Professional Documents
Culture Documents
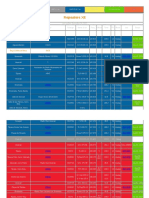
Hepatitis A, B, C
Uploaded by
Rafael CataluñaOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hepatitis A, B, C
Uploaded by
Rafael CataluñaCopyright:
Available Formats
Hepatitis A
Hepatitis A (formerly known as infectious hepatitis) is an acute infectious disease of the liver caused by the hepatitis A virus (HAV),[1] which is most commonly transmitted by the fecal-oral route via contaminated food or drinking water. Every year, approximately 10 million people worldwide are infected with the virus.[2] The time between infection and the appearance of the symptoms, (the incubation period), is between two and six weeks and the average incubation period is 28 days.[3] In developing countries, and in regions with poor hygiene standards, the incidence of infection with this virus is high[4] and the illness is usually contracted in early childhood. HAV has also been found in samples taken to study ocean water quality.[5] Hepatitis A infection causes no clinical signs and symptoms in over 90% of infected children and since the infection confers lifelong immunity, the disease is of no special significance to the indigenous population. In Europe, the United States and other industrialized countries, on the other hand, the infection is contracted primarily by susceptible young adults, most of whom are infected with the virus during trips to countries with a high incidence of the disease.[3] Hepatitis A does not have a chronic stage, is not progressive, and does not cause permanent liver damage. Following infection, the immune system makes antibodies against HAV that confer immunity against future infection. The disease can be prevented by vaccination, and hepatitis A vaccine has been proven effective in controlling outbreaks worldwide.[3] Signs and symptoms Early symptoms of hepatitis A infection can be mistaken for influenza, but some sufferers, especially children, exhibit no symptoms at all. Symptoms typically appear 2 to 6 weeks, (the incubation period), after the initial infection.[6] Symptoms can return over the following 69 months and include:[7] * Fatigue* Fever* Abdominal pain * Nausea * Diarrhea * Appetite loss* Depression* Jaundice, a yellowing of the skin or whites of the eyes* Sharp pains in the right-upper quadrant of the abdomen* Weight loss* Itching* Bile is removed from blood stream and excreted in urine giving a dark amber colour* Feces tend to be light in colour due to lack of bilirubin in bile* Strong aversion to cigarette smoking Prevention For information about the vaccine, its properties, and its application, see Hepatitis A vaccine. Hepatitis A can be prevented by vaccination, good hygiene and sanitation.[1][12] Hepatitis A is also one of the main reasons not to surf or go in the ocean after rains in coastal areas that are known to have bad runoff.[5] The vaccine protects against HAV in more than 95% of cases for 10 years. It contains inactivated Hepatitis A virus providing active immunity against a future infection.[13][14] The vaccine was first phased in 1996 for children in high-risk areas, and in 1999 it was spread to areas with elevating levels of infection.[15]
The vaccine is given by injection into the muscle of the upper arm. An initial dose provides protection two to four weeks after vaccination; the second booster dose, given six to twelve months later, provides protection for up to twenty years.[13][15] Treatment There is no specific treatment for hepatitis A. Sufferers are advised to rest, avoid fatty foods and alcohol (these may be poorly tolerated for some additional months during the recovery phase and cause minor relapses), eat a well-balanced diet, and stay hydrated. Approximately 610% of people diagnosed with hepatitis A may experience one or more symptomatic relapse(s) for up to 40 weeks after contracting this disease.[16]
Hepatitis B
