Professional Documents
Culture Documents
US Vascular Central Perif - Érico Brasil
Uploaded by
Patricio GutierrezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
US Vascular Central Perif - Érico Brasil
Uploaded by
Patricio GutierrezCopyright:
Available Formats
190
RevIew ARTICle
Uri Adrian Prync Flato1, Gustavo Mascari Petisco2, Fernanda Bezerra dos Santos3
Ultrasound-guided venous cannulation in a critical care unit
Puno venosa guiada por ultra-som em unidade de terapia intensiva
1. Physician at the Intensive Care Unit of the Centro de Referncia da Sade da Mulher - So Paulo (SP), Brazil. 2. Physician at the Intensive Care Unit of the Centro de Referncia da Sade da Mulher - So Paulo (SP), Brazil. 3. Physician at the Intensive Care Unit of the Centro de Referncia da Sade da Mulher - So Paulo (SP), Brazil.
ABSTRACT Use of ultrasound introduced as part of intensive care therapy makes viable bedside invasive procedures and diagnosis. Due to portability, combined with team training, its use guarantees less complications related to insertion, as well as patients safety. It also reduces severe conditions re-
lated to the catheter, such as pneumothorax among others. Probably, in a near future, as purchase of ultrasound equipment becomes easier and team training more adequate, this tool will become essential in daily clinical practice. Keywords: Ultrasonography; Echocardiography; Intensive care
INTRODUCTION In the intensive care setting, ultrasound guided venous cannulation has now become an essential procedure for critically ill patients, however it has risks inherent to its insertion as well as permanence. To reduce risks related to insertion, the applicability of ultrasonography to aid insertion of a central and peripheral venous catheter will be discussed. This is a technology available in our daily clinical practice with some advantages in intensive care units, such as absence of exposure of patients to radioactivity, reproducibility, low cost, practicality and portability. Further, the method is not invasive and provides important bedside information, as well as support in invasive procedures. (1-4) Initially, its use was restricted to medical radiologists and echocardiographers. However, universalization of the method and standardizing of training by some societies such as the American College of Emergency Physicians (ACEP), (5) European Federation of Societies for Ultrasound in Medidicine and Biology (6) and World Interactive Network Focused on Critical Ultrasound (WINFOCUS, (7) furthered implementation in the developed countries while it is still incipient in developing countries such as Brazil. In the last decade, applicability of this method was not merely restricted to the intensive care setting, but also to the pre-hospital emergency system, intra-operative and during cardiac arrest (CA). (8-10) Another interesting point is the growing number of publications related to the method in indexed journals, stressing its importance as a complementary tool for care of the critically ill. (11)
Received from the Intensie Care Unit of the Centro de Referncia da Sade da Mulher So Paulo (SP), Brazil. Submitted on November 27, 2008 Accepted on May 16, 2009 Author for correspondence: Uri Adrian Prync Flato Gerncia Hospitalar - Centro de Referncia da Sade da Mulher Avenida Brigadeiro Lus Antnio, 683 CEP: 01317-000 - So Paulo (SP), Brazil. Phone/Fax: (11) 5081-4531 Email: uriflato@gmail.com
Rev Bras Ter Intensiva. 2009; 21(2):190-196
Ultrasound-guided venous cannulation in a critical care unit
191
BASIC pRINCIpleS Of UlTRASOUND Sound waves are mechanical vibrations that induce alternate refractions and compressions in any physical medium they cross. Sound waves are defined by their amplitude and frequencies. The classical image of general ultrasound or echography relies on echoes and is based upon the principles of reflection, refraction and dispersion of energy of ultrasound waves. The ultrasound equipment (US) generates an electronic wave and the piezoelectric transducers transform the electric wave into a mechanical wave. US is used in frequencies between 01 MHz and 50MHz. Attenuation of the echographic wave depends on the frequency of repetition of the wave peaks and valleys. Frequency of insonation also controls axial resolution of the echographic image. The greater the frequency the smaller the distance between peaks and valleys of the wave, which is called wave length that establishes the image axial resolution. Axial direction is based upon a model of lines to display tissue isonation. Depth of US wave penetration in the body is directly related to wave length - a short length wave has a lesser penetration into tissues when compared to longer waves. A linear transducer creates parallel beams that penetrate into the tissue perpendicular to the skin, which is why they are preferred for structures such as veins and arteries. The sectorial transducer creates divergent beams, creating an angular sector, that is why linear trasducers present greater axial resolution. UlTRASOUND gUIDeD veNOUS CANNUlATION Today, in the USA more than 5 million central venous catheters are introduced, associated with a complication rate of about 15%.(12) Main complications are arterial puncture, pneumothorax, hematoma and to a large degree , failure in catheter insertion of up to 35%. A series of factors are related to this percentage, among them operator experience and the patients anatomical aspects (morbid obesity, coagulopathy, urgency of the procedure, etc.) Noteworthy about anatomy and position of the internal jugular vein in relation to the carotid artery, discloses that 50% of the times it (jugular vein) is positioned anterior to the carotid artery.(13-17) With use of US its location can be assessed, as well as the diameter and adverse conditions such as venous thrombosis, facilitating insertion and or choice of puncture site (Figures 1 and 2).
