Professional Documents
Culture Documents
Planning Assignment (3 Field Rectum)
Uploaded by
api-280277788Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Planning Assignment (3 Field Rectum)
Uploaded by
api-280277788Copyright:
Available Formats
1
Jenny Kouri
Clinical Practicum I
4/3/15
Planning Assignment (3 field rectum)
Use a CT dataset of the pelvis. Create a CTV by contouring the rectum (start at the anus and stop
at the turn where it meets the sigmoid colon). Expand this structure by 1 cm and label it PTV.
Create a PA field with the top border at the bottom of L5 and the bottom border 2 cm below the
PTV. The lateral borders of the PA field should extend 1-2 cm beyond the pelvic inlet to include
primary surrounding lymph nodes. Place the beam isocenter in the center of the PTV and use the
lowest beam energy available (note: calculation point will be at isocenter). Contour all critical
structures (organs at risk) in the treatment area. List all organs at risk (OR) and desired
objectives/dose limitations, in the table below:
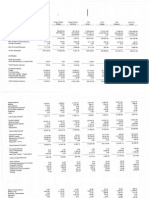
Organ at risk
Bladder
Desired objective(s)
40% < 40 Gy
Achieved objective(s)
7.99%
Small Bowel
Maximum dose < 50Gy
4804.2cGy
Femoral Head (R,L)
100cc < 40Gy
40% < 40 Gy
3947.0cGy
Right= 0.29%
Left= 1.26%
Maximum dose <5 0 Gy
Right= 4489.0cGy
Left= 4680.7cGy
*** Results are from the 3-field FINAL plan.
a. Enter the prescription: 45Gy at 1.8 /fraction (95% of the prescribed dose to cover the
PTV). Calculate the single PA beam. Evaluate the isodose distribution as it relates to CTV
and PTV coverage. Also where is/are the hot spot(s)? Describe the isodose distribution; if
a screen shot is helpful to show this, you may include it.
In this plan, a single 6MV posterior beam was used. The maximum dose point was 6699.4cGy.
At the VA Medical Center in Minneapolis, the maximum dose point is kept under 120% of the
prescription dose. For this plan, the hot spot should be less than 5400cGy. The hot spot was
6699.4cGy. This goal is not met and therefore this plan is not acceptable. The PTV coverage
was 88.42%. The 100% isodose line (red) clipped the PTV anteriorly. In the coronal plane, the
100% isodose line is not clean or distributed homogenously.
b. Change to a higher energy and calculate the beam. How did your isodose distribution
change?
This plan used an 18MV posterior beam. In comparison to the previous 6MV posterior beam,
dose was pushed more anteriorly with 18MV. 18MV has a greater dose build up region than
6MV and as a result, dose was spread at a greater distance before fall-off. The difference of dose
build up, allowed the 18MV maximum dose point to be cooler than the 6MV point. The 18MV
hot spot was 11% cooler than the 6MV hot spot. This plans maximum hot spot was 5962cGy.
This plan was unacceptable due to the hot spot being 132% higher than the prescription dose.
Insert a left lateral beam with a 1 cm margin around the ant and post wall of the PTV. Keep the
superior and inferior borders of the lateral field the same as the PA beam. Copy and oppose the
left lateral beam to create a right lateral field. Use the lowest beam energy available for all 3
fields. Calculate the dose and apply equal weighting to all 3 beams. Describe this dose
distribution.
All 3 fields in this plan utilized 6MV beam energy. Although all the beams are equally weighted,
the right lateral produced a warmer pool of dose. However, the maximum dose point is located
to the left of the PTV. The hot spot was 5145.7cGy. The PTV coverage was 65.69%. In the
transverse plane, the PTV appeared to be covered by the 100% isodose line (red) but in the
sagittal plane, the PTV was clipped anteriorly. The PTV was clipped inferiorly in the coronal
plane.
c. Change the 2 lateral fields to a higher energy and calculate. How did this change the dose
distribution?
This plans right and left laterals used 18MV beam energy. The posterior beam used 6MV. The
PTV is not fully covered by the 100% isodose line (red). The PTV coverage was 77.53%. The
hot spot was 5145.7cGy. Even though the hot spot was under 120% of the prescription dose, this
plan was still unacceptable due to the low PTV coverage.
Increase the energy of the PA beam and calculate. What change do you see?
All the beams were changed to 18MV. The PTV coverage was 84.05%. The maximum hot spot
was 5156.8cGy. Like the previous plan, the hot spot was under 120% of the prescription dose.
