Professional Documents
Culture Documents
Congenital Mesoblastic Nephroma
Uploaded by
Sintya Paramitha Purba0 ratings0% found this document useful (0 votes)
22 views2 pagesCongenital mesoblastic nephroma is the most common solid tumor in neonates. It is usually diagnosed in the first three months of life, and is generally benign. Urography reveals a large, non-functional intrarenal mass.
Original Description:
Original Title
Congenital mesoblastic nephroma
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
DOC, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCongenital mesoblastic nephroma is the most common solid tumor in neonates. It is usually diagnosed in the first three months of life, and is generally benign. Urography reveals a large, non-functional intrarenal mass.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
22 views2 pagesCongenital Mesoblastic Nephroma
Uploaded by
Sintya Paramitha PurbaCongenital mesoblastic nephroma is the most common solid tumor in neonates. It is usually diagnosed in the first three months of life, and is generally benign. Urography reveals a large, non-functional intrarenal mass.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as DOC, PDF, TXT or read online from Scribd
You are on page 1of 2
Congenital mesoblastic nephroma
A renal mass in children may result from numerous causes, including
infection, infarction, lymphatic malformation, trauma and benign and malignant
neoplasms, such as Wilms’ tumor and renal teratoma. It is important to stress the
predominance of mesoblastic nephroma at this age group and the importance of
understanding its characteristics in imaging exams to make a differential diagnosis.
Thus, it is possible to make a correct early diagnosis, decide about management and
avoid complications.
Congenital mesoblastic nephroma, also known as fetal renal hamartoma or
mesenchymal hamartoma, is the most common solid tumor in neonates,
corresponding to approximately 3% of all renal neoplasias in children, and is
generally benign. It is usually diagnosed in the first three months of life (90% in the
first year), and there is a greater incidence among males(1). Although most of the
time patients have a palpable abdominal mass, 14% of the cases present
polyhydramnios, gastrointestinal malformations, neuroblastoma and genitourinary
anomalies, and such alterations can be identified by a prior fetal ultrasound
examination. Other less common symptoms include hypercalcemia associated with
arterial hypertension, congestive heart failure, and hematuria.
Polyuria and anemia may also be present(2-3). Although rarely necessary,
urography reveals a large, non-functional intrarenal mass which shifts and distorts
the adjacent parenchyma and the collecting system. Usually, there is no
hydronephrosis associated. The ultrasound often shows a well outlined unilateral,
homogeneous and hypoechogenic mass. The presence of hyperechogenic and
hypoechogenic concentric rings helps in the diagnosis. A more complex pattern
caused by hemorrhage or necrosis can be observed. Color Doppler usually shows
hypervascularization and shifting of adjacent vessels. The CT scan demonstrates an
intrarenal mass with unspecific attenuation pattern, which can be homogeneous or
heterogeneous(4). The characteristics of the lesions on magnetic resonance imaging
are not well established yet.
From the pathology standpoint, we know the classic, cellular and mixed
subtypes. The classic variant is seen in the macroscopic exam as a large and firm
mass, with infiltrating borders and appearance similar to that of uterine leiomyoma.
The cellular variant is softer, with cystic areas and irregular contours.
In the classic variant microscopy, enlarged cells (myofibroblasts) are seen
infiltrating the surrounding renal parenchyma, impairing the growth of tubules and
glomeruli. It is characterized by low cellularity, predominance of matrix and no
atypia. Conversely, the cellular variant has a high cellularity, high nucleus/cytoplasm
ratio, with mitoses, nuclear atypia and areas of necrosis, thus having a more
aggressive behavior(4).
Complete tumor excision spares patients from subsequent complementary
treatment. Nonetheless, an insufficient surgical margin requires a new intervention
in order to remove the residual disease. Chemotherapy is occasionally used in cases
of residual microscopic disease or in cases of tumor rupture, as well as in rare
recurrences or metastases.
