Professional Documents
Culture Documents
Cleveland Clinic Journal of Medicine 2014 AYACHE 525 7
Uploaded by
Sundar Ramanathan0 ratings0% found this document useful (0 votes)
27 views3 pagesmedicine
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentmedicine
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views3 pagesCleveland Clinic Journal of Medicine 2014 AYACHE 525 7
Uploaded by
Sundar Ramanathanmedicine
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
Q: Can we reduce the risk of readmission
for a patient with an exacerbation of COPD?
MIRNA B. AYACHE, MD, MPH, FACP
Department of Hospital Medicine, Cleveland Clinic
SHAFIK BOYAJI, MD
Department of Hospital Medicine, Cleveland Clinic
JAMES C. PILE, MD
Department of Hospital Medicine, Cleveland Clinic; Associate Professor,
Cleveland Clinic Lerner College of Medicine of Case Western Reserve
University, Cleveland, OH; Deputy Editor, Cleveland Clinic Journal of Medicine
We think so. Some strategies to re-
duce readmission rates, such as co-
ordinating care and managing comorbidities,
apply to chronic diseases in general, while oth-
ers are disease-specifc. To reduce the need for
hospital readmission for chronic obstructive
pulmonary disease (COPD), coordinated ef-
forts involving both inpatient and outpatient
care are necessary. This can be achieved by us-
ing a checklist before discharge (TABLE 1) and
by implementing outpatient COPD programs
that continue patient education and provide
rapid access to medical support if needed.
See related commentary, page 528
There is room for improvement. COPD
is common and expensive, with high rates of
hospital readmission,
1
and up to 70% of the
money we spend on it goes for hospital care.
2
No wonder then that the Centers for Medicare
and Medicaid Services has now expanded its
Readmissions Reduction Program to include
acute COPD exacerbations.
3
Yet in a retrospec-
tive study, Yip et al
4
found that fewer than half
of patients hospitalized with acute exacerbation
of COPD received appropriate vaccinations,
counseling on smoking cessation, and long-act-
ing inhalersall of which are on our checklist.
4
The following interventions have been
demonstrated to be useful in reducing COPD
hospital admissions and the risk of death.
SMOKING CESSATION
Cigarette smoking is the most common and
easily identifable risk factor for COPD exac-
erbation.
5
Au et al
5
found that quitting smoking re-
duces the risk of COPD exacerbation (adjust-
CLEVELAND CLI NI C J OURNAL OF MEDI CI NE VOLUME 81 NUMBER 9 SEPTEMBER 2014 525
1-MINUTE CONSULT
doi:10.3949/ccjm.81a.13139
BRIEF ANSWERS
TO SPECIFIC
CLINICAL
QUESTIONS
A:
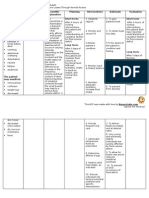
TABLE 1
Checklist for COPD patients
before they leave the hospital
Counseling on smoking cessation if the patient is a smoker or is
at risk of starting smoking again
Appropriate inuenza and pneumonia vaccinations
Long-acting bronchodilators: an anticholinergic or a beta-ago-
nist, or both (except GOLD group A patients, who have few symptoms
and are at a low risk of exacerbations); inhaled steroids for those
with previous exacerbations who are at high risk of relapse
Long-term oxygen therapy, if indicated, ie, in those with chronic
resting hypoxemia (room air PaO
2
55 mm Hg or 59 mm Hg with
signs of right-sided heart strain or polycythemia)
Home exercise program or pulmonary rehabilitation referral
after an exacerbation
Patient education regarding symptom monitoring and in-
haler therapy, including proper inhaler technique (see http://
my.clevelandclinic.org/disorders/Chronic_Obstructive_Pulmonary_
Disease/hic_Understanding_COPD.aspx)
Consider home noninvasive ventilator support in select
patients with recurrent hospitalization for acidotic exacerbation of
COPD if the patient qualies under Centers for Medicare and Medic-
aid Services guidelines,
20
ie:
Paco
2
52 mm Hg and
Evidence of nocturnal hypoventilation based on nocturnal oximetry
showing sustained desaturation to < 89% for 5 min on oxygen use and
Sleep apnea excluded
COPD = chronic obstructive pulmonary disease; GOLD = Global Strategy for the Diag-
nosis, Management, and Prevention of Chronic Obstructive Lung Disease
6
on September 5, 2014. For personal use only. All other uses require permission. www.ccjm.org Downloaded from
526 CLEVELAND CLI NI C J OURNAL OF MEDI CI NE VOLUME 81 NUMBER 9 SEPTEMBER 2014
REDUCE COPD READMISSION
ed hazard ratio 0.78, 95% confdence interval
[CI] 0.750.87), and the risk keeps decreasing
the longer the patient stays off tobacco.
