Professional Documents
Culture Documents
Handouts Nutrition Set B
Uploaded by
Kashien Arianna ReglosOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Handouts Nutrition Set B
Uploaded by
Kashien Arianna ReglosCopyright:
Available Formats
Vitamins This Session Describe the general characteristics of vitamins; Explain the health benefits of each vitamin; State
the recommendations for vitamins to maintain normal bodily functions; and Name the potential health risk of consuming too much and too little of a vitamin. Vitamins are substances in food which the body must have in order to be healthy. FAT-SOLUBLE TYPE: Vitamins A, D, E, K WATER-SOLUBLE VITAMINS Vitamin C B-vitamins or the B-complex Thiamin Riboflavin Vitamin B6 Folate Vitamin B12 Biotin Pantothenic acid Niacin FAT-SOLUBLE VITAMINS CHARACTERISTICS Do not dissolve or mix with water Unaffected by normal temperature and methods of food preparation. Are absorbed in the intestine along with fat. WATER-SOLUBLE VITAMINS CHARACTERISTICS Easily affected by cooking processes and exposure to air. Vitamin C is quickly destroyed by heat (dry or moist), exposure to air, presence of an alkali, and water. Thiamin is easily destroyed by prolonged cooking. Riboflavin is destroyed if heated in the presence of alkali (such as baking soda) and when exposed to light. Niacin is the most stable of the B vitamins in normal cooking process. WATER-SOLUBLE VITAMINS CHARACTERISTICS Because water-soluble vitamins dissolve in water, the body cannot store them in large amounts; The kidneys filter out any extra coming from the diet. Conservation Sensitivity of vitamins to cooking processes Vitamins are particularly vulnerable to destruction. Five factors responsible for most nutrient loss in foods: Heat Cooking in water Exposure to air Use of baking soda Exposure to light Cutting fruits into serving bites only when they are about to be eaten; Not overcooking vegetables, especially the leafy and green varieties; Not adding baking soda on green vegetables Use of only minimal water in cooking Not soaking vegetables before cooking Storing cut up foods, especially vitamin-C-rich foods in airtight wrappers and juices in closed containers Avoiding prolonged storage Keeping skin of fruits and vegetables intact
Roles, Food Sources, Health Effects The FAT-SOLUBLE VITAMINS Forms: Retinol Retinoic acid Precursor: beta carotene You need vitamin A for cells which line passages in your body such as inside the GIT and nostrils. You also need it to see at night as it helps certain cells in the eyes adjust to the dark. Helps to keep skin healthy It helps prevent cancer RETINOL (animal foods) Liver Egg yolk Cream, butter Fortified milk and cheese Fortified margarine BETA CAROTENE (plant foods) Green and yellow vegetables Deep orange fruits and vegetables Hypovitaminosis A Night blindness -slow recovery of vision after exposure to flashes of bright light at night Xerophthalmia thickening, opacity, and irreversible blindness Xerosis an early sign of xerophthalmia characterized by drying of the cornea Anemia small-cell type Cessation of bone growth Painful joints Tendency for tooth decay Diarrhea Changes in the lining of the gut Kidney stones Impaired growth Red blood cell breakage Nosebleeds Bone pain Risk of hip fracture Growth retardation Headaches Nausea and vomiting Abdominal cramps Weight loss Dry skin Loss of hair Ergocalciferol (D2) Cholecalciferol (D3) Dihydroxy vitamin D Precursor: cholesterol Vitamin D can be produced in the body through sunlight Exposure:
Generally b/n 9am and 3 pm, about 20 to 30 minutes for 2 to 3 times per week. Fortified milk, butter, margarine and cereal Egg Liver Helps in building of strong bones and teeth Aids in keeping nerves ad muscles healthy Growing children need extra from foods; otherwise their bones do not harden and become bent (called rickets). Osteomalacia (in adults) softening of bones with joint pains, bending of spine and bowed legs. High blood calcium and muscle spasm Excessive thirst Headaches Irritability Weakness Nausea and vomiting Kidney stones Anorexia Death FUNCTIONS: Vitamin E protects fats, vitamin A and other helpful body chemicals from damage. It makes blood more efficient in carrying oxygen around the body. PUFA-rich plant oils Leafy green vegetables Wheat germ Almonds, hazel nuts Seeds Whole-grain cereals Breakdown of RBC leading to anemia Nerve degeneration Weakness Difficulty walking and leg cramps General discomfort Phylloquinone or K1 (plants) Menaquinone or K2 (produced by bacteria in the colon) Liver Milk Vegetable oils Green leafy vegetable Eggs, meats Bacterial synthesis in the digestive tract Vitamin K aids in normal blood clotting. Without it you would bleed to death. Vitamin K is needed for the formation of a protein (osteoclastin) that binds calcium in the bone. Reduced ability to form clots leading to excessive bleeding and easy bruising No known side effects or toxicity symptoms from consuming excess. The WATER-SOLUBLE vitamins Most B vitamins help release energy from food
Others aid in making healthy blood cells (B-12, B-6, Folate) and nerves (B-1, Folate, B-6, Niacin) FUNCTIONS stimulates appetite supports normal function of the heart, nerves and muscles Present in all nutritious foods in moderate amounts Pork, beef, liver Whole or enriched grains Seeds and nuts legumes Beriberi Anorexia Mental confusion Muscle weakness Fatigue Nerve damage Paralysis Heart failure Health effects due to Excess B1 toxicity rarely happens FUNCTIONS: Supports normal vision and skin health ARIBOFLAVINOSIS CHEILOSIS FUNCTIONS: Sore throat Swollen red tongue Magenta tongue Eye irritation Skin rash FOOD SOURCES: Milk Yogurt Meats Cottage cheese Enriched cereals Green vegetables FUNCTIONS For healthy skin Keeps the normal activity of stomach, intestines and nervous system Meat Nuts and legumes Whole grains Enriched breads Milk Fish Poultry All protein-containing foods PELLAGRA Flaky skin rash on exposed to Diarrhea Dementia GLOSSITIS - black, smoothness tongue Failure to grow
sunlight
areas
of the
confusion needed in the making of fatty acids, amino acids and purines needed for the formation of glycogen in muscle and liver widespread in foods can be synthesized in the GIT natural deficiency is unknown Helps the body use amino acids to form tissue proteins Helps convert tryptophan to niacin Helps make red blood cells Support the synthesis of neurotransmitter and the myelin coating around nerves. Whole grains Poultry, meat, fish and shellfish Seeds and legumes Liver and kidney Milk and eggs Fruits and green-leafy vegetables Abnormal brain wave pattern Muscle twitching Greasy dermatitis Rashes Bloating Depression Fatigue Impaired memory irritability FOOD SOURCES Animal foods like liver, meat, fish, poultry, eggs None in plants Helps in the formation of new cells including red bloods cells Helps maintain nerve cells. Megaloblastic Anemia or pernicious anemia - due to lack of intrinsic factor Deterioration of the nerves leading to paralysis Hypersensitivity of the skin No reported symptoms Folacin Folate Pteroyglutamic acid FOOD SOURCES Chicken liver Breakfast cereals Spinach, cooked broccoli Lentils, chickpeas, lima and kidney beans Black beans, baked beans with pork FOOD SOURCES Tomato juice Orange Fortified wheat bread Wheat germ EFFECTS OF DEFICIENT INTAKE Megaloblastic anemia large immature red blood cells Glossitis Heartburn Diarrhea, constipation EFFECTS OF DEFICIENT INTAKE Frequent infections
Smooth red tongue Depression, mental confusion Fainting Neural tube defects (malformation of central nervous system in fetus) in pregnant woman EFFECTS OF EXCESS INTAKE Helps release energy in the body Helps to make fatty acids and cholesterol Widespread in foods Vomiting, GI distress Insomnia Fatigue Muscle cramps Not recognized Vitamin C Helps build strong resistance to infection Promotes healing of cuts, bruises, bone break (fractures), and bleeding gums Vitamin C Serves as antioxidant, protecting the body from cell damage Vitamin C Provides the matrix for bone growth Helps the body absorb iron better Vitamin C ASCORBIC ACID Vitamin C DEFICIENCY DISEASE/ SYMPTOM Vitamin C DEFICIENCY DISEASE/SYMPTOM Vitamin C SYMPTOMS OF EXCESS Inhibitors Vitamin inhibitors Absorption of vitamins may be inhibited by certain medications of food: Vitamin B1 alcohol, sulfur drugs, antacids, tea, coffee, red cabbage, water Vitamin inhibitors Vitamin B12 oral contraceptive pills, alcohol, sulfur drugs, some tranquilizers, and antidepressants Niacin sulfur drugs and alcohol Vitamin inhibitors Pantothenic acid caffeine, sulfur drugs, and alcohol Vitamin B6 alcohol, oral contraceptive pill, some antibiotics like isoniazid Vitamin inhibitors Vitamin B12 antacids, laxatives, oral contraceptive pill, alcohol, anticonvulsants Folate alcohol, contraceptive pill, aspirin, alcohol, anticonvulsants Vitamin inhibitors Vitamin C contraceptive pill, anticonvulsants, analgesics Biotin sulfur drugs Vitamin inhibitors Vitamin A alcohol, very low fat diet Vitamin D mineral oil, alcohol, laxatives, some anticonvulsants, and glucocorticoids Vitamin E large intakes of vitamin K, laxatives