The treatment advocated is immediate tumor resection by radical
nephrectomy(5-7). Most cases have favorable outcomes.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Severe Sepsis Screening Tool NhsDocument2 pagesSevere Sepsis Screening Tool NhsDavide Antonelli LaghiNo ratings yet
- Infection Control in Dental RadiologyDocument41 pagesInfection Control in Dental RadiologyDrShweta Saini0% (1)
- The Pharmacists Guide To Antimicrobial Therapy and StewardshipDocument244 pagesThe Pharmacists Guide To Antimicrobial Therapy and StewardshipAyman Khalil100% (1)
- Case Study 51 Acute PancreatitisDocument6 pagesCase Study 51 Acute PancreatitisKelsey LloydNo ratings yet
- Medical Tribune May 2012Document36 pagesMedical Tribune May 2012Sintya Paramitha PurbaNo ratings yet
- Medical Tribune June 2012Document41 pagesMedical Tribune June 2012Sintya Paramitha PurbaNo ratings yet
- Medical Tribune September 2012Document39 pagesMedical Tribune September 2012Sintya Paramitha PurbaNo ratings yet
- Medical Tribune November 2012Document50 pagesMedical Tribune November 2012Sintya Paramitha PurbaNo ratings yet
- Medical Tribune October 2012Document48 pagesMedical Tribune October 2012Sintya Paramitha PurbaNo ratings yet
- Do and Don'ts in Antibiotics-Dr. TonnyDocument25 pagesDo and Don'ts in Antibiotics-Dr. TonnySintya Paramitha PurbaNo ratings yet
- Rectal CancerDocument6 pagesRectal CancerIqra FatemahNo ratings yet
- Practical Approach To GIB Dr. Chris Huang 7.12.2013Document86 pagesPractical Approach To GIB Dr. Chris Huang 7.12.2013Juni Zuhairah Abd GhafarNo ratings yet
- Brugia MalayiDocument12 pagesBrugia Malayimuga restunaeshaNo ratings yet
- (MS II Lec) Endocrine System2Document8 pages(MS II Lec) Endocrine System2IlawNo ratings yet
- 2017 AAS ProgramDocument20 pages2017 AAS ProgramSiddharth NandaNo ratings yet
- Women and Schizophrenia ComplianceDocument7 pagesWomen and Schizophrenia ComplianceDhen MarcNo ratings yet
- Burnout Among NursesDocument6 pagesBurnout Among NursesYousef KhalifaNo ratings yet
- Stroke NoteDocument2 pagesStroke NoteHanry WijayaNo ratings yet
- SarcoidosisDocument17 pagesSarcoidosisapi-678326591No ratings yet
- Health 8 Q3 TGDocument67 pagesHealth 8 Q3 TGAngelica TumamakNo ratings yet
- HEALTH QUESTIONNAIRE (Talatanungan Ukol Sa Kalusugan) :: Please Read Carefully (Basahin NG Mabuti)Document2 pagesHEALTH QUESTIONNAIRE (Talatanungan Ukol Sa Kalusugan) :: Please Read Carefully (Basahin NG Mabuti)Karen Kaye PasamonteNo ratings yet
- CT Public v82 8 9Document2 pagesCT Public v82 8 9Dida HermaNo ratings yet
- APPENDICITISDocument2 pagesAPPENDICITISRichie Marie BajaNo ratings yet
- Prenatal Screening and Diagnostic TestingDocument39 pagesPrenatal Screening and Diagnostic TestingakashNo ratings yet
- Spindle Cell TumorsDocument138 pagesSpindle Cell TumorsMadhura ShekatkarNo ratings yet
- Diagnosing Patients With Acute-Onset Persistent DizzinessDocument7 pagesDiagnosing Patients With Acute-Onset Persistent DizzinessMuhammed ElgasimNo ratings yet
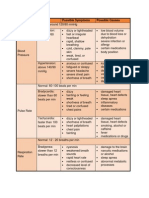
- Vital Signs Assessment TableDocument2 pagesVital Signs Assessment Tableapi-250869701No ratings yet
- Approach To SOBDocument25 pagesApproach To SOBabdiyare7134No ratings yet
- Bobcat Skid Steer Loader s770 Operation Maintenance ManualsDocument22 pagesBobcat Skid Steer Loader s770 Operation Maintenance Manualsmorganweiss270691imz100% (64)
- Coding With Meddra f2f CourseDocument54 pagesCoding With Meddra f2f CoursetudorNo ratings yet
- The Treatment of Diarrhea: Skill LabDocument16 pagesThe Treatment of Diarrhea: Skill LabnovylatifahNo ratings yet
- ChickenpoxDocument2 pagesChickenpoxNorhana LangiNo ratings yet
- Assessment Diagnosis Outcome Intervention Rationale EvaluationDocument7 pagesAssessment Diagnosis Outcome Intervention Rationale EvaluationArmie Joy Embat CariazoNo ratings yet
- HepatosplenomegalyDocument49 pagesHepatosplenomegalyTarun SinghNo ratings yet
- ABC Medical AbbreviationsDocument158 pagesABC Medical AbbreviationsXiaxin Liu100% (1)