Professional Documents
Culture Documents
The Role of Fear of Movement/ (Re) Injury in Pain Disability
Uploaded by
Wilbur WhateleyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of Fear of Movement/ (Re) Injury in Pain Disability
Uploaded by
Wilbur WhateleyCopyright:
Available Formats
Journal of Occupational Rehabilitation, VoL 5, No.
4, 1995
The Role of Fear of Movement/(Re)Injury in Pain
Disability
Johan W. S. Vlaeyen, 1,2,4 Ank M. J. Kole-Snijders, 1 Annemarie M.
Rotteveel, 1 Renske Ruesink, 3 and Peter H. T. G. Heuts 3
It is now well established that in chronic low back pain, there is no direct relationship
between impairments, pain, and disability. From a cognitive-behavioral perspective,
pain disability is not only influenced by the organic pathology, but also by
cognitive-perceptual, psychophysiological, and motoric-environmental factors. This
paper focuses on the role of specific beliefs that are associated with avoidance of
activities. These beliefs are related to fear of movement and physical activity, which is
(wrongfully) assumed to cause (re)injury. Two studies are presented, of which the first
examines the factor structure of the Tampa Scale for Kinesiophobia (TSK), a recently
developed questionnaire that is aimed at quantifying fear of movement/(re)injury. In
the second study, the value of fear of movement/(re)injury in predicting disability levels
is analyzed, when the biomedical status of the patient and current pain intensity levels
are controlled for. In addition, the determinants of fear of movement/(re)injury are
examined. The discussion focuses on the clinical relevance of the fear-avoidance model
in relation to risk assessment, assessment of functional capacity, and secondary
prevention.
KEY WORDS: chronic low back pain; fear-avoidance; fear of movement; fear of (re)injury; fear of pain;
kinesiophobia; behavioral assessment.
INTRODUC~ON
Many people suffer from low back pain in the course of their lives, of which
not all seek health care. In the majority of the patients who seek care and refrain
from work, the pain problem resides within a few weeks. Data presented by the
Quebec Task Force on Spinal Disorders (1) show that 74% of the group of patients
1Institute for Rehabilitation Research, Zandbergsweg 111, 6432 CC Hoensbroek, The Netherlands.
2Department of Medical Psychology, University of Limburg, PO Box 616, 6400 MD Maastricht, The
Netherlands.
3Lucas Foundation for Rehabilitation, Zandbergsweg 111, 6432 CC Hoensbroek, The Netherlands.
4Correspondence should be directed to Dr. Johan W. S. Vlaeyen, Institute for Rehabilitation Research,
P.O. Box 192, 6430 AD Hoensbroek, The Netherlands.
235
1053-0487/95/1200-0235507.50/0 9 1995 Plenum Publishing Corporation
236
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
17 %
t
I
7da~m
4wko
7wks
13 %
I /'
12wks
8 %
1
24wks
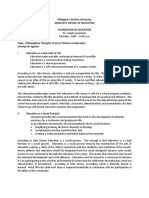
Fig. 1. The natural history of chronic back pain. Percentage of sick leave in relation to pain
duration since onset (based on Spitzer et al., 1987).
with acute back pain resume their work within the period of 4 weeks after the
acute pain onset (Fig. 1). If a worker has not returned to work by 7 weeks, there
is a 50% probability that he/she will be off work at 6 months. About 8% of the
patients still is sick leaving 6 months after the acute pain onset. Similar findings
have been reported by Crook and Moldofsky (2): If a worker has not returned to
work by 3 months, there is a 50% probability that he/she will be off work at 15
months. The relatively small group of chronic back pain patients is responsible
for enormous health care and societal costs (75-90% of the costs) of back problems (3). What are the reasons for this group to become chronic pain sufferers?
