Professional Documents
Culture Documents
Electronic Spirometer For The Assessment of Lung's Functionality
Uploaded by
nagarajkaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Electronic Spirometer For The Assessment of Lung's Functionality
Uploaded by
nagarajkaCopyright:
Available Formats
Electronic Spirometer for the Assessment of
Lung’s Functionality 1
K.A.Nagaraja, 2Nanda.S
Dept. of Instrumentation Technology, S.J.C.E., Mysore- 570 006
E-mail: 1 ka_nagaraj@hotmail.com, 2nanda_prabhu@yahoo.co.in.
Abstract
Electronic Spirometer is a device employed to diagnose Extrinsic (allergic) asthma, Intrinsic asthma, Triad
the disease processes that impairs the lung’s function. asthma and Nasal polyp asthma are the commonly
Airflow obstruction, volume restrictions are the major observed types of asthma.
causes of lungs functional impairments that can be Extrinsic (allergic) Asthma is a type of asthma usually
diagnosed by electronic spirometry. Microcontroller affects children and young adults who have a personal or
based single channel Spirometer has been designed and family history of being hypersensitive to substances in the
developed for diagnosing the lung’s functionality for the environment, foods, or air substances that are inhaled. An
patients affected with obstructive or destructive diseases. individual can inherit the allergy to drugs, vaccines, and
This spirometer has been designed to determine FEV anesthetic agents also. Intrinsic Asthma is a type of asthma
(Forced expiratory volume), FVC (Forced vital capacity) that is more common among adults over 35, especially
and TV (Tidal volume) as basic maneuvers that are used women. Upper and lower respiratory tract infections may
in spirometry analysis by the doctors. The designed cause intrinsic asthma even though there has been no
hardware uses personal computer with serial interface to family or childhood history of the disease. All these types
display the different parameters associated with this of diseases associated with lungs results in air way
electronic spirometer. obstruction. This airflow obstruction can be diagnosed
using spirometry and volume restriction can be diagnosed
Key words: Spirometer, FEV, FVC, TV, Obstructive by other PFT (Pulmonary Function Tests) like nitrogen
and Destructive diseases. washout method and body plethysmography [7]. Since
Spirometer is a hand-held device, diagnosis of obstructive
I. INTRODUCTION lung disease can easily be made in an outpatient setting.
Spirometry is performed in order to diagnose and However, spirometry is accurate at predicting pulmonary
classify the disease processes that impair the lung’s (Example. A low FVC seen on spirometry may be a clue to
function. Impairments in lung’s function can be broadly a restrictive impairment) restriction but the initial
classified as those resulting in airflow obstruction, volume investment for the existing equipment is very high. It can
restriction, or a combination of obstructive and restrictive also be seen in patients with severe obstruction with air
defects. Chronic obstructive pulmonary diseases (COPD) trapping. If spirometry suggests a restrictive disorder,
are the common diseases associated with lungs [1]. Asthma patients with this pattern are usually referred for additional
and bronchitis are the common forms of COPD and are PFT to confirm the diagnosis. Diagnosis of a restrictive
found more often in men than women [15]. The incidence impairment depends on detecting a reduced total lung
of these diseases is more common among cigarette capacity (TLC) by lung volume measurement; lung
smokers than people who do not smoke [14]. Asthma is a volumes can be measured by plethysmography (“body
disease characterized by attacks of wheezing and difficult box”), by helium-dilution methods, or by the nitrogen-
breathing. Spasms of the smooth muscles that lie in the washout method. Measurement of lung volumes is almost
walls of the smaller bronchi and bronchioles bring on the exclusively done in licensed pulmonary function
attacks and cause these passageways to close partially. laboratories [2]. With very few exceptions, measurements
Asthma can be caused by environmental factors such as of lung volumes are ordered to diagnose restrictive
dust or cold air. Asthma can also be caused by an infection, pulmonary impairment with spirometry or to follow-up
exercise, or emotional upset. In an asthma attack, several patients with suspected restrictive pulmonary impairment.
bodily changes make it difficult for air to go through In the present work, we have designed and
bronchi passageways. These changes include bronchi developed a simple low cost electronic Spirometer to
constriction (bronchial muscles constricting), mucus measure lung volumes and lung capacity namely forced
secretion in the bronchi, and edema (fluid retention) in the vital capacity (FVC), Forced expiratory volume (FEV) [11]
bronchial wall. The difficulty in bringing air through those
Flow and Active
and Maximum voluntary ADC ventilation (MVV).
