Professional Documents
Culture Documents
Drug Classification
Uploaded by
RPh Krishna Chandra JagritCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Drug Classification
Uploaded by
RPh Krishna Chandra JagritCopyright:
Available Formats
CLASSIFICATION OF DRUGS
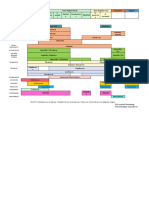
AUTONOMIC NERVOUS SYSTEM
We can classify drugs related to nervous system under 4 headings 1-Sympathomimetics. 2-Sympatholytics. 3-Parasympathomimetics. 4-Parasympatholytics.
SYMPATHOMIMETICS
These can be classifieds on following basis! A-ACCORDING TO MECHANISM OF ACTION 1- DIRECT ACTING ADRENERGIC A GONISTS They bind to adrenergic receptors without interacting with the presynaptic neurons and activate them. After their activation the 2nd messenger system begins to produce their pharmacological actions. Examples 1-Epinephrine. 2-Norepinephrine. 3-Dopamine. 4-Isoprotrenol. 5-Dobutamine. 6-Clonidine. 7-Phenylephrine. 2-INDIRECT ACTING ADRENERGIC AGONISTS They do not act directly by binding to receptors but cause the release of nor-epinephrine from presynaptic terminals thus potentiating the effect of nor-epinephrine on the presynaptic receptors. Examples 1-Amphetamine. 2-Tyramine. 3-Methylamphetamine. 4-Hydroxyamphetamine. 3-MIXED ACTION ADRENERGIC AGONISTS They release nor-epinephrine from presynaptic terminals and activate postsynaptic adrenergic receptors. Examples 1-Ephidrine. 2-metaraminol. B-ACCORDING TO CHEMICAL NATURE. 1-CATECHOLAMINES Examples 1-Epinephrine. 2-Norepinephrine. 3-Dopamine. 4-Isoproterinol. 5-Dobutamine. 2-NONCATACHOLAMINES Examples 1-Amphetamine. 2-Tyramine. 3-Methylamphetamine. 4-Hydroxyamphetamine. 5-Ehidrine.
6-Phenylephrine. C-ACCORDING TO RECEPTORS ON WHICH DRUG ACTS 1-ALPHA-1 SELECTIVE Examples 1-Phenylephrine. 2-Methoxamine. 3-Cirazoline. 4-Metazoline. 2-ALPHA-2 SELECTIVE Examples 1-Clonidine. 2-Guanabenz. 3-Oxymetazoline. 4-Methylepinephrine. 3-BETA-1 SELECTIVE Examples 1-Dobutamine. 2-Prenalterol. 4-BETA-2 SELECTIVE Examples 1-Salbutamol. 2-Turbutaline. 3-Ritodrine. 4-Fenoterol. 5-ALPHA AND BETA NON-SELECTIVE Examples 1-Epinephrine. 2-Norepinephrine. 3-Dobutamine. 4-Ephedrine. 5-amphetamine. 6-DOPAMINE RECEPTOR STIMULANTS Examples 1-Dopamine 2-Bromocryptine.
SYMPATHOLYTICS
1-ALPHA RECEPTOR ANTAGONIST These can be classified on following basis A-ACCORDING TO ALPHA RECEPTOR SELECTIVITY 1-ALPHA-1 SELECTIVE ANTAGONISTS Examples 1-Prazosin. 2-Terazosin. 3-Doxazosin. 4-Urapidil. 2-ALPHA-2 SELECTIVE ANTAGONIST Example 1-Yohimbine. 3-ALPHA 1 AND 2 NON SELECTIVE Examples 1-Phenoxybenzamine. 2-Phentolamine. 3-Tolazoline. 4-Ergotamine[ergot derivative] 2-ACCORDING TO DURATION OF ACTION
1-REVRSIBLE ALPHA BLOCKERS Examples 1-Phentolamine. 2-Prazosin. 3-Ergot derivative. 2-IREVERSIBLE ALPHA BLOCKERS Examples 1- Phenoxybenzamine[It is a nitrogen mustard and links both a-1(postsynaptically) and a-2(postsynaptically)This bond is irreversible and noncompetitive and new a receptor must be synthesized to revive the functions] B-BETA RECEPTOR ANTAGONIST 1-BETA-1 SELECTIVE ANTAGONIST Examples 1-Metoprolol. 2-Alebutolol. 3-Atenolol. 4-Esmolol. 2-BETA-2 SELECTIVE ANTAGONIST Examples 1-Butoxamine. 3-BETA 1 AND 2 NON SELECTIVE ANTAGONIST Examples 1-propanolol. 2-Pindolol. 3-Alprenolol. 4-Sotalol. 5-Timolol. 6-Nadolol. C-ALPHA AND BETA NON SELECTIVE ANTAGONIST Examples 1-Lobetalol. D-CENTRALLY ACTING SYMPATHOLYTICS Examples 1-Methyldopa. 2-Clonidine. 3-Guanabenz. E-ADRENERGIC NEURON BLOCKER Examples 1-Reserpine. 2-Guanithidine 3-Guanadrel.
