Professional Documents
Culture Documents
Uri P. Monte de Ramos Bsn-Iii Group G
Uploaded by
Uri Perez MontedeRamosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Uri P. Monte de Ramos Bsn-Iii Group G
Uploaded by
Uri Perez MontedeRamosCopyright:
Available Formats
Uri P.
Monte de Ramos
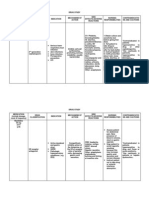
ASSISTING WITH A CAST APPLICATION
BSN-III
Group G 2013
Purpose: To support and protect injured bones and soft tissue, reducing pain, swelling, and muscle spasm, maintains alignment and prevents movement of the bones while it heals.
Special Considerations: Before and after cast application: 1. Assess for signs of restricted circulation 2. Take the clients pulse rate, respiratory rate, and blood pressure Administer ordered analgesics before cast application Before cast is applied, remove clothing from the body area and rings from fingers of the affected limb Ensure safe storage of the clients valuables Wash the skin area to receive the cast and dry it thoroughly if ordered Stabilize and support the limb appropriately during cast application. Remove excess cast material from clients skin after application. Document assessment and interventions.
Equipment: Rolls of cast materials Plastic lined bucket of water at the prescribed temperature: 1. Tepid water for Plaster of Paris and water activated 2. Cool water at 26 C (80 F) for polyester and cotton cast or A thermostatically controlled hydro collator or a boiler or cooking pot with a temperature- regulating thermometer for a thermoplastic cast.
Uri P. Monte de Ramos
Stockinet Cotton sheet wadding or padding Felt padding (optional) Plaster Splints (optional) Moisture- resistant drapes Rubber gloves Plastic aprons Water- soluble lubricant Plaster knife Large bandage scissors Pillows Damp cloth
BSN-III
Group G 2013
PROCEDURE 1. Explain the procedure to the client, including the length of time the cast material requires for drying. Explain that the cast may feel warm during and after the application 2. Provide an analgesic as ordered 3. Assist the client into a comfortable sitting or lying position 4. Remove clothing from the body area and rings from fingers of the affected limb and give them to a family member or store safely in a locked safe.
RATIONALE
Uri P. Monte de Ramos
5. Support the part to receive the cast 6. Wash the skin area, and dry it thoroughly, if ordered. If there is no open wound, powder may be applied. 7. Provide stockinet of the correct size if used, and cut it several inches longer than the length of the extremity so that it will extend beyond the plaster edges. Then roll the stockinet to facilitate application. 8. Provide sheet wadding and felt pads as needed. Usually 2- 3 layers are applied. 9. Provide gloves for the physician prior to application of the cast material. 10. Hand the physician the casting material or place the material within the physicians reach. Preparation of cast material varies depending on the type of casting material used. 11. Squeeze a generous amount of water-soluble lubricant on the physicians gloves as requested 12. Support the limb while the physician applies the stockinet, padding, and cast material. With one hand, grasp the clients toes for a leg cast or fingers for an arm cast, and with the other hand support beneath the limb areas on which the physician is not working. 13. After the cast is applied, pull the stockinet out over the proximal and distal cast opening edges, while the
BSN-III
Group G 2013
Uri P. Monte de Ramos
physician secures it in place with one or two layers of cast material. 14. Remove any excess cast material deposited accidentally on the clients skin. 15. Assess the client with special reference to the cast. 16. Provide firm support for the cast. 17. Gather and dispose the used materials appropriately 18. Document.
BSN-III
Group G 2013
Uri P. Monte de Ramos
BSN-III
Group G 2013
CLIENT CARE IMMEDIATELY AFTER A CAST APPLICATION
Equipment: Soft, pliable pillows PROCEDURE 1. Assess the toes and fingers for nerve or circulatory impairments every 30 mins for several hours following application and then every 3 hours for the first 24-48 hours or until all signs and symptoms of impairment are negative RATIONALE 1 2 3 4 5
2. Immediately after the cast is applied, place it on pillows. Avoid using plastic or rubber pillows. 3. Support the cast in the palms of your hands rather than your fingertips 4. Control swelling by elevating arms or legs on pillows or, for leg fracture, by elevating the foot of the bed 5. Report excessive swelling and indications of neurovascular impairments to the physician or nurse in charge. 6. Apply ice packs to a hip spica cast 7. Expose the cast to the circulating air
Uri P. Monte de Ramos
8. Check agency policy about the recommended turning frequency for clients with different kinds of cast 9. Avoid the use of artificial means to facilitate drying. This means including fans, hairdryers, infrared lamps, and electric heaters 10. Monitor drainage for 24-72 hours after surgery. Outline the stained area every 8 hours.
