Professional Documents
Culture Documents
ScopeMed Fulltext
Uploaded by
Choco MartiniOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ScopeMed Fulltext
Uploaded by
Choco MartiniCopyright:
Available Formats
Case Report
Chromoblastomycosis
Chromoblastomycosis
Dr. Harshada Shah*, Dr. K.Verma**, Dr. P.L.Dhand***, Dr. Rajesh Soni****, Ms. Pragya Shakya ****
*Prof. & Head, Dept. of Microbiology, **Prof. & Head, Dept. of Skin & Venereal Disease, ***Prof. & Head, Dept. of Pathology, ***Assistant Professor, ****P.G. Student, Dept. of Microbiology, RDGMC, Ujjain
Abstract: Chromoblastomycosis is a chronic fungal infection primarily of skin and subcutaneous tissue caused by a variety of dematiaceous fungal species belonging to different genera. We report a case which remains undiagnosed for 15 years although it presented with the most common manifestation. It was diagnosed and treated with excellent clinico-microbiological and histo-pathological correlation. Key words: Chromoblastomycosis, Cladosporium carionii, Copper penny bodies. Corresponding Author: Dr. Harshada Shah, Professor & Head, Dept of Microbiology, R.D.Gardi Medical College, Surasa, Agar Road, Ujjain (MP) 456006, E mail: sharshada1955@yahoo.com
INTRODUCTION: Chromoblastomycosis is a chronic, relatively uncommon, localized mycotic infection of the skin and subcutaneous tissue. Normally, it follows a traumatic implantation of dematiaceous fungi. The lesions range from verrucoid, ulcerated, crustate or cauliflower like growth to raised or flat plaques. Satellite lesions develop following autoinoculation and by lymphatic spread to adjacent areas. The disease has been described worldwide, but the incidence is greater in subtropical regions. Large numbers of cases have been reported from Madagascar and Brazil. Farming is the most common occupation associated with this lesion1. In India, most of the cases have been reported in belts from North to South sparing the Eastern and Western regions2. We present a case of Chromoblastomycosis from Central India. CASE REPORT: A 50 year old male agriculturist from Ujjain district in Madhya Pradesh visited the Skin OPD of C.R Gardi hospital in Jan, 2008. He presented with a 15 years long history and a cauliflower like lesion associated with itching and depigmentation of right lower limb. History revealed that it began with a small papular lesion on the external surface of right foot with itching. He went pole to post to seek medical attention until the lesion increased in size over a period of last 5 years. He also tried several home remedies. He was diagnosed as a case of tuberculosis at other center and received anti-tubercular treatment without
getting any clinical response. The lesion continued to progress and reached up to his knee (fig.1).
Fig 1 Initial KOH mount showed a fair number of round, non-septate structures resembling fungal spores. The skin biopsy done at our center revealed a pseudoepitheliomatous hyperplasia with micro abscesses and granulomatous infiltrate (fig.2).
NJIRM 2011; Vol. 2(1).Jan-March
eISSN: 0975-9840
pISSN: 2230 - 9969
Page
Fig 2
57
Case Report Classical copper penny bodies with brown pigmentation (sclerotic/ Meddler bodies) were present amidst the inflammatory infiltrate (fig.3).
Chromoblastomycosis Hematological & biochemical parameters were within normal limits. X-ray chest was normal. The patient was treated with Terbinafine and Itraconazole resulting in improved mobility and substantial drying of lesions with warty changes in first 3 months of the treatment. Unfortunately in spite of our efforts the patient could not be followed up beyond 6 months. DISCUSSION: Chromoblastomycosis usually occurs on hands, feet and upper legs. In our patient the lesion extended from foot up to the knee joint. It developed gradually starting as papular lesion to a cauliflower like growth. This is a common development reported in several other studies. A case of primary involvement of face has been reported by4. Usually the lesions remain confined to skin and subcutaneous tissue. However, hematogenous and lymphatic dissemination of the mycotic infection with fatal outcome has been documented in rare cases. The disease occurs commonly between 20-40 years of age with male preponderance. In a review of 34 patients by5, the patients aged from 12 to 80 years with a male to female ratio of 5.8:1. The above mentioned was a male who got infected at the age of 35 years .Indian patients with subcutaneous pheohyphomycosis are affected at an earlier age2 .Culture was positive in 72% of cases and sclerotic bodies were observed in 84% cases. In our case, the histopathology revealed sclerotic bodies and the culture was also positive. Although, a relatively a higher prevalence (15%) Fonsecaea compacta has been observed6, we identified Cladosporium carroini. A case of chromoblastomycosis caused by Fonsecaea pedrososi presenting as a small plaque on the left upper arm: has been reported in review of cases of dematiaceous fungal infections in Japan7. Extracutaneous involvement has been reported in 24 % of cases8. Surprisingly with 15 years long history there was no extra cutaneous involvement in this case. The characteristic histological and culture findings described for the disease were present in this patient. The clinical and histological features of
Fig 3 Culture on SDA with chlormphenicol and cycloheximide from skin scrapings revealed fungal colonies, which were identified as Cladosporium carroionii based on colony morphology and microscopy (fig.4)3 .
