Professional Documents
Culture Documents
2 Pathophysiology of HIV
Uploaded by
Ismail SalimOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2 Pathophysiology of HIV
Uploaded by
Ismail SalimCopyright:
Available Formats
Pathophysiology of the human
immunodeficiency virus
Nancy R. Calles, MSN, RN, PNP, ACRN, MPH
Desiree Evans, MD, MPH
DeLouis Terlonge, MD
Overview
Objectives
1.
2.
3.
4.
5.
The human immunodeficiency virus (HIV) is a retrovirus
belonging to the family of lentiviruses. Retroviruses can
use their RNA and host DNA to make viral DNA and
are known for their long incubation periods. Like other
retroviruses, HIV infects the body, has a long incubation
period (clinical latency), and ultimately causes the signs
and symptoms of disease, here AIDS. HIV causes severe
damage to the immune system and eventually destroys it
by using the DNA of CD4+ cells to replicate itself. In that
process, the virus eventually destroys the CD4+ cells.
Provide an overview of the healthy immune system.
Describe the human immunodeficiency virus (HIV).
Describe the major components of the HIV life cycle.
Identify the various HIV types and subtypes.
Discuss HIVs effects on the immune system.
Key Points
1. The immune system protects the body by
recognizing invading antigens on pathogens
(bacteria, viruses, fungi, and parasites) and reacting
to them.
2. T lymphocytes, or T cells, regulate the immune
system and destroy antigens.
3. HIV continuously uses new host cells to replicate
itself.
4. The HIV life cycle includes six phases: binding and
entry, reverse transcription, integration, replication,
budding, and maturation.
5. Once HIV is in the circulatory system, it targets the
CD4+ lymphocyte.
6. Two types of HIV cause AIDS: HIV type 1 (HIV-1)
and HIV-2.
7. Primary infection refers to the time when HIV first
enters the body.
8. Clinical latency refers to the time before onset of
symptoms and complications in the HIV-infected
individual. In HIV-infected adults, this phase may
last 8-10 years.
9. Early signs and symptoms of HIV can include
candidiasis, lymphadenopathy, cervical carcinoma,
herpes zoster, and peripheral neuropathy.
10. Late signs and symptoms of HIV and AIDS-defining
illnesses can include the development of lifethreatening infections and malignancies.
The Healthy Immune System
The immune system protects the body by recognizing
antigens on invading bacteria and viruses and reacting to
them. An antigen is any substance that induces a state of
sensitivity and immune responsiveness. These antigens
interact with antibodies and immune cells, initiating an
immune response. This process destroys the antigen,
allowing the body to be free of infections. Types of
antigens include bacteria, viruses, fungi, and parasites.
When the immune system is weakened or destroyed by a
virus such as HIV, the body is left vulnerable to infections.
The immune system consists of lymphoid organs and
tissues, including the bone marrow, thymus gland,
lymph nodes, spleen, tonsils, adenoids, appendix, blood,
and lymphatic vessels (Figure 1). All components of
the immune system are vital in the production and
development of lymphocytes, or white blood cells. B
lymphocytes (or B cells) and T lymphocytes (or T cells)
are produced from stem cells in the bone marrow. B cells
stay in the bone marrow to complete the maturation
process, but T lymphocytes travel to the thymus gland
to complete their maturation. There T lymphocytes
become immunocompetent, multiply, and become more
differentiated.
HIV Curriculum for the Health Professional
cells, T-suppressor cells, inhibits or suppresses immune
responses. Normal CD8+ cell count is between 300 and
1,000 cells in adults and children. The normal CD4+:CD8+
ratio is between 1.0 and 2.0.
Tonsils and
Adenoids
T cells can secrete cytokines (chemicals that kill cells),
such as interferon. Cytokines can bind to target cells and
activate the inflammatory process. They also promote
cell growth, activate phagocytes, and destroy target cells.
Interleukins are cytokines that serve as messengers
between white blood cells. Recombinant (laboratory
synthesized) interleukins are currently being studied in
clinical trials for patients with HIV infection.
Thymus
Lymph
Nodes
Spleen
Phagocytes
Peyers
Patches
Phagocytes include monocytes and macrophages,
large white blood cells that engulf and digest cells
carrying antigenic particles. Found throughout the
body, phagocytes rid the body of worn-out cells,
initiate the immune response by presenting antigens
to lymphocytes, are important in immune response
regulation and inflammation, and carry receptors for
cytokines. Dendritic cells, another type of phagocyte, also
are antigen-presenting cells. They have long, threadlike
extensions that help trap lymphocytes and antigens and
are found in the spleen and lymph nodes. Neutrophils
are granulocytic phagocytes that are important in the
inflammatory response.