However, this plan was still unacceptable due to the low PTV coverage.
d. Add the lowest angle wedge to the two lateral beams. What direction did you place the
wedge and why? How did it affect your isodose distribution? (To describe the wedge
orientation you may draw a picture, provide a screen shot, or describe it in relation to the
patient. (e.g., Heel towards anterior of patient, heel towards head of patient..)
I was curious how the orientation of the wedges would affect the plan. To compare, I created
plans with 15-degree wedges oriented as a wedge pair with the heels posterior and another
oriented anterior. These are shown below.
This plan used 15-degree wedges with the heels oriented posterior. The PTV coverage was
89.50%. The hot spot was 4995.9cGy. The PTV is almost covered by the 100% isodose line
(red) but is barely clipped anteriorly. In comparison to the previous plans, the anterior portion of
the PTV is covered more than without the wedges. The wedges allowed for more dose to shift
anteriorly due to more attenuation by the thicker end of the heels. If this plan were normalized
down from 100% to 98%, this plan would have been acceptable.
This plan used 15-degree wedge pair with the heels placed anterior. The PTV coverage was
74.87%. The hot spot was 5199.7cGy. Dose was pushed posteriorly due to the wedging. The
100% isodose line (red) clipped the anterior portion of the PTV. In comparison to the heels
oriented posterior, PTV coverage was better in the previous plan.
e. Continue to add thicker wedges on both lateral beams and calculate for each wedge angle
you try (when you replace a wedge on the left, replace it with the same wedge angle on
the right). What wedge angles did you use and how did it affect the isodose distribution?
This plan used a 30-degree wedge pair with the heels placed posterior. The PTV
coverage was 98.57%. The hot spot was 4927.7cGy. The thicker heels allow for more
dosage to cover the PTV anteriorly.
10
This plan used a 30-degree wedge pair with the heels placed anterior. The PTV coverage was
81.45%. The hot spot was 5317.6cGy. This wedge orientation cooled the anterior portion of the
PTV too much. The 100% isodose line (red) clipped the PTV anteriorly.
f. Now that you have seen the effect of the different components, begin to adjust the
weighting of the fields. At this point determine which energy you want to use for each of
the fields. If wedges will be used, determine which wedge angle you like and the final
weighting for each of the 3 fields. Dont forget to evaluate this in every slice throughout
your planning volume. Discuss your plan with your preceptor and adjust it based on their
input. Explain how you arrived at your final plan.
11
The best dose coverage and homogenous beam distribution was achieved with 45-degree wedge
pair with the heels oriented posterior. The beam weighting for the posterior, left lateral, and right
lateral is 46%, 27%, and 27%, respectively. The PTV coverage was 100%. The hot spot was
4918cGy. This hot spot is 1.09% hotter than the prescription dose. The rule of thumb at this
clinical department is to keep the hot spot under 120% of the prescription dose.
g. In addition to the answers to each of the questions in this assignment, turn in a copy of
your final plan with the isodose distributions in the axial, sagittal and coronal views.
Include a final DVH.
The axial, sagittal, and coronal views are shown above.
12
Even though both femurs were kept under 50Gy, blocking or IMRT would significantly
lower the dose to the right and left femur.
4-field pelvis
Using the final 3-field rectum plan, copy and oppose the PA field to create an AP field. Keep the
lateral field arrangement. Remove any wedges that may have been used. Calculate the four fields
and weight them equally. How does this change the isodose distribution? What do you see as
possible advantages or potential disadvantages of adding the fourth field?
13
The maximum hot spot was 4845, 107% hotter than the prescription dose. The isodose lines
created a clean look and described the beam orientation of a 4-field box. The PTV is fully
covered by the 100% isodose line.