Fig - 04Crooked hyphae
Fig - 04 spherical / oval conidia in chains
NJIRM 2011; Vol. 2(1).Jan-March
eISSN: 0975-9840
pISSN: 2230 - 9969
Page
58
Case Report chromoblastomycosis are often misdiagnosed as squamous cell carcinoma or cutaneous tuberculosis, if a high level of suspicion and early diagnosis is not made. Similarly our patient was treated for cutaneous tuberculosis for two years. Numerous studies reported from India describe the distribution of the disease in the country in a belt from north to south, more so in sub-Himalayan belt6, 9,10. There are sporadic reports from eastern and western regions. Since, there are sparse reports from our region, we report this case. Intra-lesional or systemic administration of amphotericin-B, flucytosine, calciferol with or without potassium iodide and INH has produced better results than ketoconazole, thiabendazole and topical heat and X-ray therapy. Variable results with ketoconazole alone have been reported. In the above referred case, terbinafine and itraconazole halted the progression of the fungus. In our opinion, a high clinical suspicion by the dermatologist and collaborative efforts done by the clinician with the pathology and microbiology laboratory has resulted into an excellent diagnosis which was unfortunately not revealed during last 15 years in spite of approaching several clinicians, from various places by the patient. Secondly, lack of microbiology facilities at most of the places may lead to under or wrong diagnosis leading to delay in proper treatment in these patients. REFERENCES: 1. Seema V. Pradhan et al; Indian Journal of Dermatology, Venerology and Leprology 2007, Vol 73, Page no 176 2. Sharma NL, Mahajan V, Sharma RC, Sharma A., 2002., Subcutaneous pheohypomycosis in Indiaa case report and review. Int. J. Dermatol. Vol 41(1), p-16-20. 3. Jagdish Chander Textbook of medical mycology 3rd edition 2009.P -181 4. Rakesh Bharti, S K Malhotra, Singh Manjit Bal, Indian journal of dermatology, venereology and leprology, 1995, vol 61(1), p 54,55 5. Sharma NL, Sharma RC, Grover PS, Gupta ML, Sharma AK, Mahajan VK(1999).,
Chromoblastomycosis Chromoblastomycosis in India. Int. J .Dermatol 38(11)., 846- 51. Rajendran C, Ramesh V, Misra RS, Kandhari S, U. preti HB, Datta K K(1997) . Chromoblastomycosis in India. Int. J. Dermatol 36(1), p-29-33. Kikuchi Y, Kondo M, Yaguchi H, Hiruma M, Ikeda S. 2007. A case of chromoblastomycosis caused by Fonsecaea pedrososi presenting as a small plaque on the left upper arm: a review of reported cases of dematiaceous fungal infection in Japan. Nippon Ishinkin Gakkai Zasshi. 48(2) 85-9. 8.. Chromoblastomycosis in India Nandlal Sharma, Ramesh Chander Sharma, Prem singh Grover, ML Gupta, AK Sharma, VK Mahajan International journal of dermatology 2001, v 38(Nov), p 846 -851. Vyas MC, Joshi YR, Bhargava N, Joshi KR, Tanwar RK. 2000. Cerebral chromoblastomicosis a rare case report of cerebral abcess and brief review of literature a case report.Indian .J. Pathol. Microbiol.43 (1), p 81- 10. Garg N, Devi IB, Vajramani GV, Nagarathna S, Sampath S, Chandramouli BA, Chandramukhi A, Shankar SK.Central nervous system cladosporiosis: an account of ten cultureproven cases. Neurol India, 55(3): 282-8.
6.
7.
8.
9.
10.