Vitamin K warfarin, mineral oil, laxatives, large doses of vitamin E Thank you. Health effects due to Excess B1 toxicity rarely happens B2 no reported symptoms Niacin - diarrhea, heartburn, nausea and vomiting, ulcer irritation, fainting, dizziness, abnormal liver function, glucose intolerance, low blood pressure Minerals This Session Describe the general characteristics of minerals; Explain the health benefits of each mineral; This Session Minerals are inorganic elements. The body cannot make them. Some are needed in minute amounts while others are in even smaller quantity (ultra-trace minerals). They give no caloric value. Macronutrient Minerals Macrominerals are elements required in the body in the amount greater than 100 mg daily. CALCIUM 1.5% to 2.2% FUNCTIONS: as main ingredient of bones and teeth helps the body form blood clot when needed FUNCTIONS: For transmission of nerve impulse and thus helps in the normal functioning of the nerves Supports muscle contraction and relaxation FUNCTIONS: Helps the body fight high blood pressure, colon cancer, and premenstrual syndrome Helps in maintaining favorable acid-base balance FOOD SOURCES: Milk and milk products Oysters Small fishes (bones are eaten like sardines and anchovies) Other significant FOOD SOURCES: Tofu Green vegetables Legumes Fortified packaged foods DEFICIENCY DISORDERS: Stunted growth in children Osteoporosis (low bone mass) DEFICIENCY DISORDERS: PROBLEMS WITH EXCESS INTAKE: Calcium can interfere with absorption of iron, zinc, and magnesium Stone formation in the kidney ROLE IN THE BODY: 1. Main component of energy molecule ADP 2. For strong bones and teeth 3. Participates in the release of energy from carbohydrates and fat ROLE IN THE BODY: 4. Transports fatty acids in the body
5. Helps the body maintain acid-base balance and fluid balance 6. Components of cells genetic material, cell membranes and lipoproteins FOOD SOURCES: All animal tissues Whole grain cereals Legumes DEFICIENCY SYMPTOMS Dietary deficiency is seldom happen except in alcoholism, severe kidney disorder, and total parental nutrition. 1. Weakness 2. Poor growth 3. Seizures EFFECTS OF TOO MUCH: - calcium excretion in the urine MAJOR FUNCTIONS: 1. For normal muscle contraction including the heart 2. Facilitates many chemical reactions such as the making of protein 3. Helps maintain water balance 4. Helps maintain electrolyte balance 5. Supports the normal functioning of the nerves FOOD SOURCES All whole foods, meats, milk, fruits, vegetables, grains, and legumes. DEFICIENCY SYMPTOMS: Dehydration Muscular weakness Abnormal heart beat Numbness and confusion SYMPTOMS OF EXCESS INTAKE: Muscular weakness Triggers vomiting ROLE IN THE BODY: 1. Supports strong bones and teeth 2. Critical cofactor for over 300 enzyme systems 3. Takes part in the release of energy in the body; 4. For normal muscle and nerve functions. FOOD SOURCES: Nuts and legumes Whole grains Dark green vegetables Seafood Chocolate, cocoa milk HEALTH EFFECTS: POOR OF INTAKE 1. Unlikely; 2. Depletion sometimes occur along with other body disturbances in certain diseases: chronic renal failure protein energy malnutrition chronic malabsorption severe diarrhea chronic alcoholism HEALTH EFFECTS: POOR OF INTAKE 3. Patients with the following conditions may experience deficiency:
Patient whose parathyroid gland was removed Those who have prolonged use of diuretics HEALTH EFFECTS: TOO MUCH INTAKE FUNCTIONS IN THE BODY: For normal muscle activity Helps the body maintain proper distribution of water in the body Aids in the transmission of nerve impulse. FOOD SOURCES: Salt, soy sauce, and processed foods Abundant in most foods except fruits FOOD SOURCES: Plant foods vs. animal foods milk, cheese, eggs, meat, fish have higher sodium content than fruits, vegetables and cereals HEALTH EFFECTS: LACK OF INTAKE Muscle cramps Mental apathy Lack of appetite Palpitation HEALTH EFFECTS: LACK OF INTAKE Depletion can occur if sweating is very profuse as may happen in hot climates. Sodium loss may occur in certain conditions: Prolonged diarrhea and vomiting Loss of exudates from burns Underactivity of the adrenal glands HEALTH EFFECTS: EXCESS INTAKE High blood pressure in sensitive persons. MAIN ROLES IN THE BODY: FOOD SOURCES: HEALTH EFFECTS HEALTH EFFECTS ROLES IN THE BODY: 1. An important part of amino acid lysine and methionine 2. Component of biotin, thiamin and the hormone insulin; 3. Combines with toxic substances to form harmless compounds; 4. Assist in keeping acid-base balance FOOD SOURCES: Meat Eggs Milk, cheese Legumes and nuts HEALTH EFFECTS TOO LITTLE INTAKE: Not known; protein deficiency would occur first Not known in humans TOO MUCH INTAKE: Not known in humans End of this Session THANK YOU FOR YOUR KIND ATTENTION. Trace minerals are needed in very small quantities (less than 100 grams per day) in the human body.
Eating a diet that consist of a variety of foods is the best way to ensure enough intakes of these microminerals. FUNCTIONS 1. For normal and healthy blood cells 2. For making of Hemoglobin which delivers oxygen to cells Myoglobin which holds oxygen in muscles FUNCTIONS: 3. Participates in the detoxification of drugs and toxic compounds in the liver and intestine FOOD SOURCES: Heme iron found in animal foods; better absorbed Non-heme iron found in plant foods; requires vitamin C for efficient absorption FOOD SOURCES: Clams, oysters, beef liver, other meats, eggs Whole grains, enriched breads and cereals FOOD SOURCES: Dark green vegetables Legumes Nuts HEALTH EFFECTS: Poor Intake causes ANEMIA, hypochromic, microcytic type HEALTH EFFECTS: Too much intake leads to HEMOSIDEROSIS and HEMOCHOMATOSIS FUNCTION: Part of a thyroid hormone that regulates the rate of energy burn and also controls the rate of tissue activities such as growth, development and metabolic rate. FOOD SOURCES: Iodized salt Seafood Bread with iodized salt HEALTH EFFECTS: (deficiency disorders) ENDEMIC GOITER CRETINISM poor mental and physical development of the child HEALTH EFFECTS: (deficiency disorders) Hypothyroidism hyperthyroidism HEALTH EFFECTS: (excessive intake) Depresses thyroid activity
Goiter-like thyroid enlargement FUNCTIONS: 1. Works with vitamins in protecting the body from harmful free radicals that can cause cell damage, cancer and heart disease FUNCTIONS: 2. Needed for making thryoid hormones which control cells activities FOOD SOURCES: Seafood Organ meats and other meats Grains and vegetables, depending on soil condition DEFICIENCY DISORDERS: Predisposition to heart disease Muscle discomfort Weakness TOXICITY SYMPTOMS: Nausea Abdominal pain Nail and hair changes Nerve damages FUNCTIONS: 1. Works with iron to form hemoglobin 2. Part of several enzymes related to energy production, collagen and elastin formation FUNCTIONS: 3. A component of CERULOPLASMIN that transport iron FOOD SOURCES: Organ meats Seafood Nuts and seeds Cocoa Whole grain foods DEFICIENCY DISORDERS: Hypercupremia low levels of copper in the blood, occurring in nephrosis and malabsoprtion SYMPTOMS OF EXCESS INTAKE: Wilsons disease Abdominal pain and cramps Vomiting and diarrhea FUNCTIONS IN THE BODY: 1. Works with zinc and copper in a major antioxidant compound; 2. Facilitates the use of carbohydrate and fat in the body as energy FUNCTIONS IN THE BODY: 3. Acts as coenzyme in the formation of urea
FOOD SOURCES: Widely distributed in foods. DEFICIENCY SYMPTOMS: None reported in humans SYMPTOMS DUE TO EXCESS: Nervous system disorders FUNCTION: Strengthen bones and teeth DEFICIENCY DISORDERS: Increased tooth decay, particularly up to the age of 13 years. EFFECT OF TOO MUCH INTAKE: Mottling or discoloration of teeth (FLUOROSIS) FUNCTIONS IN THE BODY: 1. Works with insulin to help the body use blood sugar; 2. Stimulates formation of fat and cholesterol FOOD SOURCES: Meats Unrefined foods Fats, vegetable oils EFFECT OF DEFICIENCY: Diabetes-like condition EFFECT OF EXCESS: Occupational exposures damage skin and kidneys ROLE IN THE BODY: 1. Needed by enzymes involved in producing waste products before they are excreted (detoxification) ROLE IN THE BODY: 2. Involves in the oxidation of body compounds FOOD SOURCES: grains, corn legumes, peas dairy products kidney, liver, spinach cauliflower DEFICIENCY SYMPTOMS: Rarely; only seen in hospital patients on deficient feed tubes impaired growth reduced appetite EFFECT OF EXCESS: None reported in humans
FUNCTIONS IN THE BODY: 1. part of insulin and many enzymes; 2. involves in the making of genetic material and protein FUNCTIONS IN THE BODY: 1. Participates in immune reactions; 2. Helps transport vitamin A in the body; FUNCTIONS IN THE BODY: 1. For normal taste perception; 2. For faster wound healing; 3. For the making of sperm and normal fetal growth . EFFECTS OF DEFICIENCY: Growth failure in children; Loss of taste; Delayed sexual maturation and impotence; EFFECTS OF DEFICIENCY: Poor wound healing; Hair loss; Eye and skin lesions. EFFECTS OF TOO MUCH INTAKE: 1. Fever 2. Diarrhea 3. Nausea and vomiting 4. Anemia EFFECTS OF TOO MUCH INTAKE: 4. Dizziness 5. Muscle incoordination 6. Kidney failure 7. Risk of atherosclerosis High phosphorus, salt or protein intake Alcohol, oxalic acid, phytic acid, dietary fiber Large doses of B complex pills Some laxatives, antibiotics Excess sodium intake Alcohol, coffee Some diuretics and anti-gout drugs Calcium supplements especially calcium carbonate, phytates Antacids Alcohol, diuretics, Phytates Tannins (in tea, coffee, red wine) Calcium supplements Aspirin, narcotics (codeine, morphine) Anti-gout drugs Phytates and fiber in whole grains and beans