5
Whether counseling hospitalized patients
on smoking cessation reduces the COPD read-
mission rate has not been well studied. How-
ever, a meta-analysis of nine randomized con-
trolled trials, two of which were done in the
hospital, revealed higher abstinence rates in
COPD patients who received extensive coun-
seling on smoking cessation.
7
For these rea-
sons, hospitalized COPD patients who smoke
should be strongly encouraged to quit.
6
PNEUMOCOCCAL AND INFLUENZA
VACCINATIONS
In a large retrospective study,
8
pneumococcal
vaccination was associated with a signifcantly
lower risk of hospitalization for pneumonia in
patients with chronic lung disease, including
those with COPD (relative risk [RR] 0.57,
95% CI 0.380.84). The beneft was even
greater with pneumococcal and infuenza vac-
cinations during the infuenza season (RR
0.28, 95% CI 0.140.58).
Randomized controlled trials indicate that
infuenza vaccination may reduce the rate of
COPD exacerbations, especially in epidemic
years when the proportion of exacerbations
due to infuenza is higher.
9
Wongsurakiat et al
10
found a signifcant re-
duction in the incidence of infuenza-related
acute respiratory illness in COPD patients in a
well-designed randomized, placebo-controlled
trial (RR 0.24, P = .005).
10
Similarly, in another randomized controlled
trial, pneumococcal vaccination was effective
in preventing community-acquired pneumonia
in COPD patients under age 65 and in those
with severe airfow obstruction, although no
statistically signifcant differences were found
among other groups of patients with COPD.
11
Therefore, infuenza and pneumococcal vac-
cinations are recommended by major COPD
guidelines, such as GOLD (Global Strategy for
the Diagnosis, Management, and Prevention of
Chronic Obstructive Lung Disease).
6
INHALERS
Inhaler therapy is recommended based on
COPD severity according to GOLD classif-
cation, and appropriate inhaler therapy with
proper inhaler technique reduces the number
of COPD exacerbations and hospitalizations.
6
Long-acting beta-agonists and anticholin-
ergics reduce the risk of COPD exacerbation
and hospitalization and so are preferred over
short-acting formulations except for patients
in GOLD group A, ie, those who have few
symptoms and are at low risk of exacerba-
tions.
6
Long-term treatment with inhaled corti-
costeroids with long-acting bronchodilators
is recommended for patients at high risk of
exacerbations (ie, those with two or more ex-
acerbations in the previous year or a forced ex-
piratory volume in 1 second [FEV
1
] less than
50% of predicted).
6
OXYGEN THERAPY
Two older randomized controlled trials, the
Nocturnal Oxygen Therapy Trial and the
Medical Research Council study, reviewed by
Stoller et al,
12
provided clear evidence that
oxygen therapy reduces the death rate and im-
proves quality of life in COPD patients who
have chronic resting hypoxemia (room air
Pao
2
55 mm Hg, or 59 mm Hg with signs
of right-sided heart strain or polycythemia).
PULMONARY REHABILITATION
Pulmonary rehabilitation likely reduces hos-
pital admissions by improving exercise capac-
ity.
13
A systematic review of six trials in 230
patients found that respiratory rehabilitation
after an acute COPD exacerbation reduced
the risk of COPD hospital admission (RR
0.26, 95% CI 0.120.54) and the risk of death
(RR 0.45, 95% CI 0.220.91).