Hepatitis B is an infectious illness caused by hepatitis B virus (HBV) which infects the liver of hominoidae, including humans, and causes an inflammation called hepatitis. Originally known as "serum hepatitis",[1] the disease has caused epidemics in parts of Asia and Africa, and it is endemic in China.[2] About a third of the world's population, more than 2 billion people, have been infected with the hepatitis B virus.[3] This includes 350 million chronic carriers of the virus.[4] Transmission of hepatitis B virus results from exposure to infectious blood or body fluids containing blood. The acute illness causes liver inflammation, vomiting, jaundice andrarelydeath. Chronic hepatitis B may eventually cause liver cirrhosis and liver cancera fatal disease with very poor response to current chemotherapy.[5] The infection is preventable by vaccination.[6] Hepatitis B virus is an hepadnavirushepa from hepatotrophic and dna because it is a DNA virus[7]and it has a circular genome composed of partially double-stranded DNA. The viruses replicate through an RNA intermediate form by reverse transcription, and in this respect they are similar to retroviruses.[8] Although replication takes place in the liver, the virus spreads to the blood where virus-specific proteins and their corresponding antibodies are found in infected people. Blood tests for these proteins and antibodies are used to diagnose the infection.[9] Signs and symptoms Acute infection with hepatitis B virus is associated with acute viral hepatitis an illness that begins with general ill-health, loss of appetite, nausea, vomiting, body aches, mild fever, dark urine, and then progresses to development of jaundice. It has been noted that itchy skin has been an indication as a possible symptom of all hepatitis virus types. The illness lasts for a few weeks and then gradually improves in most affected people. A few patients may have more severe liver disease (fulminant hepatic failure), and may die as a result of it. The infection may be entirely asymptomatic and may go unrecognized.[citation needed] Chronic infection with hepatitis B virus may be either asymptomatic or may be associated with a chronic inflammation of the liver (chronic hepatitis), leading to cirrhosis over a period of several years. This type of infection dramatically increases the incidence of hepatocellular carcinoma (liver cancer). Chronic carriers are encouraged to avoid consuming alcohol as it increases their risk for cirrhosis and liver cancer. Hepatitis B virus has been linked to the development of Membranous glomerulonephritis (MGN).[20]
Prevention Several vaccines have been developed for the prevention of hepatitis B virus infection. These rely on the use of one of the viral envelope proteins (hepatitis B surface antigen or HBsAg). The vaccine was originally prepared from plasma obtained from patients who had long-standing hepatitis B virus infection. However, currently, it is made using a synthetic recombinant DNA technology that does not contain blood products. You cannot catch hepatitis B from this vaccine.[31] Following vaccination, hepatitis B surface antigen may be detected in serum for several days; this is known as vaccine antigenaemia.[32] The vaccine is administered in either two-, three-, or four-dose schedules into infants and adults, which provides protection for 8590% of individuals.[33] Protection has been observed to last 12 years in individuals who show adequate initial response to the primary course of vaccinations, and that immunity is predicted to last at least 25 years.[34] Unlike hepatitis A, hepatitis B does not generally spread through water and food. Instead, it is transmitted through body fluids; prevention is thus the avoidance of such transmission: unprotected sexual contact, blood transfusions, re-use of contaminated needles and syringes, and vertical transmission during child birth. Infants may be vaccinated at birth.[35] Multiple injections of small doses of hepatitis B immune globulin (HBIg, 200-400 IU per month), or lamivudine (100mg per day) in HBV carrier mothers with a high degree of infectiousness (>106 copies/ml) in late pregnancy (the last three months of pregnancy), effectively and safely prevent HBV intrauterine transmission.