Professional Documents
Culture Documents
Anti Fungal Drugs
Uploaded by
Qairul AzmanOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Anti Fungal Drugs
Uploaded by
Qairul AzmanCopyright:
Available Formats
Antifungal drugs
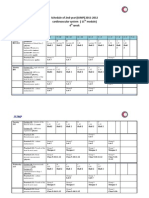
Drug Amphotericin B Characteristic -Broad spectrum -Inhibit cell membrane -Initial treatment, then replaced by other less toxic drugs -Poorly absorbed through GIT Amphotericin B complex and liposomal amphotericin B -Less infusion associated side effects -Decrease in nephrotoxicity (highly protein bound) Route of Administration Systemic (IV), topical Adverse Effects Systemic -Infusion related side effects -Chill, fever, muscle spasm, vomit, hypotension -Encountered by slow infusion rate and premedication of antihistamine, antipyretics -Nephrotoxicity, anaemia (decreased production of erythropoietin by kidney) Topical -Local irritation -Hypersensitive (rare) -Bone marrow toxicity -Elevated hepatic enzymes -Alopecia Treatment of Diseases Systemic -Some pulmonary fungal infection Topical -Candida infection Drug Interaction
Flucytosin
Azoles
-Narrow spectrum -Inhibit nucleic acid -Pro drug - need to be activated to form 5-fluorouracil (5-FU) -Specific to fungi as converted to 5-FU less in mammalian cells -Weak drug (used in combination to avoid resistance and for synergism) -Broad spectrum -Inhibit cell membrane through inhibition of cytochrome P450 dependant enzymes to synthesize sterols -Classified into: -Imidazoles (ketoconazole, clotrimazole) -Triazoles (1st generation: itraconazole and fluconazole;
Systemic (oral)
Systemic (oral/IV), systemic mucocutaneous, topical
Systemic -Triazoles (generally safe): -Hepatotoxicity -Idiosyncratic (no cross sensitivity occurs) -Imidazoles: -Endocrine disturbance (inhibition of gonadal and adrenal steroids due to P450 inhibition)
Systemic -Amphotericin-resistant fungi Systemic mucocutaneous -Dermatophytes -Candidiasis Topical -Dermatophytes -Candidiasis
-Inhibit cytochrome P450 -Greater for itraconazole and voriconazole, lower for fluconazole
Created by Qosru Iskandariah
Echinocandins
Griseofulvin
Terbinafine
Nystatin
2nd generation: voriconazole) -Triazoles differ from imidazole: -Broader spectrum -Better distribution -Less effect on human steroid synthesis as less affinity -2nd generation differs from 1st generation: -Extended spectrum -Active against fluconazoleresistant fungi -Narrow spectrum -Inhibit cell wall -Poor oral absorption -Specific to fungal glucan cell wall, so toxicity is infrequent -Inhibit microtubular -Taken up selectively by newlyformed skin and concentrated in keratin -Triazoles and terbinafine are used alternatively due to less problems with tolerability and adverse effects -Inhibit cell membrane -Accumulates in skin, nail, subcutaneous -More effective than azoles and griseofulvin -Inhibit cell membrane -Not absorbed through GIT, so no systemic effect -Never given parenterally due to serious systemic toxicity
Systemic (IV)
-Hepatotoxicity -Hypersensitivity -Fever
-Not metabolized in liver minimal drug interaction EXCEPT cyclosporin raised liver transaminase Systemic mucocutaneous -Dermatophyte - P450 inducer which may reduce efficacy of concomitant drug
Systemic mucocutaneous
-Hepatotoxicity -Hypersensitivity -Bone marrow suppression
Systemic mucocutaneous, topical
-GIT disturbance -Headache
Systemic mucocutaneous -Dermatophyte Topical -Dermatophyte
Topical
