Professional Documents
Culture Documents
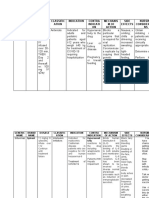
Syphilis signs, stages, and diagnosis
Uploaded by
Khristine Dyanne San Joaquin0 ratings0% found this document useful (0 votes)
528 views6 pagesSyphilis is a sexually transmitted disease caused by the spirochetal bacteria Treponema pallidum subspecies pallidum. The primary route of transmission is through sexual contact. It can also be transmitted from mother to fetus during pregnancy or at birth resulting in congenital syphiis. It has an incubation period of between 9 days and 3 months.
Original Description:
Original Title
SYPHILIS
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSyphilis is a sexually transmitted disease caused by the spirochetal bacteria Treponema pallidum subspecies pallidum. The primary route of transmission is through sexual contact. It can also be transmitted from mother to fetus during pregnancy or at birth resulting in congenital syphiis. It has an incubation period of between 9 days and 3 months.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
528 views6 pagesSyphilis signs, stages, and diagnosis
Uploaded by
Khristine Dyanne San JoaquinSyphilis is a sexually transmitted disease caused by the spirochetal bacteria Treponema pallidum subspecies pallidum. The primary route of transmission is through sexual contact. It can also be transmitted from mother to fetus during pregnancy or at birth resulting in congenital syphiis. It has an incubation period of between 9 days and 3 months.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 6
SYPHILIS of this sequence has given researchers new
insights as to how T. pallidum functions.
I. SYNONYM
IV. MODE OF TRANSMISSION
1. AIDS (Acquired immune deficiency syndrome)
2. HIV Treponema pallidum is transmitted from one
3. SIDA infected person to another. It is usually spread
4. STD through sexual contact. However, transmission
5. VD can occur anytime the infected ulcer comes in
6. Chancroid contact with mucous membranes or other broken
7. Chlamydia skin. It cannot, however, be transmitted by toilet
8. Clap seats, door handles, swimming pools, bath tubs,
9. Crab louse, crabs shared clothing, or eating utensils. A pregnant
10. Genital herpes woman can also pass the bacterium on to her child
11. Genital warts possibly resulting in mental or physical problems,
12. Gonorrhea or even still born birth.
13. Herpes, herpes simplex
14. Scabies, social disease Sexual contact, but in rare cases blood transfusion
15. Tabes, dorsalis
16. Venereal disease V. INCUBATION PERIOD
II. DEFINITION Syphilis has an incubation period of between 9
days and 3 months. Syphilis is almost always a
result of unprotected sex with an infected person.
Syphilis- is a sexually transmitted disease caused
by the spirochetal bacteria Treponema The incubation period is around 10-90 days with
pallidum subspecies pallidum. The primary route an average of 21 days.
of transmission of syphilis is through sexual
contact however it may also be transmitted from VI. SIGNS AND SYMPTOMS
mother to fetus during pregnancy or at birth
resulting in congenital syphilis. The signs and symptoms of syphilis vary
depending on which of the four stages it presents
III. ETIOLOGICAL AGENT
in (primary, secondary, latent, and tertiary). The
primary stage typically presents with a single
Treponema pallidum is a novel pathogen whose
physical properties allow it to be highly invasive chancre, secondary syphilis with a diffuse rash,
and evade host defense mechanisms. T. latent with little to no symptoms, and tertiary
pallidum is a gram-negative spirochete, helical with gummas, neurological, or cardiac symptoms.
shaped bacteria that cannot be cultured on Diagnosis is usually via blood tests. It can be
artificial media and must be grown in rabbit effectively treated with antibiotics, specifically
testicles. This is one of the main reasons for why
intramuscular penicillin G.
little is known anout this pathogen. Recently, its
genome of 1.14 Mb was sequenced and analysis
Syphilis is believed to have infected 12 million tis, optic neuritis, uveitis, and interstitial keratitis.
people worldwide in 1999 with greater than 90% The acute symptoms usually resolve after 3 to
of cases in the developing world. Rates of 6 weeks.
