Professional Documents
Culture Documents
1 s2.0 S0002937803001388 Main
Uploaded by
Andi Bintang0 ratings0% found this document useful (0 votes)
25 views3 pagesjhggvj
Original Title
1-s2.0-S0002937803001388-main
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjhggvj
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
25 views3 pages1 s2.0 S0002937803001388 Main
Uploaded by
Andi Bintangjhggvj
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 3
1202
The rate of unplanned pregnancy in the United States
remains high. A study performed by the Alan Guttmacher
Institute showed that 49% of all pregnancies in the United
States were unintended; 46% of those pregnancies re-
sulted in live births and 54% in induced abortions.
1
Unin-
tended pregnancies can result in serious personal,
socioeconomic, and public health consequences.
Multiple reasons have been suggested for the contin-
ued rate of unintended pregnancy. These include a lack
of patient education, ineffective contraceptive methods,
inconsistent use of contraception, unplanned sexual ac-
tivity, and contraceptive failure. Improvement of contra-
ceptive education has the potential to positively impact
rates of contraceptive failure, inconsistent contraceptive
use, and subsequently, rates of unintended pregnancy. An
individuals education and knowledge level of concep-
tion and contraception may influence the rate of unin-
tended pregnancies within a population. An appropriate
time to ensure exposure to educational material is during
the postpartum period of hospitalized women.
Health care providers are not fully using the postpar-
tum hospitalization period to promote contraception.
After the delivery, additional written literature may pro-
vide women with more valuable information than verbal
counseling alone.
2
In our university setting after the de-
livery, the women come from a variety of backgrounds,
and many of the women have had little or no prenatal
care or exposure to contraceptive counseling. The pa-
tients are seen in the postpartum period by a variety of
providers (including medical students, residents, mid-
wives, and faculty members), and the postpartum con-
traceptive counseling quality is highly variable and
difficult to control. Minimal pamphlets on various con-
traceptive options, but no comprehensive information,
are available currently to distribute in the postpartum
period. An hypothesis-driven cohort study that measured
baseline satisfaction levels and confidence in contracep-
tion decisions was performed in mothers after the deliv-
ery before and after the distribution of standardized
comprehensive written information about contracep-
tion. We proposed that the addition of comprehensive,
complete written information on all contraceptive op-
tions would increase the patients ability to make an in-
formed decision regarding the choice of postpartum
birth control.
Material and methods
Consent to survey hospitalized patients during the
postpartum period at Oregon Health and Sciences Uni-
versity was received from the institutional review board.
All English- and Spanish-speaking parturients during
April and May 2002 were invited to participate by com-
From the Department of Obstetrics and Gynecology, Oregon Health and
Science University.
Reprint requests: Lisa K Johnson, MD, 3181 SW Sam Jackson Park
Road L466,Portland, OR 97201. E-mail johnsoli@ohsu.edu
2003, Mosby, Inc. All rights reserved.
0002-9378/2003 $30.00 + 0
doi:10.1067/mob.2003.308
Patient satisfaction and the impact of written material about
postpartum contraceptive decisions
Lisa K. Johnson, MD, Alison Edelman, MD, and Jeffrey Jensen MD, MPH
Portland, Ore
OBJECTIVE: The purpose of this study was to evaluate the impact of written educational material about pa-
tient satisfaction and decision-making regarding postpartum contraception.
STUDY DESIGN: Baseline patient satisfaction and effectiveness of contraceptive counseling on a postpar-
tum unit was evaluated with the use of a self-administered questionnaire. Data were compared with patients
who received additional comprehensive written educational material during their postpartum hospitalization.
RESULTS: A total of 109 women participated in the study (control subjects, 53; intervention group, 56). De-
mographics and patient satisfaction with contraceptive counseling were similar between groups. Thirty-four
percent of the control subjects reported having received some sort of written information; all women in the in-
tervention group received a standardized comprehensive booklet of information during their postpartum stay
(P < .01). Among the women who received written information, the intervention group was more likely to
state that written material contributed to their ultimate choice in birth control (P < .01).
CONCLUSION: The postpartum distribution of written material about contraceptive options increases a womans
ability to make an informed decision regarding birth control. (Am J Obstet Gynecol 2003;188:1202-4.)