Instrumentation
passages accounts for a sign almost always associated with (Analog to
differential
asthma wheezing. amplifier Band pass
Pressure filter digital
sensors converter)
Fig. 1. Block Diagram of the Electronic Spirometer.
Power supply Personal 8 bit
+5V, -5V, GND computer with Micro controller
serial interface
II. DESIGN OF ELECTRONIC SPIROMETER This amplified signal is fed to the band pass filter
with pass band frequency between 0.05Hz to 13Hz. The
In order to maximize the potential information from Spirometer signal lies in the range of 0.1 to 12Hz. Hence
Spirometer [3], individual variables as well as the filter is designed for above frequency and it uses
combinations of variables are taken into consideration at Butterworth second order filter due to its flat response in
the time of design and development. To be practical for the pass band and low ripples. Output of ADC is the digital
most busy clinicians, and to effectively direct patient equivalent of the measured parameters related to lung’s
management, the algorithm used is having clear guidelines function. ADC used in our work is 14-bit Successive
for interpretation and be applicable to almost all patients Approximation type.
presenting for spirometry. An impetus toward development Microcontroller is programmed for particular
of this algorithm was to significantly reduce the number of sampling rate to read the data from the ADC (analog to
unnecessary lung volume measurements that were being digital converter) depending on the signal frequency. In
ordered in the hospital to screen for restrictive disease. this work, we have used a sampling rate of 500Hz for
Figure 1 shows the block diagram of low cost signal frequency of 13Hz. The Microcontroller used in our
Spirometer which includes flow sensor, [8] differential work is AT89S8253. The AT89S8253 is a low-power high
pressure sensor, instrumentation amplifier, low pass filter, performance CMOS 8-bit Microcontroller based on the
ADC, microcontroller and personal computer. In this basic RISC architecture. The architecture of this microcontroller
set up, the flow sensor is a Pitot tube type [8]. The basic is more code efficient while achieving throughputs up to
equation governing the output of a Pitot tube device is ten times faster than conventional CISC microcontroller.
Bernoulli’s theorem that relates the kinetic energy to the Again the same microcontroller is used to communicate
potential energy in a flow streamline. By decelerating the with the personal computer through the serial port. Serial
flow, kinetic energy (velocity) is converted to potential port is configured for particular baud rate depending on
energy (pressure). Thus a standard Pitot tube senses the serial port standards.
impact or total pressure caused by stopping the flow. If the
static pressure in the duct is measured and subtracted from III ALGORITHM
the total pressure, the result is related to the density and The software used in this work will classify the type of
velocity of the flowing fluid (or air). lung impairments. The steps involved in the algorithm are
The basic equation is: as follows:
ΔP = 1/2Kρ V2----------------------(1)
Where ΔP = Differential Pressure, K = Calibration Factor, Determine if the test is interpretable.
ρ= Gas Density and V = Actual Velocity. If interpretable, Assess FVC, FEV and absolute
After the flow sensor part, differential pressure FEV/FVC ratio.
sensor is used. This sensor works on the principle of Compare these values with standard FVC, FEV
Pneumo-tacometer. It uses a non-invasive method to and FEV/FVC ratio.
measure the capability of pulmonary functionality that may Determine whether it is restrictive, obstructive
be evaluated from flux/volume curve of pulmonary system. ventilatory impairment or normal spirometry.
Again Pneumo-tacograph principle is based on Poiseuille’s If it is normal end the test.
law, that from relationship between pressure difference and If it is restrictive ventilatory impairment refers to
volume-flow rate, measurement of difference in pressure MVV check and determines the severity.
yields an estimate of flow (liter/min.). Here the flow is If it is obstructive ventilatory impairment
laminar and going to be governed by Poiseuille’s law. performs other tests and determines severity.