One of possibilities would be that this group has more serious impairments than
the group of workers who resume their work earlier. However, there are no research reports that support this assumption. On the contrary, numerous studies
have shown that there is no perfect relationship between impairments, pain and
disability and suggest that the behavioral or biopsychosocial approach offers the
foundations for a better insight in how pain can become a persistent problem (48). The main assumption is that pain and pain disability are not only influenced
by organic pathology, if found, but also by psychological and social factors. For
example, from a biomedical view, return to work should only be encouraged when
the underlying pathology has healed. Otherwise, the risks of reinjury and repeated
failures would increase, subsequently leading to the promotion of chronicity. From
this biomedical perspective, staying off too long would be much safer than resuming work activities too early. Results reported by Crook and Moldofsky (2), however, are in support of the conjecture that early return to work contributes to a
decrease in work disability in musculoskeletal pain patients. The arguments include
the recognition that musculoskeletal incidents are enhanced by the immediate consequences such as diminished pain, increased attention from others, avoidance of
unpleasant and fearful situations, and the stabilization of the sick role. Moreover,
longstanding avoidance leads to disuse of the musculature which in turn augments
the deficits in the necessary motoric, social and vocational skills. In other words,
the pain disability is subject to a graded shift from structural/mechanical to cognitive/environmental control. Studies by Deyo et al. (9), Philips and Grant (10),
and Klenerman et al. (11) suggest that this shift occurs quite rapidly, probably
within the period of 4-8 weeks after the acute pain onset.
Fear and Pain Disability
237
From a behavioral perspective (chronic) pain can best be studied as a hypothetical construct, which is not observable in itself but which can be inferred only
by its effects at some observable level. Three observable levels or response systems
of pain have been described repeatedly: psycho-physiological reactivity, the cognitive-perceptual system, and the overt motoric system (12).
Psycho-Physiological Reactivity
When confronted with a stressor, the individual will respond automatically
with an increase in sympathetic arousal. Evidence exists that patients with low back
pain display elevations in paraspinal electromyographic activity, and delayed return
to baseline following exposure to personally relevant and not just general stressors
(13). Increased sympathetic arousal to pain or psychosocial stressors may contribute
to a reduced ability to tolerate pain, and subsequently to functional limitations and
pain disability (14).
Cognitive-Perceptual Factors
Cognitive-perceptual responses refer to the way the patient perceives and interprets his/her environment, and the extent to which he/she thinks that control
can being excerted over the situation. One of the possible attributions is that pain
is a sign of a serious health problem, and has been referred to as "illness (or disease) conviction" (15). Such an appraisal may be based on a misinterpretation of
proprioceptive signals (16). A common appraisal reported by chronic pain patients
is "Catastrophizing," referring to an attentional bias toward negative aspects and
exaggeration of their situation. Catastrophizing is known to be associated with increasing distress, which in turn can increase pain by reducing pain tolerance levels
and by triggering unnecessary sympathetic arousal (17).
Overt Motoric Factors
The overt-motoric system covers observable gross motor behaviors, referred
to in pain research as pain behaviors and the avoidance of health behaviors and
activity (4). Pain can be associated with verbal and nonverbal expressions, such as
grimacing, lying down, the use of supportive devices, which communicate suffering
to the social environment. Fordyce (4) not only introduced the concept of pain
behaviors, he also applied the operant conditioning principle to pain. When pain
behavior is expressed by a patient, desirable things can happen (positive reinforcement) and unpleasant situations can be avoided (avoidance learning). By means of
these environmental influences, pain disability can be maintained long after healing
has occurred. In this paper, we will focus more specifically on the mechanism of
avoidance learning on pain and disability.
238
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
Avoidance Learning
In 1982, Fordyce et al. (5) described how pain behavior may result from avoidance learning. Avoidance refers to "the performance of a behavior which postpones
or averts the presentation of an aversive event" (18). Avoidance learning has long
been considered to underly the formation of many so-called "neurotic" symptoms
(19). In the case of pain, a patient may no longer perform certain activities because
he/she anticipates that these activities increase pain and suffering.
In the acute phase, avoidance behaviors such as resting, limping, or the use
of supportive equipment are effective in reducing suffering from nociception. Later
on, these protective pain and illness behaviors may persist in anticipation of pain,
instead of as a response to it. Longlasting avoidance of motoric activities can have
detrimental consequences, both physically (loss of mobility, muscle strength, and
fitness, possibly resulting in the "disuse syndrome") (20) and psychologically (loss
of self-esteem, deprivation of reinforcers, depression, somatic preoccupation).
Philips and Jahanshahi (21) found that, in a group of headache sufferers, avoidance
was the most prominent behavior reported by these individuals. In their study,
avoidance was not limited to avoidance of movement, but also withdrawal from
social situations. Philips (22) argued in favor of a cognitive theory of avoidance
behavior, rather than the operant theory. She takes the view that avoidance is influenced by the expectancy that further exposure to certain stimuli will promote
pain and suffering. This expectancy is assumed to be based on previous aversive
experiences with the same or similar situations. She also pointed to the similarities
between avoidance behavior displayed by pain patients and that of patients with
excessive fears and phobias, and suggests that "chronic pain and chronic fear--both
aversive experiences which result in avoidance behavior--may share important characteristics" (22, p. 277). Recent studies have focused on the relationship between
fear/anxiety and chronic pain, of which the object of fear has been fear of pain
(23-25), fear of work-related activities (26), and fear of movement that is assumed to
cause (re)injury (27-29).