Large amount of tea/coffee, alcohol Diet high in non-heme iron Iron or calcium supplements Some diuretics, contraceptive pill Hormone replacement therapy High zinc diet, zinc supplements Large intake of Fe, Mn, Mo, and vitamin C antacids Goitrogenic substances in foods (turnips, cabbage, cassava, and Brussels sprouts) End of this Session THANK YOU FOR YOUR KIND ATTENTION. W ATER and Body Fluids 1. List the functions of water in the body; 2. Identify the consequences of poor water intake; and 3. State the recommendations of experts to meet individual water needs. Water: A vital nutrient 1. Water is an essential macronutrient. 2. It is the precious fluid that keeps the body functioning at an efficient and healthy level. 3. An appropriate amount of fluids must be present in the body because it transports nutrients and carries away waste. 4. Water provides the medium for chemical reactions and carries medicines to the proper places in the body. 5. It acts as lubricant and cushion around joints and inside the eyes, the spinal cord, and, in pregnancy, the amnionitic sac surrounding the fetus in the womb. 6. It also hydrates skin, helps in the regulation of body temperature and ensures proper blood volume. BODY WATER COMPOSITION Over half of the body weight is water. BODY WATER COMPOSITION Of the total body fluids: 2/3 is within the cells 1/3 is outside the cells. BODY WATER COMPOSITION Newborns body at term is about 75% to 80%. BODY WATER COMPOSITION An average adult male has 60% of body weight and an average adult female has 50% of body weight. FLUID INTAKE Fluid intake is supplied to the body via three routes: 1. oral fluids 2. solid foods 3. metabolic water FLUID INTAKE ORAL FLUIDS by ingestion of liquids FLUID INTAKE SOLID FOODS - from preformed fluid foods esp. fruits and
FLUID INTAKE from the production of water during nutrient metabolism Metabolic Water The estimated water produced for every 100 grams of energy nutrients: Fat 107 ml Carbohydrate 55 ml Protein 41 ml Fluid Excretion The kidneys typically produce about 1 to 2 L of urine daily. However, urine volume is actually highly variable depending on the amount of fluid intake and the amount of waste products that need to be eliminated. Fluid Excretion Materials that normally must be excreted in largest amount by the kidney are products of protein metabolism, mainly, urea. Fluid Excretion In addition, excess sodium, potassium, and chloride must be removed. WATER REQUIREMENTS: Extensive physical activity, such as in sports, increases the water requirement because water is lost in sweat and breathing. More water is required for the higher metabolic work involved in the physical activity. WATER REQUIREMENTS Conditions that affect the normal functioning of the body such as in the case of diarrhea, water retention (in kidney or liver failure), fever, coughing and a runny nose, will increase the amount of water needed. WATER REQUIREMENTS Age plays an important role in determining body needs: infants needs more water per day compared to older children and adults. SYMPTOMS OF DEHYDRATION 1 to 2 % body weight loss: EFFECTS OF DEHYDRATION 3 to 4 % body weight loss - impaired physical performance - dry mouth - reduction in urine - flushed skin - impatience - apathy EFFECTS OF DEHYDRATION 5 to 6 % body weight loss: difficulty in concentrating headache irritability sleepiness impaired temperature regulation increased respiratory rate EFFECTS OF DEHYDRATION 7 to 10 % body weight loss:
vegetables
- dizziness, spastic muscles, loss of balance, delirium, exhaustion, collapse WATER RECOMMENDATIONS To maintain healthy body fluid levels in the body, intake has to be balanced with excretion. WATER RECOMMENDATIONS Water needs vary, depending primarily on age, diet, activity, environmental temperature, and humidity. Accordingly, a general water requirement is difficult to establish. WATER RECOMMENDATIONS Fluid needs are best met by water, but milk and juices can account for part of the days recommended intake. Alcoholic beverages and those containing caffeine are not good alternatives. Gen. guidelines in estimating needs: Infants require 1.5 ml per kilocalorie expended Gen. guidelines in estimating needs: Children (1-18 years) If weight is 10 to 20 kilos: 1000 ml + 50 ml per kg for each kg in excess of 10; Gen. guidelines in estimating needs: Children (1-18 years) If weight is more than 20 kilos: 1500 ml + 20 ml per kg for each kg in excess of 20 kilos Gen. guidelines in estimating needs: Adults need 1.0 to 1.5 ml per kcal expended; generally 10-12 glasses a day for most adults; More glasses are needed for those who are perspiring considerably. Gen. guidelines in estimating needs: Older person (65 and above): 1500 ml Gen. guidelines in estimating needs: Pregnant women: Extra 300 ml above normal requirements RATIONALE: This additional water intake is needed as fluids are continually rerouted to the fetus and amniotic fluid. Gen. guidelines in estimating needs: Lactating women (1-6 months): Additional 750 to 1000 ml. RATIONALE: Breastfeeding increases fluid loss through production of milk. Higher protein intake, more water With increased protein intake, an additional 100 ml per gram of nitrogen intake is needed. Higher protein intake, more water SAMPLE CALCULATION: A person on a high-protein diet of 100 grams protein per day at 2500 kilocalories will require a total of 4,100 ml of water: HOW: [2500 ml + (100 6.25 g N / gram CHON)] Keeping enough body fluids Health experts suggest the following tips to maintain adequate fluids in the body: 1. Take water breaks throughout the day; Keeping enough body fluids
Health experts suggest the following tips to maintain adequate fluids in the body: 2. Always carry a jug or bottle of water with you in the office, in the car, jeepney, or on the train. To maintain enough body fluids: 1. Have a glass of water or juice with your meals. Start off with a cup of soup. How to maintain enough body fluids 4. Drink water before, during, and after exercise or physical activity. Is bottled water better? A lot of people believe that bottled water is better and safer but in reality, bottled water may not be any safer than tap water. The standards that regulate bottled water are no more rigid than those regulating tap water. Which is better among bottled water? Distilled water can be considered the safest choice among bottled water. Distillation procedure In distillation process, nonvolatile chemicals are removed, and the heat destroys bacteria and other microbial contaminants. Thirst and water needs Thirst cannot be relied on to ensure the body is getting enough water. Not drinking water enough to replace losses can be a problem and may lead to low body fluids. Thirst and water needs People dont or cant always drink water when they are thirsty. The best way is to maintain proper fluid balance is to drink regularly. Weight loss remedies and DHN A lot of weight-loss medications readily availed from the market can cause increased fluid loss. Weight loss remedies and dehydration Consumption of diuretics, drugs that excrete fluid via urine, can result in serious dehydration. Severe dehydration is associated with impaired physical and mental function and even death. Remember . . . Make a habit to drink fluids even you dont feel thirsty. End of this session Nutrition in Pregnancy and Lactation Objectives 1. Explain the benefits of adequate nutrition to mother and baby during pregnancy and lactation; 2. List and explain common nutrition-related concerns among pregnant and lactating women; and 3. Suggest appropriate food choices to meet nutritional their dietary needs. Importance of adequate nutrition Nutrition prior to and throughout pregnancy and lactation has a great impact not only on the mothers health but also on growth, development, and health of her child after birth. Importance of adequate nutrition Research indicates that in addition to heredity and socio-economic environment, fetal health and intelligence can be determined by the mothers nutrition.
Impact of poor nutrition Poor nutrition, either the mother is underweight or overweight, presents medical risks of pregnancy and childbirth. Effect of prepregnancy weight Good pregnancy outcome is ensured when the mother enters pregnancy with healthy body weight, good nutrient stores, and sound eating habits. Effect of prepregnancy weight Infant birthweight strongly links to prepregnancy weight and is the most powerful single predictor of the childs future health and survival. Babies who were born with low birthweight are likely to have illnesses and are likely to die in the early months of life. in Pregnancy Protein intake Normal requirements based on age and sex plus additional of 9 to 10 grams per day throughout the pregnancy. Emphasize high-quality, complete protein foods. High-quality, complete protein foods Energy Requirements Adjust calorie intake depending on physical activity, current weight, and if the pregnant is a teen. Calorie Recommendation Normal requirements based on age and activity with additional of 300 kcal for the second and third trimester of pregnancy. Rationale for the kcal increase Additional energy is needed to support the growth of the uterus, the breast, the fetus, increase in blood volume, and the buildup of storage fat. For pregnant teens: Evaluate teens individually according to age and pre-pregnancy weight. Teens, aged 13 to 16 years old, should strive for pregnancy weight gain between 30 to 35 pounds to reduce the risk of delivering lowbirth weight infants. Monitoring adequacy of intake The best indicator of kcal adequacy is a constant weight gain of approximately 0.4 kg per week after the first trimester. Monitoring of body weight A sudden, sharp increase in maternal body weight after the 20th week of pregnancy may indicate water retention and the possible onset of complication called pre-eclampsia. Added energy is best obtained from carbohydrate foods: Energy Requirements Excess weight gain during pregnancy should be avoided. Too much weight gain has been associated with pregnancy complications, including Cesarean delivery, and later obesity. Carbohydrate intake Rationale: A generous amount of carbohydrate is critical to spare protein and to supply energy needs for higher basal energy expenditure and for building tissues. Carbohydrate food choices should emphasize minimally processed foods (unrefined carbo) so that other nutrients are also supplied. Best sources of carbohydrates: Blood sugar and pregnancy Pregnancy may precipitate the onset of diabetes in some women because placental hormones alter the way insulin works. Blood sugar may become abnormally high.