Importantly, halving the radius of a tube will increase the
resistance by sixteen times. Note that with laminar flow, IV RESULTS
the drop in pressure is related to the flow rate, and so we The more commonly measured parameters to assess
can talk about the "resistance" of a tube, independent of the lung’s function using our Spirometer are: Forced vital
flow [9]. i.e., capacity (FVC), Forced expiratory volume (FEV) [11] and
Pressure drop α Flow---------------- (2) tidal volume (TV). FVC is the amount of air that can be
The differential sensor gives the electrical exhaled with force after the deep inhalation. FEV is the
quantity corresponding to the flow. In order to eliminate amount of air that the subject can exhale with force in one
noise and amplify signal level, instrumentation amplifier is breath. TV is the amount of air that can be inhaled and
used. The design involves computation of gain. The gain exhaled during normal respiration.
equation for instrumentation amplifier is as follows:
G = 5+ (80KΩ/RG) ------------------- (3) Other derived parameters are as follows: The amount
Where G is the gain; 80KΩ is internal feedback resistor of air that the subject can exhale may be measured at 1
value, RG external gain adjustment resistor. second (FEV1), 2 seconds (FEV2), or 3 seconds (FEV3).
FEV1/FVC ratio can also be determined [12]. Forced
expiratory flow between 25% to 75% measures the air flow
halfway through an exhale (FVC). Peak expiratory flow
(PEF) gives an indication of how quickly the subject can
exhale. It is usually measured along with forced vital
capacity (FVC). Maximum voluntary ventilation (MVV) is
a measure of maximum amount of air the subject can
breathe in and out during a period of one minute. Total
lung capacity (TLC) measures the amount of air present in
the lungs after the deep breadth.
We have tested the ability of the Spirometer to detect
restriction for the patients with suspected parenchyma,
pleural, or chest wall restriction. Out of the 40 patients
tested with our spirometer whose referral diagnosis
indicated suspected restrictive impairment, 24 patients Figure 3 Data after filtration.
ultimately had a restrictive pulmonary impairment
confirmed by body-box lung volume testing [6]. All 24
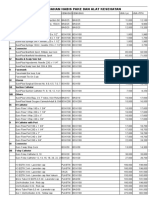
patients picked up by the spirometer are recommended for Table 1 Normal values of spirometry [16].
further lung volume testing.
Patients with moderate-to-severe obstructive defects were FEV 80% to 120%
also analyzed as a subgroup. These are a group of patients FCV 80% to 120%
with at least moderate airflow obstruction, for whom the Absolute FEV1/FVC With in 5%of the predicted
spirometer does not recommend lung volume testing. value
The following two graphs show the output waveforms of TLC 80% to 120%
the spirometer. This graph was obtained for FEV. From this FRC 75% to 120%
we can derive FEV, Peak Flow, and FVC etc. In our work, RV 75% to 120%
the designed spirometer gives very accurate readings with
the small deviation of 0.1% error and this is due to very
small change in Pitot tube angle [9]. This can be eliminated
by proper placement of the Pitot tube (maintaining 900). As V DISCUSSION
per ATS (American thoracic society) the normal values are The objective of this work is to design and development of
shown in the table [5]. simple and low cost spirometer that would help rural
primary health care centers, private clinicians and
pulmonary function laboratories to procure low cost
spirometer with minimal investment. Also, to decide which
patients should undergo measurement of lung volumes
following spirometry. Since lung volume measurements
are almost always ordered to diagnose restrictive
pulmonary disease, [4] the spirometer was designed to
predict the presence or absence of pulmonary restriction.
The patients with an FVC of 85% and FEV1/FVC ratio of
55% require further lung volume measurements to confirm
the diagnosis of restrictive lung disease. Those patients
with an FVC 85% predicted are unlikely to be restricted
and do not require lung volume measurements. Similarly,
patients with a low vital capacity, but who also have
obstructive disease on spirometry (ie, FVC 85% of
Figure 2 Acquired raw data. predicted and an FEV1/FVC 55%), have a reduced vital
capacity because of air trapping, with impingement on
their vital capacity by a high residual volume. These
patients are also very unlikely to have true restrictive
pulmonary disease and do not require measurements of
lung volumes. Developed Spirometer is economical than
the currently available spirometer in the market. The
results obtained were consistent and reproducible [10]
when compared with the standard spirometers [13].