BSN-III
Group G 2013
11. Never ignore any complaints of pain, burning or pressure. If patient is unable to communicate, be alert to changes in temperament, restlessness, or fussiness.
12. Give pain medications selectively 13. Do not disregard the cessation of persistent pain or discomfort complaints 14. Document
Uri P. Monte de Ramos
BSN-III
Group G 2013
CONTINUING CARE FOR CLIENTS WITH CASTS
Special Considerations: Remove crumbs of plaster from the skin, petal rough cast edges. For bed- confined patients, provide skin care over all bony prominences and turn the clients at least every 4 hours Keep the cast clean and dry Encourage clients to move toes or fingers of the casted extremity frequently Provide necessary instructions about cast care, ways to move safely, activity allowed, exercises, elevating the involved extremity, signs of neurovascular problems, ways to handle itching
Equipment: Rubbing alcohol Mineral, olive, or baby oil to apply to the skin after cast removal Adhesive tape Scissors Damp washcloth for Plaster of Paris Warm water and a mild soap for synthetic casts Pillows Fracture pan
Uri P. Monte de Ramos
PROCEDURE 1. Wash crumbs of plaster from the skin with a damp cloth and feel along the cast edges or areas that press into the clients skin. It may be necessary to use a duck billed cast bender to bend cast edges that may irritate the skin 2. Cover rough edges of the cast when it is dry. If the stockinet has not been used to line the cast, petal the edge with small strips of adhesive tape. 3. Check the cast daily for foul odors 4. Discourage the patient from using long sharp objects to scratch under the cast 5. When cast is removed, dry, flaky and encrusted skin is observed, remove this debris gently and gradually by: a. Apply oil (mineral, olive, or baby) RATIONALE
BSN-III
Group G 2013
1 2 3 4 5
b. Soak the skin with warm water and dry it
c. Caution the client not to rub the area too vigorously
d. repeat steps a and b for several days
Keeping the Cast Clean and Dry 6. Tub baths and showers are contraindicated. POP cast is
Uri P. Monte de Ramos
kept clean by wiping it with a damp cloth. Place a bib or towel over a body cast to catch spills. If a spill does wet the cast, allow the area to air dry.
BSN-III
Group G 2013
7. Use a fracture bedpan for people with long leg, hip spica, or body casts. 8. Before placing the client on the bed pan, tuck plastic or other waterproof material around the top of a long leg cast or in around the perineal cutout. Remove plastic when elimination is completed 9. For people with long leg casts, keep the cast supported on pillows while the client is on bed pan. 10. For clients with hip spica casts, support both extremities and the back on pillows so that they are as high as the buttocks 11. When removing the bedpan, hold it securely while the client is turning or lifting the buttocks. After removing the bedpan, thoroughly clean and dry the perineal area
12. Synthetic casts: Synthetic casts can be cleaned readily and may, with the physicians permission, be immersed in water if polypropylene stockinet and padding were applied. a. Wash the soiled area with warm water and a mild
Uri P. Monte de Ramos
soap
BSN-III
Group G 2013
b. Thoroughly rinse the soap from the cast
c. Dry thoroughly to prevent skin maceration and ulceration under the cast.
d. If the cast is immersed in water, the cast and underlying padding and stockinet must be dried thoroughly. First blot excess water from the cast with a towel. Then use a handheld blow-dryer on the cool or warm setting, directing the air stream in a sweeping motion over the exterior of the cast for about 1 hour or until the client no longer feels a cold clammy sensation like that produced by a wet bathing suit.
Turning and Positioning Clients 13. Place pillows in such a way that: a. Body parts press against the cast edges as little as possible.
b. Toes, heels, elbows, etc., are protected from pressure against bed surface.
Uri P. Monte de Ramos
BSN-III
Group G 2013
c. Body alignment is maintained
14. Plan and implement a turning schedule incorporating all possible positions.
Exercise 15. Unless contraindicated, encourage active ROM exercises for all joints on the affected extremities, as well as on the joints proximal and distal to the cast
16. Encourage the client to move the toes and/or fingers of the casted extremity as frequently as possible.
17. With the physicians approval, teach isometric (muscle setting) exercises.
18. Teach isometric exercises on the clients unaffected limb before the person applies it to the affected limb. Demonstrate muscle palpation while the client is carrying out the exercise. 19. Document assessments and nursing implementations on the appropriate records.
