Professional Documents
Culture Documents
Negative Pressure Therapy (Vacuum) For Wound Bed Preparation Among Diabetic Patients: Case Series
Uploaded by
Caroline AlmeidaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Negative Pressure Therapy (Vacuum) For Wound Bed Preparation Among Diabetic Patients: Case Series
Uploaded by
Caroline AlmeidaCopyright:
Available Formats
Case series
Negative pressure therapy (vacuum) for wound bed
preparation among diabetic patients: case series
Terapia por presso negativa (vcuo) no preparo do leito da ferida
em pacientes diabticos: srie de casos
Marcus Castro Ferreira1, Viviane Fernandes de Carvalho2, Fbio Kamamoto3, Paulo Tuma Junior4, Andr Oliveira Paggiaro5
Plastic Surgery Division, Faculdade de Medicina da Universidade de So Paulo (FMUSP), So Paulo, Brazil
ABSTRACT
KEY WORDS:
Diabetic foot.
Skin transplantation
Surgical flaps.
Negative-pressure wound therapy.
Wound healing.
CONTEXT: Complications from diabetes mellitus affecting the lower limbs occur in 40 to 70% of such patients. Neuropathy is the main cause of ulceration
and may be associated with vascular impairment. The wound evolves with necrosis and infection, and if not properly treated, amputation may be the end
result. Surgical treatment is preferred in complex wounds without spontaneous healing. After debridement of the necrotic tissue, the wound bed needs to
be prepared to receive a transplant of either a graft or a flap. Dressings can be used to prepare the wound bed, but this usually leads to longer duration
of hospitalization. Negative pressure using a vacuum system has been proposed for speeding up the treatment. This paper had the objective of analyzing
the effects of this therapy on wound bed preparation among diabetic patients.
CASE SERIES: Eighty-four diabetic patients with wounds in their lower limbs were studied. A commercially available vacuum system was used for all
patients after adequate debridement of necrotic tissues. For 65 patients, skin grafts completed the treatment and for the other 19, skin flaps were used.
Wound bed preparation was achieved over an average time of 7.51 days for 65 patients and 10 days for 12 patients, and in only one case was not
achieved.
CONCLUSIONS: This experience suggests that negative pressure therapy may have an important role in wound bed preparation and as part of the
treatment for wounds in the lower limbs of diabetic patients.
PALAVRAS-CHAVE:
P diabtico.
Transplante de pele
Retalhos cirrgicos.
Tratamento de ferimentos com
presso negativa.
Cicatrizao de feridas.
RESUMO
CONTEXTO: Complicaes do diabetes mellitus que afetam os membros inferiores ocorrem em 40 a 70% dos pacientes. A neuropatia a principal
causa de ulcerao e pode estar associada com problemas vasculares. A ferida evolui com necrose e infeco, e se no for corretamente tratada
poder terminar em amputao. O tratamento cirrgico preferido em feridas complexas, quando no h cicatrizao espontnea. Aps desbridamento
cirrgico do tecido necrtico do leito da ferida este precisa ser preparado para receber um transplante, seja um enxerto ou um retalho. Curativos podem
ser usados para o preparo do leito da ferida, mas frequentemente levam a um longo tempo de hospitalizao. A presso negativa usada atravs de um
sistema vcuo foi proposta para acelerar o tempo de tratamento. O presente trabalho teve como finalidade analisar os efeitos desta terapia no preparo
do leito de feridas em pacientes diabticos.
SRIE DE CASOS: Oitenta e quatro pacientes diabticos com feridas em membros inferiores foram estudados. Um sistema vcuo de uso comercial foi
utilizado em todos os pacientes aps adequado desbridamento de tecidos necrticos. Em 65 pacientes enxertos de pele completaram o tratamento e
em outros 19 retalhos cutneos. O preparo do leito da ferida foi conseguido, em mdia, em 7,51 dias em 65 pacientes, em 10 dias para 12 pacientes
e em somente um caso no foi efetivo.
CONCLUSO: A experincia sugere que a terapia por presso negativa possa ter um papel importante no preparo do leito e como parte do tratamento
de feridas nos membros inferiores de pacientes diabticos.