Created by Qosru Iskandariah
You might also like
- Antifung G6Document28 pagesAntifung G6Nigel MaphosaNo ratings yet
- Antimicrobial DrugsDocument83 pagesAntimicrobial DrugspooshadhanasekaranNo ratings yet
- Antifungal Agents 17971Document35 pagesAntifungal Agents 17971TES SENNo ratings yet
- Antifungal Agents: A Guide to Classification and Mechanisms of ActionDocument41 pagesAntifungal Agents: A Guide to Classification and Mechanisms of ActionDeribe BekeleNo ratings yet
- Antifungal DrugsDocument43 pagesAntifungal DrugsMohammed WasimNo ratings yet
- Anti Fungal AgentsDocument44 pagesAnti Fungal Agentsqruz Mohamed DiisNo ratings yet
- AntifungalDocument20 pagesAntifungalAliImadAlKhasakiNo ratings yet
- Antifungaldrugs 150519204813 Lva1 App6892Document54 pagesAntifungaldrugs 150519204813 Lva1 App6892Jennifer S ZiegenNo ratings yet
- Antifungal Drugs 3Document54 pagesAntifungal Drugs 3Mikee MeladNo ratings yet
- Antifungal Drugs: Dr. K. Sreedhara R. Pai Professor Department of Pharmacology Mcops, Mahe, MANIPAL-576 104Document88 pagesAntifungal Drugs: Dr. K. Sreedhara R. Pai Professor Department of Pharmacology Mcops, Mahe, MANIPAL-576 104jhanavi rajeshNo ratings yet
- Drug For Systemic Mycoses: Systemic Mycoses Can Be Subdivided Into Two CategoriesDocument39 pagesDrug For Systemic Mycoses: Systemic Mycoses Can Be Subdivided Into Two CategoriesCurex QANo ratings yet
- Anti-Fungal Drugs Guide for Mycosis TreatmentDocument6 pagesAnti-Fungal Drugs Guide for Mycosis Treatmentbilal ahmadNo ratings yet
- Clinical KHAIRANI's Antifungal AgentsDocument27 pagesClinical KHAIRANI's Antifungal AgentsRhomizal MazaliNo ratings yet
- AMPHOTERICIN B (Fungicidal Antifungal Agent W/ The Broadest Spectrum of Action)Document5 pagesAMPHOTERICIN B (Fungicidal Antifungal Agent W/ The Broadest Spectrum of Action)Lysa VeeNo ratings yet
- FTX Infeksi JamurDocument64 pagesFTX Infeksi JamurNafisah SofiaNo ratings yet
- Remove PDFcamp watermark with PDFcamp PrinterDocument4 pagesRemove PDFcamp watermark with PDFcamp PrinterElijah ChiumyaNo ratings yet
- 13 - Antibiotic III Nalidixic AcidDocument7 pages13 - Antibiotic III Nalidixic AcidMoataz TrabehNo ratings yet
- Systemic Antifungal Drugs for Fungal InfectionsDocument5 pagesSystemic Antifungal Drugs for Fungal InfectionsLysa VeeNo ratings yet
- Antifungals NagamaniDocument77 pagesAntifungals NagamaniNagu KopparapuNo ratings yet
- Antifungal Drugs: Types, Mechanisms & ClassificationDocument21 pagesAntifungal Drugs: Types, Mechanisms & Classificationعبدالرحمن دودينNo ratings yet
- Antifungal DrugsDocument20 pagesAntifungal DrugsboeykhNo ratings yet
- Antifungal AgentsDocument48 pagesAntifungal AgentsIman Saksouk100% (1)
- ANTIFUNGALS Lecture Notes Colour - 2022Document35 pagesANTIFUNGALS Lecture Notes Colour - 2022Dr Jaco MaraisNo ratings yet
- Antifungal AgentsDocument41 pagesAntifungal AgentsSami YGNo ratings yet
- Antifungal DrugsDocument28 pagesAntifungal DrugsKhairunnisa RasyidinNo ratings yet
- Revized 5 - Antifungal Medications - 2021Document28 pagesRevized 5 - Antifungal Medications - 2021احمد علىNo ratings yet
- Antifungal Classification and Mechanisms of ActionDocument55 pagesAntifungal Classification and Mechanisms of ActionAssssssNo ratings yet
- Antifungal Agents: EchinocandinsDocument2 pagesAntifungal Agents: EchinocandinsCourtney TownsendNo ratings yet
- Mycology AssignmentDocument7 pagesMycology AssignmenttenawNo ratings yet