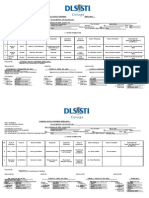
Jugular vein
Position Medial Anterior Anterolateral Carotid artery More lateral Lateral Posterior Not visualized or thrombotic Percentage % 0-5.5 0-16(54%)* 9-92 0-4 0-84 0-9 0-18
figure 1 A - Anatomical variation of the jugular vein(13-16); (*) 54% are located anterior to the carotid artery; B - Ultrasound image site of the internal jugular vein.
Based on two meta analyses,(18-19) the American Agency for Healthcare Research and Quality) published in 2001 a recommendation for use US guided cannulation. It is one of the 10 main practices of safety ands improves patients care.(20) US guided venous cannulation prevents one puncture accident for every seven central accesses (number needed to treat (NNT=7) and prevents one case of failure in the insertion for every five trials (NNT= 5). Similar to recommendations of the North American agency, the British National Institute for Clinical Excellence included in 2004, these recommendations in its guidelines.(21) Another factor related with this procedure would be the cost/ effectiveness analysis of implementing training of a team and acquisition of the equipment, Reviewing literature, we found the work of Calvert and Hind,(22) who by an analytical model of cost/effectiveness for each thousand catheters inserted, saved 2 thousand sterling pounds, when compared to usual insertion. Development of new equipment and cost reduction in a near future will foster utilization of US as a routine practice in the intensive care setting. To aid cannulation the probe must preferably be the straight linear (Vascular probe 5-10 MHz), as they have
Rev Bras Ter Intensiva. 2009; 21(2):190-196
192
Flato UAP, Petisco GM, Santos FB
figure 3 Types of probes, respectively: microconvex (2.5 MHz), linear (5-10MHz), convex (3.5-5.0MHz), transvaginal.
figure 2 A - Cross sectional incidence with color doppler (short axis); B - longitudinal incidence with color doppler (long axis).
high resolution and good penetration in tissue. However, as described in literature any type of probe may be used including the transvaginal (Figures 3 and 4).(23-25) Differences between probes are based upon positioning of the quartz crystals and emission of US waves at different frequencies (Hertz) and distance between them. The higher the probes frequency, the greater the resolution, however lesser the depth. The lower the frequency, the greater the depth, the lesser the resolution. The possibility to change frequency and distance of the waves in the same equipment must be highlighted. Insertion through the US may be guided by two wave modes: the B mode (Bright) or through the Doppler mode, transformation of US waves reflected from a moving object, for instance, blood into an audio or color signal. Due to lack of availability of US with Doppler mode in all equipment, a longer learning curve and a
figure 4 A - longitudinal incidence (experimental puncture model) using linear probe (vascular); B - micro-convex probe (sectorial echocardiograph.