MD, PhD. Full professor and chairman, Plastic Surgery Division, Faculdade de Medicina da Universidade de So Paulo (FMUSP), So Paulo, Brazil.
PhD. Attending physician at Hospital das Clnicas, Faculdade de Medicina da Universidade de So Paulo (FMUSP), So Paulo, Brazil.
3
MD, MSc. Attending physician at Hospital Universitrio, Faculdade de Medicina da Universidade de So Paulo (HC/FMUSP), So Paulo, Brazil.
4
MD, PhD. Attending plastic surgeon at Hospital das Clnicas, Faculdade de Medicina da Universidade de So Paulo (HC/FMUSP), So Paulo, Brazil.
5
MD. Medical preceptor, Plastic Surgery Division, Faculdade de Medicina da Universidade de So Paulo (FMUSP), So Paulo, Brazil.
1
2
166
Sao Paulo Med J. 2009; 127(3):166-70
Negative pressure therapy (vacuum) for wound bed preparation among diabetic patients: case series
INTRODUCTION
CASE SERIES
Diabetes mellitus is a chronic multifactorial disease. The worldwide
prevalence was 120 million cases in 1996 but the prediction for 2025 is
for 250 million cases, because of longer life expectancy, greater obesity
and greater sedentarism.1 In Brazil, it has been estimated that around
10million people are diabetic.2
The complications from this disease are serious and those affecting
the lower limbs represent 40% to 70% of these patients.3 Such patients
usually present lesions on their lower limbs that do not heal primarily.
Although simply controlling blood glucose levels is important, this is
not necessarily followed by healing of these ulcers.4 The wounds may
evolve with extensive necrosis and infection, which may lead to amputation of parts of or even the whole limb.5,6
Obstruction of major blood vessels is responsible for less than 20%
of these wounds.7 The main cause recognized today is neuropathy, consisting of progressive degeneration of sensitive nerves in the foot, induced by microangiopathy of the small vessels to the nerve fascicles.
This is sometimes associated with external compression at anatomical
sites, such as the tarsal tunnel.8-10 Small traumas suffered by feet that
have abnormal (decreased) sensation can cause ulcerations that do not
heal primarily.11
Such wounds are considered to be complex and are best treated surgically, including debridement of necrotic tissues. This provides preparation for the wound bed, for subsequent skin replacement by means of
skin grafts or flaps.12
The concept of wound bed preparation was introduced in 2002 by
Schultz et al.13 The aim was to create favorable conditions that would
speed up the endogenous cure of the wound. More recently, wound bed
preparation has been used to improve the acceptance of skin grafts.12
The preparation includes controlling the microorganisms, reducing the
exudate volume and stimulating the granulation tissue.14
Nonetheless, in many complex wounds, the conventional dressings that are used to prepare the wound bed still take a long time to
achieve ideal conditions. Some alternatives have been tried out over the
last 10years.15
The use of negative pressure was proposed by Argenta et al.16 and
Morykwas et al.17 in 1997. This consisted of developing a mechanical
system (vacuum-assisted closure) to help the healing process. Negative
pressure is created by a machine that is connected by a plastic tube to a
sponge placed over the wound bed. The pressure is adjusted to between
-50 and -125 mmHg, continuously or intermittently. The wound bed
should be completely covered by the sponge, thus creating an environment under vacuum when the machine is switched on.
We introduced this method to Hospital das Clnicas, Faculdade de
Medicina da Universidade de So Paulo (HCFMUSP) in 2002, to treat
complex wounds. An initial paper reported three cases of wounds for
which the vacuum system was used.18 A more extensive report on our
clinical experience with the vacuum system, mostly on pressure sores,
was presented by our group in 2006.19
The purpose of the present paper is to present a series of 84 cases
of negative pressure therapy on lower-limb wounds among diabetic
patients.
Eight-four diabetic patients with a single complex wound on one
lower limb were treated using negative pressure (vacuum system) at the
Plastic Surgery Division of HCFMUSP, between 2004 and 2006.
All the patients were informed about the proposed treatment and
consented to the use of this treatment. This study was approved by the
Ethics Committee of HCFMUSP.
