Professional Documents
Culture Documents
Ocr Online
Uploaded by
Sebastián RivadeneiraOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ocr Online
Uploaded by
Sebastián RivadeneiraCopyright:
Available Formats
Treatment Options Therapeutic options for specific esophageal disorders are discussed below.
These should be em- rioved in conjunction with appropriate treatment *: r coexisting conditions that exacerbate primary - ."use secondary esophageal disorders. Lifestyle modifications for GERD include avoid- isce of such triggers as large meals, eating shortly ?*fore sleeping, and consuming foods and beverages that predictably cause symptoms. Patients nighttime symptoms should elevate the head si the bed. Patients should be cautioned regardthe hazards of obesity, smoking, and use of --.steroidal drugs, and encouraged to modify ----Tic risk factors. While the currently available r- wince to support these suggested lifestyle -_ir.ges is weak, their lack of expense and addi-
when needed, the vast majority t patients with erosive reflux disease will heal ir.d their symptoms will resolve on PPI therapy. Maintenance therapy at the dose needed for \ca.;ng has the highest chance of maintaining remission, but patients may be titrated down to the lowest daily dose that permits control of symptoms. Patients with nonerosive disease also respond to PPI therapy, and many can use on-demand therapy for symptom recurrence, rather than continuous therapy. The current concerns for longterm therapy are an increased risk for hip fractures and infections such as Clostridium difficile, and there is concern that certain agents may interfere with die metabolism of clopidogrel. For patients who have intolerance to or contraindications for PPI therapy, the histamine2- receptor antagonists and sucralfate have some demonstrated efficacy above placebo, although the benefits are less than for PPI therapy. Laparoscopic antireflux surgery also has efficacy similar to PPI therapy in long-term follow-up.133 For surgery, a somewhat higher improvement in primary GERD symptoms is offset by more symptoms of dysphagia and gas- bloat. About half of patients undergoing surgery require surgical revision or medical therapy over time. This, plus the risk of postoperative complications and the small risk of operative mortality, indicate that surgery should be reserved for those patients whose GERD-related symptoms and complications cannot be controlled adequately by medical therapy. For patients with morbid obesity complications warranting bar- iatric surgery, Roux-en-Y gastric bypass can be
rial benefits to health make them reasonable --ir. cations. However; these will be inadequate
-
-- r~ selves for most patients with GERD.
-
The mainstay for medical treatment of 3ERD in the twenty-first century is PPI ther- :: Most patients with GERD respond ad- ;. _;tely to a single daily PPI dose, taken before tie first meal of the day. With dose escalation tc twice daily
an effective antireflux procedure.134 However, vertical-banded gastroplasty is associated with a high rate of postoperative GERD. A variety of endoscopically delivered approaches to create an antireflux barrier have been developed. However none to date have demonstrated adequate control of reflux over a prolonged interval, and these should be considered investigational at this point. Dilation of peptic strictures improves symptoms of dysphagia. Control of GERD with PPI therapy reduces the need for repeat stricture dilation.135 The primary role of therapy in patients with Barrett's esophagus is to control the symptoms of GERD, since neither medical nor surgical treatment results in clinically meaningful regression of Barrett's mucosa. Given the reduced sensitivity of the esophagus to acid exposure in many patients with Barrett's esophagus, reflux therapy adequate to control symptoms may not result in normalization of esophageal acid exposure. Ongoing PPI therapy may inhibit the development of dysplasia in Barrett's esophagus.134 However,
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Doulci Activator For IOS 9Document2 pagesDoulci Activator For IOS 9Syafiq Aiman100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