infection have increased during the 2000s in many
countries. LATENT
Syphilis can present in one of four different Latent syphilis is defined as having serologic
stages: primary, secondary, latent, and tertiary. It proof of infection without signs or symptoms of
may also occur congenitally. It has been referred
to as the “great imitator of skin diseases" due to disease. It is further described as either early (less
its varied presentations. than 1 yr after secondary syphilis) or late (more
than 1 year after secondary syphilis). Early latent
PRIMARY
syphilis may have relapses of symptoms. Late
Primary syphilis is typically acquired via direct
sexual contact with the infectious lesions of latent syphilis is asymptomatic and not as
another person. Approximately 3–90 days after contagious as early latent syphilis.
the initial exposure (average 21 days) a skin
lesion appears at the point of contact called TERTIARY
a chancre. This is classically (40% of the time) a
single firm, painless, non itchy skin ulceration Tertiary syphilis may occur approximately 3 to 15
with a clean base and sharp borders between 0.3 years after the initial infection and may be divided
and 3 cm in size. Occasionally multiple lesions into three different forms: late neurosyphilis
maybe present. Lesions outside of the genitals
(6.5%), cardiovascular syphilis (10%) and
may be painful. Lymph node enlargement
frequently (80%) occurs around the area of gummatous syphilis (15%). Without treatment a
infection.The lesion may persist for 3 to 6 weeks third of people develop tertiary disease.[5]People
without treatment.
with tertiary syphilis are not infectious.[1]
Gummatous
SECONDARY
Gummatous syphilis or late benign syphilis
Secondary syphilis occurs approximately 4 to
usually occurs 1–46 years after the initial
10 weeks after the primary infection. There are
infection, with an average of 15 years.[1] This
many different manifestations of secondary
stage is characterized by the formation of
disease. There may be a symmetrical reddish-pink
chronic gummas, which are soft, tumor-like balls
non-itchy rash on the trunk and extremities
of inflammation which may vary considerably in
including the palms and soles the rash may
size. They typically affect the skin, bone, and
become maculopapular or pustular. On mucous
liver, but can occur anywhere.
membranes it may form flat, broad, whitish, wart-
Late neurosyphilis
like lesions known as condyloma latum.All of
Neurosyphilis refers to an infection involving
these lesions are infectious harboring bacteria.
the central nervous system. It may occur early
Other symptoms may include fever, sore
being either asymptomatic or in the form of
throat, malaise, weight loss, hair loss, and
syphilitic meningitis or late as meningovascular
headache. Rare manifestations
syphilis, general or tabes dorsalis.[1] Late
include hepatitis, kidney disease, arthritis, periosti
neurosyphilis typically occurs 4 to 25 years after
the initial infection. Meningovascular syphilis 4. VDRL (Venereal Disease Research
typically presents with apathy and seizure, general Laboratory)
5. RPR (rapid plasma reagin) test
paresis with dementia and tabes dorsalis is
6. Syphilis antibody tests
associated with poor balance and lightening pains 7. .Fluorescent treponemal antibody-
in the lower extremities. absorption (FTA-ABS) test
8. Treponema pallidum hemagglutination
CARDIOVASCULAR
assay (TPHA)
Cardiovascular syphilis usually occurs 10– 9. Lumbar puncture (spinal tap) - to test CSF
30 years after the initial infection. The most for syphilis exposure
common complications is syphilitic aortitis which 10. CSF syphilis tests
may result in aneurysm formation. 11. Repetition of blood tests - some blood
tests take up to 3 months to be positive
after infection.
CONGENITAL
Syphilis may be confirmed
Congenital syphilis may occur during pregnancy Either via blood tests or direct visualization
or during the birth process. Most infants (2/3) are using microscopy.
born without symptoms. Common symptoms that Typical diagnosis is with blood tests using
then develop over the first couple years of life nontreponemal and/or treponemal tests.
include: hepatosplenomegaly (70%), rash (70%), Nontreponemal test are used initially and
include venereal disease research
fever (40%), neurosyphylis
laboratory (VDRL) and rapid plasma
(20%), pneumonitis (20%). If untreated late
reaginhowever as these test occasionally are
congenital syphilis may occur in 40% falsely positive confirmation is required with a
including: saddle treponemal test such as treponemal pallidum
nose deformation, Higoumenakis sign,saber shin, particle agglutination (TPHA) or fluorescent
or Clutton's joints among others. treponemal antibody absorption test (FTA-Abs).
False positives on the nontreponemal tests can
occur with some viral infections such as
VII. PATHOGOMONIC SIGN
(varicella and measles), as well as
with lymphoma, tuberculosis, malaria,endocarditi
Syphilis — painless chancre or ulceration. s, connective tissue disease, pregnancy.