Rev Bras Ter Intensiva. 2009; 21(2):190-196
Ultrasound-guided venous cannulation in a critical care unit
193
longer time of insertion, our review is restricted to the two-dimensional mode. The technique must follow the same steps of conventional cannulation of the central venous access: operator and patient asepsis and antisepsis, placement of sterile drapes, use of sterile devices protecting the probe (sterile glove or specific device for probe, placement of sterile gel between interface of the probe of patient body surface, between probe and sterile device to ease wave propagation and reduce artifacts). The technique may be carried out with two operators, that is to say, one positioning the probe and the other doing the puncture or one operator performing the entire procedure. The static puncture technique,(26) that is to say, the anatomical assessment of the vein in which the catheter will be inserted and outline of the puncture point are carried out. Once the puncture point is outlined, puncture is performed. Another way to perform puncture is the dynamic technique, as it permits real time visualization of the catheter with immediate assessment of complications. In both techniques, orientation of the probe in relation to the anatomic structures may be with a cross-sectional axis (short axis) (Figure 4) or longitudinal axis (long axis) (Figure 5A). The differentiation of the anatomical structures in this case, the visualization of the jugular vein and carotid artery are made through compression movements, using the probe (compressibility sign of the venous system) (Figure 5B). Differentiation between both structures must not rely only on pulsatility, because not everything that pulsates is an artery. Other form to differentiate these vessels is compression of the liver (hepatojugular reflux) and by observing engorgement of the venous system. This method (US) permits to assess thrombosis of the potential puncture segments, thereby avoiding complications. Some bedside maneuvers facilitate puncture: Trendelemburg position, Valsalva maneuver (increase of intrathoracic pressure), among others. The vein must be positioned in the center of the monitor and needle insertion at a 45 degrees angle in relation to the probe and equidistant from this with the vein must be carried out, similar to the Pythagorean Theorem (Figure 6). Once skin is overcome in the cross-sectional direction with the needle, it must progress towards the anterior wall of the vein, with its movement as a reference. Nonvisualization of the needle or non-visualization of the movement of structures on the monitor, probably points to non-alignment of the probe in relation to needle insertion. In this case, the needle should be pulled back and a
figure 5 A - Cross sectional axis (short axis) showing the right carotid artery in yellow and the internal jugular vein in green; B - Signs of collapse of the internal jugular vein upon performance of probe compression (compressibility sign).
new angulation and insertion must be made. After assuring that the needle is inside the vein, by blood aspiration with the plunger, the later is withdrawn and the line is introduced by the usual technique (Seldinger). Advantage of the cross- sectional axis (short axis) technique is lesser time of the learning curve and possibility to visualize smaller veins. Nevertheless, ACEP(5) recommends the longitudinal axis due to better visualization of the guide-line (Figure 7), when maybe, there is a lesser a perforation of the veins posterior wall. Some equipment, currently make both axes simultaneously available. After central venous cannulation and its due securing, control X-rays of the chest are carried out also a complementary lung ultrasound to discard pneumothorax.(27-28)
Rev Bras Ter Intensiva. 2009; 21(2):190-196
194
Flato UAP, Petisco GM, Santos FB
Needle Probe Probe
Needle
Jugular vein Carotid artery
Jugular vein
figure 6 A - Needle positioning and insertion, cross-sectional axis; B - longitudinal axis.
figure 7 guide-line insertion longitudinal axis.
The internal jugular vein is the preferred access way for ultrasound-guided venous cannulation, however the subclavian vein has some peculiarities. Visualization of the subclavian vein by infraclavicular projection is made difficult by the clavicular acoustic shadow, thereby the dynam-
ic puncture technique is unviable. The static technique should be used, outlining the puncture site. An alternative would be puncture by the supraclavicular pathway at the emergence of the subclavian vein with the jugular vein. However, it is not often used today, due to needle orientation towards the pleura and elevated chances of puncture accidents. An approach described in literature is puncture of the axillary vein as alternative to the subclavian vein, since it is easily visualized with US, more laterally located, associated with a longer distance between the probe and clavicula make dynamic insertion easier, with lower complication rates than the traditional method.(29-31) Peripheral veins should be used as first option in an emergency setting, however, some clinical situations, for instance, edematous patient, obesity, among others, make the insertion difficult. US, preferentially the linear ones (high resolution and discernment of structures with less than 1mm) make possible catheterization, using cross- sectional or longitudinal axes of basilica, cephalic and or axillary veins. Care must be given to the pressure applied on the probe to avoid collapse of the structure to be visualized (Figure 8).
Baslica vein
Brachial artery
figure 8 A - performance of the procedure by the nursing team; B - Anatomic location cross sectional axis; C - Compressibility maneuver of the venous system; D - portrait of the venous system.