PARASYPATHOMIMETICS
DIRECT ACTING
1-CHOLINE ESTERS Examples 1-acetylcholine. 2-Methacholine. 3-Carbachol.
4-Bethanechol. 2-CHOLINERGIC ALKALOIDS Examples 1-Muscarine. 2-Pilocarpine. 3-Arecholine. 4-Oxotremorine. They mimic the effects of acetyl choline by binding directly to Cholinoreceptors.
INDIRECT ACTING
A-REVERSIBLE 1-ALCOHOLS Examples 1-Edrophonium. 2-CARBAMATES Examples 1-Tertiary amines[can cross blood brain barier] They include Physostigmine. 2-Quaternary amines[can not cross blood brain barier] They include 1-Neostigmine. 2-Pyridostigmine. 3-Distigmine. 4-Tecrine. B-IRREVERSIBLE ORGANOPHOSPHORUS COMPOUND Examples 1-Disopropyl flouro phosphate. 2-Sarin. 3-Parathion. 4-Tabun. 5-Samon. 6-Eicothiopate. 7-TEPP. The irreversible anticholinesterases bind covalently to acetylcholinesterase.
PARASYMPATHOLYTICS
ANTIMUSCRINIC AGENTS THEY ARE CLASSIFIED INTO TWO SUB TYPES A-NATURAL Examples 1-Atropine. 2-Scopolamine. 3-Hyoscine. B-SYNTHATIC Examples 1-Homotropine. 2-Tropicamide. 3-Piorenzipine. 4-Isopropamide. 5-Benztropene 6-Benzhexone. GANGLIONIC BLOCKERS[ANTI NICOTINIC] Examples 1-Mecamylamine. 2-Nicotine. 3-Pempidine.
4-Hexamethonium. N-M BLOCKER[ANTI NICOTINIC] They can be further subdivided as follows A-DEPOLARIZERS Examples 1-Suxamethonium. 2-Decamethonium. B-COMPETITIVE Examples 1-Atracurium. 2-Doxacurium. 3-Metocurium. 4-Vecurium. 5-Tubocurarine. CHOLINEESTERASE REACTIVATOR Examples 1-Pralidoxamine. 2-Obidoxime.
OPHTHALMOLOGICAL DRUGS
THESE CAN BE CLASSIFIED UNDER 3 MAIM HEADINGS 1-ANTI GLAUCOMA DRUGS. 2-MIOTICS. 3-MYDRIATICS.
ANTI GLAUCOMA DRUGS
They can be further sub- classified as follows DRUGS FOR CLOSED GLAUCOMA Examples 1-Pilocarpine. 2-Manitol. 3-Physostigmine. 4-Acetazolamide. DRUGS FOR OPEN GLAUCOMA Examples 1-Pilocarpine[Parasympathomimetics]. 2-Eicothiopate[Parasympathomimetics].. 3-Physostigmine[Parasympathomimetics].. 4-Carbachol[Parasympathomimetics].. 5-Epinephrine. 6-Timolol.
MIOTICS
These can be further sub divided as follows. PARASYMPATHMIMETICS Examples 1-Pilocarpine. 2-Carbachol. 3-Neostigmine. 4-Physostigmine. 5-Eicothiopate. SYMPATHOLYTICS Examples 1-Tolazoline.
2-Phentolamine. 3-Reserpine.
MYDRIATICS
These can be further classified as below SYMPATHOMIMETICS Examples 1-Epinephrine. 2-Norepinephrine. 3-Phenylephrine. 4-Ephidrine. PARASYMPATHOLYTICS Examples 1-Atropine. 2-Scopolamine. 3-Homatropine.
SKELETAL MUSCLE RELAXANT
N-M BLOCKERS OR PEREPHERAL MUSCLE RELAXANT
These can be classified as follows DRUGS INHIBITING ACETYLCHOLINE OUT PUT Examples 1-Neomycine[Dec. calcium] 2-Gentamycine[Inc. magnecium] 3-Botulinium toxin[local anesthetic] DRUGS INHIBITING STORAGE AND SYNTHESIS OF ACETYLCHOLINE Examples 1-Hemicholinium. 2-Triethylcholine. DRUGS INHIBITING ACTION OF RELEASED ACETYLCHOLINE These can be further classified as follows A-NON DEPOLARISERS[COMPETITIVE N-M RELAXANTS] Examples 1-d-tubocurarine. 2-Gallamine. 3-Atracurium. 4-Pancuronium. 5-Mivacurium. B-DEPOLARISERS[NON COMPETITIVE] Examples 1-Succinylcholine. 2-Suxamethonium. 3-Decamethonium.