Appendix
Bone
Marrow
Lymph
Nodes
Lymphatic
Vessels
Figure 1. Organs of the Immune System
B Lymphocytes
The main function of B lymphocytes is humoral (anti
body) immunity. Each B cell can recognize specific
antigen targets and can secrete specific antibodies.
Antibodies function by coating antigens, which makes
the antigens more vulnerable to phagocytosis (engulfing
and ingestion of invading organisms by leukocytes and/
or macrophages), or by triggering the complement
system, leading to an inflammatory response. Antibodies
are highly specialized serum protein molecules. They
are grouped into five classes, each having a specialized
function: immunoglobulin G (IgG), IgA, IgM, IgE, and
IgD.
Complement
The complement system consists of 25 proteins.
Complement can induce an inflammatory response when
it functions with antibodies to facilitate phagocytosis or
weaken the bacterial cell membrane. The complement
proteins interact with one another in a sequential
activation cascade, promoting the inflammatory process.
Despite the heavy artillery that the immune system has
against foreign predators (Figures 2 and 3), HIV defeats
it over time.
T Lymphocytes
T lymphocytes have two major functions: regulation of
the immune system and killing of cells that bear specific
target antigens. Each T cell has a surface marker, such as
CD4+, CD8+, and CD3+, that distinguishes it from other
cells. CD4+ cells are helper cells that activate B cells, killer
cells, and macrophages when a specific target antigen is
present. There are two main types of CD8+ cells. The first
type, cytotoxic CD8+ cells, kills cells infected by viruses or
bacteria, as well as cancer cells. The second type of CD8+
HIVs Structure
HIV consists of a cylindrical center surrounded by a
sphere-shaped lipid bilayer envelope. There are two
major viral glycoproteins in this lipid bilayer, gp120 and
gp41. The major function of these proteins is to mediate
recognition of CD4+ cells and chemokine receptors,
thereby enabling the virus to attach to and invade CD4+
cells. The inner sphere contains two single-stranded
8
Pathophysiology of the Human Immunodeficiency Virus
Stem Cell
Lymphoid
Precursor
Myeloid
Precursor
Platelets
Helper T-Cell
Monocyte
Eosinophil
H-Cell
Cytotoxic
T-Cell
Suppressor
T-Cell
Neutrophil
Mast Cell
Basophil
Plasma Cell
Macrophage
Figure 2. Cells of the immune system
White Blood Cells
Neutrophils
Lymphocytes
B-Cells
Eosinophils
T-Cells
CD4+
CD8+
Binds directly to
antigen and kills it
In charge of the army
Summons B-cells,
natural killer (NK) cells,
macrophages
Plans for a direct
attack
Figure 3. Immune response by white blood cells
Basophils
HIV Curriculum for the Health Professional
copies of the genomic material, RNA, as well as multiple
proteins and enzymes necessary for HIV replication and
maturation: p24, p17, reverse transcriptase, integrase,
and protease (Figure 4). Unlike other retroviruses, HIV
uses nine genes to code for the necessary proteins and
enzymes. The three principal genes are gag, pol, and
env. The gag gene encodes core proteins. The pol gene
encodes the enzymes reverse transcriptase, protease,
and integrase. The env gene encodes the HIV structural
components known as glycoproteins. The rest of the
genesrev, nef, vif, vpu, vpr, and tatare important for
viral replication and enhancing HIVs infectivity rate.
cells make their way to the lymph nodes and eventually
to the peripheral blood, where viral replication becomes
rapid. CD4+ lymphocytes that are recruited to respond to
viral antigen migrate to the lymph nodes. These become
activated and then proliferate via complex interaction of
cytokines released in the microenvironment of the lymph
nodes. This sequence of events makes the CD4+ cells
more susceptible to HIV infection, and it explains the
generalized lymphadenopathy characteristic of the acute
retroviral syndrome seen in adults and adolescents. In
contrast, HIV-infected monocytes allow viral replication
but resist killing. Thus, monocytes act as reservoirs of
HIV and as effectors of tissue damage in organs such as
the brain.
HIVs Life Cycle
Host cells infected with HIV have a shortened life span as
a result of the viruss using them as factories to produce
multiple copies of new HIV. Thus, HIV continuously uses
new host cells to replicate itself. As many as 10 million
to 10 billion virions (individual viruses) are produced
daily. In the first 24 h after exposure, HIV attacks or is
captured by dendritic cells in the mucous membranes
and skin. Within 5 days after exposure, these infected
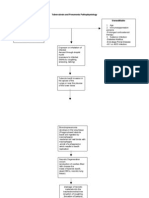
The HIV life cycle includes six phases: binding and entry,
reverse transcription, integration, replication, budding,
and maturation (Figure 5).