Rev Bras Ter Intensiva. 2009; 21(2):190-196
Ultrasound-guided venous cannulation in a critical care unit
195
CONClUSION Utilization of ultrasound warrants precise visualization of the target, direct visualization of the needle and guide-lines progression, reduces puncture attempts, improves success rates of insertion, minimizes catheter related complications and reduces insertion time, mainly in patients with a difficult vascular access. Therefore, the disadvantages of equipment cost, team training time and interpersonal barriers represent obstacles to be overcome in view of the methods benefits.
ReSUMO A utilizao da ultrassonografia inserida no contexto de terapia intensiva possibilita a realizao de procedimentos invasivos e diagnsticos beira-leito. Atravs da portabilidade dos equipamentos atuais, associado ao treinamento da equipe, sua implementao assegura diminuio das complicaes relacionada insero assim como segurana aos pacientes. Sua implementao reduz complicaes graves relacionada ao cateter, como pneumotrax e leso vascular, entre outras. Provavelmente, em um futuro prximo, com a facilitao de aquisio de equipamentos de ultra-som e treinamento adequado da equipe, esta ferramenta se tornar indispensvel na prtica clinica diria. Descritores: Ultra-sonografia; Ecocardiografia; Cuidados intensivos
RefeReNCeS
1. Lichtenstein DA. General ultrasound in the critically ill. Berlin: Springer-Verlag; 2004. 2. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part 2. Chest. 2005;128(3):1766-81. 3. Beagle GL. Bedside diagnostic ultrasound and therapeutic ultrasound-guided procedures in the intensive care setting. Crit Care Clin. 2000;16(1):59-81. 4. Price S, Nicol E, Gibson DG, Evans TW. Echocardiography in the critically ill: current and potential roles. Intensive Care Med. 2006;32(1):48-59. Comment in: Intensive Care Med. 2006;32(8):1283. Intensive Care Med. 2006;32(1):9-10. 5. American College of Emergency Physicians. American College of Emergency Physicians. ACEP emergency ultrasound guidelines - 2001. Ann Emerg Med. 2001;38(4):470-81. 6. European Federation of Societies for Ultrasound in Medicine and Biology. Minimum training requirements for the practice of medical ultrasound. Eur J Ultrasound. 2006;27(1):79 105. 7. World Interactive Network Focused on Critical Ultrasound. (WINFOCUS). Ultrasound in critical care medicine - Continuing medical education. [cited 2008 Jan 1]. Available from: http://www.winfocus.org/usccm . 8. Vignon P, Goarin JP, editors. Echocardiographie doppler en ranimation, anesthsie et mdecine durgence. Paris: Elsevier; 2002 9. 9. Sloth E. Echocardiography in the ICU. Intensive Care Med. 2006;32(8):1283. Comment on: Intensive Care Med. 2006;32(1):48-59. Intensive Care Med. 2006;32(1):9-10. 10. Denault AY, Couture P McKenty S, Boudreault D, Plante F, , Perron R, et al. Perioperative use of transesophageal echocardiography by anesthesiologists: impact in noncardiac surgery and in the intensive care unit. Can J Anaesth. 2002;49(3):287-93. 11. Vieillard-Baron A, Slama M, Cholley B, Janvier G, Vignon P. Echocardiography in the intensive care unit: from evolution 12. 13.
14.
15.
16.
17. 18.
19.
20. 21.