CENTRAL MUSCLE RELAXANTS
They can be further classified as follows BENZODIAZIPINES Examples 1-Diazepam. 2-Medazepam. BENZOXAZOLE DERIVATIVE Examples 1-Chlorzoxazone. 2-Benzimidazole. PROPANEDIOLE DERIVATIVE
Examples 1-Styramate. 2-Meprobamate. GABA ANALOGUE Examples 1-Baclofen.
DIRECT ACTING MUSCLE RELAXANT
Example 1-Dantrolene REFERENCES: R &Dale pharmacology of autonomic nervous system, Goodman, Gillman pharmacology.
AUTONOMIC NERVOUS SYSTEM
By, yasir akeel 3rd year pmc.
EPINEPHRINE
It is a potent stimulant of both E and F adrenoceptors thats why its effects on different target organs are complex . It is a direct acting drug and is related to sympathomimetic group of drugs. SITE OF PRODUCTION. It is produced mainly in adrenal medulla by chromaffin tissue. Its response varies in different organs
It constricts blood vessels in the skin -- because of E1 receptors It dilate - muscular arterioles because of F2 activation It reacts with E1 , E2 , F1 , F2 adrenoceptors. at low concentration F2-predominates dilation occurs at high conc. E1 predominates - constriction occurs
a. Blood pressure - large doses increases BP due to vasoconstriction mediated through E1 activation. increase HR, increase contraction of heart - F1 action
- low doses decreases BP, or no change increase HR, increase contraction potent bronchodilator b. Metabolic effects 1. increase glucose production - energy - F2 - fight or flight (ie. increase glucagon, glycogen to glucose) 2. Inhibition of insulin secretion - E2 3. Increase in oxygen consumption
4. increased renin from juxtaglomerular - F1- renin- angiotensin (vasoconstriction) - aldosterone -Na retention c. Pharmacologic effect of NOREPINEPHRINE 1. equal to Epin. in F1 action -- ie.) heart 2. slightly less a (ie. constriction) 3. no F2 activity -therefore, no dilation, no bronchodilation Norepinephrine- acts at E1, E2, F1 adrenocepters d. Pharmacokinetics of Epinephrine and Norepinephrine ABSORPTION 1. Absorption is poor with oral administration because drugs are rapidly conjugated and oxidized in intestinal mucosa and in liver (first pass metabolism). 2. Absorption is slow with subcutaneous administration because drugs cause local vasoconstriction. 3. Inhaled solution can be used for their action on respiratory tract ( F2 epinephrine) 4. Drugs IV administration must be careful so that heart does not fibrillate 5.It may be applied topically at mucous membrane to produce local effects. METABOLISM. . Liver is important in degradation - COMT, MAO enzymatic systems are involved in their degradation. EXCRETION. The metabolites of epinephrine appeared in urine. Only a small amount of epinephrine (unchanged) appears in urine. In pheochromocytoma la rge amounts of epinephrine and norepinephrine along with their metabolites appear in urine e. Therapeutic uses 1. Epinephrine a) Treat bronchospasm F2 b) Primary treatment for anaphylactic shock (allergy - exposure to antigen- bee venom -powerful antibody response Ig E. --- mast cells produce histamine and PG, get leakage of fluid and dilation of blood vessels, also bronchoconstricton ****- can't breath (often injected SC - there is some rapid absorption) c) Restore cardiac activity in cardiac arrest (in physiology lab --give to animals to restore heart activity 2. Norepinephrine - treating hypotension during anesthesia - not used much (given IV) f. Untoward effects (troubling) 1. anxiety - stimulus of CNS- later 2. headaches - increase blood flow to brain - F1 (increase heart rate and increase contraction)
3. cerebral hemorrhage - vasopressor effect 4. pulmonary edema - pulmonary hypertension above are due to alterations in blood flow g. Prolonged exposure can lead to receptor downregulation -- true for all receptors -- desensitization -- this has been studied for adrenoceptors -- ie. internalization of receptors -- or for F receptors ---FARK - Fadrenergic receptor kinase -- phosphorylates/disrupts G protein so no adenylyl cyclase to produce cAMP B. Other Sympathomimetic Drugs----Isoproterenol F1, F2