Binding and Entry
The envelope proteins gp120 and gp41 bind to CD4+ cell
receptors and coreceptors on the outside of CD4+ cells
HIV Structure
Envelope Proteins
gp120
Envelope
gp41
Matrix Proteins
p17
Core Proteins
p14
RT
RNA
Integrase
Protease
Figure 4. The Human Immunodeficiency Virus
10
Pathophysiology of the Human Immunodeficiency Virus
sCD4
CD4-lgG
Penetration
Reverse Transcriptase Inhibitors
Zidovudine
Didanosine
Zalcitabine
Stavudine
Lamivudine
Nevirapine
Uncoating
Reverse
transcription
Protease Inhibitors
Saquinavir
Indinavir
Ritonavir
Nelfinavir
Tat Antagonists
Trans- TransIntegration cription lation Assembly
Release
HIV
HIV
Host
chormosome
Double-stranded
unintegrated DNA
cDNA
CD4
and chemokine
receptors
Proviral
DNA
Genomic
RNA
Viral
mRNA
Nucleus
Cytoplasm
Figure 5. The HIV life cycle This depiction of the HIV life cycle shows the sites of action of some antiretroviral agents.
and macrophages. The chemokine receptors CCR5 and
CXCR4 facilitate viral entry. T-cell tropic viruses require
CXCR4 to bind, and macrotropic strains of the virus
require CCR5. R5 is the most common virus transmitted
during acute infection, and later during infection X4
is the virus that is most common. The presence of a
homozygous inactive mutation of the CCR5 allele has
caused resistance to infection by the R5 virus.
incorporation must occur for the virus to multiply. The
conversion of HIV RNA to DNA is known as reverse
transcription and is mediated by the HIV enzyme reverse
transcriptase. The result is the production of a single
strand of DNA from the viral RNA. The single strand of
this new DNA then undergoes replication into doublestranded HIV DNA.
The joining of the proteins and the receptors and
coreceptors fuses the HIV membrane with the CD4+
cell membrane, and the virus enters the CD4+ cell and
macrophage. The HIV membrane and the envelope
proteins remain outside of the CD4+ cell, whereas the
core of the virus enters the CD4+ cell. CD4+ cell enzymes
interact with the viral core and stimulate the release of
viral RNA and the viral enzymes reverse transcriptase,
integrase, and protease.
Once reverse transcription has occurred, the viral DNA
can enter the nucleus of the CD4+ cell. The viral enzyme
integrase then inserts the viral DNA into the CD4+ cells
DNA. This process is known as integration. The CD4+
cell has now been changed into a factory used to produce
more HIV.
Reverse Transcription
The HIV RNA must be converted to DNA before it can
be incorporated into the DNA of the CD4+ cell. This
Integration
Replication
The new DNA, which has been formed by the integration
of the viral DNA into the CD4+ cell, causes the production
of messenger DNA that initiates the synthesis of HIV
proteins.
11
HIV Curriculum for the Health Professional
Budding
Subtypes are unevenly distributed throughout the world.
Subtype C currently accounts for more than half of all
new HIV infections worldwide. Africa has most subtypes,
although subtype B is less prevalent. There are no known
subtypes of HIV-2.
The HIV proteins and viral RNA, all the components
needed to make a new virus, gather at the CD4+ cell
membrane to form new viruses. These new viruses push
through the different parts of the cell wall by budding.
Many viruses can push through the wall of one CD4+ cell.
These new viruses leave the CD4+ cell and contain all the
components necessary to infect other CD4+ cells.
Effects on the Immune System
The pathogenesis of HIV is basically a struggle between
HIV replication and the immune responses of the patient,
via cell-mediated and immune-mediated reactions. The
HIV viral burden directly and indirectly mediates CD4+
T-cell destruction. There is destruction of mature CD4+
cells; CD4+ progenitor cells in bone marrow, the thymus,
and peripheral lymphoid organs; as well as CD4+ cells
within the nervous system, such as microglia. The result
of this destruction is failure of T-cell production and
eventual immune suppression.
Maturation
The new virus has all the components necessary to infect
other CD4+ cells but cannot do so until it has matured.
During this process, the HIV protease enzyme cuts the
long HIV proteins of the virus into smaller functional
units that then reassemble to form a mature virus. The
virus is now ready to infect other cells.
HIV Types
There are two types of HIV that cause AIDS: HIV type 1
(HIV-1) and HIV-2. We know little about HIV-2. Studies
have shown striking similarities but also important
differences between HIV-1 and HIV-2. They have the
same modes of transmission and are associated with
the same opportunistic infections, but HIV-2 appears
to progress more slowly. Most HIV-2 cases are found
in western Africa and in countries related to western
Africa in some way such as Portugal, France, Angola,
Mozambique, Brazil, and India.