Neurosyphilis is diagnosed by finding high
VIII. DIAGNOSTIC TEST numbers
of leukocytes (predominate lymphocytes) and
high protein levels in the fluid in the setting of a
The list of diagnostic tests mentioned in various
known syphilis infection.
sources as used in the diagnosis 1. Antibody screening tests (nontreponemal)
of Syphilis includes: o Rapid plasma reagin (RPR)
1. Swab of chancre - in primary and o Venereal Disease Research
secondary syphilis phases Laboratory (VDRL)
2. Swab/scraping test o Unheated serum reagin (USR)
3. Syphilis blood tests o Reagin screen test (RST)
2. Antibody confirmatory tests (treponemal) contracted through toilet seats, daily activities, hot
o Fluorescent treponemal antibody
absorption (FTA-ABS) tubs, or sharing eating utensils or clothing
o Fluorescent treponemal antibody
absorption double staining (FTA-
ABS DS)
Control
o Microhemagglutination assay for
antibody to T. pallidum (MHA-TP) The control of early infectious syphilis is essential
o Hemagglutination treponemal test for the control of congenital syphilis. When the
for syphilis (HATTS) prevalence of infectious syphilis substantially
o Bio-enzaBead Test (ELISA)
3. Direct examination of lesion or tissue increases among reproductive-age women, cases
o Darkfield microscopy of congenital syphilis very likely will follow.
o Direct fluorescent antibody test for Increased prevalence has been observed in several
T. pallidum (DFA-TP)
areas of the United States in recent years. To
o Silver stains (modified Steiner)
o Hematoxylin and eosin (H & E) prevent future cases of congenital syphilis, STD
stains control programs need to place more emphasis on
Experimental Tests early syphilis control, especially in areas with a
4. FTA-ABS immunoglobulin (IgM)
5. FTA-ABS 19S IgM high incidence.
6. IgM capture ELISA Prevention of Congenital Syphilis
1. Ensure that official public health statutes
and/or regulations mandate STS on all
pregnant women at the time of the initial
IX. DRUG OF CHOICE prenatal visit and early in the third
trimester.
Parenteral penicillin continues to be the drug of 2. Monitor public and private laboratories
choice for treatment of all stages of syphilis regularly to ensure the prompt and
thorough reporting of reactive STS.
3. Assess the pregnancy status of women
X. IMMUNIZATION with diagnosed syphilis and of women
who are the sex partners of men with
diagnosed syphilis.
As of 2010 there is no vaccine effective for 4. Ask early infectious syphilis patients or
Syphilis. their unexamined sex partners who reside
in neighborhoods with a high incidence of
syphilis to identify women in the area who
XI. PREVENTION AND CONTROL may be pregnant. Refer all identified
women for serologic testing and prenatal
Abstinence from intimate physical contact with an care.
5. Inform every woman of reproductive age
infected person is effective at reducing the who is seen in an STD clinic (for any
transmission of syphilis, as is the proper use of reason) about the need for prenatal care
a latex condom. Condom use, however, does not and STS in future pregnancies.
6. Encourage prenatal screening for syphilis
completely eliminate the risk. Syphilis cannot be wherever pregnant women are seen for
health care, including women, infants, and
children (WIC) programs, methadone 6. Teach the couple about the importance of
maintenance clinics, detention facilities, treatment to the health of their infant.
and prenatal care facilities; whenever 7. Instruct the patient to refrain from sexual
possible, review existing clinic protocols contact for at least 2 weeks or until lesions
and suggest specific amendments to the heal and return for serology testing in 1
clinic medical director. month and then every three months for 1
7. Conduct selective serologic screening of years.
women of childbearing age in groups with 8. Tell the patient that the disease should be
an increased risk of infection, e.g., women reported to the local health authority and
residing in neighborhoods that have a that the confidentiality will be maintained.
particularly high incidence of syphilis. 9. Identifying and treating the sexual partners
8. Deliver educational messages to the of the infected patient is an important
medical community about laboratory tests, intervention.
diagnostic criteria, treatment, and follow- 10. Provide care for the patient’s lesions, keep
up of patients who are at risk of infection them clean and dry.
and who may be pregnant. 11. Dispose the contaminated material from
9. Develop and disseminate public service draining lesions properly.
educational messages to women who share 12. Focus on prevention.
demographic characteristics with the 13. Educated patients about the course of the
women most often diagnosed with early disease and need to return for a follow up
syphilis. In many areas of the United treatment or blood tests.