VI. ACKNOWLEDGEMNT 16. Goldman HI, Becklake MR. Respiratory function tests:
Authors would like to take this opportunity to hearty thank normal values at median altitudes and the prediction of normal
to all those who have helped in the successful completion results. Am Rev Respir Dis 1969; 79:457–467
of this work. It is a matter of immense pleasure to express
our sincere thanks to Mr.Sameer Sawarkar, CEO Mr.
Rajeev Kumar, MD and also Mrs.Richa Kumar, HR
Neurosynaptic Communications Pvt Ltd, for considering
and giving this opportunity for completing this work. We
render heartfelt thanks to Mr.M.Shiva Kumar, Asst Prof
Department of Instrumentation Technology, B.I.E.T.,
Davangere for his help.
VII REFERENCES
1. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS;
GOLD Scientific Committee. Global strategy for the diagnosis,
management, and prevention of chronic obstructive pulmonary
disease. NHLBI/WHO Global Initiative for Chronic Obstructive
Lung Disease (GOLD) Workshop summary. Am J Respir Crit
Care Med2001; 163:1256-76.
2. Ries A. Measurement of lung volumes. Clin Chest Med 1989;
10:177–186
3. Ferguson GT, Enright PL. Office spirometry for lung health
assessment in adults. Chest 2000; 117:1146–1161
4 Aaron SD, Dales RE, Cardinal P. How accurate is spirometry at
predicting restrictive pulmonary impairment? Chest 1999;
115:869–873.
5. American Thoracic Society. Lung function testing: selection of
reference values and interpretative strategies. Am Rev Respir Dis
1991; 144:1202–1218.
6. Kilburn KH, Miller A, Warshaw RH. Measuring lung volumes
in advanced asbestosis: comparability of plethysmographic and
radiographic versus helium rebreathing and single breath
methods. Respir Med 1993; 87:115–120
7. Gold WM. Pulmonary function testing. In: Murray JF, Nadel
JA, eds. Textbook of respiratory medicine, 3d ed. Philadelphia:
Saunders, 2000:781-871.
8."Filtrete.TM. Air Filter Media Type G, GS and GSB"
(Technical Data of 3M Filtration Products of St. Paul, MN), 4
pgs. International Search Report for PCT/US01/46787.
9. Ingram RH, Schilder DP: Effect of gas compression on
pulmonary pressure flow and volume relationship; J Appl Physio,
21:1821-2826, 1966.
10. Celli BR, MacNee W; ATS/ERS Task Force.Standards for the
diagnosis and treatment of patients with COPD: a summary of the
ATS/ERS position paper. Eur Respir J. 2004 Jun; 23(6):932-46.
11. Swanney MP, Jensen RL, Crichton DA, Beckert LE, Cardno
LA, Crapo RO. FEV6 is an acceptable surrogate for FVC in the
spirometric diagnosis of airway obstruction and restriction. Am J
Respir Crit Care Med 2000; 162:917-919.
12. Enright PL, Connett JE, Bailey WC. The FEV1/FEV6
predicts lung function decline in adult smokers. Resp Med 2000;
96:444-449.