1. Pharmacologic effects a. mostly F effect b. IV- decreases peripheral resistance - F2 - decreases BP c. Blood pressure falls slightly - vasodilation, but also increased heart rate, increased contractility F1, thus there is an increased CO d. Relaxation of bronchial smooth muscle e. less hyperg lycemia (glycogen-glucose) than epinephrine (F2) because isoproterenol directly stimulates insulin secretion from pancreatic islet cells (glucose - to glycogen) 2. Pharmacokinetics a. oral unreliable b. good parenteral absorption - bypass GI (ie. SC no vasoconstriction) c. metabolized by COMT- little by MAO 3. Therapeutic uses a. bronchodilator b. cardiac stimulant 4. Untoward effects similar to epin. - if take too much, increase rate of sudden heart failure -- OD of inhalation (aerosol) - fatal ventricular arrhythmias C. Dopamine (intermediate of NE synthesis) a (high doses), F1 1. Pharmacologic effects
a. important NT of CNS, also has F1 effect, and causes release of NE from nerve terminals b. receptors for dopamine in kidney D1 (decrease kidney arterial resistance (vasodilation via increased cAMP) - increase pressure in kidneys - increase glomerular filtration. also D2 receptors - discuss later c. at high doses it has an a effect -- vasoconstriction 2. Pharmacokinetics a. similar to Epinephrine 3.Therapeutic uses a. shock, cardiogenic - loss of contraction b. congestive heart failure 4. Untoward effects a. Heart pain, arrhythmias, hypertension, short lived - because of rapid metabolism D. Phenylephrine E
1. Pharmacologic effects a. Direct stimulant of E receptors, less potent than NE but longer lasting because not broken down by COMT - vasoconstriction - increased AP (arterial pressure) - reflex decrease in the heart rate 2. Therapeutic usage a. nasal decongestant b. increases blood pressure c. to provide local vasoconstriction (As a 10% opthalmic solution for eyes "gets the red out") 3. Untoward effects a. cardiac irregularities b. administration to eyes and nose - can be systemically absorbed E. Ephedrine-occurs in various plants--used in China for 2000 yearsin US 70 years ago- first orally active sympathomimetic drug 1. Pharmacologic effe cts a. mixed-acting agent - that is both indirect and direct
1) Primary effect is indirect, it causes the release of NE from storage terminals. This is accomplished by displacing NE from storage granules inducing release 2) The direct effect - adrenergic receptors (E, F1, and F2) b. When administered IV - action similar to Epin. - but less potent, longer lasting. It does cause central nervous system stimulation - which can result in insomnia, nervousness, nausea, agitation 2. Pharmacokinetics a. Ephedrine- absorbed when taken orally b. resistant to COMT and MAO, therefore long lasting. 3. Therapeutic uses a. Treatment for bronchial asthma b. nasal decongestant [similar drug pseudoephedrine ---Sudafed] F. Amphetamine -CNS stimulant-talk about later -but also sympathomimetic -- mimics the action of the sympathetic nervous system 1. Pharmacologic effects a. Acts indirectly by releasing norepinephrine b. amphetamine also CNS stimulant --enters CNS easily 1) stimulates respiratory center -medulla 2) wakefulness 3) alertness 4) decreased sense of fatigue 5) elevation of mood 6) physical activity of athletes is improved 7) depresses appetite center in lateral hypothalamus (dextroamphetamine , Dexedrine- you buy dexatrim)
. a2 agonists [decreased cAMP] -used for treating hypertension Clonidine and methyl dopa prevent NE release
VII. Sympathetic Antagonists -Block adrenergic receptors -called sympatholytics -antiadrenergic A. E Adrenergic blocking agents -agonists- NE, phenylephrine 1. Phenoxybenzamine - orally - not used much anymore a. Mechanism of action 1) Binds covalently to the E receptor, producing irreversible blockade (not permanent--14-48 hours) -also blocks Histamine (H1), Ach. and serotonin receptors, role of these actions is not known. It is Non Competitive Inhibitor