Fear of Pain
In an attempt to explain how and why some individuals develop a chronic
pain syndrome, Lethem et al. (23) introduced a so-called "fear-avoidance" model.
The central concept of their model is fear of pain. "Confrontation" and "avoidance"
are postulated as the two extreme responses to this fear, of which the former leads
to the reduction of fear over time. The latter, however, leads to the maintenance
or exacerbation of fear, possibly leading to a phobic state. The avoidance results
in the reduction of both social and physical activities, which in turn leads to a number of physical and psychological consequences augmenting the disability. Rose et
al. (30) demonstrated the validity of the fear-avoidance model in three different
chronic pain populations, regardless of the kind of pathology present. In 1992, the
Pain Anxiety Symptoms Scale (PASS; 24) was developed to measure cognitive,
Fear and Pain Disability
239
physiologic, and motoric aspects of fear of pain. The authors found correlations
with measures of anxiety, cognitive errors, depression, and disability. In a second
study (25), the authors showed that, in a group of chronic low-back pain patients,
greater pain-related anxiety was associated with higher predictions of pain and less
range of motion during a procedure involving a passive but painful straight leg
raising test. They also showed that different types of pain-anxiety symptoms have
different relations with pain coping responses as measured with the Coping Strategies Questionnaire (CSQ; 31). Cognitive anxiety responses (e.g., "I find it hard to
concentrate when I hurt") negatively interfered with coping strategy use, whereas
physiological anxiety responses appeared to enhance coping (32).
McCracken and Gross (25) also found a substantial overlap between the CSQfactor "Catastrophizing" and anxiety symptoms. This is of interest as previous studies found strong correlations between catastrophizing attributions and depression.
Fear of Work-Related Activities
CLBP patients may not only fear pain, but also activities that are expected
to cause pain. In this case, fear is hypothesized to generalize to other situations
that are closely linked to the feared stimulus. Vlaeyen (33) found that a group of
50 CLBP patients had mean elevated scores that were clinically significant on the
"social phobia" and "agoraphobia" scales of the Fear Survey Schedule (FSS-III;
34, 35). More specifically, Waddell et al. (26) developed the Fear-Avoidance Beliefs
Questionnaire (FABQ), focusing on the patient's beliefs about how work and physical activity affect his/her low back pain. The FABQ consists of two scales, fearavoidance beliefs of physical activity, and fear-avoidance beliefs of work, of which
the latter was consistently the stronger in predicting work disability. The authors
found that fear-avoidance beliefs about work are strongly related with disability of
daily living and work lost in the past year, and more so than biomedical variables
such as anatomical pattern of pain, time pattern, and severity of pain.
Fear of Movement/(Re)Injury
A more specific kind of fear-avoidance concerns fear of movement and physical activity that is (wrongfully) assumed to cause (re)injury. In accordance with
Lethem et al. (23), Crombez (29) empirically derived a subgroup of 'Avoiders" and
"Confronters" among a sample of CLBP patients using self-report. Although there
were no differences found in gender, age, number of back surgeries, use of medication, and reported pain intensity, "avoiders" reported a higher frequency of pain,
pain of longer duration, more fear of pain, more fear of injury, and more attention
to back sensations than the confronters. When exposed to a maximal performance
test with minimal back muscle involvement (flexion and extension of the knee),
confronters showed a significantly better performance than the avoiders. Regression
analyses revealed that when variance due to gender, age, and body weight was cor-
240
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
rected for, behavioral performance was significantly predicted by both reported fear
of pain and reported fear of injury.
Kori et al. (27) introduced the term "kinesiophobia" (kinesis = movement)
for the condition in which a patient has "an excessive, irrational, and debilitating fear
of physical movement and activity resulting from a feeling of vulnerability to painful
injury or reinjury." These authors also developed the Tampa Scale for Kinesiophobia
(TSK) as a measure for fear of movement/(re)injury. The TSK consists of 17 items,
each of which are provided with a 4-point Likert scale. In a previous study using
a Dutch version of the TSK (36), we found that fear of movement/(re)injury appears
to be related to gender and compensation status, when variance due to current
pain intensity was corrected for. However, even stronger associations were found
with catastrophizing and depression, rather than with pain intensity and pain coping.