13. American Thoracic Society. Standardization of spirometry.
Am Rev Respir Dis 1987; 136:1286–1296
14. Crapo RO, Morris AH, Clayton PD, et al. Lung volumes in
healthy nonsmoking adults. Bull Eur Physiopath Respir 1982;
18:419–425
15. Morris JF, Koski A, Johnson LC. Spirometric standards for
healthy non-smoking adults. Am Rev Respir Dis 1971; 103:
57–67
You might also like
- 12 OET Sample Referral Letter (Nurse) WritingDocument43 pages12 OET Sample Referral Letter (Nurse) WritingAL ' ARIS98% (41)
- q2 Grade 9 Pe DLL Week 1Document11 pagesq2 Grade 9 Pe DLL Week 1Airaa A. Baylan88% (8)
- Target Electric Blanket InstructionsDocument15 pagesTarget Electric Blanket Instructionsbritt16110% (1)
- Investigation Into The Rate of Respiration Using A SpirometerDocument10 pagesInvestigation Into The Rate of Respiration Using A SpirometerNayantara GopiNo ratings yet
- B Alert x10 User ManualDocument25 pagesB Alert x10 User ManualfrancistsyNo ratings yet
- Perfusion SystemDocument30 pagesPerfusion SystemShailendra Singh Khichi100% (1)
- Siamese-rPPG Network: Remote Photoplethysmography Signal Estimation From Face VideosDocument19 pagesSiamese-rPPG Network: Remote Photoplethysmography Signal Estimation From Face Videos李翊安No ratings yet
- Case ManagementDocument4 pagesCase ManagementPraveena.R100% (1)
- Diagnostic SpirometerDocument3 pagesDiagnostic SpirometerseventhsensegroupNo ratings yet
- MEDICAL ELECTRONICS PROJECTS ABSTRACT-Digital Pulmonary Function Test - SpirometryDocument4 pagesMEDICAL ELECTRONICS PROJECTS ABSTRACT-Digital Pulmonary Function Test - SpirometryR.ASHOKKUMAARNo ratings yet
- Diclofenac From Administration To Adverse Effect A Mini-ReviewDocument5 pagesDiclofenac From Administration To Adverse Effect A Mini-ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Coursework 1-Personal Development Plan: Student ID: Word CountDocument12 pagesCoursework 1-Personal Development Plan: Student ID: Word CountrajeshNo ratings yet
- Defibrillatorppt 131028115457 Phpapp01Document41 pagesDefibrillatorppt 131028115457 Phpapp01Simon JosanNo ratings yet
- BMI403.3 Biomedical InstrumentationDocument2 pagesBMI403.3 Biomedical InstrumentationDarpan Specchio PudasainiNo ratings yet
- Oxygen CascadeDocument12 pagesOxygen Cascadehy3pjb1984No ratings yet
- Chapter 17 Single Photon Emission Computed TomographyDocument28 pagesChapter 17 Single Photon Emission Computed TomographyJohnnie LópezNo ratings yet
- Contrast MediaDocument6 pagesContrast MediardmdelarosaNo ratings yet
- HP Diagnosis ChallengesDocument51 pagesHP Diagnosis ChallengesskchhabraNo ratings yet
- Basic Considerations in Nuclear MedicineDocument12 pagesBasic Considerations in Nuclear Medicinechberg13No ratings yet
- 1.0 The Origin of Biopotentials (New)Document62 pages1.0 The Origin of Biopotentials (New)Hanif HussinNo ratings yet
- SAR PPT 1-Program - 07Document36 pagesSAR PPT 1-Program - 07ni60No ratings yet
- Cherenkov RadiationDocument17 pagesCherenkov RadiationMayank GargNo ratings yet
- Baska MaskDocument8 pagesBaska MaskAnish H DaveNo ratings yet
- Anesthesia Considerations for Microlaryngoscopy and Direct LaryngoscopyDocument6 pagesAnesthesia Considerations for Microlaryngoscopy and Direct LaryngoscopyRubén Darío HerediaNo ratings yet
- A History of InnovationFromNovametrix To PhilipsDocument64 pagesA History of InnovationFromNovametrix To PhilipsEdgar GodinhoNo ratings yet
- EasyOn PC ManualDocument120 pagesEasyOn PC Manualasdfasdf87No ratings yet
- Non-Invasive Glucose SensorsDocument12 pagesNon-Invasive Glucose SensorsGerman GodiNo ratings yet