Various subtypes of HIV-1 have been found in specific
geographic areas and in specific high-risk groups. A
person can be coinfected with different subtypes. The
following are HIV-1 subtypes and their geographic
distributions:
Subtype A:
Central Africa, sub-Saharan Africa
Subtype B:
South America, Brazil, United States,
Thailand, Europe, Caribbean, India, Japan
Subtype C:
Brazil, India, South Africa
Subtype D:
Central Africa, sub-Saharan Africa
Subtype E:
Thailand, Central African Republic,
Southeast Asia
Subtype F:
Brazil, Romania, Democratic Republic of
Congo (Zaire)
Subtype G:
Democratic Republic of Congo (Zaire),
Gabon, Thailand, Russia, Central Africa
Subtype H:
Democratic Republic of Congo (Zaire),
Gabon, Russia, Central Africa
Subtype I:
Cyprus
Subtype O:
Cameroon, Gabon
12
There are many mechanisms of CD4+ cell depletion
by HIV infection. Direct HIV-mediated cytopathic
effects include single-cell killing as well as cell fusion,
or syncytium formation. The syncytium is a fusion of
multiple uninfected CD4+ cells with one HIV-infected
CD4+ cell via CD4gp120 interaction. This fusion results
in a multinucleated syncytium, or giant cell, which may
ultimately serve as a means to produce many virions. The
hosts natural immune responses also play a role in CD4+
cell depletion, mainly through cytotoxic CD8+ T-cells,
antibody-dependent cellular cytotoxicity, and natural
killer cells. Other mechanisms include autoimmune
responses, anergy, superantigen-mediated activation of
T cells, and programmed cell death (apoptosis).
HIV can infect many types of cells. The spread of HIV
outside lymphoid organs to the brain, spinal cord, lung,
colon, liver, and kidney usually occurs late during illness.
Table 1 gives a partial list of cells susceptible to HIV
infection.
The immune systems of HIV-infected children undergo
changes that are similar to those in adults. B-cell
activation occurs in most children early in the infection,
evidenced by the presence of hypergammaglobulinemia
(>1.750 g/L) with high levels of antiHIV-1 antibody. This
reflects both dysregulation of T-cell suppression of B-cell
antibody synthesis as well as active CD4+ enhancement
of B-lymphocyte humoral response. Also, as HIV disease
progresses through more severe immunosuppression
and depletion of CD4+ cells, the CD8+ count increases,
yielding an overall decrease in the CD4+:CD8+ ratio.
Pathophysiology of the Human Immunodeficiency Virus
Table 1. Cells Susceptible to HIV Infection
System
Cell
Hematopoietic
T-cells (CD4+ OR CD 8+)
Macrophages/monocytes
Dendritic cells
Fetal thymocytes and thymic epithelium
B-cells
NK cells
Megakaryotic cells
Stem cells
Central
Nervous
Microglia
Capillary endothelial cells
Astrocytes
Oligodendrocytes
Large Intestine
Columnar epithelium
Other
Kupfer cells (liver
Synovial cells
Placental tophoblast cells
Adapted from Levy L.A. Microbiological Reviews, 57:183-289, March 1993
Clinical Categories of HIV
Infection
Children infected with HIV often have severe disease
when first evaluated, or they may develop AIDS over
time, much like adults infected with HIV. Infants and
young children normally have higher CD4+ counts than
those of adults. The normal CD4+ count in children varies
with age, but it is equal to the adult value by the time the
child is 6 years old. Immunologic and clinical categories
are used to evaluate the HIV disease status in children
and to make treatment decisions.
Primary Infection, or Acute Retroviral Syndrome
Primary infection refers to the time when HIV first
enters the body. At the time of primary infection with
HIV, a persons blood carries a high viral load, meaning
that there are many individual viruses in the blood. The
number of copies of virus per milliliter of plasma or
blood can exceed 1 million. Newly infected adults often
experience an acute retroviral syndrome. Signs and
symptoms of acute retroviral syndrome include fever,
myalgia (muscle pain), headache, nausea, vomiting,
diarrhea, night sweats, weight loss, and rash. These signs
and symptoms usually occur 24 weeks after infection,
subside after a few days, and often are misdiagnosed as
influenza or infectious mononucleosis. An important
differentiating symptom that is often absent is the
presence of a runny nose or nasal congestion.
During primary infection, the CD4+ count in the
blood decreases remarkably but rarely drops to less
than 200 cells/L. The virus targets CD4+ cells in the
lymph nodes and the thymus during this time, making
the HIV-infected person vulnerable to opportunistic
infections and limiting the thymuss ability to produce
T lymphocytes. HIV antibody testing using an enzymelinked immunosorbent assay or enzyme immunoassay
may yield positive or negative results depending on the
time of seroconversion. DNA PCR and RNA PCR will be
positive, but confirmation with Western blot analysis
may yield an indeterminate result because seroconversion
can take up to 28 weeks to occur. The average time to
seroconversion is 25 days.