13
OTHER INTERVENTIONS
Home noninvasive ventilator support re-
duced hospital and intensive care unit read-
missions in select patients recurrently hospi-
talized for acidotic exacerbations of COPD in
one small study.
14
Long-term antibiotic therapy. Although
there is evidence that azithromycin, taken
daily for 1 year, decreases the frequency of
COPD exacerbations,
15
concern persists that
this approach promotes antibiotic resistance,
and the GOLD guidelines do not recommend
Needed:
coordinated
efforts
involving both
inpatient and
outpatient care
on September 5, 2014. For personal use only. All other uses require permission. www.ccjm.org Downloaded from
CLEVELAND CLI NI C J OURNAL OF MEDI CI NE VOLUME 81 NUMBER 9 SEPTEMBER 2014 527
AYACHE AND COLLEAGUES
routinely using antibiotics in patients with
clinically stable COPD.
6
Rofumilast. According to the GOLD
guidelines, the phosphodiesterase-4 inhibi-
tor rofumilast (Daliresp) may be useful in
reducing exacerbations in patients who have
an FEV
1
less than 50% of predicted, chronic
bronchitis, and frequent exacerbations.
6
Referral. Patients who have severe recur-
rent COPD exacerbations despite appropriate
therapy will likely beneft from referral to a
pulmonary specialist for other options such
as theophylline, lung-reduction surgery, and
lung transplantation.
PATIENT EDUCATION AND OUTPATIENT
COPD PROGRAMS
There is growing evidence that outpatient
programs that provide education and medical
support signifcantly reduce the rate of hospi-
talizations for COPD.
1618
Patient education
includes symptom monitoring, early recogni-
tion of an exacerbation, appropriate use of in-
halers and nebulizers, and advice on smoking
cessation.
16
On the other hand, a Veterans Administra-
tion randomized controlled trial was stopped
early because of a higher rate of death in the
group that underwent a comprehensive care-
management program of COPD education, an
action plan for identifcation and treatment of
exacerbations, and scheduled proactive tele-
phone calls for case management.
19
Further study is needed to investigate the
cost-effectiveness and safety of COPD man-
agement programs and whether to adopt such
programs on a systematic level.
In conclusion, COPD patients require a
comprehensive approach based on studied
interventions. This may be achieved through
systematic methods that allow each patient to
beneft from all possible interventions appro-
priate for him or her. Hospitalization of COPD
patients provides an excellent opportunity to
implement this comprehensive approach.
REFERENCES
1. Westert GP, Lagoe RJ, Keskimki I, Leyland A, Murphy M. An inter-
national study of hospital readmissions and related utilization in
Europe and the USA. Health Policy 2002; 61:269278.
2. Halpern MT, Stanford RH, Borker R. The burden of COPD in the
USA: results from the Confronting COPD survey. Respir Med 2003;
97(suppl C):S81S89.
3. Centers for Medicare and Medicaid Services. Readmissions reduc-
tion program. www.cms.gov/Medicare/Medicare-Fee-for-Service-
Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html.
Accessed August 9, 2014.
4. Yip NH, Yuen G, Lazar EJ, et al. Analysis of hospitalizations for
COPD exacerbation: opportunities for improving care. COPD 2010;
7:8592.
5. Au DH, Bryson CL, Chien JW, et al. The effects of smoking cessation
on the risk of chronic obstructive pulmonary disease exacerbations.
J Gen Intern Med 2009; 24:457463.
6. Vestbo J, Hurd SS, Agust AG, et al. Global strategy for the diagno-
sis, management, and prevention of chronic obstructive pulmonary
disease: GOLD executive summary. Am J Respir Crit Care Med 2013;
187:347365.
7. Thabane M; COPD Working Group. Smoking cessation for patients
with chronic obstructive pulmonary disease (COPD): an evidence-
based analysis. Ont Health Technol Assess Ser 2012; 12:150.