b. Pharmacologic effects -antagonizes sympathetic responses mediated by a adrenergic receptors 1) Cardiovascular A) increases cardiac output - result of decreased TPR DP CO = --------TPR B) postural hypotension - lack of compensatory symp. vasoconstriction
PA in brain falls - normally sensed by baroreceptors - if phenoxybenzamine, no norepinephrine a receptor response - thus no increased TPR - called orthostatic hypotension drugs that block both E and F1 would produce even more orthostatic hypotension 2) CNS- stimulates CNS --direct effect -- nausea, hyperventilation c. Therapeutic uses 1) For acute hypertensive episodes ---due to sympathomimetics or MAO inhibitors i.e. tranylcypromine (a MAO inhibitor - derivative of amphetamine)
was once used to reverse vasoconstriction in shock but not anymore -- ie. constriction in gut and kidney- irreversible shock --Must be careful so that BP does not fall too much 2) To relieve vasospasm in Raynaud's Phenomenon - contraction of blood vessels to digits- results from great increase in sympathetic activity 3) Pheochromocytoma- tumor of adrenal medulla - get excess NE and E d. Untoward effects 1) Hypotension- reflex tachycardia 2. Phentolamine and tolazoline - slowly absorbed orally reversible E1, E2 adrenergic blockade. a. Pharmacologic effects -lowers blood pressure, reflex cardiac stimulation -used for acute hypertensive episodes B. F-adrenergic blocking agents (agonists -- Isoproterenol, Epinephrine) 1 . Propranolol - F1 and F2 competitive antagonist a. Pharmacologic effects 1) Propranolol decreases heart rate, CO 2) Decreases blood flow to most tissues except brain 3) Decreases oxygen consumption in coronary 4) Propranolol inhibits renin secretion (kidney) renin - angiotensinogenangiotensin I - angiotensin II - aldosterone- (angiotensin is a potent vasoconstrictor - decrease in resistance) F1 5) Increase airway resistance - F2 blockade b. Pharmacokinetics 1) Completely absorbed from GI tract, but large portion is metabolized by liver 2) 90% is bound to plasma proteins 3) Elimination half-time ~ 3 hours - but is much longer in cirrhosis c. Therapeutic uses 1) Treatment of hypertension
2) Prevention of angina pectoris (heart doesn't work so hard) 3) Prevention of ventricular arrh ythmias 4) Long term prevention of sudden death in patients with myocardial infarction 5) Prevention of migraine headaches --excessive pulsation of temporal arteries propranolol decreases HR and BP. 6) Reduces intraoccular pressure (ie. glaucoma) Other examples a. Timolol- blocks F1 and F2 b. Metoprolol- blocks F1 c. dozens of others in testing phase All three are important anti-hypertensive and antiarrhythmic
C. Agents that inhibit action of adrenergic nerves
1) reserpine- depletes stores of NE (MAO destroys NE) in nerve terminal hypertension treatment 2) Guanethidine- inhibits release from presynaptic terminal - long term antihypertensive - but get orthostatic hypotension because no E1 or F1 -stand up pass out) 3) Bretylium- blocks release of NE -- it also inhibits reuptake of NE into nerve terminal -initially used as antiarrythmic and antihypertension - via local anesthetic effect, same with guanethidine
You might also like
- Drugs PharmacologyDocument75 pagesDrugs Pharmacologyapi-25987870100% (16)
- Krav Maga Pressure Points - Military Hand To Hand Combat GuideDocument27 pagesKrav Maga Pressure Points - Military Hand To Hand Combat Guidebrogan98% (135)
- Pharmacology Complete Drug TableDocument6 pagesPharmacology Complete Drug Tableninja-2001100% (4)
- Comprehensive Pharmacology SummaryDocument25 pagesComprehensive Pharmacology Summarysubash p100% (1)
- Pharmacology Illustrated Notes: Calcium Channel Blockers and DigoxinDocument148 pagesPharmacology Illustrated Notes: Calcium Channel Blockers and DigoxinShikha Khemani88% (8)