Key words: Contraception, postpartum, patient satisfaction
Volume 188, Number 5 Johnson, Edelman, and Jensen 1203
Am J Obstet Gynecol
pleting an anonymous self-administered questionnaire.
After the baseline collection of data during April, a stan-
dardized, comprehensive information booklet about con-
traceptive options in English and Spanish was given out
to all parturients on the postpartum unit during May. All
subjects during both months completed identical ques-
tionnaires. Basic demographic information was obtained
from each patient. Satisfaction of antenatal and postpar-
tum contraceptive counseling was assessed with a 100-mm
visual analog scale (most satisfied, 0 mm; dissatisfied, 100
mm). Patients reported the type of counseling received
(whether verbal and/or written) and how much the
counseling contributed to their ultimate choice of con-
traceptive.
The primary outcome was whether written informa-
tion better enabled patients to reach decisions about
contraceptive options. The visual analog scale scores
were analyzed with the use of the t test. Categoric and
ordinal data were analyzed with the
2
test and Mann-
Whitney U test. All comparisons were performed on a
desktop computer running SPSS (version 9.0; SPSS Inc,
Chicago, Ill) for Windows (Microsoft Corporation, Red-
mond, Wash).
Results
There were a total of 198 and 203 deliveries during the
baseline and intervention collection periods, respectively.
A total of 109 (27.1%) women participated, 53 women
(27%) in the baseline group and 56 women (27.6%) in
the intervention group. There were no significant differ-
ences in the baseline characteristics of the two groups.
The average age was 25.9 (SD) 6.23 years in the baseline
group and 25.3 6.68 years in the intervention group (P
= .646). Approximately 45% of the women in both groups
were Hispanic (P = .661); the median education level was
equal (high school, some college; P = .287).
Forty-two women (79.2%) in the baseline group and
46 women (82.1%) in the intervention group stated that
they received contraceptive counseling by their health
care providers during their prenatal care (P = .701).
Mean satisfaction of prenatal counseling in the baseline
group was 2.45 cm and 2.72 cm in the intervention
group (P = .654). Thirty-seven women (69.8%) in the
baseline group and 38 women (67.9%) in the interven-
tion group reported postpartum contraceptive counsel-
ing by a health care provider (P = .825). Patient
satisfaction with postpartum counseling was 3.24 cm in
the baseline group and 2.48 cm in the intervention
group (P = 2.6). Only 18 women (34%) in the baseline
group reported having received any written information
during their postpartum hospitalization compared with
56 women (100%) of the intervention group (P < .01).
Among those women who reported the receipt of written
information, women in the intervention group were
more likely to state that this information helped con-
tribute to their ultimate choice in birth control (1.16 vs
4.02 women, P < .01).
Comment
We conceived this project to address the hypothesis that
increasing a patients knowledge of contraception could
increase the patients satisfaction with postpartum contra-
ceptive decision making. Although the ultimate aim of
this intervention is to decrease the incidence of unin-
tended pregnancies, this exact outcome was not studied.
However, our results indicate that the provision of high-
quality, standardized information to women improves the
satisfaction with counseling. This, in turn, may translate
to improved satisfaction with contraceptive choice.
Although antenatal contraceptive counseling is impor-
tant, readdressing the issue with patients in the postpar-
tum setting remains essential. In 2000, researchers at
Wayne State University examined contraceptive decision
making among a population of low-income pregnant
women in Detroit.
3
They discovered that women were not
using the method of contraception consistently that they
planned to use in the prenatal period. Although antena-
tal counseling is imperative, readdressing the issue in the
postpartum period may help to reinforce a decision re-
garding birth control and improve patient satisfaction
and continuation rates.
An evaluation of verbal postpartum counseling was per-
formed in Scotland in 1996.
4
Eight-four percent of the
women reported having a discussion regarding contra-
ception while in the postpartum unit. Fifty percent of
these women, however, had a negative opinion of the
conversation. The most common complaint was that the
discussion was given as a necessary routine undertaken
with reluctance by the physician and that only 50% of the
population was discharged with a method of contracep-
tion. Researchers from this study concluded that the post-
partum unit was not the appropriate setting for
contraceptive counseling, but no other intervention was
evaluated. Many patients may feel, in fact, that these post-
partum conversations are not adequate and that they may
need additional time or information to make a decision.