- Pharma Uro Cotrimoxazole +fqsDocument14 pagesPharma Uro Cotrimoxazole +fqsHussein AlhaddadNo ratings yet
- Antifungal Agents: Dewi Selvina R & Instiaty Department of Pharmacology FmuiDocument37 pagesAntifungal Agents: Dewi Selvina R & Instiaty Department of Pharmacology Fmuisalsa2506No ratings yet
- 408 Antifungal Stu 1 07Document6 pages408 Antifungal Stu 1 07Hassan.shehriNo ratings yet
- Anti Fungal: Dr. Dr. Nico L Lumbuun, SPFKDocument45 pagesAnti Fungal: Dr. Dr. Nico L Lumbuun, SPFKAudhrey BNo ratings yet
- Anti - TB DrugsupdatedDocument35 pagesAnti - TB DrugsupdatedgNo ratings yet
- Antimicrobials MD 3 GISDocument26 pagesAntimicrobials MD 3 GISmus zaharaNo ratings yet
- Drug Use in LeprosyDocument23 pagesDrug Use in LeprosyIrish Nicole DCNo ratings yet
- Anti Fungal & Anthelminthic DrugsDocument62 pagesAnti Fungal & Anthelminthic DrugsKasturiRangan SrivatsaNo ratings yet
- Amphotericin B Pharmacology & Antifungal DrugsDocument24 pagesAmphotericin B Pharmacology & Antifungal DrugsshehranNo ratings yet
- Antifungal Drugs0Document26 pagesAntifungal Drugs0yaya mohaNo ratings yet
- Mycology AssignmentDocument9 pagesMycology AssignmenttenawNo ratings yet
- Antifungals AgentsDocument58 pagesAntifungals AgentsKofi Frimpong-MansonNo ratings yet
- Week 3 & 4 AntimicrobialsDocument120 pagesWeek 3 & 4 AntimicrobialsQuerubin DandoyNo ratings yet
- 15 Antifungal Drugs-Notes-3Document43 pages15 Antifungal Drugs-Notes-3Sindhu BabuNo ratings yet
- Anti Fungi / Anti JamurDocument32 pagesAnti Fungi / Anti Jamurrifqi_udinNo ratings yet
- Quinolones, Folic Acid Antagonist, and Urinary Tract AntisepticsDocument29 pagesQuinolones, Folic Acid Antagonist, and Urinary Tract AntisepticsAliImadAlKhasakiNo ratings yet
- Antifungal LectureDocument62 pagesAntifungal LectureVandana TayalNo ratings yet
- Antifungals MayerDocument28 pagesAntifungals Mayeralishba100% (2)
- Antifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesDocument18 pagesAntifungal Drugs: - Polyene Antibiotics: Amphotericin B, Nystatin - Antimetabolites: 5-Fluorocytosine - AzolesgopscharanNo ratings yet
- DR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtDocument45 pagesDR Retno Budiarti, DR., M.Kes Microbiology Department FK UhtalyaNo ratings yet
- PRESENTED TO: Sir Zafar Iqbal Presented By: Group-EDocument31 pagesPRESENTED TO: Sir Zafar Iqbal Presented By: Group-EAdia MasooraNo ratings yet
- Medical Management of Invasive Fungal Sinusitis-1Document20 pagesMedical Management of Invasive Fungal Sinusitis-1Nandini GuptaNo ratings yet
- Antifungal AgentsDocument23 pagesAntifungal AgentsDiriba feyisaNo ratings yet
- Introduction to Antimicrobial Chemotherapy: Mechanisms and SpectrumDocument31 pagesIntroduction to Antimicrobial Chemotherapy: Mechanisms and SpectrumPrasad SangishettyNo ratings yet
- AminoglycosidesDocument20 pagesAminoglycosidesHassan.shehri100% (5)
- Antifungal Drugs: Evi Sovia Pharmacology DepartementDocument55 pagesAntifungal Drugs: Evi Sovia Pharmacology DepartementKresna Denta ElygioNo ratings yet
- UAW Respiratory Antimicrobial Pharm Guide MedstuDocument19 pagesUAW Respiratory Antimicrobial Pharm Guide MedstuNabeel ShahzadNo ratings yet
- Anti-fungal Drug TargetsDocument19 pagesAnti-fungal Drug TargetsSparks Francis EzikaNo ratings yet
- Aminoglycosides AntibioticsDocument2 pagesAminoglycosides AntibioticsHlaSoe WinNo ratings yet
- Top 300 Drugs Pocket Reference Guide (2021 Edition)From EverandTop 300 Drugs Pocket Reference Guide (2021 Edition)Rating: 5 out of 5 stars5/5 (1)