NJIRM 2011; Vol. 2(1).Jan-March
eISSN: 0975-9840
pISSN: 2230 - 9969
Page
59
You might also like
- Complete Outline SpecificationsDocument16 pagesComplete Outline SpecificationsChoco MartiniNo ratings yet
- Safety House StructuralDocument1 pageSafety House StructuralChoco MartiniNo ratings yet
- Definite ArticleDocument5 pagesDefinite ArticleChoco MartiniNo ratings yet
- Suffixes Spelling RulesDocument4 pagesSuffixes Spelling RulesChoco Martini100% (1)
- Modal Verb CanDocument15 pagesModal Verb CanChoco MartiniNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- DkaDocument83 pagesDkaRajaKumar Ponnana100% (1)
- Pelvic FracturesDocument17 pagesPelvic FracturesDiane IsmaelNo ratings yet
- Foreign Body AspirationDocument4 pagesForeign Body AspirationpriscaNo ratings yet
- MagnecalmfactsheetDocument5 pagesMagnecalmfactsheetKeith TippeyNo ratings yet
- Acute Epididymoorchitis and Torsion of Testis: Seminar 6Document37 pagesAcute Epididymoorchitis and Torsion of Testis: Seminar 6Kumutha MalarNo ratings yet
- Dr. Gyan P. SinghDocument4 pagesDr. Gyan P. SinghMohammed AL-TuhamiNo ratings yet
- Management of Stroke PDFDocument6 pagesManagement of Stroke PDFtarmo angsanaNo ratings yet
- Module 7 Taking Vital SignsDocument7 pagesModule 7 Taking Vital SignsMary Joy CejalboNo ratings yet
- Electrolyte Disturbances Causes and ManagementDocument19 pagesElectrolyte Disturbances Causes and Managementsuci triana putriNo ratings yet
- Phenylketonuria PkuDocument8 pagesPhenylketonuria Pkuapi-426734065No ratings yet
- Sleep Disorders in Children and Adolescents: Deepti Shenoi MDDocument50 pagesSleep Disorders in Children and Adolescents: Deepti Shenoi MDCitra Sukri Sugesti100% (1)
- Îeéuwûéaéié Uréékéï: (Diseases of Tongue)Document87 pagesÎeéuwûéaéié Uréékéï: (Diseases of Tongue)Pranit Patil100% (1)
- Fundamentals of NursingDocument44 pagesFundamentals of Nursingtheglobalnursing100% (2)
- Lecture - 7 - Work - Capacity, - Stress - and - Fatigue (Autosaved)Document51 pagesLecture - 7 - Work - Capacity, - Stress - and - Fatigue (Autosaved)Aizat RomainoNo ratings yet
- Chronic PeriodontitisDocument3 pagesChronic Periodontitisapi-537687828No ratings yet
- Master Tecniques TornozeloDocument834 pagesMaster Tecniques TornozeloOrtopedia FabioNo ratings yet
- Topic 5. MEDICAL TECHNOLOGY EDUCATIONDocument7 pagesTopic 5. MEDICAL TECHNOLOGY EDUCATIONSophia GarciaNo ratings yet
- 68 AdaptiveDocument17 pages68 AdaptiveAmit YadavNo ratings yet
- Family Therapy and Systemic PracticeDocument4 pagesFamily Therapy and Systemic PracticeUyên TrươngNo ratings yet
- EpsiotomyDocument2 pagesEpsiotomyJazzlyneNo ratings yet
- Letter Explanation To DoctorDocument1 pageLetter Explanation To DoctorDonnaNo ratings yet
- Mia SmsDocument8 pagesMia SmsGlasiNo ratings yet
- Anesthesia Management For Pulmonary Hypertension PatientsDocument18 pagesAnesthesia Management For Pulmonary Hypertension PatientsAliNasrallahNo ratings yet
- Revisiting Structural Family TherapyDocument2 pagesRevisiting Structural Family TherapyKim ScottNo ratings yet
- Etiology, Classification and Clinical Approach: EndophthalmitisDocument42 pagesEtiology, Classification and Clinical Approach: EndophthalmitisHieLdaJanuariaNo ratings yet
- EM Basic - Pocket Guide PDFDocument97 pagesEM Basic - Pocket Guide PDFHansK.Boggs100% (1)
- Thrombocytopenia Brief DiscussionDocument11 pagesThrombocytopenia Brief Discussionriel100% (3)
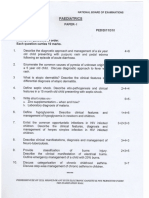
- Paediatrics: Final Exam National Board of Examinations December 2011Document4 pagesPaediatrics: Final Exam National Board of Examinations December 2011AlolikaNo ratings yet
- Acute Otitis Media: Jama Patient PageDocument1 pageAcute Otitis Media: Jama Patient PageS. JohnNo ratings yet
- Approach To The Adult With Epistaxis - UpToDateDocument29 pagesApproach To The Adult With Epistaxis - UpToDateAntonella Angulo CruzadoNo ratings yet