Advantages of the 4-field box include the following:
-Better coverage of PTV
-More homogenous dose distribution
-Less conformal in the event of rectal filling
Disadvantages of the 4-field box include the following:
14
-Increase dose to bladder
You might also like
- 3 FD RectumDocument13 pages3 FD Rectumapi-279520503No ratings yet
- Pelvis Lab 1 1Document13 pagesPelvis Lab 1 1api-632146706No ratings yet
- Pelvis Clinical Planning Lab 2018Document9 pagesPelvis Clinical Planning Lab 2018api-374655242No ratings yet
- Pelvis Clinical Lab AssignmentDocument9 pagesPelvis Clinical Lab Assignmentapi-428652649No ratings yet
- Pelvis Lab 2021new-1 6Document6 pagesPelvis Lab 2021new-1 6api-635186395No ratings yet
- Pelvis Lab HT 2Document15 pagesPelvis Lab HT 2api-642692363No ratings yet
- PelvisplanninglabDocument7 pagesPelvisplanninglabapi-268707929No ratings yet
- Pelvis Clinical Lab AssignmentDocument11 pagesPelvis Clinical Lab Assignmentapi-425716959No ratings yet
- 3+fd+rectum Planning AssignmentDocument5 pages3+fd+rectum Planning Assignmentapi-265264098No ratings yet
- Planning Project LungDocument5 pagesPlanning Project Lungapi-282901112No ratings yet
- Pelvis Lab 2021-1 2Document11 pagesPelvis Lab 2021-1 2api-642376263No ratings yet
- Pelvis Lab ReportDocument12 pagesPelvis Lab Reportapi-631272802No ratings yet
- Planning Project RectumDocument5 pagesPlanning Project Rectumapi-282901112No ratings yet
- Pelvis Clinical Lab AssignmentDocument8 pagesPelvis Clinical Lab Assignmentapi-432489466No ratings yet
- Pelvis Clinical Lab AssignmentDocument5 pagesPelvis Clinical Lab Assignmentapi-426737835No ratings yet
- Clinical Practicum II Parotid Planning AssignmentDocument13 pagesClinical Practicum II Parotid Planning Assignmentapi-299270003No ratings yet
- Pelvis Lab AllisonwrightDocument7 pagesPelvis Lab Allisonwrightapi-632741700No ratings yet
- Wael Mekhael Planning Assignment (3 Field Rectum)Document10 pagesWael Mekhael Planning Assignment (3 Field Rectum)api-267335639No ratings yet
- Pelvis Lab Assignment or 1Document17 pagesPelvis Lab Assignment or 1api-527669043No ratings yet
- Lung AssignmentDocument7 pagesLung Assignmentapi-280277788No ratings yet
- Pelvis LabDocument12 pagesPelvis Labapi-630263039No ratings yet
- Pelvis Lab AssignmentDocument13 pagesPelvis Lab Assignmentapi-534702185No ratings yet
- Lung Lab Instructions 1Document12 pagesLung Lab Instructions 1api-635186395No ratings yet
- Clinical Pelvis Lab - Due March 9thDocument25 pagesClinical Pelvis Lab - Due March 9thapi-569174359No ratings yet
- Lung Clinical Lab Assignment Write UpDocument16 pagesLung Clinical Lab Assignment Write Upapi-431720460No ratings yet
- LunglabpdfDocument21 pagesLunglabpdfapi-632827798No ratings yet
- Clinical Lung LabDocument17 pagesClinical Lung Labapi-632526087No ratings yet
- Pelvis Lab RavernewDocument7 pagesPelvis Lab Ravernewapi-635923017No ratings yet
- Lung Clinical Lab AssignmentDocument8 pagesLung Clinical Lab Assignmentapi-432489466No ratings yet
- Pelvis Clinical Lab AssignmentDocument13 pagesPelvis Clinical Lab Assignmentapi-528136686No ratings yet
- Lung Clinical Lab AssignmentDocument10 pagesLung Clinical Lab Assignmentapi-429099049No ratings yet
- Pelvis Clinical Planning Lab FinalDocument7 pagesPelvis Clinical Planning Lab Finalapi-405398222No ratings yet
- Planning Assignment (3 Field Rectum)Document13 pagesPlanning Assignment (3 Field Rectum)api-268623363No ratings yet
- Lung LabDocument12 pagesLung Labapi-642376263No ratings yet
- Lung LabweeblyDocument7 pagesLung Labweeblyapi-312374730No ratings yet
- Lung Lab-Clinical 1Document14 pagesLung Lab-Clinical 1api-633434674No ratings yet
- Lung Clinical Lab AssignmentDocument8 pagesLung Clinical Lab Assignmentapi-534702185No ratings yet
- Lung Lab Write UpDocument17 pagesLung Lab Write Upapi-631272802No ratings yet
- Lung Clinical Lab Assignment2Document10 pagesLung Clinical Lab Assignment2api-425716959No ratings yet