- The Artificial Heart: A Design Example: BIOE 1000 October 18, 2001Document17 pagesThe Artificial Heart: A Design Example: BIOE 1000 October 18, 2001Paspulati Leelaram100% (1)
- Senior Radiographer Nuclear MedicineDocument1 pageSenior Radiographer Nuclear Medicinetafi66No ratings yet
- 65 PDFDocument7 pages65 PDFShajan SNo ratings yet
- Sample Size CalculationsDocument5 pagesSample Size CalculationsAKNTAI002100% (1)
- Vant Hof SpringerProtocols 2019 V2finalDocument38 pagesVant Hof SpringerProtocols 2019 V2finalSusi SusantiNo ratings yet
- Role of Simulation in Anesthesia PracticeDocument39 pagesRole of Simulation in Anesthesia PracticeNitin ..100% (1)
- EEGDocument16 pagesEEGadibaronessNo ratings yet
- Nuclear Medicine GuideDocument3 pagesNuclear Medicine GuidejeffsunilNo ratings yet
- BioMedical TelemetryDocument7 pagesBioMedical TelemetrySean Matthew L. OcampoNo ratings yet
- Grip Strength and ElectromyogramDocument8 pagesGrip Strength and ElectromyogramChandra Murali100% (1)
- Abebaw Research ProposalDocument32 pagesAbebaw Research ProposalDerese BishawNo ratings yet
- Nuclear Medicine Inc.'s Iodine Value Chain AnalysisDocument6 pagesNuclear Medicine Inc.'s Iodine Value Chain AnalysisPrashant NagpureNo ratings yet
- Chapter 3 - Introduction To Nuclear MedicineDocument4 pagesChapter 3 - Introduction To Nuclear MedicineunknownxemNo ratings yet
- Aeroneb Solo DFU - EN - Rev JDocument56 pagesAeroneb Solo DFU - EN - Rev Jyagnaashi9092No ratings yet
- 17 Aususgt Final ProtocolDocument22 pages17 Aususgt Final ProtocolRishabh VermaNo ratings yet
- 3-EEG Fni$Document50 pages3-EEG Fni$chanlalNo ratings yet
- Pulseless Pumps & Artificial HeartsDocument23 pagesPulseless Pumps & Artificial HeartscafemedNo ratings yet
- Guidelines For Sedation and Anesthesia in GI Endos PDFDocument11 pagesGuidelines For Sedation and Anesthesia in GI Endos PDFHernan RuedaNo ratings yet
- Ch2 BiosignalsDocument15 pagesCh2 BiosignalsDip PaulNo ratings yet
- Tissue Optics Light Scattering Methods and InstrumDocument7 pagesTissue Optics Light Scattering Methods and InstrumDaniela UrreaNo ratings yet
- Design and Prototyping of A Low-Cost Portable Mechanical - DMD - 2010 - Al - Husseini - MITDocument13 pagesDesign and Prototyping of A Low-Cost Portable Mechanical - DMD - 2010 - Al - Husseini - MITSebastian100% (1)
- Spirometry E-Guide 2013Document28 pagesSpirometry E-Guide 2013Vidal Odon Ramos MermaNo ratings yet
- Dopaminergic and Serotonergic Neurohumoural TransmissionDocument23 pagesDopaminergic and Serotonergic Neurohumoural TransmissionChaitanya Kiran PullelaNo ratings yet
- Nuclear Medicine Tehnologist or Lead Nuclear Medicine TechnologiDocument2 pagesNuclear Medicine Tehnologist or Lead Nuclear Medicine Technologiapi-78955179No ratings yet
- Receptor PhysiologyDocument34 pagesReceptor PhysiologyKarl Torres Uganiza RmtNo ratings yet
- Palm Vein Authentication - Novák PDFDocument25 pagesPalm Vein Authentication - Novák PDFSatheesh Kumar100% (1)
- SaranDocument23 pagesSaranAbhishek BNo ratings yet
- Wearable BiosensorDocument26 pagesWearable BiosensorViolet blossomNo ratings yet
- MedicalelectricalsafetyDocument89 pagesMedicalelectricalsafetyMeruva LokeshwarNo ratings yet
- 2007 PFTs The Forced Oscillation TechniqueDocument50 pages2007 PFTs The Forced Oscillation TechniqueServiço de Imunoalergologia - H.S. João100% (1)
- 1.5.0.potentials and EquilibriumDocument8 pages1.5.0.potentials and EquilibriumAnonymous G3DRjDMkNo ratings yet
- Manipulation of The Cervical Spine A Systematic Review of Case Reports of Serious Adverse Events1995-2001Document5 pagesManipulation of The Cervical Spine A Systematic Review of Case Reports of Serious Adverse Events1995-2001Carlos Martín De RosasNo ratings yet