Clinical Latency/Asymptomatic Disease
(Clinical Stage 1)
Although patients recently infected with HIV usually
experience a clinically latent period of years between
HIV infection and clinical signs and symptoms of AIDS,
evidence of HIV replication and host immune system
destruction exists from the onset of infection. Early
during this time, referred to as Clinical Stage 1 , the
immune system produces antibodies in an attempt to
protect itself from HIV. This is when the viral set point
is established. The viral load of the set point can be used
to predict how quickly disease progression will occur.
People with higher viral load set points tend to exhibit
more rapid disease progression than those with lower
viral load set points.
During latency, HIV-infected patients may or may not
have signs and symptoms of HIV infection though
persistent lymphadenopathy is common. In HIVinfected adults, this phase may last 810 years. The HIV
enzyme-linked immunosorbent assay and Western blot
or immunofluorescence assay will be positive. The CD4+
count is greater than 500 cells/L in children over 5 years
of age.
Mild Signs and Symptoms of HIV
(Clinical Stage 2)
HIV-infected people may appear to be healthy for
years, and then minor signs and symptoms of HIV
infection begin to appear. They may develop candidiasis,
lymphadenopathy, molluscom contagiosum, persistent
13
HIV Curriculum for the Health Professional
References
hepatosplenomegaly, popular pruritic eruptions, herpes
zoster, and/or peripheral neuropathy. The viral load
increases, and the CD4+ count falls is between 350-499/
uL in children older than 5 years. Once patients are in
this stage they remain in stage 2. They can be reassigned
stage 3 or 4 if a condition from one of those occurs, but
they cannot be reassigned to Clinical Stage 1 or 2 if they
become asymptomatic.
1. Behrman RE, Kliegman RM, Jenson HB. Nelson
Textbook of Pediatrics. Philadelphia: W.B. Saunders;
2004.
2. Bullock BL, Rosendahl PP. Immunity:
Pathophysiology Adaptations and Alterations in
Function. Philadelphia: Lippincott; 1992.
3. Centers for Disease Control and Prevention. (1994).
1994 revised classification system for human
immunodeficiency virus infection in children
less than 13 years of age. MMWR Recomm. Rep.
1994;43(RR-12):110.
4. Lusso P. (2006). HIV and the chemokine system: 10
years later. EMBO J. 2006;25:447456.
5. Montero J, Nadler JP. Pathophysiology of HIV
Infection. In HIV/AIDS Primary Care Guide. Crown
House Publishing Limited; 2005:114.
6. Noble R. Introduction to HIV types, groups and
subtypes. http://www.avert.org/hiv-types.htm.
Accessed June 24, 2009.
7. Azevedo-Pereira JM, Moniz-Pereira J, Santos-Costa
Q. HIV-2 infection and chemokine receptor usage
clues to reduced virulence of HIV-2. Curr. HIV Res.
2005;3:316.
8. Klatt EC. Human Immunodeficiency Virus.
Pathology of AIDS. University of Utah; 1999.
9. Ungvarske PJ, Flasderud HJ. Overview and
Update of HIV/AIDS: A Guide to Primary Care and
Management. Philadelphia: W.B. Saunders; 1999.
10. U.S. Department of Health and Human Services,
National Institutes of Health, National Institute of
Allergies and Infectious Diseases. Understanding the
Immune System and How It Works. Bethesda, MD;
2007.
Advanced Signs and Symptoms of HIV
(Clinical Stage 3)
HIV-infected patients with weakened immune systems
can develop life-threatening infections. The development
of cryptosporidiosis, pulmonary and lymph node
tuberculosis, wasting, persistent fever (longer than
one month), persistent candidasis, recurrent bacterial
pneumonia, and other opportunistic infections is
common. These patients may be wasting, or losing weight.
Their viral load continues to increase, and the CD4+ count
falls to less than 200-349 cells/L in children older than 5
years.
Clinical Stage 4
Patients with advanced HIV disease, or AIDS, can
continue to develop new opportunistic infections,
such as Pneumocystis jirovecii pneumonia (formerly
Pneumocystis carinii pneumonia), cytomegalovirus
infection, toxoplasmosis, Mycobacterium avium
complex, cryptococcal meningitis, progressive multifocal
leukoencephalopathy, Kaposi sarcoma and other infections
that commonly occur with a severely depressed immune
system. The viral load is very high, and the CD4+ count is
less than 200 cells/L in children older than 5 years. At this
point in the disease course death can be imminent.