States, these women are young, single, 14. Patients need to understand that although
members of a minority group, and their lesions may heal, the infection may
residents of a central city neighborhood. not be gone.
Brief, well-targeted radio announcements 15. Teach patients how to reduce the risk
in the language and vernacular of the factors on how to prevent future infections
audience may be particularly effective. by limiting the number of sexual partners
and practising SAFER SEX.
XII. NURSING MANAGEMENT 16. Advise patients to use condoms with
spermicides and inspecting partners for
any rashes or lesions may reduce exposure
1. Administer IM injection of benzathine to disease.
penicillin G as ordered,and document. 17. Patients also need an ongoing emotional
2. Discuss the importance of abstaining from support to make lifestyle changes.
sexual activity until he and his partners are 18. Explain the need for a regular laboratory
cured, and of using condoms to prevent re- testing.
infection. 19. Explain the relationship between human
3. Explain the need to return for follow-up immunodeficiency virus (HIV) and
testing in 3 months and again at 6 months. syphilis and perform HIV TESTING of
Provide a copy of the STI prevention the patient wishes.
checklist, and document that reminders 20. Instruct the patient given oral tetracycline
need to be sent at 3- and 6-month to take the medication 1 hour before or 2
intervals. hours after meals and to avoid dairy
4. Notify sexual partners that they need to products, antacids, iron, and sunlight while
come to the clinic for testing. taking the drug.
5. Refer to a social worker for counseling
about the impact of the disease on their
relationship.
XIII. POSSIBLE NURSING DIAGNOSIS
1.acute pain
2.impaired skin/tissue integrity
3.delayed growth and development
4.deficient knowledge regarding pathophysiology
of condition,transmissibility,therapy
needs.expected outcomes,and potential
complications
Submitted by:
Ace A. San Joaquin
BSN III-F
Group # 24
Submitted to:
Mr. Armando A. De los Santos, RN,MAN
Clinical Instructor
You might also like
- SyphilisDocument20 pagesSyphilisDhebra Mia Inot Suano100% (3)
- SyphilisDocument89 pagesSyphilisAnuZ13thNo ratings yet
- SyphilisDocument21 pagesSyphilisNinfa LansangNo ratings yet
- 4 Nursing Research Alpha 2017Document8 pages4 Nursing Research Alpha 2017Nicole DimarucutNo ratings yet
- Rare Kidney Cancer in ChildrenDocument12 pagesRare Kidney Cancer in ChildrenKath CamachoNo ratings yet
- HistoplasmosisDocument12 pagesHistoplasmosis사이맄 진No ratings yet
- STIs: Learn About Chlamydia, Gonorrhea, HPV, Hepatitis B, Herpes, HIV and Syphilis (35 charactersDocument25 pagesSTIs: Learn About Chlamydia, Gonorrhea, HPV, Hepatitis B, Herpes, HIV and Syphilis (35 charactersMohamoud MohamedNo ratings yet
- Malaria Diagnosis and TreatmentDocument27 pagesMalaria Diagnosis and TreatmentnasibdinNo ratings yet
- Orchitis (Eng)Document15 pagesOrchitis (Eng)Ferzy Awwali FadhilaNo ratings yet
- Widal Test: Dr. Neelu Jain Department of Microbiology B.M.CDocument25 pagesWidal Test: Dr. Neelu Jain Department of Microbiology B.M.Cnafiul islamNo ratings yet
- HPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDocument21 pagesHPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDaffa IbnurasyNo ratings yet
- Sexually Transmitted InfectionsDocument34 pagesSexually Transmitted InfectionsMariana Creciun100% (1)
- NTB Control Program ObjectivesDocument46 pagesNTB Control Program ObjectivesJai AdoraNo ratings yet
- Acute Lymphoblastic LeukemiaDocument25 pagesAcute Lymphoblastic Leukemiaapi-396564080No ratings yet
- NCP For CSDocument7 pagesNCP For CSJamielyn BassigNo ratings yet