- Lung LabDocument11 pagesLung Labapi-302696314No ratings yet
- Pelvis Lab AssignmentDocument13 pagesPelvis Lab Assignmentapi-631250296No ratings yet
- Dos 771 - Lung Lab CompleteDocument16 pagesDos 771 - Lung Lab Completeapi-645531105No ratings yet
- PelvislabpdfDocument17 pagesPelvislabpdfapi-632827798No ratings yet
- Dans Lung Lab AssignmentDocument8 pagesDans Lung Lab Assignmentapi-395602816No ratings yet
- Lung Clinical Lab AssignmentDocument6 pagesLung Clinical Lab Assignmentapi-373874340No ratings yet
- DOS Clinical Practicum I Planning Assignment (Lung Lab) Ashley CoffeyDocument8 pagesDOS Clinical Practicum I Planning Assignment (Lung Lab) Ashley Coffeyapi-308717184No ratings yet
- Lung Write-UpDocument15 pagesLung Write-Upapi-632493717No ratings yet
- Lung Planning AssignmentDocument5 pagesLung Planning Assignmentapi-265264098No ratings yet
- Lung Lab Assignment Copy 8Document15 pagesLung Lab Assignment Copy 8api-529438966No ratings yet
- Lunglab Josephspencer 1Document15 pagesLunglab Josephspencer 1api-633248237No ratings yet
- LungDocument3 pagesLungapi-247959633No ratings yet
- Lung Clinical Lab AssignmentDocument7 pagesLung Clinical Lab Assignmentapi-404851310No ratings yet
- Lung Lab-Ht 2Document17 pagesLung Lab-Ht 2api-642692363No ratings yet
- Final Lung Lab 1Document7 pagesFinal Lung Lab 1api-431732695No ratings yet
- Lung Lab Final 1 1Document11 pagesLung Lab Final 1 1api-428652649No ratings yet
- LungDocument8 pagesLungapi-267335639No ratings yet
- Lung Clinical Lab AssignmentDocument13 pagesLung Clinical Lab Assignmentapi-528136686No ratings yet
- Pelvis LabDocument7 pagesPelvis Labapi-431732695No ratings yet
- Lung Lab RaverDocument9 pagesLung Lab Raverapi-635923017No ratings yet
- 2015 ResumeDocument3 pages2015 Resumeapi-280277788No ratings yet
- BrachyDocument3 pagesBrachyapi-280277788No ratings yet
- Responses About You - Summary - "IMRT Planning Competency (Rev2015) "Document3 pagesResponses About You - Summary - "IMRT Planning Competency (Rev2015) "api-280277788No ratings yet
- Nov DecDocument6 pagesNov Decapi-280277788No ratings yet
- Nov DecDocument6 pagesNov Decapi-280277788No ratings yet
- Responses About You - Summary - "IMRT Planning Competency (Rev2015) "Document3 pagesResponses About You - Summary - "IMRT Planning Competency (Rev2015) "api-280277788No ratings yet
- Pros W NodesDocument2 pagesPros W Nodesapi-280277788No ratings yet
- Breast Case StudyDocument12 pagesBreast Case Studyapi-280277788No ratings yet
- Responses About You - Summary - "IMRT Planning Competency (Rev2015) "Document3 pagesResponses About You - Summary - "IMRT Planning Competency (Rev2015) "api-280277788No ratings yet
- Responses About You - Summary - "Photon Planning Competency Evaluation (Rev2015) "Document3 pagesResponses About You - Summary - "Photon Planning Competency Evaluation (Rev2015) "api-280277788No ratings yet
- Responses About You - Summary - "Photon Planning Competency Evaluation (Rev2015) "Document3 pagesResponses About You - Summary - "Photon Planning Competency Evaluation (Rev2015) "api-280277788No ratings yet
- Nov DecDocument6 pagesNov Decapi-280277788No ratings yet
- Budget ActivityDocument2 pagesBudget Activityapi-280277788No ratings yet
- Fall Case Log TotalsDocument2 pagesFall Case Log TotalsBen LemieuxNo ratings yet
- Nov DecDocument6 pagesNov Decapi-280277788No ratings yet
- Bed Eqd2Document3 pagesBed Eqd2api-280277788No ratings yet
- Nov DecDocument6 pagesNov Decapi-280277788No ratings yet
- Summer Semester Volunteer RDocument2 pagesSummer Semester Volunteer Rapi-280277788No ratings yet
- Brittany Jenny Ben Final Paper 1Document12 pagesBrittany Jenny Ben Final Paper 1api-280277788No ratings yet
- Va BudgetDocument4 pagesVa Budgetapi-280277788No ratings yet
- Sample BudgetDocument6 pagesSample Budgetapi-280277788No ratings yet
- Fall Case Log TotalsDocument2 pagesFall Case Log TotalsBen LemieuxNo ratings yet