With gestational diabetes Women with gestational diabetes need to: select foods rich in complex carbohydrates and limit their consumption of concentrated sweets. Vitamin and Mineral Needs Nutrition experts recommend a multivitaminmineral supplement for women who are nutritionally at risk: Those carrying multiple fetuses Underweight or overweight at the beginning of pregnancy Women who gain insufficient or excessive weight during pregnancy Vitamin and Mineral Needs Adolescents Those who usually consume inadequate diet such as women who avoid eating all animal-derived food Vitamin and Mineral Needs Women who lack nutrition knowledge or who have limited financial means to buy enough foods Lactose intolerant More Folate and Vitamin B12 Rationale: High folate (400 to 600 micrograms a day) and vitamin B12 (2.6 micrograms per day) intake are critical for rapid cell multiplication of tissues and for the increase in the mothers red blood cells. Folate and Vitamin B12 Adequate folate is important to prevent neural tube defects. Getting enough Folate and Vit. B12 How to meet needs through food: 1. by eating 5 servings of fruits and vegetables daily 2. by taking of folate supplement Getting enough Folate and Vit. B12 Folate is found in green leafy vegetables, legumes, liver, orange juice, melons, whole-wheat products. Vitamin B12 may be obtained by consuming modest amount of meat, fish, eggs, or milk products. Strict vegetarians may need daily supplements. Vitamin D, Ca, P, F, and Mg Rationale: These are the nutrients needed to build skeleton of the fetus. Fluoride is important in the mineralization of the fetus bone and teeth. Fluoride supplementation is not recommended for pregnant who drink fluoridated water. Iron and Vitamin C Intake Rationale: (1) Iron-deficiency anemia in women and pregnant women is common; (2) Iron is needed in red blood cell production; (3) Vitamin C enhances absorption of iron from foods. Vitamin C enhances absorption of iron from foods. Vitamin C deficiency (as well as lack of vitamin E and magnesium) is linked to higher risk of preeclampsia, a pregnancy-induced hypertension. Iron and Vitamin C Intake Recommended intake is 27 to 38 mg/day, depending on pregnancy stage. Significant food sources include liver, oysters, red meat, fish, and other meats, dried fruits (mango, raisins, prunes), legumes (mongo beans, peas, lima beans), and dark green vegetables.
Iron and Vitamin C Intake Recommended intake is 80 mg/day. Vitamin C-rich foods include fresh fruits and vegetables, especially citrus fruits, melons, strawberries, potatoes. No other foods except for organ meats, such as liver and kidneys, contain vitamin C. Zinc Intake Rationale: (1) it is required for DNA and RNA synthesis; and (2) low zinc predicts low birthweight. Significant sources: protein-rich foods such as meat, shellfish, and nuts. Iron interferes with the bodys absorption and use of zinc, thus women taking iron supplements of more than 30 milligrams per day may also need zinc supplements of about 15 mg per day. On caffeine intake . . . At what dose and to what extent caffeine causes harm is still being investigated. Increased risk of miscarriage and low-birth weight is possible. Include in the meal plan sources of essential fatty acids like fish, seafood, and vegetable oils (corn oil, soy oil, sunflower oil). Other dietary recommendations: Vegan usually needs supplements containing vitamin B12 supplement, calcium, vitamin D (unless exposed to sunlight, iron, and zinc. Consumption of calcium-fortified soy milk or orange juice might be required as calcium content of a regular prenatal supplement is not enough. Other dietary recommendations: For excessive weight gain, the goal should be to restore eating patterns to match a normal growth curve. Dieting (low calorie intake) is not advisable during pregnancy. Water intake (6 to 8 glasses) Other dietary recommendations: Be sure to use iodized salt but avoid excesses. Include iodine-rich foods or an additional allowance of 25 microgram is recommended. Other dietary recommendations: It is sensible to omit alcohol. Alcohol is a known teratogen and is associated with birth defects; these effects are dose-dependent. Other dietary recommendations: Heavy drinking throughout pregnancy can result in fetal alcohol syndrome (FAS). Other dietary recommendations: Vegan usually needs supplements containing vitamin B12 supplement, calcium, vitamin D (unless exposed to sunlight, iron, and zinc. Consumption of calcium-fortified soy milk or orange juice might be required as calcium content of a regular prenatal supplement is not enough. Other dietary recommendations: For excessive weight gain, the goal should be to restore eating patterns to match a normal growth curve. Dieting (low calorie intake) is not advisable during pregnancy. Other dietary recommendations:
Pregnant women with high blood pressure (including those with preeclampsia) should limit salty food products like processed meats, canned goods, and snack chips. Managing heartburn: (1) consume small meals at frequent intervals; (2) drink fluids between meals but stay away from orange or grapefruit juice, soft drinks, chocolate, and coffee; Managing heartburn: (3) avoid spicy or fatty foods; (4) wait an hour after meals before lying down; and (5) wait two hours after eating before exercising. Alleviating morning sickness/nausea (1) eat dry toast, dry cereals, or crackers before getting out of bed in the morning; (2) try chewing gum or hard candies from time to time; Alleviating morning sickness/nausea (3) take small meals at frequent intervals; (4) avoid greasy foods and foods with offensive odors; Alleviating morning sickness/nausea (5) omit citrus juice, milk, coffee, or tea; (6) dont drink liquids with food. Easing constipation (1) drink at least 8 glasses of water or other non-caffeine and non-alcoholic fluids; (2) include fruits and vegetables daily; (3) enjoy dried fruits during snacks, especially prunes; and (4) select more often whole grain cereals and breads. When lactose intolerance is present: Substitute soy milk if regular, lactose-containing milk is not tolerated. If milk is totally omitted for medical reason, try to obtain calcium, phosphorus from other foods. In case of pica: (1) correct calcium deficiency or iron deficiency anemia if present through supplementation and emphasizing balanced diet. Pica has been linked to these deficiencies; In case of pica: (2) seek advice from health care professionals regarding the unfavorable effect of this behavior on nutritional status as well as on the fetus. Water retention: Edema of pregnancy does not require dietary intervention. Leg cramps during pregnancy may be relieved by magnesium or calcium supplementation. Pregnant women who are in particular need of nutrition counseling Less that 18 years of age at onset of pregnancy; Underweight (10% below the DBW) or overweight (20% above DBW) prior to pregnancy; Pregnant women who are in particular need of nutrition counseling Insufficient weight gain: gain of 1 kilo/month in the 2nd or 3rd trimester;
Excessive weight gain: gain of 3 kilos or more per month; Pregnant women who are in particular need of nutrition counseling Teenagers who are multigravidas; Women who are pregnant within 1 year of the last pregnancy; Pregnant women who are in particular need of nutrition counseling Women with any of the following medical problems: drug/alcohol abuse or addiction, diabetes, kidney or heart disease, anemia, seizure disorders, multiple food allergies, lactose intolerance, GI disease, especially malabsorption syndrome; Pregnant women who are in particular need of nutrition counseling Women with limited income and/or food sources; Vegetarians or those with unusual food habits (faddism, pica, etc); Multiple fetuses. During Importance of correct nutrition The physiologic needs of lactation are greater that those of pregnancy. Adequate nutrition of the mother supports successful lactation. By continuing to eat nutritious foods and enjoying enough amounts of foods and fluids throughout lactation, the mother who chooses to breast-feed her infant will be nutritionally prepared to provide enough breast milk. Importance of healthy eating The quality of milk is maintained at the expense of maternal stores. The nutrients in breast milk that are most likely to decline due to prolonged insufficient maternal intakes are vitamin B6, vitamin B12, and vitamin D. Because of the enormous benefits of breast-feeding, mothers are encouraged to breast feed their babies at least for the first 12 months of life. Breast milks unique nutrient composition and protective factors promote optimal infant health and development Calorie requirement: Throughout the lactation period, an additional 500-kcal energy intake above normal needs for age and activity is recommended. Rationale for the increment: This extra energy is based on three factors: (1) to fortify milk with enough calorie content; (2) to support milk production; and (3) for maternal adipose tissue storage. Calorie requirement: The period of lactation is the natural time for a woman to lose the extra fat she gained during pregnancy. Yet, an intake of <1200 kcalories per day is not advised since this will hold back milk production. Calorie requirement: Weight loss can be achieved by eating nutritious foods that are modest in calorie content. Protein requirement: Protein needs increases by 16 grams (first six months) and 12 grams (7 months onwards) grams per day over the normal recommendations for age. Eating protein foods of high quality (milk and milk products, egg, meats, poultry, and seafood) is suggested. Suggested fat intake
Fat should provide 20% to 35% of total calories. PUFA-rich foods are important Sources of polyunsaturated fatty acids must be emphasized in the diet because of their crucial role in fetal and infant retina and brain development. Regular consumption of fatty fish rich in omega-3 fatty acids is encouraged. Vitamin-Mineral Supplementation Only lactating women with poor diet or inadequate in one or more nutrients may need to take supplements. Adequate vitamin D will be necessary if maternal intake is poor or if infant receives little sunshine exposure. Water and fluids Fluid intake is higher during breastfeeding, about 8 cups or more to prevent DHN. Avoid alcohol, caffeine, and most drugs as they are transmitted through breast milk to infants. END OF THIS TOPIC Nutrition in 1. Describe the dietary needs of an infant fed during the first year, including the progression of solid foods; and 2. List and explain common nutrition-related concerns during infancy. Early nutrition affects later development, and early feeding sets the stage for eating habits that will influence nutrition status for lifetime. An infant grows faster during the first year than ever again. An infants birth weight doubles by about four to five months of age, and it triples by the age of one year. By the end of the first year, the growth rate slows considerably. A newborn requires only about 650 kilocalories per day and this is about 100 kilocalories per kilogram of body weight. Breast milk (or alternatively, iron-fortified milk) provides the needed calorie needs during the first year. Calorie allowance can be estimated using desirable body weight (DBW). To compute DBW: DBW (k) = [age (mo.) 2] + 3 To estimate calorie intake: Total energy allowance (TEA (kcals / day): First 1-6 months: 120 kcal per kilo DBW 7 months up to 1 year: 110 kcal per kilo DBW Milk and/or formula contribute the majority of energy in the diets of children throughout infancy. The risk of dehydration is ever present during infancy. Breast milk and formula normally provides enough water to replace losses from the skin, lungs, feces, and urine. Supplemental water is needed in case of diarrhea, vomiting, and when the infant is exposed to hot environment to prevent dehydration. Water intake must be higher once solid foods are given. Foods high in protein or electrolytes such as meat and eggs can cause dehydration if offered without water. Offer water as regularly as possible. Additions to diet, apart from milk, are not needed until about midinfancy.