- Measles: PGI Nicole Jenne C. TanDocument40 pagesMeasles: PGI Nicole Jenne C. TanNicole Jenne TanNo ratings yet
- INFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Document6 pagesINFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Rusida LiyaniNo ratings yet
- Systemic Lupus Erythematosus 2012Document564 pagesSystemic Lupus Erythematosus 2012Dan MunteanuNo ratings yet
- Dengue FeverDocument26 pagesDengue FeverathulpjoseNo ratings yet
- WILMs TumorDocument3 pagesWILMs TumorLorie May GuillangNo ratings yet
- MalariaDocument29 pagesMalariarhimineecat71No ratings yet
- MalariaDocument11 pagesMalariaWynli Fullo AncogNo ratings yet
- Dengue Fever Signs, Symptoms, and PreventionDocument9 pagesDengue Fever Signs, Symptoms, and PreventionKyla BalboaNo ratings yet
- Key elements of viruses and viral infectionsDocument44 pagesKey elements of viruses and viral infectionsMay BerNo ratings yet
- Syphilis Diagnosis and TreatmentDocument11 pagesSyphilis Diagnosis and TreatmentkanetrebleNo ratings yet
- Gonorrhoea FactsheetDocument4 pagesGonorrhoea FactsheetWilhelmus Wincent WijayaNo ratings yet
- Impetigo: A Bacterial Skin InfectionDocument13 pagesImpetigo: A Bacterial Skin InfectionTasya SyafhiraNo ratings yet
- Herpes Simplex KeratitisDocument2 pagesHerpes Simplex KeratitisSugam GouliNo ratings yet
- Bacterial MeningitisDocument1 pageBacterial MeningitisDavid HylandNo ratings yet
- STDDocument78 pagesSTDKrupa KarnikNo ratings yet
- Haemophilus SPPDocument109 pagesHaemophilus SPPJamie CañebaNo ratings yet
- Derma Report Contact DermatitisDocument25 pagesDerma Report Contact DermatitisYusnida RahmawatiNo ratings yet
- Case Study RPH TanawanDocument20 pagesCase Study RPH TanawanKarlo BartolomeNo ratings yet
- MeaslesDocument32 pagesMeaslesYum C100% (2)
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- Sexually Transmitted DiseasesDocument17 pagesSexually Transmitted DiseasesChrystele Ann Ramilo100% (1)
- Comhealth NursingDocument58 pagesComhealth NursingericNo ratings yet
- Tuberculous Meningitis Diagnosis, Treatment and Impact of HIVDocument34 pagesTuberculous Meningitis Diagnosis, Treatment and Impact of HIVLuvi PujiNo ratings yet
- Pulmonary Tuberculosis 2016Document17 pagesPulmonary Tuberculosis 2016Nikka Moreen Dagdag100% (1)
- Typhoid FeverDocument23 pagesTyphoid FeverAs ShahirahNo ratings yet
- Sexually Transmitted InfectionsDocument28 pagesSexually Transmitted InfectionsanjramNo ratings yet
- Mumps: Causes, Incidence, and Risk FactorsDocument6 pagesMumps: Causes, Incidence, and Risk FactorsRan SisonNo ratings yet
- Implications of HIV and AIDSDocument17 pagesImplications of HIV and AIDSfarah_hhrrNo ratings yet
- SyphilisDocument3 pagesSyphilisstaci_lutchman100% (2)
- TetanusDocument23 pagesTetanusRiska PriyaniNo ratings yet
- HIV/AIDS Determinants and Control FactorsDocument4 pagesHIV/AIDS Determinants and Control FactorsahiNo ratings yet
- Hereditary SpherocytosisDocument39 pagesHereditary SpherocytosisjoannaNo ratings yet
- Communicable DiseaseDocument22 pagesCommunicable DiseaseheheeheheNo ratings yet
- HEPA B and PIDDocument40 pagesHEPA B and PIDNica PinedaNo ratings yet
- Human Immunodeficiency Virus Case AnalysisDocument5 pagesHuman Immunodeficiency Virus Case AnalysisAllen Bugarin CabadingNo ratings yet
- Neisseria gonorrhoeae (GonococcusDocument28 pagesNeisseria gonorrhoeae (GonococcusRoni Ananda Perwira HarahapNo ratings yet
- DengueDocument41 pagesDengueJonathan00711100% (1)
- Cellular AberrationDocument71 pagesCellular AberrationMichael CoronadoNo ratings yet
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutFrom EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutRating: 5 out of 5 stars5/5 (1)