Uri P. Monte de Ramos
TRACTION CARE
BSN-III
Group G 2013
Purpose: To apply a continuous pulling force to an extremity or body part, maintain its alignment, and prevent infection.
Guidelines: All traction should have a counter traction to prevent the client from being pulled by the force of traction against the pulleys or the bed, thus negating the traction To apply and maintain the correct amount of traction, all traction weights should be hanging freely and the ropes should not touch any part of the bed. The traction force should follow an established line of pull. The line of pull determines the position and alignment of the body as prescribed by the physician Traction should always be applied while the client is in proper body alignment in a supine positio
Equipment: Protective skin devices, e.g. heel protectors Trapeze Rubbing alcohol Antiseptic agent Sterile gauze dressing Picking forceps PROCEDURE 1. Inspect the traction apparatus regularly, whenever you are at the bedside or at prescribed intervals, such as every 2 hours 2. Provide protective devices and measures to safeguard RATIONALE 1 2 3 4 5
Uri P. Monte de Ramos
the skin. E.g. heel protectors, pillows, etc) massage the skin. 3. Maintain the client in supine position unless there are other orders 4. Provide a trapeze to assist the client to move and lift the body for back care if the person is unable to turn, e.g., if the client has balanced suspension traction 5. Do not remove skeletal and adhesive skin traction. 6. Non adhesive skin traction is intermittent and can be removed; check agency policy about any orders required. Remove weights first; then unwrap the bandage and provide skin care. Rewrap the limb and slowly reattach the weights 7. Provide pin site care and this varies with different hospital protocols. Carefully inspect the site Use sterile technique Remove crusts with a rolling technique Cover sites with a sterile barrier Determine the frequency of care by the amount of drainage 8. Teach client deep breathing and coughing. 9. Teach the client appropriate exercises 10. Document
BSN-III
Group G 2013
Uri P. Monte de Ramos
BSN-III
Group G 2013
You might also like
- Microbiology and ParasitologyDocument14 pagesMicrobiology and ParasitologyTyRa cHiAnE A. LaPeRa86% (43)
- Procedure for Staple and Suture RemovalDocument15 pagesProcedure for Staple and Suture RemovalRajaNo ratings yet
- Cast Care GuideDocument12 pagesCast Care GuidesuperduperfriendshipNo ratings yet
- Skin Preparation and Draping On Surgical SiteDocument5 pagesSkin Preparation and Draping On Surgical SiteHannah Quion100% (2)
- 2 Skin Preparation and DrapingDocument34 pages2 Skin Preparation and Drapingclaire yowsNo ratings yet
- Cast CareDocument1 pageCast CareCarmelita SaltNo ratings yet
- Colostomy Care ChecklistDocument6 pagesColostomy Care ChecklistTensai Olive DundundNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- CNN Practice QuestionsDocument5 pagesCNN Practice QuestionsUri Perez MontedeRamosNo ratings yet
- (Oxy) Med-Surg Checklist With RationaleDocument13 pages(Oxy) Med-Surg Checklist With RationaleUri Perez MontedeRamos100% (1)
- GTA 03-08-002 Contaminated Casualty CareDocument2 pagesGTA 03-08-002 Contaminated Casualty Carerickoshea160No ratings yet
- Fiction story with suspicious eventsDocument20 pagesFiction story with suspicious eventsjop pojNo ratings yet
- Guest Room LayoutDocument8 pagesGuest Room LayoutAjaypal Singh Rawat100% (1)
- Elie Saab Case StudyDocument19 pagesElie Saab Case Studysitanshubindra100% (4)
- POP cast application procedure guideDocument2 pagesPOP cast application procedure guideGopi RajNo ratings yet