- Adult Infectious Disease Bulletpoints HandbookFrom EverandAdult Infectious Disease Bulletpoints HandbookRating: 4.5 out of 5 stars4.5/5 (9)
- Night Shift Gen 1Document2 pagesNight Shift Gen 1Qairul AzmanNo ratings yet
- Night Shift Gen 2Document2 pagesNight Shift Gen 2Qairul AzmanNo ratings yet
- Study PlanDocument2 pagesStudy PlanQairul AzmanNo ratings yet
- The "A" Wave of The Atrial Pressure Curve Is Due To: A. Distension of The Atria Due To Blood Accumulation During Ventricular Systole B. S.A Node Contraction C. Contraction of The AtriumDocument8 pagesThe "A" Wave of The Atrial Pressure Curve Is Due To: A. Distension of The Atria Due To Blood Accumulation During Ventricular Systole B. S.A Node Contraction C. Contraction of The AtriumQairul AzmanNo ratings yet
- 3rdweek 2nd Year CVSDocument3 pages3rdweek 2nd Year CVSQairul AzmanNo ratings yet
- Modified Skill Lab Time Tabel MALYSIA Net.Document2 pagesModified Skill Lab Time Tabel MALYSIA Net.Qairul AzmanNo ratings yet
- 3rdweek - 2nd - Year CVS (With Histology)Document3 pages3rdweek - 2nd - Year CVS (With Histology)Qairul AzmanNo ratings yet
- Revision SecondDocument2 pagesRevision SecondQairul AzmanNo ratings yet
- Revision SecondDocument1 pageRevision SecondQairul AzmanNo ratings yet
- 4 WeekDocument3 pages4 WeekQairul AzmanNo ratings yet
- 4th Week 2nd Year CVSDocument3 pages4th Week 2nd Year CVSQairul AzmanNo ratings yet
- 2ndweek 2nd Year CVSDocument3 pages2ndweek 2nd Year CVSQairul AzmanNo ratings yet
- Hospital Timplet - 2Document142 pagesHospital Timplet - 2Qairul AzmanNo ratings yet
- The Exam Place in The Convention Center: The Time Table Exam For Module 1 For The 2 Year Students For 2011-2012Document1 pageThe Exam Place in The Convention Center: The Time Table Exam For Module 1 For The 2 Year Students For 2011-2012Qairul AzmanNo ratings yet
- 4th Week 2nd Year CVSDocument3 pages4th Week 2nd Year CVSQairul AzmanNo ratings yet
- Skill Lab Time Tabel MALYSIA Net.Document1 pageSkill Lab Time Tabel MALYSIA Net.Qairul AzmanNo ratings yet
- Jaw ThrustDocument1 pageJaw ThrustQairul AzmanNo ratings yet
- 1st Week 2nd Year CVSDocument3 pages1st Week 2nd Year CVSQairul AzmanNo ratings yet
- Orophryngeal Airway InsertionDocument1 pageOrophryngeal Airway InsertionQairul AzmanNo ratings yet
- Bag Valve Mask VentilationDocument2 pagesBag Valve Mask VentilationQairul AzmanNo ratings yet
- Chest AuscultationDocument1 pageChest AuscultationQairul AzmanNo ratings yet
- Heart AuscultationDocument1 pageHeart AuscultationQairul AzmanNo ratings yet
- Revision PhysiologyDocument3 pagesRevision PhysiologyQairul AzmanNo ratings yet
- Head Tilt/chin Lift: Clinical Learning GuideDocument1 pageHead Tilt/chin Lift: Clinical Learning GuideQairul AzmanNo ratings yet
- Sedative Hypnotic DrugsDocument1 pageSedative Hypnotic DrugsQairul Azman100% (1)
- Histology of The EarDocument3 pagesHistology of The EarQairul Azman100% (1)
- Accessory Nerve, HypoglossalDocument2 pagesAccessory Nerve, HypoglossalQairul AzmanNo ratings yet
- All WeeksDocument2 pagesAll WeeksQairul AzmanNo ratings yet
- Week 9 QuestionsDocument8 pagesWeek 9 QuestionsQairul AzmanNo ratings yet
- Blood Supply of The BrainDocument2 pagesBlood Supply of The BrainQairul AzmanNo ratings yet
- Effects of Restricted Feed Intake On Heat Energy BDocument14 pagesEffects of Restricted Feed Intake On Heat Energy BdrcdevaNo ratings yet