14
You might also like
- Pathophysiology: HIV Infection and AIDSDocument7 pagesPathophysiology: HIV Infection and AIDSmeylin SNo ratings yet
- Pathophysiology of AIDS: Transmission and Immune System DestructionDocument1 pagePathophysiology of AIDS: Transmission and Immune System DestructionJason A. Adoyogan0% (1)
- Student Nurses' Community: Nursing Care Plan Aids/HivDocument2 pagesStudent Nurses' Community: Nursing Care Plan Aids/HivAdha100% (1)
- PathophysiologyDocument6 pagesPathophysiologyElbert Hermogino ﭢNo ratings yet
- Drug-Study NCPDocument5 pagesDrug-Study NCPMURILLO, FRANK JOMARI C.No ratings yet
- Pathophysiology of Hypersensitivity Type IIDocument2 pagesPathophysiology of Hypersensitivity Type IItwin_smartyNo ratings yet
- B. Diagram: Predisposing Factors: Precipitating Factors EtiologyDocument3 pagesB. Diagram: Predisposing Factors: Precipitating Factors EtiologyKenneth Torres100% (1)
- Components of Foood Home Work AdhritDocument3 pagesComponents of Foood Home Work AdhritMrudula GummuluriNo ratings yet
- Non-Modifiable Factor Modifiable Factor: South-East Asia, Eastern, Mediterranean, Western Pacific, and The AmericasDocument2 pagesNon-Modifiable Factor Modifiable Factor: South-East Asia, Eastern, Mediterranean, Western Pacific, and The Americaschristian quiaoitNo ratings yet
- Iv. Review of Anatomy and Physiology Figure 1. The Immune SystemDocument7 pagesIv. Review of Anatomy and Physiology Figure 1. The Immune SystemNejie Zarrah Diaz100% (1)
- Pre Term Case OlieDocument10 pagesPre Term Case OlieKimsha ConcepcionNo ratings yet
- NCP Risk For InfecctionDocument2 pagesNCP Risk For Infecctionsnay axieNo ratings yet
- NCP Hyperbilirubinemia Staff NursingDocument3 pagesNCP Hyperbilirubinemia Staff NursingVerajoy DaanNo ratings yet
- Dengue FeverDocument8 pagesDengue Feverramoli1988No ratings yet
- Pathophysiology: Incubation StageDocument3 pagesPathophysiology: Incubation StageWilliam Soneja CalapiniNo ratings yet
- Medical Management For PneumoniaDocument2 pagesMedical Management For PneumoniaSue Elaine100% (1)
- PP Insect Bite 2007 (Print)Document16 pagesPP Insect Bite 2007 (Print)Ali RumiNo ratings yet
- Drug Study - CefotaximeDocument5 pagesDrug Study - CefotaximeAngel laurestaNo ratings yet
- Malaria PathophysiologyDocument1 pageMalaria Pathophysiologykaye040375% (4)
- The Immune System: A Finely Tuned DefenseDocument5 pagesThe Immune System: A Finely Tuned DefenseKathleen DimacaliNo ratings yet
- Pathophysiology Dengue Hemorrhagic FeverDocument1 pagePathophysiology Dengue Hemorrhagic FeverShiella Heart Malana100% (1)
- TB Drug StudyDocument15 pagesTB Drug StudyKaloy KamaoNo ratings yet
- Tetanus Toxoid Vaccine Nursing Care PlanDocument3 pagesTetanus Toxoid Vaccine Nursing Care PlanDwight DiazNo ratings yet
- Nursing Care Plan On SepsisDocument6 pagesNursing Care Plan On SepsisleoNo ratings yet
- Pelvic Inflammatory Disease - 1Document8 pagesPelvic Inflammatory Disease - 1fatqur28No ratings yet
- Resource Unit OliveDocument14 pagesResource Unit OliveCaryl AlivioNo ratings yet
- Individual Activity 3 PDFDocument11 pagesIndividual Activity 3 PDFBanana QNo ratings yet
- HIV - PathogenesisDocument14 pagesHIV - Pathogenesisjunaidiabdhalim100% (1)
- HepatitisDocument3 pagesHepatitisRosendo Dacuyan100% (1)
- Watery Vaginal Discharge Patient CaseDocument14 pagesWatery Vaginal Discharge Patient CaseCathleen Nasis ForrosueloNo ratings yet
- NCP - Preeclampsia (A)Document6 pagesNCP - Preeclampsia (A)Ronel ResurricionNo ratings yet
- Chickenpox 1Document7 pagesChickenpox 1Nica Joy CandelarioNo ratings yet
- Dengue Hemorrhagic FeverDocument12 pagesDengue Hemorrhagic FeverJohn Maurice AbelNo ratings yet
- X Pathophysiology Dengue FeverDocument1 pageX Pathophysiology Dengue FeverkarlNo ratings yet