The patients were first seen by the vascular surgery service or were
referred by their primary physician for a consultation with our complex
wound group of the Plastic Surgery Division. All the patients underwent
Doppler examination regarding the vascular status of their legs and were
considered satisfactory. There was no indication for revascularization or
amputation of the limb in any case. The patients diabetes status was
controlled by their primary physician and was not part of this study.
In most cases, the ulcer had been present for a time of between two
and three months. It had been treated by means of conventional dressings alone, while awaiting spontaneous closure.
Surgical debridement was usually indicated, if needed, and any necrotic tissue was removed as soon as possible, as dictated by the patients general condition. After removal of the necrosis, a less-than-ideal
wound bed was almost always revealed. The quality of the wound bed
was assessed in terms of the poor vascularity, gross inflammatory reaction or signs of infection that left doubts regarding whether the take
of the skin graft would be assured.
The vacuum system (V.A.C. Vacuum Assisted Closure, KCI Inc.,
San Antonio, Texas, USA) was then installed. The sponge was placed directly on the wound, and the connections with the machine enableda
pressure of minus 125 mmHg. Sponge shrinkage within the sealed environment indicated that the machine was effective. The sponge was
changed every 72 hours, and the condition of the wound bed was reassessed at that time.
The wound bed was considered prepared, i.e. ready for surgical closure (mostly by means of a meshed skin graft, but sometimes by flaps),
when the volume of exudate was less than 20 ml/day, no signs of infectious process were seen around the wound and healthy granulation tissue could be observed over at least 75% of the wound surface. The time
elapsed between installation of the vacuum machine at the first consultation and the reconstruction (wound preparation) was recorded, along
with the outcome after the plastic surgery.
Skin grafts were indicated as the first choice for diabetic ulcers. Local flaps were used on smaller wounds or when specialized structures
like tendons or bones were exposed and needed a thicker composite tissue. In some special indications, a microvascular muscle-free flap had to
be transferred.
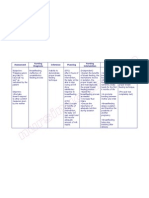
For 65 (77.3%) of the patients, the mean time taken to prepare the
wound was 7.51 1.87 days. For another 12 patients (14.2%), it was
10.87 1.48 days and for one patient (1.3%), the negative pressure therapy was not efficient for improving the quality of the wound bed. For six
patients (7.14%), the wound closed in nine days without the need for
surgical reconstruction: only the vacuum system was used (Figure 1).
For 49 patients (58.4%), the wound was successfully closed by
means of partial-thickness skin grafts taken from the thigh area. Most
Sao Paulo Med J. 2009; 127(3):166-70
167
Ferreira MC, Carvalho VF, Kamamoto F, Tuma Junior P, Paggiaro AO
of the grafts were meshed (using a mesh graft machine) (Zimmer Inc.,
Dover, Ohio, USA) and the vacuum system was applied over the graft,
in order to enhance the integration of the skin grafting (Figure 2).
For 28 patients (33.4%), skin or muscle-skin flaps were the method
chosen for closing the wound, usually because there was some exposed
structure (bone or tendon) that would be better treated by flap coverage.
Nineteen (22.6%) cases presented a satisfactory outcome, with no
necrosis or dehiscence of the flap, and nine (10.7%) presented small necrotic areas that healed after some short delay (Figure 3). No complications relating to the use of the vacuum device were observed.
DISCUSSION
For proper resolution of any chronic wound, a logical sequence of
events should be followed in order to transform the wound bed into a
1 Non Response
6 Spontaneously
closed
84 Patients
49 Skin Grafts
17 Local Flaps
28 Flaps
11 Free Flaps
Figure 1. Distribution of the patients according to the treatment chosen.
healthier condition and then achieve healing. This may take place using intrinsic mechanisms alone, or it may be helped by autogenous tissue transplantation, skin grafts or flaps. These sequential events consistof debridement (removal of necrotic tissue), edema control, reduction ofexudate, reduction of the bacteria count and increasing the numbersof blood vessels, with correspondingly better granulation tissue.13
The negative pressure action elicited by the vacuum system has
been associated with controlling the exudate, reducing the bacterial
population and stimulating the formation of granulation tissue since
the first patient with a complex wound was treated by Argenta et al.,16
16yearsago.