- A Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Parathyroid Adenoma, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- SYPHILIS1Document78 pagesSYPHILIS1Med PoxNo ratings yet
- Syphilis: Castro, Khristine Marie Laudencia BSNDocument8 pagesSyphilis: Castro, Khristine Marie Laudencia BSNPlan Can JoxNo ratings yet
- 4 - Routine and Non-Routine Data Collection MethodDocument15 pages4 - Routine and Non-Routine Data Collection Methoddani0% (2)
- Total Leukocyte Count by HemocytometerDocument4 pagesTotal Leukocyte Count by HemocytometerMalkish RajkumarNo ratings yet
- The Neurobiology of Sleep Continuum 2013Document13 pagesThe Neurobiology of Sleep Continuum 2013Habib G. Moutran BarrosoNo ratings yet
- BiostatisticsDocument147 pagesBiostatisticskartik paulNo ratings yet
- ERPM Viva Long Cases III v2.0Document17 pagesERPM Viva Long Cases III v2.0Bhagya Pramodh AriyarathnaNo ratings yet
- Effects of Infection On Nutritional StatusDocument6 pagesEffects of Infection On Nutritional Statuscaleb kimetoNo ratings yet
- Complete Forensic BCQsDocument31 pagesComplete Forensic BCQsShaheryar HasanNo ratings yet
- Providing Healthcare for Indigenous PeopleDocument6 pagesProviding Healthcare for Indigenous PeopleCielo AndreiNo ratings yet
- 10 Herbal Medicines Approved by DOH in The Phil.Document5 pages10 Herbal Medicines Approved by DOH in The Phil.Marie Angelique Cruz Crestani50% (2)
- Chap 1-3Document70 pagesChap 1-3Jaela ChumaceraNo ratings yet
- Summative Test ScoresDocument2 pagesSummative Test ScoresmaricelNo ratings yet
- 5it Would Be Foolish of Him Not To Consider This Opportunity. If It Would Be Foolish of Him ............................... This OpportunityDocument2 pages5it Would Be Foolish of Him Not To Consider This Opportunity. If It Would Be Foolish of Him ............................... This OpportunityAndrea Balon-RuffNo ratings yet
- AppendicitisDocument1 pageAppendicitisvaleriaNo ratings yet
- Self Assessment CasesDocument512 pagesSelf Assessment CasesmixandgoNo ratings yet
- Solve For X If 8Document3 pagesSolve For X If 8Gellie BuenaventuraNo ratings yet
- GonorreheaDocument5 pagesGonorreheaSunny OZNo ratings yet
- Book Chapter National Nutritional PolicyDocument15 pagesBook Chapter National Nutritional Policyscience worldNo ratings yet
- Medical Laboratory Questions and Answers for ExpertsDocument56 pagesMedical Laboratory Questions and Answers for ExpertsMaaryMeee RMT100% (1)
- 1800s City LifeDocument4 pages1800s City LifeErik KloseNo ratings yet
- Freshwater Fish Disease GuideDocument12 pagesFreshwater Fish Disease GuideSullip MajhiNo ratings yet
- Anamnesis AnemiaDocument10 pagesAnamnesis AnemiashevmyrNo ratings yet
- 93 DaysDocument2 pages93 DaysErbie MagpaleNo ratings yet
- Best Practices in Infection Prevention and Control PDFDocument198 pagesBest Practices in Infection Prevention and Control PDFYunita Panjaitan100% (2)
- Y2S2 Mosquitoes - RumalaDocument45 pagesY2S2 Mosquitoes - RumalamicroperadeniyaNo ratings yet
- Good Laboratory Practice SOPPD102 02Document11 pagesGood Laboratory Practice SOPPD102 02jsembiringNo ratings yet
- OET Reading Test 6 - Part BDocument11 pagesOET Reading Test 6 - Part BLOTSOFTESTS100% (2)
- 8d9c PDFDocument11 pages8d9c PDFJulian AshbourneNo ratings yet
- Thyroid CarcinomaDocument27 pagesThyroid CarcinomaGanesh MarutinathNo ratings yet
- Leonardo Da Vinci's Ideal CityDocument4 pagesLeonardo Da Vinci's Ideal CityJoyceCulturaNo ratings yet
- Functional Cure of Hiv Using Crispr - Adlene Jenitta, Vikrant Thokchom, W. Jasmine Karunya Institute of Technology and Sciences, CoimbatoreDocument2 pagesFunctional Cure of Hiv Using Crispr - Adlene Jenitta, Vikrant Thokchom, W. Jasmine Karunya Institute of Technology and Sciences, CoimbatoreRaj WillseeNo ratings yet