document12 pagesChapter 14 Neurologic Disorders Study Guide Outline #2Del Delgado100% (1)
- StrokeDocument50 pagesStrokeABREHAM BUKULONo ratings yet
- Increased Intracranial PressureDocument38 pagesIncreased Intracranial Pressureroshanleung11No ratings yet
- CVA-NCPDocument7 pagesCVA-NCPAiza Oronce0% (1)
- Traumatic Brain Injury NCPDocument4 pagesTraumatic Brain Injury NCPwyneNo ratings yet
- Concept Map, Neil Floyd Ventura PDFDocument1 pageConcept Map, Neil Floyd Ventura PDFNeil Floyd VenturaNo ratings yet
- Lewis: Medical-Surgical Nursing, 8th EditionDocument6 pagesLewis: Medical-Surgical Nursing, 8th Editionlpirman05No ratings yet
- Abdominal Compartment SyndromeDocument24 pagesAbdominal Compartment SyndromePrateek Vaswani100% (1)