These effects were clearly demonstrated in the present series. They
led to improvements in the treatment of the diabetic ulcer, over a shorter time. Although we did not conduct any comparisons with controls, it
is well known from practical experience of any surgery procedure that,
with conventional dressings, much more time is needed to prepare a
wound bed. Furthermore, although we did not investigate the costs, the
reduction in the time taken to close the wound will have had a positive
impact regarding reduction of the cost of the treatment.
The mechanism through which the negative pressure achieved the
increase in the blood vessel count, i.e. an angiogenic effect, is not completely clear yet. The vacuum system promotes the removal of excessive fluids in the wound, thus reducing the bacterial population and
the edema. There is consequently an improvement in the blood flow
to the area, thereby leading to better-quality granulation tissue.20,21 The
mechanical force applied to the wound bed by the vacuum may explain the cell proliferation, since this would act as a physical substitute
for the normal extracellular matrix. This is important for restarting the
proliferation phase of wound healing.22,23 Another possible explanation
3;6%
17;35%
29;59%
Total
Partial (75 to 100%)
Partial (50 to 75%)
Figure 2. Results from skin grafts. A Results from patients undergoing skin graft surgery. B - Wound on dorsum of foot before surgical debridement. C Wound after surgical debridement. D - Wound after seven days of negative pressure therapy. E - Wound after skin grafting.
168
Sao Paulo Med J. 2009; 127(3):166-70
Negative pressure therapy (vacuum) for wound bed preparation among diabetic patients: case series
2;7%
7;5%
19;68%
Satisfactory
Slight necrosis
New surgery
Figure 3. Results from treatment with flaps. A - Distribution of patients undergoing skin flap surgery. B - Wound on foot before surgical debridement. C
Appearance of the wound after first debridement and seven days of negative pressure therapy. Amputation of the necrotic toes was indicated. D - Wound
located on the sole of the same diabetic patient after second surgical debridement and amputation of the toes. The heads of the metatarsal bones can be
seen. E Anterolateral microsurgical flap from thigh. F Result after six months of defatting of the flap.
for the action of the vacuum system could be that it removes proteolytic enzymes, especially the metalloproteinases and cytokines in the
exudate. These enzymes degrade the extracellular matrix and prevent
wound resolution.24
In an experimental study on pigs, Morykwas et al.17 showed that the
blood flow around the wound increased gradually with each elevation
of 25 mmHg of vacuum applied to the wound. The improved blood
flow was optimized at -125 mmHg. On the other hand, when the vacuum was greater than -400 mmHg, the blood flow fell back to below
the baseline.
The vacuum system has also been shown to enhance the quality of
the granulation tissue in the wound. Granulation tissue is a mixture
ofblood vessels and connective tissue and it plays an essential role in
cell growth in the wound and thus in its closure. It is considered, clinically, to have a good appearance when it presents a bright red color, a
beefy appearance.
In the same experimental study,17 two groups of wounds were compared: one using the vacuum system and the other covered by saline
dressings alone. It was observed that there was a significantly higher
growth rate for the granulation tissue in the vacuum group. Moreover,
intermittent negative pressure at -125 mmHg seemed to be more efficient than continuous application was. Chen et al.25 showed experimentally that negative pressure caused an increase in the number of capillary blood vessels that sprouted, as measured by biopsies and compared
with controls.
This angiogenic effect from negative pressure therapy seems to be a
very important factor in reducing the time needed for wound bed preparation and thus for the wound to be able to receive and integrate skin
grafts. In cases of diabetic foot ulcer, as observed in the present series,
this effect will correspond to a reduction in the duration of hospitalization and the need for antibiotics.
The decrease in the bacterial population, down to under the level of
105 colonies in the tissue cultures, will have been important not only
because it reduced the expenditure on antibiotics, but also because it enhanced the oxygen and nutrient levels. These are important as healing
mechanisms and would have been diverted for the needs of the bacteria. So far, no consensus has been reached regarding the role of negative
pressure therapy on bacteria clearance from the wound, although Morykwas et al.17 showed that there was a decrease in bacterial counts in the
vacuum group, compared with controls.
In our hospital, quantitative counting of tissue bacteria is not done
routinely and for this reason, we cannot affirm that the vacuum therapy
applied to the wound had the effect of decreasing the bacterial count.