- Care for Clients with CastsDocument2 pagesCare for Clients with CastsCarl Michael RazoNo ratings yet
- Caring for a Cast: Monitoring for ComplicationsDocument39 pagesCaring for a Cast: Monitoring for ComplicationsGrape JuiceNo ratings yet
- Bandaging: Process of Covering A Wound and An Injured PartDocument23 pagesBandaging: Process of Covering A Wound and An Injured Partclarheena100% (1)
- Caring of Client With Immobilization DevicesDocument6 pagesCaring of Client With Immobilization DevicesJmarie Brillantes PopiocoNo ratings yet
- Cast - Report On AfpmcDocument20 pagesCast - Report On AfpmcGillarhymesNo ratings yet
- Operating Room Orientation Manual Goals &Document4 pagesOperating Room Orientation Manual Goals &bhuselleNo ratings yet
- Colostomy Care DefinitionDocument3 pagesColostomy Care DefinitionAICEL A. ABILNo ratings yet
- Performing Surgical Skin Preparation and DrapingDocument12 pagesPerforming Surgical Skin Preparation and DrapingZerimar Dela CruzNo ratings yet
- Figure Eight Bandage ChecklistDocument2 pagesFigure Eight Bandage ChecklistLene Medi100% (1)
- Surgical AsepsisDocument29 pagesSurgical AsepsisRyan Llanto100% (1)
- COLOSTOMYDocument5 pagesCOLOSTOMYangelaNo ratings yet
- UntitledDocument10 pagesUntitledmelissa guillermoNo ratings yet
- Standard Care and PracticeDocument4 pagesStandard Care and PracticeBlue's CluesNo ratings yet
- GASTROSTOMYDocument3 pagesGASTROSTOMYangelaNo ratings yet
- Incontinence Brief Change ProcedureDocument1 pageIncontinence Brief Change ProcedurelmaoheartsNo ratings yet
- Cast Care LectureDocument43 pagesCast Care LectureMicaNo ratings yet
- ChecklistDocument14 pagesChecklistYooleen SanchezNo ratings yet
- CASTINGDocument44 pagesCASTINGMaria Sofia Stephanie SatoriNo ratings yet
- Explain The Principles Invloved in Perineal Care and Perilite ExposureDocument5 pagesExplain The Principles Invloved in Perineal Care and Perilite ExposureCarmel Marie VenezuelaNo ratings yet
- Modified surgical positions and skin preparationDocument7 pagesModified surgical positions and skin preparationNicole Soo100% (1)
- Wound Dressing and Caring For Jackson Pratt DrainDocument3 pagesWound Dressing and Caring For Jackson Pratt DrainLyssa Marie EgeNo ratings yet
- 2 Changing A Dry Sterile DressingDocument3 pages2 Changing A Dry Sterile DressingAnn Jalover PerezNo ratings yet
- Presentation 4Document28 pagesPresentation 4Carmel Marie VenezuelaNo ratings yet
- Duties of A Scrub NurseDocument43 pagesDuties of A Scrub Nursejay kusainNo ratings yet
- Procedure For Simple Bandaging and Use of CrutchesDocument2 pagesProcedure For Simple Bandaging and Use of Crutchesyou.are.good.sonNo ratings yet
- Routine Pratice - Infection Control (Document4 pagesRoutine Pratice - Infection Control (Em HadleyNo ratings yet
- Lab Manuals, Paraffin, HydrocollatorDocument12 pagesLab Manuals, Paraffin, HydrocollatorChristian MontesNo ratings yet
- Suctioning and Tracheostomy Care Checklist 2021Document3 pagesSuctioning and Tracheostomy Care Checklist 2021CARL ANGEL JAOCHICO100% (1)
- Colostomy CareDocument3 pagesColostomy Care2-YA-4 ABEGAEL FERNANDEZNo ratings yet
- Name: Bontilao, Jimnah Rhodrick M. Level: 3-B Instructor in Charge: MRS. AISSA CARLIT Date Materials Checked: Date PerformedDocument7 pagesName: Bontilao, Jimnah Rhodrick M. Level: 3-B Instructor in Charge: MRS. AISSA CARLIT Date Materials Checked: Date PerformedJimnah Rhodrick BontilaoNo ratings yet
- External Douches or Perineal Care: DefinitionDocument48 pagesExternal Douches or Perineal Care: DefinitionKenneth Myro GarciaNo ratings yet
- Skin TraksiDocument19 pagesSkin TraksiAhmad RizkyNo ratings yet