8. Nichol KL, Baken L, Wuorenma J, Nelson A. The health and eco-
nomic benets associated with pneumococcal vaccination of elderly
persons with chronic lung disease. Arch Intern Med 1999; 159:2437
2442.
9. Poole PJ, Chacko E, Wood-Baker RW, Cates CJ. Inuenza vaccine
for patients with chronic obstructive pulmonary disease. Cochrane
Database Syst Rev 2006; 1:CD002733.
10. Wongsurakiat P, Maranetra KN, Wasi C, Kositanont U, Dejsomritru-
tai W, Charoenratanakul S. Acute respiratory illness in patients with
COPD and the effectiveness of inuenza vaccination: a randomized
controlled study. Chest 2004; 125:20112020.
11. Alfageme I, Vazquez R, Reyes N, et al. Clinical efcacy of anti-
pneumococcal vaccination in patients with COPD. Thorax 2006;
61:189195.
12. Stoller JK, Panos RJ, Krachman S, Doherty DE, Make B; Long-term
Oxygen Treatment Trial Research Group. Oxygen therapy for
patients with COPD: current evidence and the long-term oxygen
treatment trial. Chest 2010; 138:179187.
13. Puhan MA, Scharplatz M, Troosters T, Steurer J. Respiratory reha-
bilitation after acute exacerbation of COPD may reduce risk for
readmission and mortalitya systematic review. Respir Res 2005;
6:54.
14. Tuggey JM, Plant PK, Elliott MW. Domiciliary non-invasive ventila-
tion for recurrent acidotic exacerbations of COPD: an economic
analysis. Thorax 2003; 58:867871.
15. Albert RK, Connett J, Bailey WC, et al; COPD Clinical Research Net-
work. Azithromycin for prevention of exacerbations of COPD.
N Engl J Med 2011; 365:689698.
16. Lawlor M, Kealy S, Agnew M, et al. Early discharge care with ongo-
ing follow-up support may reduce hospital readmissions in COPD.
Int J Chron Obstruct Pulmon Dis 2009; 4:5560.
17. Gadoury MA, Schwartzman K, Rouleau M, et al; Chronic
Obstructive Pulmonary Disease axis of the Respiratory Health
Network, Fonds de la Recherche en Sant du Qubec (FRSQ). Self-
management reduces both short- and long-term hospitalisation in
COPD. Eur Respir J 2005; 26:853857.
18. Rice KL, Dewan N, Bloomeld HE, et al. Disease management
program for chronic obstructive pulmonary disease: a randomized
controlled trial. Am J Respir Crit Care Med 2010; 182:890896.
19. Fan VS, Gaziano JM, Lew R, et al. A comprehensive care manage-
ment program to prevent chronic obstructive pulmonary disease
hospitalizations: a randomized, controlled trial. Ann Intern Med
2012; 156:673683.
20. COPD Working Group. Noninvasive positive pressure ventilation for
chronic respiratory failure patients with stable chronic obstructive
pulmonary disease (COPD): an evidence-based analysis. Ont Health
Technol Assess Ser 2012; 12(9):151.