Furthermore, subjects who report a high degree of fear of movement/(re)injury
showed more fear and escape/avoidance when exposed to a simple movement consisting of lifting a 5.5-kg bag. They also quit lifting the bag significantly sooner than
the less fearful patients. This study also supports the validity of the TSK-DV in
distinguishing CLBP patients suffering from high and low fear of movement/(re)injury. However, as also noted by Crombez (29), one of the problems is that it remains
difficult to disentangle whether the bad performance is caused by fear or by physical
limitations due to mechanical back problems, or by current pain intensity levels.
In this paper, two studies will be presented. The first study examines the factor
structure of the Tampa Scale for Kinesiophobia (TSK-DV), and the validity of the
factors found. In the second study, an experiment was set up to analyse the value
of fear-avoidance beliefs in predicting disability levels, when biomedical status of
the patient and current pain intensity levels are taken into account. Second, principal determinants of fear-avoidance beliefs were looked for.
STUDY 1: FACTOR STRUCTURE OF THE TSK-DV
Method
Subjects
One hundred and twenty-nine CLBP patients that were admitted to the
Hoensbroek Rehabilitation Center for an inpatient behavioral rehabilitation program were included in this study. The sample consisted of 50 men and 79 women
with a mean age of 40.1 years (SD = 9.0). The duration of pain complaints was
9.9 years (SD = 8.8). Of the total sample, 63.9% received financial disability compensation for at least 1 year, with a mean duration of 3.7 years (SD = 4.7), 38%
had received one or more back surgeries, and 24.8% used supportive equipment
for ambulation. All patients had minimal organic findings or displayed pain complaints that were disproportionate to the demonstrable organic basis of their pain.
Fear and Pain Disability
241
Measures
Pain Intensity. The Pain Rating Index (PRI-total) score of the Dutch version
of the McGill Pain Questionnaire (MPQ-DV; 37, 38) a widely used measure of
pain experience, is used in this study.
Pain Cognitions. The Pain Cognition List (PCL-e; 39) is a 77-item questionnaire aimed at the assessment of distorted pain cognitions and experienced selfcontrol. Five scales are factor-analytically derived: Pain Impact, Catastrophizing,
Outcome-Efficacy, Acquiescence, and Reliance on Health care. For this study only
the subscales Pain impact and Catastrophizing were selected. "Pain impact" reflects
the extent to which the pain interferes with daily activities. "Catastrophizing" refers
to an attentional focus on negative aspects of the patient's situation.
Fear of Movement/(Re)Injury. A Dutch version of the Tampa Scale for Kinesiophobia (27, 36) is a questionnaire that is aimed at the assessment of fear of
(re)injury due to movement. The original 17-item TSK was translated into Dutch
(TSK-DV) by the authors and subsequently corrected by a professional translater.
The same scoring format and keys were maintained. Each item is provided with a
4-point Likert scale with scoring alternatives ranging from "strongly disagree" to
"strongly agree." A total score is calculated after inversion of the individual scores
of items 4, 8, 12, and 16. Based on the data of the current patient sample, following
information underscores the reliability of the TSK-DV. According to the Kolmogorov-Smirnov goodness-of-fit test, the scores on the TSK were normally distributed
(K-S, z = .820, p = 0.512). Cronbach's alpha was 0.77, which is fair. These data
are consistent with an earlier study using a different chronic pain sample (28).
Fear. The Dutch version of the Fear Survey Schedule (FSS-III-R; 34, 35) is
used. The FSS-III-R is a 76-item questionnaire consisting of clusters of phobic complaints: Social Phobia, Agoraphobia, Fear of Bodily Injury, Illness and Death, Fear
of Sex and Aggression, and Fear of Living Organisms. For this study only the cluster
fear of Bodily Injury, Illness, and Death is selected.
Pain Control The Pain Control scale of a Dutch version of the Coping Strategies Questionnaire (31), developed by Spinhoven and Linssen (40) was selected for
this study.
Procedures
The 17 TSK items were subjected to a principal component analysis with
oblique rotation. Items with a factor loading < .40 on all factors were excluded.
For those items having high factor loadings on more than one factor, the item was
assigned to one of the factors based on its contents. For each factor, internal consistency (Cronbach's alpha) is calculated. In order to assess the validity of the TSK
subscales derived, correlations are calculated among the subscales and a number
of concurrent measures including catastrophizing, pain impact, pain control, pain
intensity, and fear.