Indications of readiness for solid foods include: (a) the infant can sit with support and can control head movements and (b) the infant is six months old. Introduce foods one at a time and give small amounts at the beginning. Sweet, sour, and salty foods are well tolerated. Bitter foods may have to be introduced over and over to develop tolerance, and, perhaps, appreciation. 4 to 5 months: Iron-fortified infant cereal, followed by other single-grain cereals mixed with breast milk, formula, or water Infants vary, and the program of additions depends on the individual babys developmental readiness, not on rigid schedule. Show pleasure when giving a new food to make the baby like to eat. Suggested amount: cup thin cereal or rice gruel; 2 tablespoons cooked dried beans, minced; 1 tablespoon cooked and flaked fish, meat or chicken and egg yolk; Suggested amount: 3 tablespoon ripe fruits; 3 tablespoon cooked and minced vegetables. 5 to 6 months: - Strained fruits and vegetables 6 to 8 months: Mashed or chopped fruits and vegetables juice from cup Suggested amount: 1 cup rice gruel or cereal; piece potato or other root crop; cup cooked and minced dried beans; Suggested amount: piece egg yolk and 2 tablespoons cooked and minced fish, meat, or chicken; cup ripe fruits; cup cooked and minced vegetables. Juices should be introduced in the diet of infants after age 6 months; that if introduced, 100% juices be used and juice be limited to 4 to 6 ounces daily*. *Am Academy of Pediatrics, 1998 8 to 10 months: (a) breads and cereals from the table; (b) soft, cooked vegetables and fruits from the table; 8 to 10 months: (c) finely cut meat, fish, chicken, casseroles, cheeses, yogurts, tofu, eggs, and legumes. Suggested amount: 1 cup rice gruel or cereal piece potato or other root crop 2 tablespoon margarine or oil (for cooking) Suggested amount: cup cooked and minced dried beans piece egg yolk and 2 tablespoons cooked and minced fish, meat, or chicken cup ripe fruits cup cooked and minced vegetables. 9 to 12 months:
Crackers, toast, plain meats, egg yolk, and finger foods Continue to introduce a variety of nutritious foods. Table foods (cooked without salt) in small portions may be blenderized and served as an option. A one-year-old baby should be eating many of the same foods as the rest of the family. Offer only bland foods and never highly salty foods and too much sugar. Never give leftover foods and handle babys food properly by keeping hands and utensils clean and sanitized. Suggested amount: 2 cups rice gruel or cereal; 1 piece potato or other root crop; 5 tablespoon margarine or oil (for cooking); to cup cooked and minced dried beans; Offer foods by spoon and cups at around 6 months. Begin with teaspoon and later a cup Feeding must be carefully watched by an adult. Observe possible cause of food allergy: New foods should be introduced singly and at interval (about 3 days apart) to allow detection of allergies. A food found to cause an allergy should be discontinued before introducing the next food. Foods that most often cause allergy: Common symptom of allergy: Foods to be avoided: sweets including baby food desserts (they are high in calories but have little essential nutrients); Foods to be avoided: canned vegetables (they often high in salt), raw carrots; Foods to be avoided: honey (because of the risk of botulism), peanut butter (choking hazards) and hard candies; Foods to be avoided: popcorn, whole grapes, whole beans, hotdog slices, and nuts (they might cause choking); Foods to be avoided: Sweets may be given occasionally but in limited amounts. Do not force food: Just give infants nutritious foods and let them select which they like and how much they will eat. Do not force food: If children refuse milk, provide alternatives like cheese and cream soups. If there is regurgitation: Position the infant at a 45 to 60-degree angle after a feed. When abdominal discomfort (colic) is a problem: In the case of diarrhea: (1) Continue breast-feeding infant; (2) give plenty of fluids, and if necessary, an oral rehydration solution made with table salt and sugar (3-finger pinch of sugar and 2-finger pinch of salt in 1 cup of boiled water);
(3) avoid too much fruit juices or hypertonic drinks and excessive fluid intake; banana may be included in the diet if the baby is old enough to eat; (4) if diarrhea is due to cows milk intolerance or allergy, eliminate milk and milk products and substitute lactose-free, hypoallergenic formula as per doctors prescription. Thank you for listening. NUTRITION in Childhood OBJECTIVES Shaping the childs food habit Early childhood is a critical time for the development of food preferences and eating patterns. Introducing the child early to good nutrition will help shape his food habits in later years. Changes in childs appetite A childs appetite declines markedly around the first birthday, consistent with the slowed growth rate. Thereafter, the appetite fluctuates. Research suggests that each childs food intake is high variable from meal to meal, but the total daily energy intake is constant; children adjust their energy intakes at successive meals, i.e. if they ate less at one meal, they will eat more at the next meal, and vice versa. Impact of eating together . . . Recent studies also show that eating meal as a family, at least once a day, can improve childrens food habits. Healthy eating must be a family affair; it begins at an early age. Avoiding not so healthy foods To prevent future problems related to food, parents should avoid introducing high-sugar foods and drinks while their kids are still very young. Fast-foods such as hamburger, fries, pizzas, and the likes, should be an occasional treat. Dietary Recommendations for Good Nutrition Energy Intake Childrens needs vary widely, depending on their growth and physical activity: Suggested kcalorie/ kilo Age desirable body weight 1 to 3 years 105 4 to 6 years 90 7 to 9 years 75 10 to 12 years 65 (boys); 55 (girls) Feeding the Child Encourage a variety of foods from each food group in amount suited to the childs appetite and needs. Meals and snacks should be served regularly and creatively to make dishes sufficient and appetizing. Food Pattern for 1-3 years old 2 1/3 cups, cooked rice or alternatives Alternatives: 1 cup cooked rice = 4 slices of loaf bread (17 grams each) or 4 pieces pandesal (about 17 grams each), or 1 cup pasta/noodles, or 1 small size root crop (180 g) Food Pattern for 1-3 years old 1 glass milk
1 glass = 4 tbsp powdered whole milk or cup evaporated milk diluted to a glass water. Food Pattern for 1-3 years old 1 serving meat or alternatives 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or 1 cups cooked dried beans. piece egg Food Pattern for 1-3 years old cup, cooked green leafy and yellow vegetables 2 tablespoons other vegetables (string beans, eggplant, etc.) Food Pattern for 1-3 years old medium size or 1 slice of a big fruit rich in vitamin C medium size or 1 slice of a big fruit (other fruits) Food Pattern for 1-3 years old 4 teaspoon sugar 6 teaspoons of fats and oils 4 to 6 glasses (240 ml each) water and beverages Food Pattern: 4 to 6 years old 3 to 4 1/2 cups, cooked rice and alternatives Food Pattern: 4 to 6 years old 1 glass milk 1 glass = 4 tbsp powdered whole milk or cup evaporated milk diluted to 1 glass water. Food Pattern: 4 to 6 years old 1 1/3 servings of meat/poultry/fish/dried beans/nuts 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or 1 cups cooked dried beans. piece egg Food Pattern: 4 to 6 years old 1/3 cup, cooked green leafy and yellow vegetables cup other vegetables (string beans, eggplant, etc.) Food Pattern: 4 to 6 years old to 1 medium-size or a slice of a big fruit rich in vitamin C to 1 serving other fruits like banana, avocado, or chico Food Pattern: 4 to 6 years old 5 teaspoons sugar (for milk, fruit juices) 6 teaspoons fats and oils (for cooking foods or as bread spreads like butter) 5 to 7 glasses water and beverages Food Pattern: 7 to 9 years old 4 to 5 cups, cooked rice and alternatives Food Pattern: 7 to 9 years old 1 glass milk 1 glass = 4 tbsp powdered whole milk or cup evaporated milk diluted to 1 glass water) Food Pattern: 7 to 9 years old 2 1/3 servings of meat/ poultry/fish/dried beans/nuts 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or 1 cups cooked dried beans piece egg Food Pattern: 7 to 9 years old 1/3 cup, cooked green leafy and yellow vegetables cup other vegetables (string beans, eggplant, etc.) Food Pattern: 7 to 9 years old to 1 medium-size or a slice of a big fruit rich in vitamin C to 1 serving other fruits like banana, avocado, or chico Food Pattern: 7 to 9 years old 5 teaspoons sugar (for milk, fruit juices)
6 teaspoons fats and oils (for cooking foods or as bread spreads like butter) 5 to 7 glasses (240 ml each) water and beverages Food Pattern: 10-12 years old 5 to 6 cups, cooked rice and alternatives Food Pattern: 10-12 years old 1 glass milk 1 glass = 4 tbsp powdered whole milk or cup evaporated milk diluted to 1 glass water. Food Pattern: 10-12 years old 2 servings of meat/poultry/fish/dried beans/nuts 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or 1 cups cooked dried beans. piece egg Food Pattern: 10-12 years old cup, cooked green leafy and yellow vegetables cup other vegetables (string beans, eggplant, etc.) Food Pattern: 10-12 years old to 1 medium-size or a slice of a big fruit rich in vitamin C to 1 serving other fruits like banana, avocado, or chico Food Pattern: 10-12 years old 5 to 6 teaspoons sugar (for milk, fruit juices) 6 to 8 teaspoons fats and oils (for cooking foods or as bread spreads like butter) 6 to 8 glasses (240 ml each) water and beverages CONCERNS about Eating Habits Not getting enough protective foods Mothers have a wealth of concerns when it comes to their childrens food intake. >Kids are not eating enough fruits and vegetables; many are picky eaters and a lot of them like to eat foods low in micronutrients. Calcium-rich foods are important >A glass of milk daily is encouraged to meet calcium, protein, and B vitamins needs. >For children who are not milk drinker, milk can be added to cereals, soups, dishes or fruit shakes. Calcium-rich foods are important Another way is to consume other foods high in calcium such as natural cheeses, small fishes eaten with bones. Morning meal 3. A good breakfast each day is important. The meal can be any combination of body-building, energygiving, and regulating foods. Children who eat breakfast do better at school, pay better attention in class and are less likely to have behavioral problems (Food Facts Asia, 2004). Fruits and veggies 4. Encourage any fruit or vegetable that the child will accept. Rejected fruit or vegetable (or other nutritious food) should be reintroduced repeatedly at some other times until the food is accepted. Keeping intake of some foods low 5. Concentrated sweets or foods with low-nutrient-density must be limited to small amounts and only occasionally.