- Basic Principles of PharmacologyDocument47 pagesBasic Principles of Pharmacologysapiah raman100% (2)
- Pharm Drug ListDocument17 pagesPharm Drug Listanon_523534678No ratings yet
- 783 Q - 650 Answered 07.04.2019Document96 pages783 Q - 650 Answered 07.04.2019Syed Ibrahim100% (1)
- Drug of Choice and First Line of TreatmentDocument2 pagesDrug of Choice and First Line of Treatmentprinz1mendezNo ratings yet
- Pharma Katzung TablesDocument16 pagesPharma Katzung TablesPrincess Arabia-ObedozaNo ratings yet
- Super Fast Mental Math - Vedic Math HistoryDocument51 pagesSuper Fast Mental Math - Vedic Math Historyvedicmath98% (41)
- Cave Rescue ActivityDocument6 pagesCave Rescue Activityshweta bambuwalaNo ratings yet
- Pharmacology NotesDocument48 pagesPharmacology NotesBheru Lal100% (1)
- Drug Receptor Types: Cut Here Cut HereDocument60 pagesDrug Receptor Types: Cut Here Cut Heredlneisha61100% (13)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- PharmacologyDocument13 pagesPharmacologyMa Carmela GuevarraNo ratings yet
- Martial Arts - Bruce Lee's Speed TrainingDocument4 pagesMartial Arts - Bruce Lee's Speed Trainingbrogan97% (33)
- SympathomimeticsDocument25 pagesSympathomimeticsMirza Shaharyar BaigNo ratings yet
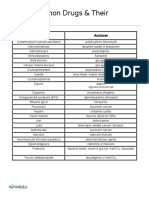
- Common Drugs and Their AntidotesDocument1 pageCommon Drugs and Their AntidoteskiranbhandarkarNo ratings yet
- Pharmacology Charts PDFDocument88 pagesPharmacology Charts PDFMohamad Samir90% (10)
- Drug Classification TableDocument6 pagesDrug Classification TableBouncesNo ratings yet
- Pharmacy MnenomicsDocument12 pagesPharmacy MnenomicsNaresh BabuNo ratings yet
- Pharm NotesDocument198 pagesPharm NotesNancy Danielz80% (5)
- Martial Arts - Bruce Lee's Training SecretsDocument3 pagesMartial Arts - Bruce Lee's Training Secretsbrogan91% (34)
- Respiratory and Cardiovascular DrugsDocument21 pagesRespiratory and Cardiovascular DrugsCandace Flowers100% (3)
- Pharmacology MnemonicsDocument19 pagesPharmacology MnemonicsAl-nazer Azer Al100% (5)
- Parasympathetic Pharmacology Drugs Muscarine and Nicotinic RecpetorsDocument56 pagesParasympathetic Pharmacology Drugs Muscarine and Nicotinic RecpetorsMatthewNo ratings yet
- MantrasDocument24 pagesMantrasg_gaurishankar@rediffmail.com100% (4)
- AntibioticsDocument2 pagesAntibioticsPGI Custodio, Ed KristianNo ratings yet
- SJDWHDJSDJSDDocument358 pagesSJDWHDJSDJSDwide mind hackerNo ratings yet
- Pharmacology OverviewDocument95 pagesPharmacology OverviewMiguel CuevasNo ratings yet
- Tally 9.2 NotesDocument1,918 pagesTally 9.2 NotesRamesh75% (4)
- Pharmacology List of DrugsDocument66 pagesPharmacology List of DrugsSohail Adnan100% (2)
- Muscarine & Nicotinic: ReceptorDocument26 pagesMuscarine & Nicotinic: ReceptorCess Lagera Ybanez88% (16)
- Pharmacology KatzDocument13 pagesPharmacology KatzFahd Abdullah Al-refaiNo ratings yet
- Pharmacology of SulphonamidesDocument21 pagesPharmacology of SulphonamidesGANESH KUMAR JELLA100% (1)
- Cytogenectics Reading ListDocument2 pagesCytogenectics Reading ListHassan GillNo ratings yet
- Classification of Drugs PDFDocument15 pagesClassification of Drugs PDFmuhammad ihtisham ul hassanNo ratings yet
- Adrenergic & Cholinergic DrugsDocument1 pageAdrenergic & Cholinergic DrugsMina Minawy100% (1)
- Pharmacology Drug ClassificationDocument4 pagesPharmacology Drug ClassificationRPh Krishna Chandra Jagrit100% (4)
- Adrenergic ReceptorsDocument9 pagesAdrenergic Receptorsrababmohsin110100% (1)
- PharmacologyDocument318 pagesPharmacologyAamir Sirohi94% (16)
- Pharmacology ReviewDocument172 pagesPharmacology ReviewJan Patrick Arrieta100% (1)
- Pharma ChartsDocument33 pagesPharma ChartsNooreen Hussain100% (1)
- Oracle Time and Labor - Data SheetDocument5 pagesOracle Time and Labor - Data Sheetbilaltanoli@gmail.comNo ratings yet
- Clinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsDocument26 pagesClinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsNadia Ancharuz100% (1)
- Pharmacology Mnemonics (Part 01) by M IhtishamDocument32 pagesPharmacology Mnemonics (Part 01) by M Ihtishammuhammad ihtisham ul hassan100% (1)
- Drug ClassificationDocument20 pagesDrug Classificationlizzeygail15No ratings yet
- Pharmacology BriefDocument287 pagesPharmacology BriefHu Mihi100% (1)
- Vijay Solvex PROJECT "Retention Strategy"Document110 pagesVijay Solvex PROJECT "Retention Strategy"Jayesh SinghNo ratings yet
- Mnemonics For Antibiotics-2Document10 pagesMnemonics For Antibiotics-2totallyfakeusernameNo ratings yet
- Rules & Guidelines of Elliott WaveDocument12 pagesRules & Guidelines of Elliott WaveNd Reyes100% (2)
- Niper Model Paper 1Document40 pagesNiper Model Paper 1GANESH KUMAR JELLANo ratings yet
- Sympathomimetic Drugs PharmacologyDocument10 pagesSympathomimetic Drugs PharmacologyHaroon JavedNo ratings yet
- Mantras - English - KundaliniDocument7 pagesMantras - English - KundaliniRPh Krishna Chandra JagritNo ratings yet
- OtcDocument10 pagesOtcJames PerianayagamNo ratings yet
- Niper Model Paper 4Document44 pagesNiper Model Paper 4RPh Krishna Chandra JagritNo ratings yet
- Vancomycin Pharmacology Indications, Mechanism, and Side Effects! PDFDocument1 pageVancomycin Pharmacology Indications, Mechanism, and Side Effects! PDFFrancis PasayNo ratings yet
- Antibiotic Summary - DraftDocument10 pagesAntibiotic Summary - DraftStrept Pneumonia100% (1)
- Antibiotics: Means Against LifeDocument13 pagesAntibiotics: Means Against Lifeshankul kumar100% (1)
- Pharmacology MCQsDocument12 pagesPharmacology MCQsSidharta ChatterjeeNo ratings yet
- Warfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureDocument6 pagesWarfarin Sodium: INR Levels 4.0 or Less Ok To Carry Out Procedure Test Atleast 72 Hrs Prior To ProcedureVimi GeorgeNo ratings yet
- Drug interaction checkerDocument1 pageDrug interaction checkermadison61404100% (3)
- Sedative-Hypnotic and Antipsychotic Drugs GuideDocument17 pagesSedative-Hypnotic and Antipsychotic Drugs GuideBijay Kumar MahatoNo ratings yet
- SAR of Macrolides, Penicillins, and Other AntibioticsDocument36 pagesSAR of Macrolides, Penicillins, and Other AntibioticsBen Paolo Cecilia RabaraNo ratings yet
- Introduction To Cns PharmacologyDocument66 pagesIntroduction To Cns PharmacologyYazan Emad Salem100% (1)
- ANS Drug ClassificationDocument11 pagesANS Drug ClassificationUrugonda Venumadhav100% (1)
- Sympathomimetic Drug - WikipediaDocument5 pagesSympathomimetic Drug - Wikipediamohammedalradai629No ratings yet
- Chapter 17 Adrenergic AgonistsDocument13 pagesChapter 17 Adrenergic AgonistsKhalil MominNo ratings yet
- L19 - Adrenergic IVDocument7 pagesL19 - Adrenergic IVyasaira707No ratings yet
- Systemic Effects of Histamine and SerotoninDocument5 pagesSystemic Effects of Histamine and SerotoninibrahimNo ratings yet
- Sympathomimetics (Catecholamines & Non Catecholamines)Document99 pagesSympathomimetics (Catecholamines & Non Catecholamines)Raheel JavaidNo ratings yet
- L17 - Adrenergics IIDocument6 pagesL17 - Adrenergics IIyasaira707No ratings yet
- Chemical Interactions and Effects on the Nervous SystemDocument6 pagesChemical Interactions and Effects on the Nervous SystemCarlo Domingo LadieroNo ratings yet
- 1 SymphatomimeticsDocument10 pages1 SymphatomimeticsJericho De GuzmanNo ratings yet
- PDFDocument33 pagesPDFIvanes IgorNo ratings yet
- Meningioma TreatmentDocument9 pagesMeningioma TreatmentRPh Krishna Chandra JagritNo ratings yet
- About MeningiomaDocument5 pagesAbout MeningiomaRPh Krishna Chandra JagritNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- Happy Birthday Nivisha... God Bless YouDocument1 pageHappy Birthday Nivisha... God Bless YouRPh Krishna Chandra JagritNo ratings yet
- RCJ CV-01 FinalDocument4 pagesRCJ CV-01 FinalRPh Krishna Chandra Jagrit100% (1)