242
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
Table I. Component Structure of the TSK-DV: Components, Internal Consistency (Cronbach's
Alpha), Correlation with TSK Total Score (r'rSK-TOT),and Component Label with Respective
Items
Component
Alpha rTSK.TOTLabel
.71
.72*
TSK-H: Harm
I wouldn't have this much pain if there weren't something
11.
potentially dangerous going on in my body.
3.
My body is telling me I have something dangerously wrong.
6.
My accident has put my body at risk for the rest of my life.
II
.63
.56*
TSK-F: Fear of (re)injury
9.
I am afraid that I might injure myself accidentally.
1.
I am afraid that I might injure myself if I exercise
Ill
.53
.38*
TSK-E: Importance of exercise
14.
It's really not safe for a person with a condition like mine
to be physically active.
4.a
My pain would probably be relieved if I were to exercise.
12.a
Although my condition is painful, I would be better off if I
were physically active.
IV
.61
.57*
TSK-A: Avoidance of activity
2.
If I were to try to overcome it, my pain would increase.
13.
Pain lets me know when to stop exercising so that I don't
injure myself.
15.
I can't do all the things normal people do because it's too
easy for me to get injured.
10.
Simply being careful that I do not make any unnecessary
movements is the safest thing I can do to prevent my pain
from worsening.
aFor these items, scores are inversed.
*p _<.001 (one-tailed).
Results
B a s e d on the ~2-test for the sufficient n u m b e r of factors extracted and the
interpretability of the factors, the solution of four factors was chosen (Table I) which
cumulatively a c c o u n t e d for 36.2% of the total variance (15.5%, 5.6%, 8.6%, and
6.5%, respectively). Factors were labeled following the c o m m o n p r o c e d u r e of giving
the greatest c o n s i d e r a t i o n to items with high loadings on each factor.
T h e following labels were assigned: Harm (TSK-H), Fear of (re)injury (TSK-F),
Importance of exercise (TSK-E), and Avoidance of activity (TSK-A). T h e internal consistency of the factors ranges from .53 (TSK-E) to .71 (TSK-H) and are lower t h a n
alpha of the TSK-total score (.77). Intercorrelations a m o n g the T S K - D V factors
range from .02 to (-).31 (Table II), which suggests that the factors are not totally
i n d e p e n d e n t . T h e p a t t e r n of correlations with concurrent m e a s u r e s (Table I I I ) suggests that the T S K - H and T S K - F factors are most reflective of the construct of fear
of movement/(re)injury. A l t h o u g h they are not strongly c o r r e l a t e d (r = .23) their
p a t t e r n of correlations with the concurrent m e a s u r e s are quite similar. T h e correlations p r e s e n t e d in Table I I I further suggests that factors T S K - E and T S K - A s e e m
to m e a s u r e different constructs. A n o t h e r interesting finding is that no significant
Fear and Pain Disability
243
Table IL Intercorrelations Among TSK-DV Subscales
TSK-harm
TSK-fear of (re)injury
TSK-exercise
TSK-F
TSK-E
TSK-A
-.23
.30
-.15
.21
-.31
.02
Table IlL Correlations Among TSK Subscales and Pain Impact (PCL-e), Catastrophizing (PCL-e),
Outcome-Efficacy (PCL-e), Acquiescence (PCL-e), Reliance on Health Care (PCLoe), Pain Control
(CSQ), Pain Intensity (MPQ), and Fear of Bodily Injury, Illness and Death (FSS-III-R)
Pain impact
Catastrophizing
Pain intensity
Pain control
Fear of blood, injury
TSK-H
TSK-F
TSK-E
.23*
.47"*
.24*
.02
.32**
.38**
.52"*
.25*
.09
.37**
.01
.06
.11
-.03
-.15
TSK-A
.13
.35**
.16
-.16
.14
TSK-TOT
.27*
.54**
.21"
-.10
.32**
*p < .01.
**p < .001 (one-tailed).
correlations are found between Pain Control and any TSK subscale, which suggests
that the T S K taps a particular aspect of beliefs that is more related to the interpretation, attribution or appraisal of the situation, rather than to expectancies about
self-efficacy and pain control. Despite the four-factor solution, arguments can be
formultated in favor of the use of the TSK total score, rather than the factors.
These are: the relatively high intercorrelations among some of the factors, the more
favorable internal consistency of the total score, and the good construct validity of
the total score as displayed by the pattern of correlations with concurrent measures.