Nonetheless, the clinical appearance of the wound, the quality of the
exudate and even the smell of the wound pointed towards diminished
colonization among most of the diabetic patients that we treated.
The low percentage of skin graft losses also points towards this effect
of infection control in the wound. It is well known that skin grafts do
not incorporate when the wound is massively infected.26 In most cases
here, antibiotics were not prescribed during the vacuum system treatment, which usually lasted for one to two weeks.
Contraction of the wound bed was observed. It is well known that
this is one the natural mechanisms of reduction of the size of the wound
and promotion of primary healing. In our series, contraction was not
important because we performed operations on our patients and covered the wounds with grafts or flaps, with the exception of six cases.
Sao Paulo Med J. 2009; 127(3):166-70
169
Ferreira MC, Carvalho VF, Kamamoto F, Tuma Junior P, Paggiaro AO
The negative effect of wound contraction was prevented by the tissue
transfer.
Our previous clinical experience with the treatment of diabetic ulcers has shown that, if clinical dressings alone are used, it has to
be expected that a long time will be required (usually more than two
months) for the wound bed to reaches a good condition for accepting
skin grafts.
CONCLUSIONS
In this series of patients, we observed that negative pressure therapy had a positive effect on the treatment of complex wounds among
diabetics. It enabled wound bed preparation in only a short time, and
allowed us to successfully close the wound using skin transplants. It is
possible that the duration of hospitalization and the overall treatment
time might be shorter than with conventional dressing, but further randomized clinical trials are still needed to confirm this hypothesis.
REFERENCES
1.
Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the
year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047-53.
2. Malerbi DA, Franco LJ. Multicenter study of the prevalence of diabetes mellitus and impaired
glucose tolerance in the urban Brazilian population aged 30-69 yr. The Brazilian Cooperative
Group on the Study of Diabetes Prevalence. Diabetes Care. 1992; 15(11):1509-16.
3. Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA.
2005;293(2):217-28.
4. Jeffcoate WJ, Price P, Harding KG; International Working Group on Wound Healing and Treatments for People with Diabetic Foot Ulcers. Wound healing and treatments for people with
diabetic foot ulcers. Diabetes Metab Res Rev. 2004;20(Suppl 1):S78-89.
5. Armstrong DG, Lipsky BA. Diabetic foot infections: stepwise medical and surgical management. Int Wound J. 2004;1(2):123-32.
6. Miyajima S, Shirai A, Yamamoto S, Okada N, Matsushita T. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006;71(3):272-9.
7. Abbott CA, Carrington AL, Ashe H, et al. The North-West Diabetes Foot Care Study: incidence
of, and risk factors for, new diabetic foot ulceration in a community-based patient cohort.
Diabet Med. 2002;19(5):377-84.
8. Dellon AL. From there to here: a personal viewpoint after three decades of neuropathy
research. Clin Podiatr Med Surg. 2006;23(3):497-508.
9. Valdivia JM, Dellon AL, Weinand ME, Maloney CT Jr. Surgical treatment of peripheral
neuropathy: outcomes from 100 consecutive decompressions. J Am Podiatr Med Assoc.
2005;95(5):451-4.
10. Aszmann O, Tassler PL, Dellon AL. Changing the natural history of diabetic neuropathy: incidence of ulcer/amputation in the contralateral limb of patients with a unilateral nerve
decompression procedure. Ann Plast Surg. 2004;53(6):517-22.
11. Mayfield JA, Reiber GE, Sanders LJ, Janisse D, Pogach LM; American Diabetes Association.
170
Sao Paulo Med J. 2009; 127(3):166-70
Preventive foot care in diabetes. Diabetes Care. 2004;27(Suppl 1):S63-4.
12. Ferreira MC, Tuma P Jr, Carvalho VF, Kamamoto F. Complex wounds. Clinics (Sao Paulo).
2006;61(6):571-8.
13. Schultz GS, Sibbald RG, Falanga V, et al. Wound bed preparation: a systematic approach to
wound management. Wound Repair Regen. 2003;11(Suppl 1):S1-28.
14. Sibbald RG, Orsted H, Schultz GS, Coutts P, Keast D; International Wound Bed Preparation
Advisory Board; Canadian Chronic Wound Advisory Board. Preparing the wound bed 2003:
focus on infection and inflammation. Ostomy Wound Manage. 2003;49(11):23-51.