- Administering Topical Medication With RATIONALEDocument3 pagesAdministering Topical Medication With RATIONALEhjl padillaNo ratings yet
- Preoperative skin preparation and draping techniquesDocument26 pagesPreoperative skin preparation and draping techniquesKatrina Ponce100% (1)
- Duties of A Scrub NurseDocument2 pagesDuties of A Scrub NurseKim Celeste MatulacNo ratings yet
- SKIN PREP REDUCE SURGICAL SITE INFECTIONDocument4 pagesSKIN PREP REDUCE SURGICAL SITE INFECTIONJerson EdilloNo ratings yet
- BandagelecDocument47 pagesBandagelecmaridelleNo ratings yet
- DONNING and DoffingDocument3 pagesDONNING and DoffingChang GelvoleoNo ratings yet
- FACDocument8 pagesFACchaitanyaNo ratings yet
- Critical Thinking Nursing Care LippincotsDocument35 pagesCritical Thinking Nursing Care Lippincotseric100% (1)
- Perioperative SkillsDocument23 pagesPerioperative Skillsapi-3722454100% (1)
- 3 - Prelim ProceduresDocument4 pages3 - Prelim ProceduresAisha CorobongNo ratings yet
- COLOSTOMYDocument4 pagesCOLOSTOMYbambam1aNo ratings yet
- Caring For A Hemovac DrainDocument15 pagesCaring For A Hemovac DrainJaily Mariano0% (1)
- Parenteral Medication: Prepared By: Level II InstructorsDocument105 pagesParenteral Medication: Prepared By: Level II InstructorsJayrelle D. SafranNo ratings yet
- Performing a sterile dressing changeDocument14 pagesPerforming a sterile dressing changeHannaNo ratings yet
- NAIL AND FOOT CARE ROUTINEDocument5 pagesNAIL AND FOOT CARE ROUTINELexie KepnerNo ratings yet
- NSG126 - 4 - G - Skills - 6&7 - Checklists - SIGNAR, NIKITADocument7 pagesNSG126 - 4 - G - Skills - 6&7 - Checklists - SIGNAR, NIKITANikita SignarNo ratings yet
- Applying Restraints ProcedureDocument2 pagesApplying Restraints ProcedureCarol Neng CalupitanNo ratings yet
- Applying Splint - CheklistDocument3 pagesApplying Splint - CheklistAh AlshaibaniNo ratings yet
- Module 2 - Bandaging of Amputated Leg With RationaleDocument3 pagesModule 2 - Bandaging of Amputated Leg With RationaleAryaj SulitNo ratings yet
- Survival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)From EverandSurvival Skills: How to Survive Anything and Anywhere in the World (A Comprehensive Guide to Preparing for and Overcoming Challenges of Earthquakes)No ratings yet
- Integrating Technology in Curriculum DevelopmentDocument2 pagesIntegrating Technology in Curriculum DevelopmentUri Perez MontedeRamosNo ratings yet
- Curriculum and Instruction Diagnostic TestDocument2 pagesCurriculum and Instruction Diagnostic TestUri Perez MontedeRamosNo ratings yet
- tHE TEACHING STRATEGYDocument4 pagestHE TEACHING STRATEGYUri Perez MontedeRamosNo ratings yet
- Chapter 2 CrappppppyyyyyyyDocument5 pagesChapter 2 CrappppppyyyyyyyUri Perez MontedeRamosNo ratings yet
- NSAIDs and Chronic Kidney DiseaseDocument2 pagesNSAIDs and Chronic Kidney DiseaseAnonymous hF5zAdvwCCNo ratings yet
- Case Study Past Health HistoryDocument2 pagesCase Study Past Health HistoryUri Perez MontedeRamosNo ratings yet
- SkinDocument23 pagesSkinUri Perez MontedeRamosNo ratings yet
- Speaker: Dr. Leo Carlo V. Baloloy: "Patient-Centered Approach To Hemodialysis: Vascular Access in The Era of Fistula"Document3 pagesSpeaker: Dr. Leo Carlo V. Baloloy: "Patient-Centered Approach To Hemodialysis: Vascular Access in The Era of Fistula"Uri Perez MontedeRamosNo ratings yet
- Case Study Past Health HistoryDocument2 pagesCase Study Past Health HistoryUri Perez MontedeRamosNo ratings yet
- G Drug StudyDocument9 pagesG Drug StudyUri Perez MontedeRamosNo ratings yet
- Potential Causes Black Stained Peritoneal Dialysis TubingDocument6 pagesPotential Causes Black Stained Peritoneal Dialysis TubingUri Perez MontedeRamosNo ratings yet