- Flow ChartDocument7 pagesFlow Chartapi-280277788No ratings yet
- BbtpsDocument3 pagesBbtpsapi-280277788No ratings yet
- CPT EncountersDocument4 pagesCPT Encountersapi-280277788No ratings yet
- Tps Qa 1Document6 pagesTps Qa 1api-280277788No ratings yet
- Dosimetry Job DescriptionnDocument3 pagesDosimetry Job Descriptionnapi-280277788No ratings yet
- Imaging Qa JennyDocument7 pagesImaging Qa Jennyapi-280277788No ratings yet
- Final Qa ChartDocument20 pagesFinal Qa Chartapi-280277788No ratings yet
- Daily Qa 1Document8 pagesDaily Qa 1api-280277788No ratings yet
- Alfa Laval Energy Balance Casestory enDocument2 pagesAlfa Laval Energy Balance Casestory enHélder FernandoNo ratings yet
- D5293Document8 pagesD5293Carlos Olivares ZegarraNo ratings yet
- Laplace Transform AssignmentDocument1 pageLaplace Transform AssignmentMohamad DuhokiNo ratings yet
- 405 Econometrics Odar N. Gujarati: Prof. M. El-SakkaDocument27 pages405 Econometrics Odar N. Gujarati: Prof. M. El-SakkaKashif KhurshidNo ratings yet
- 2 Linking Operations To Finance and ProductivityDocument14 pages2 Linking Operations To Finance and ProductivityAidan HonnoldNo ratings yet
- Comparing characteristics and properties of various crude oilsDocument2 pagesComparing characteristics and properties of various crude oilsnishant bhushanNo ratings yet
- Word Trek Lesson OutlinesDocument8 pagesWord Trek Lesson Outlinesapi-289048378No ratings yet
- ADAMHAND8A4Document11 pagesADAMHAND8A4Elker José Camargo100% (1)
- 066 LW Tensile Tester v2.0 PDFDocument4 pages066 LW Tensile Tester v2.0 PDFMarkusNo ratings yet
- Renal Cortical CystDocument2 pagesRenal Cortical Cystra222j239No ratings yet
- Output Configurations and Connections: NPN Open CollectorDocument2 pagesOutput Configurations and Connections: NPN Open Collectordorin serbanNo ratings yet
- Connorized Classical CatalogDocument37 pagesConnorized Classical CatalogPablo Olea RodríguezNo ratings yet
- TATA Gluco PDFDocument5 pagesTATA Gluco PDFsidharth dasNo ratings yet
- Interaction of Radiation With Matter: Dhruba GuptaDocument36 pagesInteraction of Radiation With Matter: Dhruba GuptaHala SweetNo ratings yet
- ABRACON's Tuning Fork Crystals and Oscillators for 32.768kHz RTC ApplicationsDocument13 pagesABRACON's Tuning Fork Crystals and Oscillators for 32.768kHz RTC Applicationsdit277No ratings yet
- Doctors Appointment - 4!14!17 Acid RefluxDocument11 pagesDoctors Appointment - 4!14!17 Acid RefluxRay Edwin Anderson IIINo ratings yet
- Serospin Operating Manual 20100407Document19 pagesSerospin Operating Manual 20100407Verdana50% (2)
- IRELAND - Rivers, Lakes and Mountains: Look at The Maps and Answer These QuestionsDocument2 pagesIRELAND - Rivers, Lakes and Mountains: Look at The Maps and Answer These QuestionsHannaNo ratings yet
- Geneaid DNA Reagent Plant GR200Document4 pagesGeneaid DNA Reagent Plant GR200Gandi SogandiNo ratings yet
- Megger FORMDocument1 pageMegger FORMCOSMOPOLITAN M&ENo ratings yet
- W2AEW Videos (Apr 29, 2017) Topics Listed NumericallyDocument12 pagesW2AEW Videos (Apr 29, 2017) Topics Listed Numericallyamol1agarwalNo ratings yet
- The UFO MonthlyDocument21 pagesThe UFO MonthlySAB78No ratings yet
- E5971 m4n68t-m Series ManualDocument0 pagesE5971 m4n68t-m Series ManualcamiloelosadaNo ratings yet
- CBSE Class 11 English Sample Paper Set 5Document8 pagesCBSE Class 11 English Sample Paper Set 5Shantam BasuNo ratings yet
- 01 UM Nutrition Training PlanDocument11 pages01 UM Nutrition Training PlanJohn Leclair100% (2)
- AbstractsDocument224 pagesAbstractsFrankmerced Emerzon Farfan HuancaNo ratings yet
- VMA 2520 eDocument7 pagesVMA 2520 eVijaya SimhaNo ratings yet
- Common Sense Renewed R. C. ChristianDocument276 pagesCommon Sense Renewed R. C. Christianwarhed76100% (3)
- RDT Steering System Pressure ChartDocument118 pagesRDT Steering System Pressure ChartAnonymous 340A7vnwV1100% (2)
- TOEFL Module 1 - ReadingDocument65 pagesTOEFL Module 1 - ReadingImam NurviyantoNo ratings yet