[36][37][38] Treatment Acute hepatitis B infection does not usually require treatment because most adults clear the infection spontaneously.[39] Early antiviral treatment may only be required in fewer than 1% of patients, whose infection takes a very aggressive course (fulminant hepatitis) or who are immunocompromised. On the other hand, treatment of chronic infection may be necessary to reduce the risk of cirrhosis and liver cancer. Chronically infected individuals with persistently elevated serum alanine aminotransferase, a marker of liver damage, and HBV DNA levels are candidates for therapy.[40] Although none of the available drugs can clear the infection, they can stop the virus from replicating, thus minimizing liver damage. Currently, there are seven medications licensed for treatment of hepatitis B infection in the United States. These include antiviral drugs lamivudine (Epivir), adefovir (Hepsera), tenofovir (Viread), telbivudine (Tyzeka) and entecavir (Baraclude) and the two immune system modulators interferon alpha-2a and PEGylated interferon alpha-2a (Pegasys). The use of interferon, which requires injections daily or thrice weekly, has been supplanted by long-acting PEGylated interferon, which is injected only once weekly.[41] However, some individuals are much more likely to respond than others and this might be because of the genotype of the infecting virus or the patient's heredity. The treatment reduces viral replication in the liver, thereby reducing the viral load (the amount of virus particles as measured in the blood).[42] Infants born to mothers known to carry hepatitis B can be treated with antibodies to the hepatitis B virus (HBIg). When given with the vaccine within twelve hours of birth, the risk of
acquiring hepatitis B is reduced 90%.[43] This treatment allows a mother to safely breastfeed her child. In July 2005, researchers from A*STAR and the National University of Singapore identified an association between a DNA-binding protein belonging to the class of protein heterogeneous nuclear ribonucleoprotein K (hnRNP K) and HBV replication in patients. Controlling the level of hnRNP K may act as a possible treatment for HBV.[44] Response to treatment differs between the genotypes. Interferon treatment may produce an e antigen seroconversion rate of 37% in genotype A but only a 6% seroconversion in type D. Genotype B has similar seroconversion rates to type A while type C seroconvets only in 15% of cases. Sustained e antigen loss after treatment is ~45% in types A and B but only 25-30% in types C and D.
Hepatitis C
Hepatitis C is an infectious disease affecting the liver, caused by the hepatitis C virus (HCV).[1] The infection is often asymptomatic, but once established, chronic infection can progress to scarring of the liver (fibrosis), and advanced scarring (cirrhosis) which is generally apparent after many years. In some cases, those with cirrhosis will go on to develop liver failure or other complications of cirrhosis, including liver cancer[1] or life threatening esophageal varices and gastric varices. The hepatitis C virus (HCV) is spread by blood-to-blood contact. Most people have few, if any symptoms after the initial infection, yet the virus persists in the liver in about 85% of those infected. Persistent infection can be treated with medication, peginterferon and ribavirin being the standard-of-care therapy. 51% are cured overall. Those who develop cirrhosis or liver cancer may require a liver transplant, and the virus universally recurs after transplantation. An estimated 270-300 million people worldwide are infected with hepatitis C. Hepatitis C is a strictly human disease. It cannot be contracted from or given to any other animal. Chimpanzees can be infected with the virus in the laboratory, but do not develop the disease, which has made research more difficult. No vaccine against hepatitis C is available. The existence of hepatitis C (originally "non-A non-B hepatitis") was postulated in the 1970s and proved conclusively in 1989. It is one of five known hepatitis viruses: A, B, C, D, and E.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Arup Blockchain Technology ReportDocument74 pagesArup Blockchain Technology ReportHarin VesuwalaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Le Nu Spa Employee HandbookDocument34 pagesLe Nu Spa Employee Handbookhamzeh abo hammourNo ratings yet