- Byproducts Utilization from Wheat Milling for Value Added ProductsDocument88 pagesByproducts Utilization from Wheat Milling for Value Added ProductsSivamani SelvarajuNo ratings yet
- Textbook of Oral Pathology-Anil G. Ghom, S. Mhaske (2013)Document1,050 pagesTextbook of Oral Pathology-Anil G. Ghom, S. Mhaske (2013)Khánh Vũ100% (2)
- Patient Satisfaction About Hospital Services: A Study From The Outpatient Department of Tertiary Care Hospital, Jabalpur, Madhya Pradesh, IndiaDocument6 pagesPatient Satisfaction About Hospital Services: A Study From The Outpatient Department of Tertiary Care Hospital, Jabalpur, Madhya Pradesh, IndiaVikram AripakaNo ratings yet
- School Form 1 (SF 1)Document6 pagesSchool Form 1 (SF 1)ᜇᜓᜇᜓᜅ᜔ ᜄᜌᜓᜐNo ratings yet
- CBR Guidelines 1st Meeting ReportDocument26 pagesCBR Guidelines 1st Meeting ReportJeffery SamuelNo ratings yet
- Updated Intake Packet 2020Document21 pagesUpdated Intake Packet 2020Allison GomoNo ratings yet
- Mission: DirectorateDocument7 pagesMission: DirectorateSRP GamingNo ratings yet
- Artifical Feeding Summary SheetDocument3 pagesArtifical Feeding Summary SheetCyrelle Jen TorresNo ratings yet
- Emergency Action Code 2013Document200 pagesEmergency Action Code 2013MiguelNo ratings yet
- Abstractbook Nsctls-2021 FinalDocument141 pagesAbstractbook Nsctls-2021 Finalijarbn editorNo ratings yet
- 187340592059Document100 pages187340592059Kashish PatelNo ratings yet
- Inguinal Hernia Repair - How It's Performed - NHSDocument4 pagesInguinal Hernia Repair - How It's Performed - NHSVishnu KumarNo ratings yet
- Meningitis Pathophysiology PDFDocument59 pagesMeningitis Pathophysiology PDFpaswordnyalupa100% (1)
- History of Experimental PsychologyDocument20 pagesHistory of Experimental PsychologyakmalrahmanNo ratings yet
- Nutrition Month Celebration 2019Document1 pageNutrition Month Celebration 2019jaymar padayaoNo ratings yet
- Jaw RelationsDocument44 pagesJaw Relationsjquin3100% (1)
- Understanding The RFA ("Relaxed Focused Attention") ProcessDocument5 pagesUnderstanding The RFA ("Relaxed Focused Attention") ProcessFriends of Max SkousenNo ratings yet
- Posterior AnatomyDocument17 pagesPosterior AnatomyAziz RanaNo ratings yet
- F&C Safety Data Sheet Catalog No.: 315407 Product Name: Ammonia Solution 25%Document7 pagesF&C Safety Data Sheet Catalog No.: 315407 Product Name: Ammonia Solution 25%Rizky AriansyahNo ratings yet
- Global Aid For Development Is A Chimera - It Brings No Substantial ChangeDocument6 pagesGlobal Aid For Development Is A Chimera - It Brings No Substantial ChangeDaya PrajapatiNo ratings yet
- Social WorkDocument13 pagesSocial WorkAyas uddinNo ratings yet
- Diabetes Treatment Report ProposalDocument4 pagesDiabetes Treatment Report ProposalrollyNo ratings yet
- Seychelles Travel GuideDocument5 pagesSeychelles Travel GuideAlex D.No ratings yet
- Lower Gi Finals 2019Document51 pagesLower Gi Finals 2019Spring BlossomNo ratings yet
- IPHO Accomplishment Report For May 2018Document12 pagesIPHO Accomplishment Report For May 2018ebc07No ratings yet
- FC Script-1lv8zpiDocument149 pagesFC Script-1lv8zpiPaulo CamiloNo ratings yet
- ICC - GMP Initiating Coverage Report - Oct 5 2017Document69 pagesICC - GMP Initiating Coverage Report - Oct 5 2017Anonymous 1pXKbrnNo ratings yet
- JournalDocument6 pagesJournalkhaiz_142989No ratings yet
- Outsourcing Aircraft MaintenanceDocument67 pagesOutsourcing Aircraft MaintenanceEromon Arumemi-IkhideNo ratings yet