In 1999, a study in Finland examined the relative im-
portance of various sources of contraceptive informa-
tion.
2
Both women and men were asked to rate their
knowledge of contraceptive methods and from what in-
formation source this information had been obtained.
Both sexes stated that most of their contraceptive knowl-
edge came from written literature rather than from physi-
cian contact. This outcome was surprising, given that this
population (unlike the United States) has excellent ac-
cess to health care.
Both the content and quality of counseling can vary be-
tween providers, and it is difficult to control a patients
perceptions and understanding of the interaction. The
postpartum period can be a difficult time to undertake
1204 Johnson, Edelman, and Jensen May 2003
Am J Obstet Gynecol
what should be considered an important conversation. Pa-
tients are fatigued and often distracted, and physicians
may be rushed and not able to take the time needed to an-
swer a multitude of questions. Most patients who are de-
livered at our university hospital site receive prenatal care
from a variety of practitioners at surrounding satellite clin-
ics. Therefore, it is difficult to assess the amount and the
quality of the information that they receive during the an-
tepartum period. In the same vein, it is difficult for us to
control the counseling that these women receive while
they are hospitalized after the delivery. The cases are fol-
lowed by a variety of providers that include students, resi-
dents, midwives, and attending physicians. Without
having 1 person see all of these patients for study pur-
poses, it is impossible to control this variable. However, in
our study population, both groups of patients reported
similar exposure to and satisfaction with the counseling
that they received, both before and after the delivery.
We chose to focus on providing patients with concise,
comprehensive written information that they can review
at their own pace and narrow down the options that may
be right for them. One problem we have faced consis-
tently is the lack of written information that is available
on the postpartum unit. Although individual brochures
have been used occasionally, never has there been an ad-
equate source of comprehensive written information. By
creating and distributing such a resource, this variable
was easier to control. As we hypothesized, our patients re-
ported a much higher level of satisfaction with this source
of information and an increased ability to make an in-
formed decision about their choice of birth control.
Limitations of the study include the lack of a direct com-
parison between individual counseling methods by a
provider and written information. By focusing on written
information, we intended to study a practical strategy that
was designed to overcome the limitations of multiple
providers at different training levels in the dissemination of
contraceptive counseling at discharge. Although patients
generally reported being satisfied overall with their antena-
tal and postpartum counseling, the value of this counseling
compared with written information was not evaluated. Al-
though satisfaction with contraceptive counseling im-
proved among subjects in the intervention group, the
impact on compliance with the chosen method of birth
control and the subsequent rate of unintended pregnancy
were beyond the scope of this investigation. However, the
positive findings in this study may prove to be a valuable
starting point for further studies of the subject.
REFERENCES
1. Henshaw S. Unintended pregnancy in the United States. Fam
Plann Perspect 1998;30:24-46.
2. Virjo I, Kirkkola AL, Isokoski M, Mattila K. Contraceptive meth-
ods: knowledge sources rated by women and men. Contracep-
tion 1999;59:257-63.
3. Miller VL, Laken MA, Ager J, Essenmacher L. Contraceptive de-
cision making among Medicaid-eligible women. J Commun
Health 2000;25:473-80.