- Economics of Money Banking and Financial Markets 12th Edition Mishkin Solutions ManualDocument3 pagesEconomics of Money Banking and Financial Markets 12th Edition Mishkin Solutions Manualalexanderyanggftesimjac100% (15)
- Schneider Electric Strategy PresentationDocument10 pagesSchneider Electric Strategy PresentationDeepie KaurNo ratings yet
- Best Practices in Implementing A Secure Microservices ArchitectureDocument85 pagesBest Practices in Implementing A Secure Microservices Architecturewenapo100% (1)
- Geometry First 9 Weeks Test Review 1 2011Document6 pagesGeometry First 9 Weeks Test Review 1 2011esvraka1No ratings yet
- Literature Circles Secondary SolutionsDocument2 pagesLiterature Circles Secondary Solutionsapi-235368198No ratings yet
- Urbanization As A Transformative Force: Quick FactsDocument20 pagesUrbanization As A Transformative Force: Quick FactsJulio CovarrubiasNo ratings yet
- The Son of Man Rides The Clouds Pt. 2b - Answering Islam BlogDocument5 pagesThe Son of Man Rides The Clouds Pt. 2b - Answering Islam BlogbenciusilviuNo ratings yet
- FINAL Conflicts 2019 Official Guidelines PDFDocument48 pagesFINAL Conflicts 2019 Official Guidelines PDFxsar_xNo ratings yet
- Commissioning Procedure for JTB-PEPCDocument17 pagesCommissioning Procedure for JTB-PEPCelif maghfirohNo ratings yet
- NUC BIOS Update Readme PDFDocument3 pagesNUC BIOS Update Readme PDFSuny Zany Anzha MayaNo ratings yet
- Laporan Keuangan Tahun 2018Document264 pagesLaporan Keuangan Tahun 2018Weni PatandukNo ratings yet
- Week 10 8th Grade Colonial America The Southern Colonies Unit 2Document4 pagesWeek 10 8th Grade Colonial America The Southern Colonies Unit 2santi marcucciNo ratings yet
- Facebook Privacy FTC Complaint Docket No. C-4365Document19 pagesFacebook Privacy FTC Complaint Docket No. C-4365David SangerNo ratings yet
- Jeff Roth CVDocument3 pagesJeff Roth CVJoseph MooreNo ratings yet
- Activity 1: 2. Does His Homework - He S 3 Late ForDocument10 pagesActivity 1: 2. Does His Homework - He S 3 Late ForINTELIGENCIA EDUCATIVANo ratings yet
- Tahap Kesediaan Pensyarah Terhadap Penggunaan M-Pembelajaran Dalam Sistem Pendidikan Dan Latihan Teknik Dan Vokasional (TVET)Document17 pagesTahap Kesediaan Pensyarah Terhadap Penggunaan M-Pembelajaran Dalam Sistem Pendidikan Dan Latihan Teknik Dan Vokasional (TVET)Khairul Yop AzreenNo ratings yet
- Gautam KDocument12 pagesGautam Kgautam kayapakNo ratings yet
- Inmarsat M2M Terminal ComparisonDocument2 pagesInmarsat M2M Terminal Comparisonmaruka33No ratings yet
- Symbiosis Law School ICE QuestionsDocument2 pagesSymbiosis Law School ICE QuestionsRidhima PurwarNo ratings yet
- Remotely Operated Underwater Vehicle With 6DOF Robotic ArmDocument14 pagesRemotely Operated Underwater Vehicle With 6DOF Robotic ArmMethun RajNo ratings yet
- Sach Bai Tap Tieng Anh8 - Mai Lan HuongDocument157 pagesSach Bai Tap Tieng Anh8 - Mai Lan Huongvothithao19750% (1)
- Kristy Gallazin Edte 431 - Assignment 2 Newsletter pdf12Document4 pagesKristy Gallazin Edte 431 - Assignment 2 Newsletter pdf12api-301047467No ratings yet
- PERTANYAAN INTERVIEW WinaDocument2 pagesPERTANYAAN INTERVIEW WinaDidi SetiadiNo ratings yet
- Repeaters XE PDFDocument12 pagesRepeaters XE PDFenzzo molinariNo ratings yet
- MICROHARDNESS TESTER HMV-2 - SeriesDocument9 pagesMICROHARDNESS TESTER HMV-2 - SeriesRicoNo ratings yet
- List of Indian Timber TreesDocument5 pagesList of Indian Timber TreesE.n. ElangoNo ratings yet
- FAQs MHA RecruitmentDocument6 pagesFAQs MHA RecruitmentRohit AgrawalNo ratings yet
- Product Data: Real-Time Frequency Analyzer - Type 2143 Dual Channel Real-Time Frequency Analyzers - Types 2144, 2148/7667Document12 pagesProduct Data: Real-Time Frequency Analyzer - Type 2143 Dual Channel Real-Time Frequency Analyzers - Types 2144, 2148/7667jhon vargasNo ratings yet