- Concept Map Group 1Document1 pageConcept Map Group 1eric macabiog100% (1)
- Cefadroxil DuricefDocument1 pageCefadroxil Duricefstaylor235No ratings yet
- PCAPDocument2 pagesPCAPMizpah DuculanNo ratings yet
- Microbial Diseases of The Skin and Eyes (Microbiology Chapter 21)Document82 pagesMicrobial Diseases of The Skin and Eyes (Microbiology Chapter 21)Katrina Isabel100% (1)
- Summary Product Charecteristics: Rabies Vaccine For Human Use, (Vero-Cell) Freeze-Dried (Speeda Vaccine)Document4 pagesSummary Product Charecteristics: Rabies Vaccine For Human Use, (Vero-Cell) Freeze-Dried (Speeda Vaccine)Ryll Dela CruzNo ratings yet
- Tetanus Toxoid For Booster Use Only: (Not Recommended For Primary Immunization)Document5 pagesTetanus Toxoid For Booster Use Only: (Not Recommended For Primary Immunization)Ade PurnaNo ratings yet
- St. Paul College of Ilocos Sur: Stages in The Natural History of Disease and The Levels of Prevention During Ncov-19Document3 pagesSt. Paul College of Ilocos Sur: Stages in The Natural History of Disease and The Levels of Prevention During Ncov-19Marie Kelsey Acena Macaraig100% (1)
- ALL PathophysiologyDocument2 pagesALL PathophysiologyDeo Michael Rivera LlamasNo ratings yet
- 2nd Drug Study FinalDocument6 pages2nd Drug Study FinalMariella Saavedra Aranda CercadoNo ratings yet
- Liver AbscessDocument3 pagesLiver AbscessStephanie Pe100% (1)
- Case Study 5 Dengue Fever CorrectedDocument13 pagesCase Study 5 Dengue Fever CorrectedyounggirldavidNo ratings yet
- HIV/AIDS Definition, Causes, Symptoms & TreatmentDocument2 pagesHIV/AIDS Definition, Causes, Symptoms & TreatmentAC, MDNo ratings yet
- Activity intolerance, fear, infection risks in thalassemiaDocument1 pageActivity intolerance, fear, infection risks in thalassemiaHannah Clarisse Monge IgniNo ratings yet
- Dengue Case StudyDocument23 pagesDengue Case Studycutie_0023No ratings yet
- Pathophysiology of Hyperemesis Gravidarum DiagramDocument1 pagePathophysiology of Hyperemesis Gravidarum DiagramQuintin MangaoangNo ratings yet
- Case Studies - Tetralogy of FallotDocument16 pagesCase Studies - Tetralogy of FallotKunwar Sidharth SaurabhNo ratings yet
- Case 1 - GDMDocument34 pagesCase 1 - GDMJan Rae Barnatia AtienzaNo ratings yet
- Favirab administration guidelines for rabies prophylaxisDocument4 pagesFavirab administration guidelines for rabies prophylaxisAugene ToribioNo ratings yet
- Pathophysiology of Dengue FeverDocument1 pagePathophysiology of Dengue FeverApple Mae100% (1)
- Assessment Nursing Diagnosis Outcome Nursing Interventions Evaluation Standard Criteria Subjective: Short Term GoalDocument6 pagesAssessment Nursing Diagnosis Outcome Nursing Interventions Evaluation Standard Criteria Subjective: Short Term GoalmitchNo ratings yet
- DRUG STUDY (Preeclampsia)Document11 pagesDRUG STUDY (Preeclampsia)Jobelle AcenaNo ratings yet
- 2 Pa Tho Physiology of HIVDocument8 pages2 Pa Tho Physiology of HIVLeepin TanNo ratings yet
- Aids and ImmunologyDocument27 pagesAids and ImmunologyIndra DhootNo ratings yet
- (Human Immunodeficiency Virus) &: Acquired Immune Deficiency SyndromeDocument61 pages(Human Immunodeficiency Virus) &: Acquired Immune Deficiency SyndromeGufron MustofaNo ratings yet
- Protection From HIV/AIDS: The Importance of Innate Immunity: Jay A. Levy, Iain Scott, and Carl MackewiczDocument8 pagesProtection From HIV/AIDS: The Importance of Innate Immunity: Jay A. Levy, Iain Scott, and Carl MackewiczSofi Papel JachoNo ratings yet
- Hiv& Aids: by Emily MuchinaDocument64 pagesHiv& Aids: by Emily MuchinaChris CizaNo ratings yet
- 10 1 1 126Document60 pages10 1 1 126Manfred GithinjiNo ratings yet
- Ajr 10 460h0Document6 pagesAjr 10 460h0Raga ManduaruNo ratings yet
- Msds 2 PDFDocument5 pagesMsds 2 PDFRaga ManduaruNo ratings yet