- Lines .Docx PDocument4 pagesLines .Docx PUri Perez MontedeRamosNo ratings yet
- Obesity in ChildrenDocument5 pagesObesity in ChildrenUri Perez MontedeRamosNo ratings yet
- VitaminsDocument4 pagesVitaminsUri Perez MontedeRamosNo ratings yet
- BadmintonDocument4 pagesBadmintonUri Perez MontedeRamosNo ratings yet
- Effect of Innovative Training for Non-Multiculturalist Chemistry TeachersDocument2 pagesEffect of Innovative Training for Non-Multiculturalist Chemistry TeachersUri Perez MontedeRamosNo ratings yet
- CP OsteoDocument4 pagesCP OsteoUri Perez MontedeRamosNo ratings yet
- 9 Labor and DeliveryDocument6 pages9 Labor and DeliveryUri Perez MontedeRamosNo ratings yet
- Leopold's ManeuversDocument5 pagesLeopold's ManeuversUri Perez MontedeRamos100% (2)
- WRAP Sustainable Clothing GuideDocument30 pagesWRAP Sustainable Clothing GuideMatt Mace100% (1)
- Pravesh, Pratham Sopan, Dwita SopanDocument26 pagesPravesh, Pratham Sopan, Dwita SopanFacebook ComNo ratings yet
- COSHH DrakerDocument2 pagesCOSHH DrakerzaimNo ratings yet
- Different Types of WeddingsDocument8 pagesDifferent Types of WeddingsViolet PateNo ratings yet
- Blast - Vorticist ManifestoDocument38 pagesBlast - Vorticist ManifestoMutabilityNo ratings yet
- Māori Culture - WikipediaDocument38 pagesMāori Culture - WikipediaJai NairNo ratings yet
- Name: Surname: Points: - Index Number: English 1-Group 1 Circle The Correct AnswerDocument2 pagesName: Surname: Points: - Index Number: English 1-Group 1 Circle The Correct Answerrwgrewg tdegberdbNo ratings yet
- Customer Service Homework IiiDocument2 pagesCustomer Service Homework IiiAleyda Altamirano NietoNo ratings yet
- Counting Methods: 4 Quarter Period Math 8Document20 pagesCounting Methods: 4 Quarter Period Math 8Penke Mejado BelenNo ratings yet
- Uttara University Department of Industrial Engineering Semester: Summer-2013 Batch: 3 Syllabus of Offered CoursesDocument4 pagesUttara University Department of Industrial Engineering Semester: Summer-2013 Batch: 3 Syllabus of Offered CoursesSudipta BainNo ratings yet
- Pediatric Checklist EditedDocument72 pagesPediatric Checklist EditedJun Man100% (2)
- Linear Programming Formulation ProblemsDocument2 pagesLinear Programming Formulation Problemsvasanthh_mechNo ratings yet
- What Do They Do? Careers and ProfessionsDocument9 pagesWhat Do They Do? Careers and ProfessionsSEGURA ROBLEDO EDGAR GABRIEL ANTONIONo ratings yet
- Kenmore 50 Sewing Machine Instruction ManualDocument52 pagesKenmore 50 Sewing Machine Instruction ManualiliiexpugnansNo ratings yet
- Nail ArtDocument145 pagesNail ArtJim WilliamsNo ratings yet
- Ijftr 38 (3) 223-229Document7 pagesIjftr 38 (3) 223-229Farrukh JamilNo ratings yet
- Mantis TillerDocument32 pagesMantis TillercamhawkinsNo ratings yet
- 17331Document20 pages17331Amit GhadeNo ratings yet
- Summer Internship in Swaraj Mahindra Tractors.Document14 pagesSummer Internship in Swaraj Mahindra Tractors.PiyuSh AngRa100% (3)
- TC - Comparatives PracticeDocument2 pagesTC - Comparatives PracticeMohammed ZraibiNo ratings yet
- Top 40 Alpha Texting AbbreviationsDocument4 pagesTop 40 Alpha Texting AbbreviationsimstillarockstarNo ratings yet
- How To Sew An Under ScarfDocument3 pagesHow To Sew An Under Scarffazam8558No ratings yet
- Bittersweet Jul 16 2013Document490 pagesBittersweet Jul 16 2013imogeniousNo ratings yet
- The Brand I Love (Positioning)Document6 pagesThe Brand I Love (Positioning)Golam Sarwar GaziNo ratings yet
- Wooden Gear Clock Instructions 10-2 PDFDocument78 pagesWooden Gear Clock Instructions 10-2 PDFLuca Alberti50% (2)