- About This Tutorial: Version HistoryDocument328 pagesAbout This Tutorial: Version HistoryKate CorralesNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- HTML-XHTML Tag SheDocument6 pagesHTML-XHTML Tag SheabcjohnNo ratings yet
- Matrimonial Resume CVDocument3 pagesMatrimonial Resume CVRPh Krishna Chandra Jagrit76% (37)
- Web DesigningDocument638 pagesWeb DesigningRPh Krishna Chandra JagritNo ratings yet
- Secret of The UniverseDocument26 pagesSecret of The UniverseRPh Krishna Chandra JagritNo ratings yet
- Niper Model Paper 5.Document47 pagesNiper Model Paper 5.GANESH KUMAR JELLANo ratings yet
- Tab CompleteDocument75 pagesTab CompleteGANESH KUMAR JELLANo ratings yet
- TocDocument72 pagesTocRPh Krishna Chandra JagritNo ratings yet
- Niper Model Paper 6.Document37 pagesNiper Model Paper 6.GANESH KUMAR JELLANo ratings yet
- Niper Model Paper 7.Document27 pagesNiper Model Paper 7.GANESH KUMAR JELLA100% (1)
- Niper Model Paper 7.Document27 pagesNiper Model Paper 7.GANESH KUMAR JELLA100% (1)
- Niper Model Paper 3.Document46 pagesNiper Model Paper 3.GANESH KUMAR JELLANo ratings yet
- Niper Model Paper 3.Document46 pagesNiper Model Paper 3.GANESH KUMAR JELLANo ratings yet
- Year 2 - Push and Pull FPDDocument18 pagesYear 2 - Push and Pull FPDRebecca LNo ratings yet
- Ultra Slimpak G448-0002: Bridge Input Field Configurable IsolatorDocument4 pagesUltra Slimpak G448-0002: Bridge Input Field Configurable IsolatorVladimirNo ratings yet
- Learn R For Applied StatisticsDocument457 pagesLearn R For Applied StatisticsyasortyNo ratings yet
- Yayasan Pendidikan Ramadanthy Milad Anniversary SpeechDocument6 pagesYayasan Pendidikan Ramadanthy Milad Anniversary SpeechDina Meyraniza SariNo ratings yet
- 1.an Overview On Membrane Strategies For Rare Earths Extraction and Separation - 2017Document36 pages1.an Overview On Membrane Strategies For Rare Earths Extraction and Separation - 2017Vasile AlexandraNo ratings yet
- Bimbo Marketing ResearchDocument27 pagesBimbo Marketing Researcheman.konsouhNo ratings yet
- Thesis PromptsDocument7 pagesThesis Promptsauroratuckernewyork100% (2)
- Vee 2003Document14 pagesVee 2003Syed faizan Ali zaidiNo ratings yet
- Curriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: ObjectiveDocument1 pageCurriculum Vitae: Name: Bhupal Shrestha Address: Kamalamai Municipality-12, Sindhuli, Nepal. Email: Objectivebhupal shresthaNo ratings yet
- Ti 1000 0200 - enDocument2 pagesTi 1000 0200 - enJamil AhmedNo ratings yet
- Mapúa Welding Shop PracticeDocument7 pagesMapúa Welding Shop PracticeJay EmNo ratings yet
- MUM202001007 - 300 TR Price BOQ ChillerDocument4 pagesMUM202001007 - 300 TR Price BOQ ChillerB DASNo ratings yet
- Wilo Mather and Platt Pumps Pvt. LTD.: Technical DatasheetDocument2 pagesWilo Mather and Platt Pumps Pvt. LTD.: Technical DatasheetTrung Trần MinhNo ratings yet
- trac-nghiem-ngu-am-am-vi-hoc-tieng-anh-đã chuyển đổiDocument18 pagestrac-nghiem-ngu-am-am-vi-hoc-tieng-anh-đã chuyển đổiNguyễn ThiênNo ratings yet
- KOREADocument124 pagesKOREAchilla himmudNo ratings yet
- French Ox Cheek Stew with MushroomsDocument2 pagesFrench Ox Cheek Stew with MushroomsMihai LeancăNo ratings yet
- Case Study On Global Branding - DuluxDocument18 pagesCase Study On Global Branding - DuluxAakriti NegiNo ratings yet
- Fci FC CotsDocument25 pagesFci FC CotsMatthew DuNo ratings yet
- Working Capital Management (2015)Document62 pagesWorking Capital Management (2015)AJNo ratings yet
- Booklet English 2016Document17 pagesBooklet English 2016Noranita ZakariaNo ratings yet
- SPH3U Formula SheetDocument2 pagesSPH3U Formula SheetJSNo ratings yet
- RRLDocument4 pagesRRLTiltshifter ViNo ratings yet
- Nec TutorialDocument5 pagesNec TutorialbheemasenaNo ratings yet
- E TN SWD Csa A23 3 94 001 PDFDocument9 pagesE TN SWD Csa A23 3 94 001 PDFRazvan RobertNo ratings yet
- Modul English For Study SkillsDocument9 pagesModul English For Study SkillsRazan Nuhad Dzulfaqor razannuhad.2020No ratings yet