- Treatment of Hypertension: JNC 8 and More: Pharmacist'S Letter / Prescriber'S LetterDocument6 pagesTreatment of Hypertension: JNC 8 and More: Pharmacist'S Letter / Prescriber'S LetterJen CanlasNo ratings yet
- Uterine Sarcoma in Patients Operated On For.17Document3 pagesUterine Sarcoma in Patients Operated On For.17Raga ManduaruNo ratings yet
- Cholera Epidemic Associated With Consumption of Unsafe Drinking WaterDocument6 pagesCholera Epidemic Associated With Consumption of Unsafe Drinking WaterRaga ManduaruNo ratings yet
- Jurnal Luar Lagi GiziDocument32 pagesJurnal Luar Lagi GiziRaga ManduaruNo ratings yet
- Drugs For The Treatment of Diabetes MellitusDocument51 pagesDrugs For The Treatment of Diabetes MellitusRaga ManduaruNo ratings yet
- Daftar Pustaka HIV/AIDSDocument1 pageDaftar Pustaka HIV/AIDSRaga ManduaruNo ratings yet
- Salmonella in Surface and Ddwringking Water Occurance and Water Mediated Transmission Levantesi - FoodResInter - 2011Document17 pagesSalmonella in Surface and Ddwringking Water Occurance and Water Mediated Transmission Levantesi - FoodResInter - 2011Raga ManduaruNo ratings yet
- Jc180 Hiv Infantfeediscng 3 en 3Document26 pagesJc180 Hiv Infantfeediscng 3 en 3Raga ManduaruNo ratings yet
- SffsfsfsssvsfvsfsdfffeefefwefefefwefDocument7 pagesSffsfsfsssvsfvsfsdfffeefefwefefefwefRaga ManduaruNo ratings yet
- 247 FulldsDocument68 pages247 FulldsRaga ManduaruNo ratings yet
- WHO HIV Clinical Staging GuidelinesDocument49 pagesWHO HIV Clinical Staging Guidelinesdonovandube8235No ratings yet
- JakartaDocument7 pagesJakartaBachtiar M TaUfikNo ratings yet
- Nasopharyngeal Carriage of Klebsiella Pneumoniae and Other Gram-Negative Bacilli in Pneumonia-Prone Age Groups in Semarang, IndonesiaDocument3 pagesNasopharyngeal Carriage of Klebsiella Pneumoniae and Other Gram-Negative Bacilli in Pneumonia-Prone Age Groups in Semarang, IndonesiaRaga ManduaruNo ratings yet
- New Classification of Ocular Surface BurnsDocument6 pagesNew Classification of Ocular Surface BurnstiaracintyaNo ratings yet
- JJJJDocument6 pagesJJJJRaga ManduaruNo ratings yet
- Sat 0715 Breakfast Symposium Donnenfeld BlepharitisDocument22 pagesSat 0715 Breakfast Symposium Donnenfeld BlepharitisRaga ManduaruNo ratings yet
- SaaaDocument5 pagesSaaaRaga ManduaruNo ratings yet
- Principles of PreventionDocument14 pagesPrinciples of PreventionprecillathoppilNo ratings yet
- Adolescent Issues - Raga ManduaruDocument102 pagesAdolescent Issues - Raga ManduaruRaga ManduaruNo ratings yet
- Comparison of Maternal and Neonatal OutcomesDocument8 pagesComparison of Maternal and Neonatal OutcomesNuardi YusufNo ratings yet
- Risk Factors and Outcomes Associated With A Short.21Document9 pagesRisk Factors and Outcomes Associated With A Short.21Raga ManduaruNo ratings yet
- New Classification of Ocular Surface BurnsDocument6 pagesNew Classification of Ocular Surface BurnstiaracintyaNo ratings yet
- Risk Factors and Outcomes Associated With A Short.21Document9 pagesRisk Factors and Outcomes Associated With A Short.21Raga ManduaruNo ratings yet
- Archives of Gynecology and Obstetrics Volume 289 Issue 4 2014 (Doi 10.1007 - s00404-013-3072-9) Narang, Yum - Vaid, Neelam Bala - Jain, Sandhya - Suneja, Amita - Gu - Is Nuchal Cord JustifiDocument7 pagesArchives of Gynecology and Obstetrics Volume 289 Issue 4 2014 (Doi 10.1007 - s00404-013-3072-9) Narang, Yum - Vaid, Neelam Bala - Jain, Sandhya - Suneja, Amita - Gu - Is Nuchal Cord JustifiRaga ManduaruNo ratings yet
- Figure 1 The Role of Insulin Resistance in Diabetic DyslipidemiaDocument1 pageFigure 1 The Role of Insulin Resistance in Diabetic DyslipidemiaRaga ManduaruNo ratings yet
- Pathology Journal Reading: Presented by Intern 曾德朋Document33 pagesPathology Journal Reading: Presented by Intern 曾德朋Raga ManduaruNo ratings yet
- Keg Aw at Daru RatanDocument25 pagesKeg Aw at Daru RatanRaga ManduaruNo ratings yet