to revolution? Intensive Care Med. 2008;34(2):243-9. Comment in: Intensive Care Med. 2008;34(2):215-7. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003;348(12):112333. Review. Gordon AC, Saliken JC, Johns D, Owen R, Gray RR. US-guided puncture of the internal jugular vein: complications and anatomic considerations. J Vasc Interv Radiol. 1998;9(2):3338. Comment in: J Vasc Interv Radiol. 1998;9(5):854-5. Turba UC, Uflacker R, Hannegan C, Selby JB. Anatomic relationship of the internal jugular vein and the common carotid artery applied to percutaneous transjugular procedures. Cardiovasc Intervent Radiol. 2005;28(3):303-6. Caridi JG, Hawkins IF Jr, Wiechmann BN, Pevarski DJ, Tonkin JC. Sonographic guidance when using the right internal jugular vein for central vein access. AJR Am J Roentgenol. 1998;171(5):1259-63. Troianos CA, Kuwik RJ, Pasqual JR, Lim AJ, Odasso DP. Internal jugular vein and carotid artery anatomic relation as determined by ultrasonography. Anesthesiology. 1996;85(1):438. Comment in: Anesthesiology. 1996;85(6):1501. Anesthesiology. 1996;85(6):1502-3. Legler D, Nugent M. Doppler localization of the internal jugular vein facilitates central venous cannulation. Anesthesiology. 1984;60(5):481-2. Randolph AG, Cook DJ, Gonzales CA, Pribble CG. Ultrasound guidance for placement of central venous catheters: a meta-analysis of the literature. Crit Care Med. 1996;24(12):20538. Comment in: ACP J Club. 1997;126(3):75. Hind D, Calvert N, McWilliams R, Davidson A, Paisley S, Beverley C, Thomas S. Ultrasonic locating devices for central venous cannulation: meta-analysis. BMJ. 2003;327(7411):361. Making health care safer: a critical analysis of patient safety practices [Internet]. 200. [cited 2008 June 12]. Available from: http\\www.ahrq.gov\clinic\ptsafety\ . Howard S. A survey measuring the impact of NICE guidance
Rev Bras Ter Intensiva. 2009; 21(2):190-196
196
Flato UAP, Petisco GM, Santos FB
22.
23. 24.
25. 26.
49: the use of ultrasound locating devices for placing central venous catheters [Internet]. 2004. [cited 2008 June 12]. Available from: http://www.nice.org.uk/pdf/final_CVC_placement_survey_report.pdf. Calvert N, Hind D, McWilliams RG, Thomas SM, Beverley C, Davidson A. The effectiveness and cost-effectiveness of ultrasound locating devices for central venous access: a systematic review and economic evaluation. Health Technol Assess. 2003;7(12):1-84. Phelan MP. A novel use of the endocavity (transvaginal) ultrasound probe: central venous access in the ED. Am J Emerg Med. 2003;21(3):220-2. Milling TJ Jr, Rose J, Briggs WM, Birkhahn R, Gaeta TJ, Bove JJ, Melniker LA. Randomized, controlled clinical trial of pointof-care limited ultrasonography assistance of central venous cannulation: the Third Sonography Outcomes Assessment Program (SOAP-3) Trial. Crit Care Med. 2005;33(8):17649. Comment in: Crit Care Med. 2005;33(8):1875-7. Untracht SH. Progress in central venous access. Crit Care Med. 1996; 24(1):183-4. Denys BG, Uretsky BF, Reddy PS. Ultrasound-assisted can-
27.
28. 29.
30. 31.
nulation of the internal jugular vein. A prospective comparison to the external landmark-guided technique. Circulation. 1993; 87(5):1557-62. Maury E, Guglielminotti J, Alzieu M, Guidet B, Offenstadt G. Ultrasonic examination: an alternative to chest radiography after central venous catheter insertion? Am J Respir Crit Care Med. 2001;164(3):403-5. Lichtenstein D, Mezire G, Biderman P, Gepner A. The lung point: an ultrasound sign specific to pneumothorax. Intensive Care Med. 2000;26(10):1434-40. Sharma A, Bodenham AR, Mallick A. Ultrasound-guided infraclavicular axillary vein cannulation for central venous access. Br J Anaesth. 2004; 93(2):188-92. Erratum in: Br J Anaesth. 2004;93(5):752. Comment in: Br J Anaesth. 2004;93(2):175-7. Sandhu NS. Transpectoral ultrasound-guided catheterization of the axillary vein: an alternative to standard catheterization of the subclavian vein. Anesth Analg. 2004;99(1):183-7. Use of ultrasound imaging by emergency physicians. American Colllege of Emergency Physicians. Ann Emerg Med. 1997;30(3):364-5.