ADDRESS: James C. Pile, MD, Department of Hospital Medicine,
M2-Annex, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH 44195;
e-mail: pilej@ccf.org
on September 5, 2014. For personal use only. All other uses require permission. www.ccjm.org Downloaded from
You might also like
- Adult Combined ScheduleDocument13 pagesAdult Combined ScheduleJustin Ng SincoNo ratings yet
- A Hands On Approach To Patch TestingDocument11 pagesA Hands On Approach To Patch TestingSundar RamanathanNo ratings yet
- How To Say No 5 Steps To Stop Being A People Pleaser Life Kit NPRDocument7 pagesHow To Say No 5 Steps To Stop Being A People Pleaser Life Kit NPRSundar Ramanathan100% (1)
- How To Say No 5 Steps To Stop Being A People Pleaser Life Kit NPRDocument7 pagesHow To Say No 5 Steps To Stop Being A People Pleaser Life Kit NPRSundar Ramanathan100% (1)
- Best Commuter Towns in NJ To NYC Midtown Direct Homes PDFDocument3 pagesBest Commuter Towns in NJ To NYC Midtown Direct Homes PDFSundar RamanathanNo ratings yet
- Rasi Navamsa: Untitled ChartDocument11 pagesRasi Navamsa: Untitled ChartSundar RamanathanNo ratings yet
- Rasi Navamsa: Untitled ChartDocument11 pagesRasi Navamsa: Untitled ChartSundar RamanathanNo ratings yet
- 28 AshtakvargaThumbRules PDFDocument11 pages28 AshtakvargaThumbRules PDFAnand AgrawalNo ratings yet
- Rasi Navamsa: Untitled ChartDocument11 pagesRasi Navamsa: Untitled ChartSundar RamanathanNo ratings yet
- What You Should Know Before Buying A Home Security SystemDocument13 pagesWhat You Should Know Before Buying A Home Security SystemSundar RamanathanNo ratings yet
- Hemodialysis KineticsDocument26 pagesHemodialysis KineticsSundar RamanathanNo ratings yet
- .. Shri Lalitasahasranama Stotram ..: August 20, 2017Document24 pages.. Shri Lalitasahasranama Stotram ..: August 20, 2017balarrusNo ratings yet
- Game of ThronesDocument34 pagesGame of ThronesSundar RamanathanNo ratings yet
- Anthem CVS Caremark Value Formulary 072020Document56 pagesAnthem CVS Caremark Value Formulary 072020Sundar RamanathanNo ratings yet
- Autism Support NJ Excellent Learning CoursesDocument6 pagesAutism Support NJ Excellent Learning CoursesSundar RamanathanNo ratings yet
- AgniDocument6 pagesAgniSundar Ramanathan100% (1)
- AWS AICamp CertificationDocument39 pagesAWS AICamp CertificationSundar RamanathanNo ratings yet
- Prescription Program: Drug List - To Be Used by Members Who Have A Three (3) Tiered Drug PlanDocument8 pagesPrescription Program: Drug List - To Be Used by Members Who Have A Three (3) Tiered Drug PlanSundar RamanathanNo ratings yet
- Arya ManDocument1 pageArya ManSundar RamanathanNo ratings yet
- Press Release OCI Reissuance 122019Document1 pagePress Release OCI Reissuance 122019Sundar RamanathanNo ratings yet
- Game of ThronesDocument34 pagesGame of ThronesSundar RamanathanNo ratings yet
- CRRT Order Set-RenalDocument4 pagesCRRT Order Set-RenalSundar RamanathanNo ratings yet
- Upakarma Devanagari 1Document15 pagesUpakarma Devanagari 1Harish KNNo ratings yet
- 2012 NDT Wetzels Genetic FSGSDocument9 pages2012 NDT Wetzels Genetic FSGSSundar RamanathanNo ratings yet
- Bangalore Property Lawyers FundaDocument15 pagesBangalore Property Lawyers FundaSundar RamanathanNo ratings yet
- Sandhyavandanam ImportanceDocument13 pagesSandhyavandanam ImportanceSundar RamanathanNo ratings yet
- VyasapujaiDocument2 pagesVyasapujaiSundar RamanathanNo ratings yet
- Bringing Parents To Live in The United States As Permanent Residents USCISDocument3 pagesBringing Parents To Live in The United States As Permanent Residents USCISSundar RamanathanNo ratings yet