15. Falanga V. Wound healing and its impairment in the diabetic foot. Lancet. 2005;
366(9498):1736-43.
16. Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and
treatment: clinical experience. Ann Plast Surg. 1997;38(6):563-76; discussion 577.
17. Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new
method for wound control and treatment: animal studies and basic foundation. Ann Plast
Surg. 1997;38(6):553-62.
18. Ferreira MC, Wada A, Tuma Jnior P. The vacuum assisted closure of complex wounds: report
of 3 cases. Rev Hosp Clin Fac Med Univ So Paulo. 2003;58(4):227-30.
19. Wada A, Ferreira MC, Tuma Jnior P, Arruntegui G. Experience with local negative
pressure (vacuum method) in the treatment of complex wounds. Sao Paulo Med J.
2006;124(3):150-3.
20. DeFranzo AJ, Marks MW, Argenta LC, Genecov DG. Vacuum-assisted closure for the treatment
of degloving injuries. Plast reconstr surg. 1999;104(7):2145-8.
21. Lambert KV, Hayes P, McCarthy M. Vacuum assisted closure: a review of development and
current applications. Eur J Vasc Endovasc Surg. 2005;29(3):219-26.
22. Saxena V, Hwang CW, Huang S, Eichbaum Q, Ingber D, Orgill DP. Vacuum-assisted closure: microdeformations of wounds and cell proliferation. Plast Reconstr Surg. 2004;114(5):108696; discussion 1097-8.
23. Chen KD, Li YS, Kim M, et al. Mechanotransduction in response to shear stress. Roles of
receptor tyrosine kinases, integrins, and Shc. J Biol Chem. 1999;274(26):18393-400.
24. Yager DR, Nwomeh BC. The proteolytic environment of chronic wounds. Wound Repair Regen.
1999;7(6):433-41.
25. Chen SZ, Li J, Li XY, Xu LS. Effects of vacuum-assisted closure on wound microcirculation: an
experimental study. Asian J Surg. 2005;28(3):211-7.
26. Krizek TJ, Robson MC. Evolution of quantitative bacteriology in wound management. Am J
Surg. 1975;130(5):579-84.
Sources of funding: None
Conflict of interest: None
Date of first submission: June 11, 2007
Last received: July 2, 2009
Accepted: July 13, 2009
Address for correspondence:
Marcus Castro Ferreira
Rua Barata Ribeiro, 483 Conj. 161 e 162
Bela Vista So Paulo (SP) Brasil
CEP 01308-000
Tel. (+55 11) 3256-4899
E-mail: mferrei@uol.com.br
E-mail: mcferrei@usp.br
You might also like
- Cirurgia OrtognáticaDocument8 pagesCirurgia OrtognáticaCaroline AlmeidaNo ratings yet
- Cressey Et Al-2017-Contact DermatitisDocument7 pagesCressey Et Al-2017-Contact DermatitisCaroline AlmeidaNo ratings yet
- Miller 2013Document1 pageMiller 2013Caroline AlmeidaNo ratings yet
- 334 V 33 N 04 A 90320965 PDF 001Document11 pages334 V 33 N 04 A 90320965 PDF 001Caroline AlmeidaNo ratings yet
- BRASIL 2-OkDocument10 pagesBRASIL 2-OkCaroline AlmeidaNo ratings yet
- A 10 V 1273Document5 pagesA 10 V 1273Caroline AlmeidaNo ratings yet
- 17227Document4 pages17227Caroline AlmeidaNo ratings yet
- Pi Is 0300957213007855Document2 pagesPi Is 0300957213007855Caroline AlmeidaNo ratings yet
- MOCADocument1 pageMOCAAna PimentelNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Labor Technician Skills and ExperienceDocument3 pagesLabor Technician Skills and ExperienceEnith Diaz HerreraNo ratings yet
- Nutrition, Physical Activity, and Quality of Life in Older AdultsDocument6 pagesNutrition, Physical Activity, and Quality of Life in Older AdultsDanusa AlvesNo ratings yet