STUDY 2: DETERMINANTS OF PAIN DISABILITY AND FEAR OF
MOVEMENT/(RE) INJURY
This study was first aimed at examining whether fear of movement/(re)injury
is a major predictor of pain disability, as compared with current pain intensity levels,
catatstrophizing and levels of impairment, after controlling for demographic variables. The second aim of this study was to examine whether catastrophizing, rather
than current-pain intensity and levels of impairment, is predictive of fear of movement/(re)injury.
Method
Subjects
Thirty-three chronic low back pain patients who were on a waiting list for a
behavioral rehabilitation program agreed to participate in the experiment. The
244
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
group consisted of 17 female and 16 male patients with a mean age of 37.4 years
(SD = 9.2, range = 22-53).
The mean duration of their pain complaints was 7.6 years (SD --- 8.2; range
= 0.7-29). As is study 1, all patients had minimal demonstrable organic findings.
Measures
Level of Impairment. The Medical Evaluation and Diagnostic Information
Coding system (MEDICS; 41) was used by a rehabilitation physician to quantify
the biomedical signs and symptoms that may be related to the patients' reports of
pain. MEDICS was completed after examination of the medical chart of the patient.
For this study, the total pathology score using the medical concensus weights reported by Rudy et al. (41) is used.
Pain Intensity. The Visual Analog Scale (VAS; 42), a widely used measure of
pain experience, is used in this study. Patients were asked to rate the mean pain
intensity over the last week. A 10 centimeter line was provided with written anchors
at the two extremes: "no pain at all" and "the worst pain ever experienced."
Pain Cognitions. For this study, the subscale Catastrophizing of the Pain Cognition List (PCL-e; 39) is selected.
Fear. A Dutch version of the Tampa Scale for Kinesiophobia (TSK-DV; 36) is
a questionnaire that is used for the assessment of fear of (re)injury due to movement.
Level of Disability. One of the best developed self-report measures of disability
in activities of daily living, the Roland Disability Questionnaire (RDQ; 43) is used
in this study.
Procedure
When entering the laboratory, all patients were given brief information about
the experiment. Subsequently they were requested to complete the questionnaires.
Then the subjects were asked to perform seven activities that were part of another
study examining the influence of prior expectations on behavioral performance (44).
The experiment ended with the completion of a number of questions regarding
their performance, and their beliefs about fear of movement/(re)injury.
Statistics
Pearson correlation coefficients among TSK-DV, RDQ, and other variables
are calculated. T-tests for the differences between low-disabled and high-disabled
subjects (RDQ), and between low-fear and high-fear subjects (TSK-DV) based on
a median split for RDQ, and a cut-off score of 37 for TSK-DV (36) are carried
out for the independent variables.
Hierarchical multiple regression analyses with a stepwise forward inclusion
method with TSK-Total score and RDQ as dependent variables were used. Pain
Fear and Pain Disability
245
duration and gender were entered into the equation first, to test whether one of
the other independent variables (Medics, Pain intensity, Catastrophizing) would
contribute significantly to the variance in the dependent variable after controlling
for these socio-demographic variables.
Results
Question 1
As displayed in Table IV, RDQ correlates significantly only with TSK-DV. Correlations with gender and compensation status were low (r= -.17 and .13, respectively). The only significant differences between the high and low disability subjects
was on TSK-DV and Catastrophizing (Table V). Consequently, Table VI shows that
among the variables entered in the regression model, fear of movement/(re)injury
is the best predictor of pain disability as measured by the RDQ. Of interest is that
catastrophizing, which is predictive for fear, does not directly predict pain disability.
However, the percentage of explained variance is rather modest (13%). On the
other hand, pain intensity and biomedical findings were not predictive of pain disability.
Table IV. Means, SD for Age, Duration of Pain (Years), Current Pain Intensity (VAS),
Catastrophizing (PCL-e), Level of Impairment (Medics), Fear of Movement/(Re)Injury
(TSK-DV), and Pain Disability (RDQ), and Pearson Correlation Coefficients r with
TSK-DV and RDQ
Age (years)
Pain duration (years)
Pain intensity (VAS)
Catastrophizing (PCL-e)
Impairment (medics)
Fear of movement (TSK-DV)
Pain disability (RDQ)
Mean
SD
37.4
7.6
51.6
48.2
-.70
40.4
13.8
9.2
8.2
22.2
13.1
.78
6.6
4.2
r with TSK-DV r with RDQ
-.26
-.45*
.00
.49*
.15
-.49*
.03
-.33
.23
.29
.04
.49*
--
*p < 0.01 (one-tailed).