Too much soft drink consumption is of particular concern as this habit is associated with higher energy intake and low consumption of essential nutrients. The role of parents . . . 6. Parent should guide children in choosing nutritious foods. Ground rules on frequency and timing of eating low-nutrientdensity foods must be set clear. For children with low-weight-for-age Ice cream or puddings and whole-grain or enriched breads are good choices for the underweight children. Serve nutritious snacks Recommended healthful snacks include: Fruit (assorted) shakes Bread with peanut butter or cheese Chocolate porridge with milk Oatmeal raisin cookies with milk Serve nutritious snacks. Recommended healthful snacks include: Homemade noodle soup with egg/chicken Bread and tuna Cereal with fruit and milk Luncheon meat on wheat bread Slices of fresh fruits Serve nutrient-loaded meals/snacks Pack nutritious lunch boxes. Packed lunch should supply at least 1/3 of the childs daily needs. Avoid giving strong foods Avoid serving too spicy and highly seasoned foods. These may destroy the appetite for the bland but highly nutritious foods. Young children do not like strong flavors; they prefer lightly to moderately seasoned foods. If iron deficiency anemia is present: (1) limit milk intake because it is a poor source of iron; (2) include iron-rich foods like eggs, poultry, canned pork and beans, cooked ground beef; peanut butter; mung bean sprouts and green peas; apple juice, dried fruits like raisins; fortified cereals and breads Lack of dietary intakes of iron (and zinc) by young children are associated with developmental delays, behavior changes, and an increased risk of infectious diseases In case of food allergy: identify the food that causes allergy; substitute alternative source of nutrient if the offending food is removed from the diet to prevent nutritional deficiency To prevent food dislikes: (1) offer a variety of food (2) serve warm and never hot foods (a childs mouth is much more sensitive than an adults); (3) food must be mild (a child has more taste buds) and preferably smooth; (4) serve only little portion of food and allow frequent meals. (5) When a food is introduced into them, kids generally reject these new foods but learn to accept then after repeated exposures. Studies suggest that 9 to 10 exposures to new food may be require before a child develop acceptance.
To prevent food dislikes: (6) For children who dislike vegetables, hide vegetables in cooking such as adding carrots in stews or pasta. To prevent choking: parents must always be alert when feeding round foods such as hotdog pieces, tough meat, popcorn, nuts, hard candies, etc. When poor appetite is a problem: (1) dont allow kids to snack too close to meal times; When poor appetite is a problem: (2) present food creatively by cutting foods into different shapes or use colorful plates and glasses; When poor appetite is a problem: (3) give nutrient-packed drinks at snack; When poor appetite is a problem: (4) provide small but frequent meals; When poor appetite is a problem: (5) keep nutritious snacks in key places at all times, including grab-and-go snacks like sandwiches, ready-to-drink juice or chocolate milk, and small boxes of cereals or cookies. If excess weight is a concern: Let the child follow a calorie-controlled diet (not a reduced-calorie diet) that is calculated based on age. This allows the child to lose weight gradually without jeopardizing normal growth and development. If excess weight is a concern: Excessive food restriction may create nutrient deficiencies and impair growth. If excess weight is a concern: Encourage the child to eat slowly and to stop eating when he is full; If excess weight is a concern: Promote the habit of drinking water throughout the day and give water after having the allowed milk or juice. If excess weight is a concern: Teach how to select low-fat snacks and to serve themselves correct portions Suggested low-fat snacks fresh fruit slices or fruit smoothies boiled camote, saba or sweet corn Binatog pancit guisado congee with egg or chicken flakes Champorado macaroni soup simple breads Suggested beverages low-fat milk after the age of two fruits juices instead of soda or soft drinks calamansi juice and lemonade If excess weight is a problem: Encourage caregivers to buy and serve lower-fat and lower-sugar food selections to promote preferences for more nutritious foods. If excess weight is a problem:
Limiting fat is not intended for children under 2 years old; they need a higher amount of fat to support rapid growth. If excess weight is a problem: Healthy meals can still include moderate amounts of a childs favorite foods even if they are high-fat, e.g., ice cream. If excess weight is a concern: Never force children to clean their plates. TV watching is linked with risk of obesity and type 2 diabetes. Encourage activities that will help children burn excess calories, e.g., swimming, badminton, and other games with frequent movements. End of this topic Adolescence OBJECTIVES: This Session Describe the nutritional needs of adolescents; and Identify the various diet-related concerns among teens and provide practical recommendations. Adolescence is a time of high nutrient demands because of the dramatic physical changes that accompany teenage growth. It is also a time when individuals experience increasing control over their food choices and developing dietary habits that affect their weight status and extend into adulthood. Nutritional concerns during this stage include eating disorders, inappropriate food patterns, the practice of food fads, and the use of alcohol and drugs. Nutritional needs are more demanding for adolescent girls who become pregnant. Teenage pregnancy is often the cause of malnutrition of the mother and the fetus. NUTRITIONAL Recommendations Energy Requirements The energy needs of teenagers vary greatly, depending on body size, rate of growth, and physical activity. Boys energy needs may be especially high since they experience a more intense growth spurt and develop more lean body mass than girls do. An average of 45 kilocalories is needed for every kilo of desirable body weight. More specifically, total calories may be estimated using the following guidelines: Suggested kcal/k Age desirable weight 13 to 15 years (boys) 55 13 to 15 years (girls) 45 16 to 19 years (boys) 45 16 to 19 years (girls) 40 Iron and Calcium Needs
Iron needs increase in girls as they begin to menstruate and in boys as their lean body mass develops. To meet this higher need, adolescents should consume iron-rich animal foods (liver and internal organs, beef, chicken, and fish), green leafy vegetables, legumes, and nuts. Iron and Calcium Needs If iron needs cannot be met by diet alone, supplements may be warranted. Include vitamin C-rich foods to absorb iron better. Vitamin C also helps maintain good defense system against common infection. Sources include citrus fruits, cabbage-type vegetables, dark-green vegetables, strawberries, papayas, lettuce, and tomatoes. Calcium requirements reach its peak during adolescence years. Milk is a significant source of calcium. Alternative sources (like sardines and other small fishes eaten with bones, oysters, tofu, green vegetables, and legumes) must be taken if the teenagers do not like milk. DAILY FOOD PATTERN for Good Nutrition 6 to 7 cups cooked rice or alternatives (13 to 15 years old) 6 to 8 cups cooked rice or alternatives (16 to 19 years old) Alternatives: 1 cup cooked rice = 4 slices of loaf bread (17 g each) or 4 pieces pandesal (about 17 g each), or 1 cup pasta / noodles, or 1 small size root crop (180 g) 6 to 8 teaspoon fats and oils (for cooking dishes and as spread for bread) 5 to 6 teaspoons sugar (to sweeten beverage and food) 2 servings meat and alternatives 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or cup cooked dried beans 1 medium-size egg, 3 to 4 times a week 1 glass milk 1 glass = 4 tbsp. powdered (whole) or cup evaporated, diluted to 1 glass water 1 cup, cooked vegetables (3/4 should be green, leafy and cup for other vegetables) 2 servings vitamin C-rich fruits and 1 serving other type of fruits WATER INTAKE 6-8 glasses water and other beverages. DIETARY CONCERNS Skipping of meals should be avoided especially breakfast. Emphasize selection of nutritious snacks but these should never be taken close to meal time. Fad and crash diets should be avoided because growth and development at this stage demand for higher nutrients. Soft drink delivers 30 to 55 milligrams of caffeine per 12-ounce serving since it may affect bone health. Cola beverages should not be taken more than three 12-ounce a day. Fruit juices and milk are better alternatives. When iron deficiency anemia exists:
Teenage girls are at high risks particularly when on a dieting and/or due to monthly menstrual period (1) include organ meat, lean beef, pork, fish and chicken regularly or add small amount of meat to vegetable dishes; When iron deficiency anemia exists: (2) avoid too much tea, coffee or alcohol; (3) eat vitamin-C rich foods with meals; and consume iron-fortified food products (read labels to identify these products). When bulimia nervosa is a problem: (1) Refrain from skipping meals; (2) avoid finger foods and select meals and snacks that require eating at the table; (3) eat meals at regularly timed meals consisting of a variety of foods in enough quantity When bulimia nervosa is a problem: (4) include fresh fruits or vegetable salad at meals to prolong eating times; (5) eat more high-fiber foods to increase bulk; When bulimia nervosa is a problem: (6) consume enough fluids, 8 to 10 glasses a day, mostly water; (7) include 30 minutes of exercise daily as this may be an important tool in controlling bulimia. If anorexia nervosa is present: The importance of food for growth, development and maintenance of the body should be explained to the client. She must be taught how to achieve a healthy weight through an adequate diet. An increase of 200 kcal per week above the usual intake can be made during the early stages of treatment, with greater increases as the patient becomes more comfortable with eating. Client should: (1) eat three meals with or without snacks depending on her preferences and food habits; and (2) follow a computed food plan but this is only as a guide and more foods can be eaten if desired. Other diet and food-related behaviors that merit concern in adolescents include: (1) inadequate food intake due to hectic schedule in school and outside home activities; (2) low consumption of fruits and/or vegetables; (3) high consumption of fast-food loaded with calories, saturated fats but low in micronutrients; (4) low intake of milk or other calcium-rich foods; and high consumption of street foods with questionable sanitation. NUTRITION Objectives 1. Explain the benefits of adequate nutrition in maintaining physical health and preventing chronic disease during the period of adulthood; and
2. Plan menus for adults with varying physical activities and/or lifestyle. Early Adulthood and Dietary Pattern With increasing age and independence, early adulthood is often characterized by exploration and marked by shifts in lifestyle. Early Adulthood and Dietary Pattern Major lifestyle changes which have potential to markedly influence meal patterns and eating habits include leaving the home of ones parents, entering full-time work or post secondary studies, getting married, and starting ones own family. Energy Needs The energy needs of an adult vary greatly, depending on body size, and physical activity. Estimating Energy Allowance Total daily calorie allowances may be projected using the guideline set by the NDAP*: Physical Activity Suggested kcal/k DBW
Male Female Sedentary 35 30 Light 40 35 Moderate 45 40 Heavy 50 *Nutritionist-Dietitians Assn of the Phils. Suggested Daily Food Patterns Energy-giving Foods 5 to 8 cups, cooked rice or substitute 5 to 8 teaspoons of sugar 6 to 9 teaspoons of fats/oils Equivalents of 1 serving portion of common starches* Suggested Daily Food Patterns Body-Building Foods 2 to 3 servings fish, meat, or poultry 1 piece med-sized egg (3-4 times/week) Equivalents of 1 serving portion 1 serving of meat = 2 pieces (60-g each) fish, or 1 slice lean meat (30 g, cooked), or cups cooked dried beans Suggested Daily Food Patterns Body-Building Foods 1 glass whole milk 1 glass = 4 tablespoon powdered milk or cup evaporated milk diluted to 1 glass water Suggested Daily Food Patterns Body-regulating Foods cup cooked, green leafy and yellow vegetables cup other vegetables Suggested Daily Food Patterns Body-regulating Foods 1 serving medium-sized or 1 slice of a big fruit rich in vitamin C 1 serving medium-sized or 1 slice of a big fruit (other fruit)
Water Intake 6 to 8 glasses of water and beverages Meal Planning Tips Eat more vegetables, fruits, and root crops. Meal Planning Tips Consume calcium-containing foods every day. Meal Planning Tips Limit intakes of salty and fatty foods. Use iodized salt instead of plain salt. Meal Planning Tips Consume recommended amounts of carbohydrate because excessive intake contributes to overweight and development of chronic diseases. Meal Planning Tips Include high-fiber foods: dried beans, peas, rolled oats, fruits, and vegetables. Meal Planning Tips Alcohol should be taken in moderation, about one to two drinks per day. One drink is equal to any of the following: 1 (12 oz) beer, 1 small glass (4 oz) wine, or 1 jigger gin Thank you. Nutrition in Objectives 1. Explain the benefits of proper nutrition in old age; 2. Plan sample menus to meet nutritional needs and prevent malnutrition. 3. Suggest appropriate food choices to manage diet-related health concerns. Basic nutrient needs do not decrease with age and some may even higher due to lower absorption and use of medications that interfere with nutrient utilization. Nutritional Concerns Physical changes that accompany aging may affect nutrition include: (1) tooth loss, gum disease, low secretion of saliva causing chewing and swallowing problems, which may reduce appetite; Nutritional Concerns (2) intestines lose muscle strength resulting in sluggish bowel that leads to constipation; (3) stomach inflammation, abnormal bacterial growth, and very low acid secretion leads to poor digestion and absorption; (4) the pancreas secretes less insulin and cells become less responsive, causing abnormal glucose metabolism; (5) reduced sensitivity of smell and taste can lead to poor appetite; (6) impaired physical function and poor eyesight can make food shopping and preparation difficult; (7) decline in lean body mass lead to decline in energy needs (8) increased frequency of urination may limit fluid intake. NUTRITIONAL Energy Needs of the Elderly There is a general decrease in energy needs because of slowing of metabolic rate, less physical activity, and loss of lean body mass (termed as sarcopenia). The following provides general rule in adjusting energy allowances for elderly.
This adjustment should only be made for elderly who are generally healthy and with no special conditions that increase the demand for extra calories. Adjustment in Energy Allowances Reduce caloric allowance by 10% for adults aged 50 to 59 years old. Adjustment in Energy Allowances Reduce caloric allowance by 20% for adults aged 60 to 69 years old. Adjustment in Energy Allowances Reduce caloric allowance by 25% for adults aged 70 y/o and above. Protein Needs Enough protein is especially important for older adults to support a healthy immune system and to prevent muscle wasting. Protein Needs The diet emphasizes low-fat, low-kcalorie sources such as: reduced-fat or nonfat milk lean portion of meats chicken without skin eggs, fish varieties legumes Protein Needs Soy milk and soy products are also good sources of protein and unsaturated fats. Protein Foods For elderly who are unable to eat enough amounts of meat, liquid supplements may be used to provide protein. Sustagen Premium is an example. Carbohydrate and Dietary Fiber Complex carbohydrates should be encouraged to spare protein from being used as an energy source. Best sources are unrefined bread and cereals, vegetables, and fruits Sugar Consumption Sugar intake must be less and it should be used only to enhance flavor and promote a nutritious diet. Fiber-rich foods Inclusion of fiber-containing foods is important to obtain vitamins, minerals and phytochemicals aside from fiber itself. Fiber-rich foods Fiber-rich foods along with liberal fluids aid in normal bowel movement, help lower cholesterol, and reduce risks of cancer. Fiber-rich foods When there is chewing difficulty, fiber-rich foods should be chopped really fine, mashed or blended. Fluid Needs Older adults are often at risk of dehydration. They dont feel as thirsty as they did when they were younger, but the need for fluids actually increases. Dehydrated older adults seem to be more prone to urinary tract infections, pneumonia, and pressure ulcers. Water and Fluid Intake