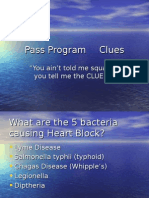
- Pass Program CluesDocument851 pagesPass Program CluesAlfyGototron100% (1)
- Keppel's lease rights and option to purchase land upheldDocument6 pagesKeppel's lease rights and option to purchase land upheldkdcandariNo ratings yet
- Maheshwar Handlooms Cluster Diagnostic StudyDocument15 pagesMaheshwar Handlooms Cluster Diagnostic Studyumang31390100% (3)
- Mini Lecture and Activity Sheets in English For Academic and Professional Purposes Quarter 4, Week 5Document11 pagesMini Lecture and Activity Sheets in English For Academic and Professional Purposes Quarter 4, Week 5EllaNo ratings yet
- CRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionDocument264 pagesCRUSADE of PRAYERS 1-170 Litany 1-6 For The Key To Paradise For DistributionJESUS IS RETURNING DURING OUR GENERATION100% (10)
- Military Divers ManualDocument30 pagesMilitary Divers ManualJohn0% (1)
- Ecr2019 C-1731Document13 pagesEcr2019 C-1731Sebastián RivadeneiraNo ratings yet
- Handling Questions Step by Step by Steven R. Daugherty, PH.D PDFDocument4 pagesHandling Questions Step by Step by Steven R. Daugherty, PH.D PDFYossef HammamNo ratings yet
- Arterias Suprarrenales: Sebastián RivadeneiraDocument19 pagesArterias Suprarrenales: Sebastián RivadeneiraSebastián RivadeneiraNo ratings yet
- PNP TELEPHONE DIRECTORY As of JUNE 2022Document184 pagesPNP TELEPHONE DIRECTORY As of JUNE 2022lalainecd0616No ratings yet
- Causes of WWI: Alliances, Militarism & AssassinationDocument4 pagesCauses of WWI: Alliances, Militarism & AssassinationJoshua De Leon TuasonNo ratings yet
- Aerospace & Aviation Job RolesDocument74 pagesAerospace & Aviation Job RolesBharat JainNo ratings yet
- Homologation Form Number 5714 Group 1Document28 pagesHomologation Form Number 5714 Group 1ImadNo ratings yet
- Postmodern Dystopian Fiction: An Analysis of Bradbury's Fahrenheit 451' Maria AnwarDocument4 pagesPostmodern Dystopian Fiction: An Analysis of Bradbury's Fahrenheit 451' Maria AnwarAbdennour MaafaNo ratings yet
- The Man of Sorrows Wednesday of Holy Week Divine IntimacyDocument5 pagesThe Man of Sorrows Wednesday of Holy Week Divine IntimacyTerri ThomasNo ratings yet
- Issues and Concerns Related To Assessment in MalaysianDocument22 pagesIssues and Concerns Related To Assessment in MalaysianHarrish ZainurinNo ratings yet
- Fundamentals of Analytics in Practice /TITLEDocument43 pagesFundamentals of Analytics in Practice /TITLEAcad ProgrammerNo ratings yet
- HRM ........Document12 pagesHRM ........Beenish AbbasNo ratings yet
- Sarina Dimaggio Teaching Resume 5Document1 pageSarina Dimaggio Teaching Resume 5api-660205517No ratings yet
- Insecticide Mode of Action Classification GuideDocument6 pagesInsecticide Mode of Action Classification GuideJose Natividad Flores MayoriNo ratings yet
- SEED TREATMENT WITH BOTANICAL EXTRACTSDocument18 pagesSEED TREATMENT WITH BOTANICAL EXTRACTSRohitNo ratings yet
- The Apostolic Church, Ghana English Assembly - Koforidua District Topic: Equipping The Saints For The MinistryDocument2 pagesThe Apostolic Church, Ghana English Assembly - Koforidua District Topic: Equipping The Saints For The MinistryOfosu AnimNo ratings yet
- Public Relations & Communication Theory. J.C. Skinner-1Document195 pagesPublic Relations & Communication Theory. J.C. Skinner-1Μάτζικα ντε Σπελ50% (2)
- Salzer Panel Accessories Price List - 01st January 2019Document40 pagesSalzer Panel Accessories Price List - 01st January 2019Chandra SekaranNo ratings yet
- AMU2439 - EssayDocument4 pagesAMU2439 - EssayFrancesca DivaNo ratings yet
- Method Statement Soil NailedDocument2 pagesMethod Statement Soil NailedFa DylaNo ratings yet
- AnnovaDocument4 pagesAnnovabharticNo ratings yet
- OutliningDocument17 pagesOutliningJohn Mark TabbadNo ratings yet
- Krittika Takiar PDFDocument2 pagesKrittika Takiar PDFSudhakar TomarNo ratings yet
- Superstitious Beliefs of MaranaoDocument13 pagesSuperstitious Beliefs of MaranaoKhent Ives Acuno SudariaNo ratings yet
- TASKalfa 2-3-4 Series Final TestDocument4 pagesTASKalfa 2-3-4 Series Final TesteldhinNo ratings yet
- KAMAGONGDocument2 pagesKAMAGONGjeric plumosNo ratings yet
- Class 7 Summer Vacation PDFDocument4 pagesClass 7 Summer Vacation PDFPrince RajNo ratings yet