Table V. t-Tests for the Differences Between Low-Disabled Subjects (RDQ _< 15) and High-Disabled
Subjects (RDQ > 15)
Low-disability subjects
High-disability subjects
(n = 18)
(n = 15)
Mean
Age (years)
Pain duration (years)
Pain intensity (VAS)
Catastrophizing (PCL-e)
Impairment (medics)
Fear of movement (TSK-DV)
Pain disability (RDQ)
36.7
7.4
45.4
44.1
-.59
38.1
10.7
SD
Mean
SD
9.5
7.0
20.7
14.3
.67
7.0
3.0
38.2
7.9
59.0
53.0
-.82
43.3
17.5
9.1
9.7
22.4
9.9
.88
4.9
1.4
NS
NS
NS
.050
NS
.022
.000
246
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
Table VI. Summary of Stepwise Hierarchical Regression Analysis of Pain Disability (RDQ), with
Pain Duration and Gender Entered in the First Step and Variables Fear of Movement/(Re)Injury
(TSK-TOT), Catastrophizing (PCL-e), Pain Intensity (VAS), and Biomedical Findings (MEDICS)
Tested with a Forward Inclusion Methoda
Ad'.ll
Step
Independent variables
R2
R2
Beta
1.
Pain duration
Gender
.04
.12
-.37
.07
2.
Pain duration
Gender
Fear of movement/(re)injury (TSK-TOT)
.17
.27
-.19
.12
.44*
"Dependent variable: Level of pain disability (RDQ). Variables not in the equation: pain intensity (VAS),
catastrophizing (PCL-e), biomedical findings (MEDICS).
*p _<0.05.
Table VII. t-Tests for the Differences Between Low-Fear Subjects (TSK-DV _<37) and High-Fear
Subjects (TSK-DV > 37)
Age (years)
Pain duration (years)
Pain intensity (VAS)
Catastrophizing (PCL-e)
Impairment (medics)
Fear of movement (TSK-DV)
Pain disability (RDQ)
Low-fear subjects
(n = 11)
Mean
SD
High-fear subjects
(n = 22)
Mean
SD
39.2
9.6
44.4
41.5
-.84
33.3
10.7
36.5
6.6
55.2
51.5
-.64
44.0
15.3
10.1
8.2
16.0
11.9
.55
3.4
3.8
8.9
8.2
24.3
12.6
.86
4.6
3.5
NS
NS
NS
.038
NS
.000
.002
Question 2
As displayed in Table IV, and consistent with previous findings, TSK-DV correlates significantly with catastrophizing and pain disability, and negatively with pain
duration. There was a modest correlation with gender (r=.20) but, in contrast to
previous findings (36), not with compensation status (r=.08). Differences between
high and low fearful subjects are found for measures of catastrophizing and pain
disability (Table VII). As shown in Table VIII, fear of movement/(re)injury can best
be predicted by catastrophizing, which accounted for an additional 17% of the variance, beyond the 15% prediction by gender and pain duration simultaneously. Pain
intensity and biomedical findings did not add any predictive value to the just-mentioned variables.
DISCUSSION
Avoidance behavior is postulated to be one of the mechanisms in sustaining
chronic pain disability. In the acute pain situation, avoidance of daily activities that
Fear and Pain Disability
247
VIII. Summary of Stepwise Hierarchical Regression Analysisof Fear of Movement
(TSK-TOT), with Pain Duration and Gender Entered in the First Step and Variables
Catastrophizing (PCL-e), Pain Intensity(VAS), and BiomedicalFindings (MEDICS)
Tested with a Forward InclusionMethod"
Table
md'.ll
Step Independentvariables
Rg
R2
Beta
1.
Painduration
Gender
.15
.21
-.40
-.11
2.
Painduration
Gender
Catastrophizing (PCL-e)
.32
.40
-.28
-.19
.45*
aDependent variable: Fear of movement/(re)injury(TSK-DV). Variables not in the equation: pain
intensity (VAS), biomedical findings(MEDICS).
*p _<0.05.
increase pain is a spontaneous and adaptive reaction of the individual (45); it usually
allows the healing process to occur. In chronic pain patients, however, avoidance
behavior appears to persist beyond the expected healing time. One of the reasons
that avoidance behaviors persist is not only the short-term effects of reduced suffering, but also the influence of certain beliefs and expectations (22). If the individual believes that further exposure to certain stimuli will increase pain and
suffering, avoidance or escape will be likely to occur. So far, little scientific attention
has been drawn to the specific beliefs that are related to avoidance. In this article,
a particular belief is put forward that is hypothesized to enhance avoidance, namely
the expectation that movement can cause (re)injury, and thus increased suffering.