4. Glasier AF, Logan J, McGlew TJ. Who gives advice about post-
partum contraception? Contraception 1996;53:217-20.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Parthasarathy2013 PDFDocument7 pagesParthasarathy2013 PDFAndi BintangNo ratings yet
- Sacral Nerve Stimulation Reduces Elevated Urinary Nerve Growth Factor Levels in Women With Symptomatic Detrusor OveractivityDocument5 pagesSacral Nerve Stimulation Reduces Elevated Urinary Nerve Growth Factor Levels in Women With Symptomatic Detrusor OveractivityAndi BintangNo ratings yet
- Medical Hypotheses: Yixian Li, Juan Zhou, Ian Burkovskiy, Pollen Yeung, Christian Lehmann TDocument3 pagesMedical Hypotheses: Yixian Li, Juan Zhou, Ian Burkovskiy, Pollen Yeung, Christian Lehmann TAndi BintangNo ratings yet
- Subarachnoid Block For Caesarean Section in Severe PreeclampsiaDocument6 pagesSubarachnoid Block For Caesarean Section in Severe PreeclampsiaAndi BintangNo ratings yet
- 1 s2.0 S0002937800704534 Main PDFDocument1 page1 s2.0 S0002937800704534 Main PDFAndi BintangNo ratings yet
- Depresión e InmunidadDocument13 pagesDepresión e InmunidadgabisaenaNo ratings yet
- Bar A Zanchi 2018Document17 pagesBar A Zanchi 2018Andi BintangNo ratings yet
- Anestesia General para Césarea PDFDocument7 pagesAnestesia General para Césarea PDFAgnese ValentiniNo ratings yet
- Anestesia General para Césarea PDFDocument7 pagesAnestesia General para Césarea PDFAgnese ValentiniNo ratings yet
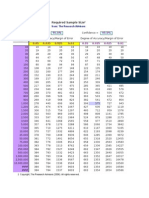
- Required Sample Size: From: The Research AdvisorsDocument3 pagesRequired Sample Size: From: The Research AdvisorsAbhishek Sharma100% (1)
- Procalcitonin As A Biomarker of Severity Degree in Sepsis Due To PneumoniaDocument5 pagesProcalcitonin As A Biomarker of Severity Degree in Sepsis Due To PneumoniaAndi BintangNo ratings yet
- 2013 Student Membership ApplicationDocument1 page2013 Student Membership ApplicationAndi BintangNo ratings yet
- Cultural Sociology of Mental Illness n28Document5 pagesCultural Sociology of Mental Illness n28Andi BintangNo ratings yet
- Overweight linked to increased risk of lower back painDocument8 pagesOverweight linked to increased risk of lower back painAndi BintangNo ratings yet
- Instruction For Author ClimactericDocument9 pagesInstruction For Author ClimactericAndi BintangNo ratings yet
- 1 s2.0 S1052305714000561 MainDocument6 pages1 s2.0 S1052305714000561 MainAndi BintangNo ratings yet
- 1 s2.0 S0021755713002003 MainDocument6 pages1 s2.0 S0021755713002003 MainAndi BintangNo ratings yet
- Association Between Constipation and Colorectal Cancer Systematic Review and Meta-Analysis of Observational StusdgdiesDocument10 pagesAssociation Between Constipation and Colorectal Cancer Systematic Review and Meta-Analysis of Observational StusdgdiesAndi BintangNo ratings yet
- Hepatitis C APASLfghDocument27 pagesHepatitis C APASLfghAndi BintangNo ratings yet
- 1 s2.0 S0021755713002003 MainDocument6 pages1 s2.0 S0021755713002003 MainAndi BintangNo ratings yet
- 1 s2.0 S0002937803001388 MainDocument3 pages1 s2.0 S0002937803001388 MainAndi BintangNo ratings yet
- Prevalence of Diabetes and Impaired Fasting Glucose in Adults in The U.S. PopulationDocument6 pagesPrevalence of Diabetes and Impaired Fasting Glucose in Adults in The U.S. PopulationAndi BintangNo ratings yet
- Anthropometry: Ergonomics Additional ResourcesDocument5 pagesAnthropometry: Ergonomics Additional ResourcesAndi BintangNo ratings yet
- Urologi PDFDocument237 pagesUrologi PDFAndi BintangNo ratings yet
- Serviks DocjhjuDocument366 pagesServiks DocjhjuAndi BintangNo ratings yet
- MK Giz Slide Infant Feeding PracticeDocument1 pageMK Giz Slide Infant Feeding PracticeAndi BintangNo ratings yet
- PCT CAP ABiuytoDocument10 pagesPCT CAP ABiuytoAndi BintangNo ratings yet