- Insulin Pump System DesignDocument10 pagesInsulin Pump System DesignmikeNo ratings yet
- The Radiation Chemistry of MacromoleculesFrom EverandThe Radiation Chemistry of MacromoleculesMalcolm DoleNo ratings yet
- Smart Home Technologies and Services for Geriatric RehabilitationFrom EverandSmart Home Technologies and Services for Geriatric RehabilitationMohamed-Amine ChoukouNo ratings yet
- Journal ClubDocument12 pagesJournal ClubAnonymous ibmeej9No ratings yet
- Revised Jones Criteria JurdingDocument41 pagesRevised Jones Criteria JurdingddantoniusgmailNo ratings yet
- Healing Through MusicDocument11 pagesHealing Through MusicMiguel MacaroNo ratings yet
- Pramipexole Effect on Depressive Symptoms in Parkinson's DiseaseDocument6 pagesPramipexole Effect on Depressive Symptoms in Parkinson's DiseaseCarmen CiursaşNo ratings yet
- Tatalaksana Emboli Paru PerkiDocument6 pagesTatalaksana Emboli Paru PerkiEviNo ratings yet
- Price List PT - Thirza 2019Document8 pagesPrice List PT - Thirza 2019Permana JuliansyahNo ratings yet
- PYQDocument2 pagesPYQAisyah OthmanNo ratings yet
- English for Nurses: A Concise GuideDocument137 pagesEnglish for Nurses: A Concise GuideLIDYANo ratings yet
- Virtual ColonosDocument200 pagesVirtual ColonosDiana VershyninaNo ratings yet
- NLEDocument18 pagesNLEKeij AranetaNo ratings yet
- Tugas B.inggris 28 Agt 2K20 Eli Irna eDocument3 pagesTugas B.inggris 28 Agt 2K20 Eli Irna eAhmad AsrullahNo ratings yet
- AIJ Clasif PRINTO 2019Document9 pagesAIJ Clasif PRINTO 2019Michael ParksNo ratings yet
- Vyanga Synopsis1Document2 pagesVyanga Synopsis1aniketNo ratings yet
- Abses Perianal JurnalDocument4 pagesAbses Perianal JurnalAnonymous tDKku2No ratings yet
- Wardlaws Perspectives in Nutrition 9th Edition Byrd Bredbenner Test BankDocument32 pagesWardlaws Perspectives in Nutrition 9th Edition Byrd Bredbenner Test Bankedricduyenuc1uw100% (19)
- Nama: Riris Putri Marito Sinaga NIM: 04022722125001 Prodi: Ilmu Kesehatan Anak No Soal 35Document13 pagesNama: Riris Putri Marito Sinaga NIM: 04022722125001 Prodi: Ilmu Kesehatan Anak No Soal 35Riris SinagaNo ratings yet
- Heart Disease in Pregnancy GuideDocument3 pagesHeart Disease in Pregnancy GuideNasehah SakeenahNo ratings yet
- NCMB317 Lec MidtermDocument55 pagesNCMB317 Lec Midterm2 - GUEVARRA, KYLE JOSHUA M.No ratings yet
- The Complete Enema Guide: by Helena BinghamDocument10 pagesThe Complete Enema Guide: by Helena BinghamJ.J.No ratings yet
- Embarazo y Ae PDFDocument13 pagesEmbarazo y Ae PDFraquel lopezNo ratings yet
- Pfin 6th Edition Billingsley Test BankDocument24 pagesPfin 6th Edition Billingsley Test BankNatalieRojasykebg100% (32)
- First Aid and Water SurvivalDocument18 pagesFirst Aid and Water SurvivalKri de Asis83% (12)
- Transcript 247 Pectasol C Modified Citrus Pectin and The Toxins It Removes With Dr. Isaac EliazDocument16 pagesTranscript 247 Pectasol C Modified Citrus Pectin and The Toxins It Removes With Dr. Isaac EliazField90No ratings yet
- Cardiovascular Physiology Applied To Critical Care and AnesthesiDocument12 pagesCardiovascular Physiology Applied To Critical Care and AnesthesiLuis CortezNo ratings yet
- APA Eating Disorders Practice Guideline Under CopyeditingDocument139 pagesAPA Eating Disorders Practice Guideline Under CopyeditingIbrahim NasserNo ratings yet
- Atom Electrosurgical SystemDocument40 pagesAtom Electrosurgical SystemOgut AjaNo ratings yet
- Physical Exam of the Eye: Structures, Findings, DiagnosesDocument16 pagesPhysical Exam of the Eye: Structures, Findings, DiagnosesriveliNo ratings yet