Rev Bras Ter Intensiva. 2009; 21(2):190-196
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Synactive Theory of Newborn Behavioral Organization and Development - WikipediaDocument14 pagesSynactive Theory of Newborn Behavioral Organization and Development - WikipediaYuseva SariatiNo ratings yet
- CsDocument7 pagesCsakosiMJcutie100% (1)
- Hydatidiform MoleDocument2 pagesHydatidiform MolePaola AgustinNo ratings yet
- Indications and Contraindications of Laparoscopy1Document18 pagesIndications and Contraindications of Laparoscopy1drhiwaomer100% (2)
- Desquamative GingivitisDocument17 pagesDesquamative GingivitisPuspandaru Nur Iman FadlilNo ratings yet
- Curriculum Vitae2011Document2 pagesCurriculum Vitae2011Rafik MargaryanNo ratings yet
- Sliwa Et Al-2010-European Journal of Heart FailureDocument12 pagesSliwa Et Al-2010-European Journal of Heart FailurealfredoibcNo ratings yet
- MRI Safety August 2009 V6Document11 pagesMRI Safety August 2009 V6Paulo Henrique Vizoná de OliveiraNo ratings yet
- American College of Women's Health PhysiciansDocument16 pagesAmerican College of Women's Health PhysiciansSex & Gender Women's Health CollaborativeNo ratings yet
- Women's Expectations From Delivery Nurses of Vaginal Birth: A Qualitative StudyDocument9 pagesWomen's Expectations From Delivery Nurses of Vaginal Birth: A Qualitative Studykaycelyn jimenezNo ratings yet
- Chlamydia: Chlamydia Rapid Test Device (Swab/Urine)Document3 pagesChlamydia: Chlamydia Rapid Test Device (Swab/Urine)Cristhian CuviNo ratings yet
- Minor Cases of Piolo PascualDocument3 pagesMinor Cases of Piolo PascualdonzkieNo ratings yet
- HBI Blacklist Journals 2018Document123 pagesHBI Blacklist Journals 2018pptpptNo ratings yet
- AFP Vision 2028: A World-Class Armed Forces, Source of National PrideDocument2 pagesAFP Vision 2028: A World-Class Armed Forces, Source of National PrideLevy Garcia SanchezNo ratings yet
- Histology of Oral Mucous Membrane and GingivaDocument86 pagesHistology of Oral Mucous Membrane and GingivahazeemmegahedNo ratings yet
- Dentistry Semester 1 SAQDocument4 pagesDentistry Semester 1 SAQKan Chang YuNo ratings yet
- Assessment of Common Criteria For Awake Extubation in Infants and Young ChildrenDocument8 pagesAssessment of Common Criteria For Awake Extubation in Infants and Young ChildrenSiti HumairahNo ratings yet
- Jurnal Obes 1Document22 pagesJurnal Obes 1mat norNo ratings yet
- K11-Urethral Stricture DiseaseDocument14 pagesK11-Urethral Stricture DiseaseagnesNo ratings yet
- UltrasonographyDocument5 pagesUltrasonographyapi-272007868No ratings yet
- PancreasDocument11 pagesPancreasCheng XinvennNo ratings yet
- Pain Assessment in PediatricDocument4 pagesPain Assessment in PediatricfitriaNo ratings yet
- 4f4f3d97-3c1c-49d9-8f67-7c1bd1d9f142Document325 pages4f4f3d97-3c1c-49d9-8f67-7c1bd1d9f142James CapplemanNo ratings yet
- Vocabulary For ExamsDocument53 pagesVocabulary For ExamsRajat AgarwalNo ratings yet
- Nogales Vs CMCDocument2 pagesNogales Vs CMCmyles15No ratings yet
- Case StudyDocument21 pagesCase StudyKavi rajput100% (3)
- GCM Clerks Guide CPCMH v1.3Document114 pagesGCM Clerks Guide CPCMH v1.3savan patelNo ratings yet
- Medical Jurisprudence LectureDocument198 pagesMedical Jurisprudence LectureErwin April Midsapak100% (3)
- Child Survival and Safe Motherhood Programme (CSSMP) : 1.CSSM Programme Initiated in The YearDocument8 pagesChild Survival and Safe Motherhood Programme (CSSMP) : 1.CSSM Programme Initiated in The YearJagveer ChauhanNo ratings yet
- Master Program in Clinical Pharmacy Curriculum 1 PDFDocument1 pageMaster Program in Clinical Pharmacy Curriculum 1 PDFhadiatussalamah100% (2)