- Cap Bts 2009 ComplitdgDocument139 pagesCap Bts 2009 ComplitdgAndi BintangNo ratings yet
- ATS Guidelines CAP ManagementDocument25 pagesATS Guidelines CAP ManagementMae Matira AbeladorNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- People Vs MadridDocument5 pagesPeople Vs MadridEunice SerneoNo ratings yet
- People v. EnriquezDocument2 pagesPeople v. EnriquezChris Erwin AlquizalasNo ratings yet
- Stradec v. SidcDocument2 pagesStradec v. SidcFrancis Jan Ax ValerioNo ratings yet
- Palaganas Vs PalaganasDocument3 pagesPalaganas Vs PalaganasLucas Gabriel JohnsonNo ratings yet
- SampleDocument64 pagesSampleJunliegh permisonNo ratings yet
- FIFA World Cup Milestones, Facts & FiguresDocument25 pagesFIFA World Cup Milestones, Facts & FiguresAleks VNo ratings yet
- Boulder District Attorneys Office Letter To Kathleen ChippiDocument1 pageBoulder District Attorneys Office Letter To Kathleen ChippiMichael_Lee_RobertsNo ratings yet
- Suffer in Silence A Novel of Navy SEAL TrainingDocument13 pagesSuffer in Silence A Novel of Navy SEAL TrainingMacmillan Publishers100% (1)
- Check Encumberance Certificate To Verify Property TitleDocument2 pagesCheck Encumberance Certificate To Verify Property TitlePVV RAMA RAONo ratings yet
- Dumaual - Crim Rev DigestsDocument18 pagesDumaual - Crim Rev DigestsJanjan DumaualNo ratings yet
- Forensic Examination Report - Kevin SplittgerberDocument16 pagesForensic Examination Report - Kevin Splittgerberapi-546415174No ratings yet
- IHL 1 BALLB ProjectDocument16 pagesIHL 1 BALLB Projectabcde fghikjNo ratings yet
- Research Proposal Sex Addiction FinalDocument14 pagesResearch Proposal Sex Addiction Finalapi-296203840100% (1)
- SCOUT OATH EXPLAINEDDocument8 pagesSCOUT OATH EXPLAINEDpiperNo ratings yet
- Strategies for Ending the Sino-Japanese and Russo-Japanese WarsDocument18 pagesStrategies for Ending the Sino-Japanese and Russo-Japanese Warscoca COLANo ratings yet
- MODULE 5 - Rizal PDFDocument12 pagesMODULE 5 - Rizal PDFKyle CuiNo ratings yet
- Supreme Court upholds dismissal of worker for serious misconductDocument2 pagesSupreme Court upholds dismissal of worker for serious misconductJoseNo ratings yet
- Esseye Medhin - 2002 - Addis Ababa Art Scene RevisitedDocument10 pagesEsseye Medhin - 2002 - Addis Ababa Art Scene RevisitedBirukyeNo ratings yet
- Sy Vs Judge DinopolDocument2 pagesSy Vs Judge DinopolMarianne Domingo100% (1)
- Judicial Clemency GuidelinesDocument13 pagesJudicial Clemency GuidelinesMunchie MichieNo ratings yet
- Special Marriage Act provisions for interfaith unionsDocument28 pagesSpecial Marriage Act provisions for interfaith unionsVed AntNo ratings yet
- Valencia V CADocument10 pagesValencia V CApjNo ratings yet
- People v Rafael Conviction Upheld for Frustrated Murder and MurderDocument35 pagesPeople v Rafael Conviction Upheld for Frustrated Murder and MurderNigel AlinsugNo ratings yet
- Boarding PassDocument2 pagesBoarding PassRupèsh GundechäNo ratings yet
- Municipal Ordinance No. 2015-01: Office of The Sangguniang BayanDocument4 pagesMunicipal Ordinance No. 2015-01: Office of The Sangguniang BayanEden Celestino Sarabia CachoNo ratings yet
- Geodesign BH Sos BrasilandiaDocument22 pagesGeodesign BH Sos BrasilandiaAdriana SandreNo ratings yet
- Resolution For AppointmentDocument3 pagesResolution For Appointmentjerome geoligaoNo ratings yet
- Status of Children in Conflict With The Law in La Trinidad 1325749101Document6 pagesStatus of Children in Conflict With The Law in La Trinidad 1325749101Jan Igor GalinatoNo ratings yet
- Ship Stability Notes BS222Document74 pagesShip Stability Notes BS222Ahmed Aboelmagd100% (1)
- Freedom of Information ActsDocument22 pagesFreedom of Information ActsSarah_GadNo ratings yet