- VG Equity Income Jan 2018Document54 pagesVG Equity Income Jan 2018Sundar RamanathanNo ratings yet
- 2012 NDT Wetzels Genetic FSGSDocument9 pages2012 NDT Wetzels Genetic FSGSSundar RamanathanNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CV Professor DR Wan Faisham Wan IsmailDocument3 pagesCV Professor DR Wan Faisham Wan IsmailRayhan CeinNo ratings yet
- Iliotibial Band Syndrome - FannyDocument13 pagesIliotibial Band Syndrome - FannyAlfiani Rosyida Arisanti Syafi'iNo ratings yet
- Medifocus April 2007Document61 pagesMedifocus April 2007Pushpanjali Crosslay HospitalNo ratings yet
- Moderna COVID-19 Vaccine: BasicsDocument2 pagesModerna COVID-19 Vaccine: BasicsCanoa TrailNo ratings yet
- Twisted Risk Assesment 2Document2 pagesTwisted Risk Assesment 2api-306671250100% (1)
- Poster Viewing I: Case ReportsDocument39 pagesPoster Viewing I: Case ReportsGaurav SaxenaNo ratings yet
- Analysis On The Green Economic Productivity ofDocument42 pagesAnalysis On The Green Economic Productivity ofIrllyshouldslepepNo ratings yet
- Bertilsson 1978Document16 pagesBertilsson 1978gemmieyeahhhhNo ratings yet
- GGGDGGDocument414 pagesGGGDGGOtiosse MyosotisNo ratings yet
- Virtual GriefDocument1 pageVirtual GriefWXYZ-TV Channel 7 DetroitNo ratings yet
- Clinico-Pathological Review On Pravahika Vis-A-Vis AmoebiasisDocument3 pagesClinico-Pathological Review On Pravahika Vis-A-Vis AmoebiasisAdvanced Research PublicationsNo ratings yet
- Aunt Minnie Pediatric NeuroDocument15 pagesAunt Minnie Pediatric NeuroRommel OliverasNo ratings yet
- Is An Intensive Outpatient ProgramDocument1 pageIs An Intensive Outpatient ProgramJack williamNo ratings yet
- PERDEV Handout - M5 (Coping With Stress) - ModifiedDocument2 pagesPERDEV Handout - M5 (Coping With Stress) - ModifiedElla MirandaNo ratings yet
- Medical Billing ProcessDocument24 pagesMedical Billing ProcessNajamHass100% (5)
- Sbo and Ecf (Doc Gallo) SGD SurgeryDocument113 pagesSbo and Ecf (Doc Gallo) SGD SurgeryNikki MacasaetNo ratings yet
- Drug StudyDocument1 pageDrug StudyBSN 3-2 RUIZ, Jewel Anne F.No ratings yet
- Curative COVID-19 Test Results ReportDocument1 pageCurative COVID-19 Test Results ReportIsabella FonsecaNo ratings yet
- Bipolar Disorder Symptoms, Causes and TreatmentDocument108 pagesBipolar Disorder Symptoms, Causes and TreatmentMaica LectanaNo ratings yet
- Physiotherapy Functional Assessment GridDocument2 pagesPhysiotherapy Functional Assessment GridILR 2019No ratings yet
- Petronas Gas PGB PDFDocument34 pagesPetronas Gas PGB PDFAhmad Aiman100% (5)
- Assessing Children's Pain: R-Flacc Pain Rating Scale For Children With Developmental DisabilityDocument1 pageAssessing Children's Pain: R-Flacc Pain Rating Scale For Children With Developmental DisabilityifanNo ratings yet
- Salicylic Acid and Sulfur (Topical Route) : Commonly Used Brand Name(s)Document9 pagesSalicylic Acid and Sulfur (Topical Route) : Commonly Used Brand Name(s)Gutu DoinaNo ratings yet
- Herboboost Capsules: Kutki, Chandan)Document3 pagesHerboboost Capsules: Kutki, Chandan)Snehal AshtekarNo ratings yet
- Lumbar PunctureDocument18 pagesLumbar PunctureJaspreet KangNo ratings yet
- Case Study Fnes 366Document6 pagesCase Study Fnes 366api-347761303No ratings yet
- SolutionDocument7 pagesSolutionapi-269290275No ratings yet
- Study On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivDocument26 pagesStudy On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivR Hari0% (1)
- Deficient Fluid Volume (AGEDocument2 pagesDeficient Fluid Volume (AGENursesLabs.com83% (6)
- Fat Burner: Fitzoye Nutrition IntroducingDocument6 pagesFat Burner: Fitzoye Nutrition IntroducingrajeshNo ratings yet