- Food Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Document3 pagesFood Safety: HABC Level 2 Award in Food Safety in Catering (QCF)Caroline FrostNo ratings yet
- BCG Vaccine: Serum Institute of India Pvt. LTDDocument1 pageBCG Vaccine: Serum Institute of India Pvt. LTDkemalahmadNo ratings yet
- The New Science of Strong TeethDocument4 pagesThe New Science of Strong TeethThe Bioclear ClinicNo ratings yet
- Intern Journal reading-MRI-osteomyelitis-OOOE-2008Document6 pagesIntern Journal reading-MRI-osteomyelitis-OOOE-2008yuni madjidNo ratings yet
- 449 Exam 1 Study GuideDocument9 pages449 Exam 1 Study Guidemandy_kenneyNo ratings yet
- Larif Jauhari, Kuat Prabowo, Arfia FridiantiDocument9 pagesLarif Jauhari, Kuat Prabowo, Arfia Fridianti181OOO199 Indah SimanjuntakNo ratings yet
- Warning Signs of Various DiseasesDocument44 pagesWarning Signs of Various DiseasesamsabavanNo ratings yet
- Differences in Toxicokinetics and PharmacokineticsDocument6 pagesDifferences in Toxicokinetics and PharmacokineticsnagpharmaaNo ratings yet
- Daily JSA - Diesel FillingDocument3 pagesDaily JSA - Diesel Fillingshoaib akhtarNo ratings yet
- Hiv Testing Laboratory LawsDocument41 pagesHiv Testing Laboratory LawsMarian GarciaNo ratings yet
- NCP Viral MeningitisDocument7 pagesNCP Viral MeningitisvincevilNo ratings yet
- Nursing Care Plan Breast Feeding IneffectiveDocument1 pageNursing Care Plan Breast Feeding Ineffectivederic88% (8)
- GMDSS Exam Schedule For Year 2023Document5 pagesGMDSS Exam Schedule For Year 2023Nilesh KumarNo ratings yet
- Chronic PancreatitisDocument94 pagesChronic PancreatitisDipendra PoudelNo ratings yet
- Assignment Obm 100 CitationDocument3 pagesAssignment Obm 100 CitationNur DiniNo ratings yet
- DPT VaccinesDocument2 pagesDPT VaccinesSowmiyaNo ratings yet
- Controlling Rabies-One Humane SolutionDocument16 pagesControlling Rabies-One Humane SolutionTatiana Vieira de LimaNo ratings yet
- Learning Plan Medsurg Clinical RotationDocument7 pagesLearning Plan Medsurg Clinical Rotationapi-275795160100% (2)
- 12th Grade Veisalgia Text - QuestionsDocument3 pages12th Grade Veisalgia Text - QuestionsNUJMATUL HUDA AHARUL HADAFINo ratings yet
- MSDs in The WorkplaceDocument403 pagesMSDs in The WorkplaceAden ParkerNo ratings yet
- Chapter 29: Multiple Choice Questions: InstructionsDocument2 pagesChapter 29: Multiple Choice Questions: InstructionsLola Muhoza100% (1)
- COMMUNITY HEALTH PROFILE OF BARANGAY 142Document20 pagesCOMMUNITY HEALTH PROFILE OF BARANGAY 142Helen Fairodz AmoraNo ratings yet
- ESP For MIDWIFERY English For Specific PDocument46 pagesESP For MIDWIFERY English For Specific PMrKanghasanNo ratings yet
- FCM1 - S01-T01-Introduction To FCM and The Five Star Doctor PDFDocument6 pagesFCM1 - S01-T01-Introduction To FCM and The Five Star Doctor PDFGianne OgacoNo ratings yet
- Respiratory Syn-Cytial Virus: Rosal, Ija Lourice PDocument21 pagesRespiratory Syn-Cytial Virus: Rosal, Ija Lourice PIja Lourice RosalNo ratings yet
- Perkembangan Epidemiologi2Document64 pagesPerkembangan Epidemiologi2Mangun AngkatNo ratings yet
- M5-Routes of Medication AdministrationDocument13 pagesM5-Routes of Medication AdministrationKristine Kim100% (1)
- Greenberg 2021 Oi 210174 1617205370.55891-1Document13 pagesGreenberg 2021 Oi 210174 1617205370.55891-1cynthia jodjanaNo ratings yet