Liberal fluid intake (usually 8 to 10 glasses/day; at least 12 glasses if perspiring a lot) is suggested to promote normal bowel movement and prevent dehydration. Recommended sources of fluids Water, nutrient-fortified fruit juices, or decaffeinated drinks are good fluid choices. Poor sources of fluids Avoid alcohol or caffeine beverages due to their diuretic effect. Nutrient Supplements Food is still the best source of nutrients for everyone. Elderly people should choose foods high in vitamins and minerals but relatively fewer in calorie content. Nutrient Supplements In general, elderly often benefit from a balanced low-dose vitamin and mineral supplement. Too much supply must be avoided. Other critical nutrients Vitamin B12, B6, folate, vitamin D and calcium are most likely to be lacking in elderly persons. The gut is not as efficient in absorbing these nutrients. Foods that are good sources of vitamins B6, vitamin B12, Folate, iron, zinc and calcium should be often incorporated in the daily diet. Folic acid is necessary to retain mental acuity and reduce the incidence of stroke and heart disease while vitamin B12 helps maintain nerve function. Importance of Vitamin D Encourage vitamin-D fortified foods when there is limited sunlight exposure. But remember that aging also reduces the skins capacity to make vitamin D and the kidneys ability to convert to its active form. Salt Consumption The diet emphasizes reduced intake of sodium by using less amount of salt in food preparation and limiting salty foods. Add spices and flavorings to improve food flavors. MANAGING Difficulty in chewing/swallowing may need some foods that are soft or cut into small portions (ground or chopped, shredded, etc.) foods must be served with sauces or soup. Difficulty in chewing/swallowing Texture modifications should be individualized and used only when absolutely needed. Consider food preferences. Poor appetite provide appetizing meal by improving food presentation through consideration of their food favorites, by varying the food served, and serving food on plates with solid colors; encourage small frequent feedings; allow them to listen to music (from their youth) while eating meals. Constipation encourage more fluid intake, particularly water;
include high-fiber foods such as bite-sized fresh fruits and finely sliced vegetables, whole-grain bread and cereals like wheat bread, corn flakes with milk, cooked rolled oats, etc. Menopausal women eat a variety of fruits, vegetables and whole grains; select foods that are lower in fat; aim for at least 3 servings of dairy products a day; Menopausal women non-milk drinker should take a daily calcium supplement with vitamin D; use alcohol and caffeine in moderation; and exercise regularly. Elderly with Multiple Medications Elderly with numerous medications is likely to experience nutrient-drug interaction. If there are medications being taken which deplete nutrients, the client must be advised to improve food intake to counterbalance the effect. Encouraging active lifestyles Active lifestyle and regular exercise should be promoted. Several studies suggest that one of the reasons why Okinawans are healthier and live longer is because they have strong social networks for the elderly. These can help prevent or delay diseases and disabilities and help boost appetite.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Good and Cheap Cookbook PDFDocument89 pagesGood and Cheap Cookbook PDFgarrettNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
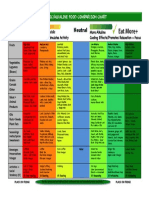
- Acid Alkaline Chart PDFDocument6 pagesAcid Alkaline Chart PDFCentaur Archer100% (1)
- Raw Food DilemmasDocument11 pagesRaw Food Dilemmas90002No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- All About WinesDocument55 pagesAll About WinesKashien Arianna ReglosNo ratings yet
- Blood Type DietDocument5 pagesBlood Type DietdraskyNo ratings yet
- Acidic Alkaline Food ChartDocument1 pageAcidic Alkaline Food ChartMaja TrajanovikjNo ratings yet
- Chapter 4 - AccessoriesDocument6 pagesChapter 4 - AccessoriesKashien Arianna Reglos100% (3)
- RP Diet Template FAQ 2Document23 pagesRP Diet Template FAQ 2Schuyler Brass100% (1)
- Flow of Food ServiceDocument19 pagesFlow of Food ServiceKashien Arianna ReglosNo ratings yet
- Care Sheet Parrots and ParakeetsDocument5 pagesCare Sheet Parrots and ParakeetsNina Sapphire100% (1)
- Table Etiquette and Cultural Differences: Chef Julie Ruth Cabatuando-SubaDocument23 pagesTable Etiquette and Cultural Differences: Chef Julie Ruth Cabatuando-SubaKashien Arianna ReglosNo ratings yet
- Flow of Food ServSafeDocument32 pagesFlow of Food ServSafecamparan100% (1)
- The Diabetic Exchange ListDocument16 pagesThe Diabetic Exchange ListJosephine Pedrina-BalatbatNo ratings yet
- Consumer Lifestyles in VietnamDocument45 pagesConsumer Lifestyles in VietnamLe Thiet Bao100% (1)
- Flow of Food IntroductionDocument15 pagesFlow of Food IntroductionKashien Arianna Reglos100% (3)
- Chapter 13 - Values and Image ImprovementDocument5 pagesChapter 13 - Values and Image ImprovementKashien Arianna Reglos75% (4)
- Application of Modified Atmosphere Packaging On Quality of Selected PDFDocument99 pagesApplication of Modified Atmosphere Packaging On Quality of Selected PDFDjany Souza100% (1)
- Before Ever After Book ReviewDocument9 pagesBefore Ever After Book ReviewKashien Arianna ReglosNo ratings yet
- Chap 14Document10 pagesChap 14Kashien Arianna ReglosNo ratings yet
- Week 1 5S of Good HousekeepingDocument12 pagesWeek 1 5S of Good HousekeepingKashien Arianna ReglosNo ratings yet
- Chap 12Document11 pagesChap 12Kashien Arianna ReglosNo ratings yet
- Presentation Week 2Document29 pagesPresentation Week 2Kashien Arianna ReglosNo ratings yet
- Chapter 8 - Dairy and Non-DairyDocument21 pagesChapter 8 - Dairy and Non-DairyKashien Arianna ReglosNo ratings yet
- Wines NewDocument45 pagesWines NewKashien Arianna ReglosNo ratings yet
- Tuition Fees Collegiate Sy 2011 2012 2ndsemDocument44 pagesTuition Fees Collegiate Sy 2011 2012 2ndsemKashien Arianna ReglosNo ratings yet
- Chapter 5 - FishDocument19 pagesChapter 5 - FishKashien Arianna ReglosNo ratings yet
- Chap 11Document13 pagesChap 11Kashien Arianna ReglosNo ratings yet
- Chapter 5.2 - ShellfishDocument17 pagesChapter 5.2 - ShellfishKashien Arianna ReglosNo ratings yet
- Chapter 4 - Meat 2Document22 pagesChapter 4 - Meat 2Kashien Arianna ReglosNo ratings yet
- Chap 10Document15 pagesChap 10Kashien Arianna ReglosNo ratings yet
- Chapter 15 - You and Your CareerDocument8 pagesChapter 15 - You and Your CareerKashien Arianna ReglosNo ratings yet
- Villa Immaculada Supreme Wedding Package 2011Document10 pagesVilla Immaculada Supreme Wedding Package 2011Kashien Arianna ReglosNo ratings yet
- Chap 13Document5 pagesChap 13Kashien Arianna ReglosNo ratings yet
- Chap 9Document17 pagesChap 9Kashien Arianna ReglosNo ratings yet
- Villa Immaculada DebutDocument4 pagesVilla Immaculada DebutKashien Arianna ReglosNo ratings yet
- VitaminsDocument7 pagesVitaminsKashien Arianna ReglosNo ratings yet
- Flow of Food Purchasing and ReceivingDocument23 pagesFlow of Food Purchasing and ReceivingKashien Arianna Reglos100% (3)
- Module7 - OrganizingDocument10 pagesModule7 - OrganizingKashien Arianna ReglosNo ratings yet
- Module6 - PlanningDocument38 pagesModule6 - PlanningKashien Arianna ReglosNo ratings yet
- Fruit & Vegetable Cleaning, Grading - 10LDocument14 pagesFruit & Vegetable Cleaning, Grading - 10LRENUSREE ENTERPRISESNo ratings yet
- Moringa Oleifera Alternative FlourDocument38 pagesMoringa Oleifera Alternative FlourhilaryblancelinsanganNo ratings yet
- South Korea: Presented by Navneesh RihanDocument19 pagesSouth Korea: Presented by Navneesh RihanNavneesh RihanNo ratings yet
- Diminishing Soil QualityDocument2 pagesDiminishing Soil QualityAlber Kristelle NalugonNo ratings yet
- PPT 2Document118 pagesPPT 2SalauddinKaderNo ratings yet
- Cancer20201206 Bonus Answer To Cancer DR Nalini Chilkov Anti Cancer Checklist Notes 4pages ICA+Fullscript+Bundles+and+Diet+Checklist+v1Document4 pagesCancer20201206 Bonus Answer To Cancer DR Nalini Chilkov Anti Cancer Checklist Notes 4pages ICA+Fullscript+Bundles+and+Diet+Checklist+v1AgnesNo ratings yet
- Paragraph Writing Grade 7Document20 pagesParagraph Writing Grade 7richie2885No ratings yet
- Structure & Written Expression: I. Sentence?Document7 pagesStructure & Written Expression: I. Sentence?Mohammad Rezzadian S. ANo ratings yet
- Bosch Steam CookBkDocument102 pagesBosch Steam CookBkSami WondimuNo ratings yet
- Diet Chart For Peptic Ulcer Patient, Peptic Ulcer Diet Chart - Lybrate.Document5 pagesDiet Chart For Peptic Ulcer Patient, Peptic Ulcer Diet Chart - Lybrate.santhosh kumarNo ratings yet
- Exemptions From GST: "It Is Not The End But The Start of The Journey"-Arun JaitleyDocument24 pagesExemptions From GST: "It Is Not The End But The Start of The Journey"-Arun JaitleyRadhika AggarwalNo ratings yet
- F122 Anglais3 L07Document18 pagesF122 Anglais3 L07AZZOUZ AHMEDNo ratings yet
- WH- QUESTION WORDS EXPLAINEDDocument9 pagesWH- QUESTION WORDS EXPLAINEDJhonny Sam VivasNo ratings yet
- KSIC2007Document98 pagesKSIC2007Yong Jee KimNo ratings yet
- Toward Improving The Food Self-Sufficiency Ratio : and Establishing Food SecurityDocument9 pagesToward Improving The Food Self-Sufficiency Ratio : and Establishing Food SecurityLeinadNo ratings yet
- MBA Report on Malabar Fruit Products CompanyDocument56 pagesMBA Report on Malabar Fruit Products CompanySHERIN1239No ratings yet
- Gat Exam 1Document16 pagesGat Exam 1snewemail1234No ratings yet
- WHFoods OnionsDocument16 pagesWHFoods Onionsgingerbd69No ratings yet
- Konsep Perubahan PerilakuDocument11 pagesKonsep Perubahan PerilakuGizi Kesehatan reproduksiNo ratings yet
- Want To Live A Longer Life Try Eating Like A CentenarianDocument2 pagesWant To Live A Longer Life Try Eating Like A CentenarianAurel AchilNo ratings yet