The first study shows that the TSK-DV is composed of four factors: Harm,
Fear of injury, Importance of exercise, and Avoidance, which are not totally independent. Based on both the intercorrelations among the four factors, the reliability
coefficients, and the validity data it can be concluded that the TSK-DV can be used
as a single factor as well. The second study revealed that fear of movement/(re)injury is the best predictor for self-reported disability levels, rather than biomedical
findings, pain intensity levels, and catastrophizing. The second finding was that
catastrophizing, rather than pain intensity ratings and biomedical findings is predictive of fear of movement/(re)injury. An unexpected finding is the negative correlation between fear of movement/(re)injury and pain duration, and would suggest
that this particular fear extinguishes with time, or that more chronically disabled
patients are less likely to acknowledge fear. Future studies need to clarify this issue.
Because of the relatively small sample size, the unexpected association may be coincidental as well.
Although positive correlations may not be confused with causal effects, both
findings underscore parts of a cognitive-behavioral model displayed in Fig. 2. This
model represents the mechanism how fear of movement/(re)injury possibly contributes to the maintenance of chronic pain disability in chronic low back pain, starting
with the injury occuring during the acute phase. The painful experiences, that are
intensified during movement, will elicit catastrophizing cognitions in some individuals and more adaptive cognitions in others.
248
Vlaeyen, Kole.Snijders, Rotteveel, Ruesink, and Heuts
As demonstrated in study 2, catastrophizing appears to be a potent predictor
of fear of movement/(re)injury. Still unknown is whether castastrophizing is a traitlike disposition that triggers fear of movement/(re)injury when the individual encounters an acute pain episode, or whether catastrophizing is merely part of the
cognitive responses associated with fear of movement/(re)injury. In the first case,
catastrophizing individuals may focus more on the negative aspects of the acute
pain situation, and are more likely to interpret physical arousal as pain signals. As
a result of this attentional focus, interoceptive information that often is associated
with movement is more easily noticed and perhaps interpreted as "dangerous" or
"signaling (re)injury." The opposite might be true as well. As Turk and Holzman
(46) have suggested, fear-avoidance beliefs may especially be the case when the
original acute pain problem resulted from traumatic injury. Indeed, when the subjects from study 2 were asked about the circumstances of the acute pain, patients
who reported traumatic pain onset (sudden onset associated with being frightened)
scored higher on catastrophizing (but not significantly) and on the TSK-DV (significantly) than subjects who retrospectively reported that the pain complaints
started gradually. The recent prospective study by Burton et al. (47), searching for
predictors of chronicity at 1 year is worth mentioning in this context. These researchers found that catastrophizing, as measured by the CSQ, was the most powerful predictor, and almost 7 times more important than the best of the clinical
and historical variables for the acute back pain patients.
Fear of movement/(re)injury subsequently leads to increased avoidance (as
demonstrated by Crombez (29) and Vlaeyen et al. (36)), and in the long run to
disuse, depression and increased disability (22, 48). Both depression and disuse are
known to be associated with decreasing pain tolerance levels (49, 50), and hence
promoting the painful experiences. In patients with adaptive cognitions, confrontation rather than avoidance is likely to occur, promoting health behaviors and early
recovery.
This study, as the studies by Rose et al. (30) and Waddell et al. (26), provides
support for the validity of the fear-avoidance concept. It should be noted, however,
that these are cross-sectional in nature, leaving the question whether fear of movement/(re)injury is secondary to the experience of low back pain, or that it is one
of the determinants of becoming a chronic pain patient. Roland and Morris (43)
and Gamsa (51), for example, have suggested that emotional distress in pain patients is more likely to be a consequence, rather than an antecedent of the chronic
pain problem. In a recent prospective study, Klenerman et al. (11) found the opposite to be true. They collected both psychological and biomedical measures from
a sample of 300 acute low back pain patients within one week of presentation, and
at 2 months, as to predict 12-month outcome. The data showed that subjects who
had not recovered by 2 months (7.3%) became chronic low back pain patients.
Moreover, fear of pain turned out to be one of the most powerful predictors of
chronicity. This recent study, as well as the study of Burton et al. (47) support the
cognitive-behavioral model outlined in Fig. 2, suggesting that psychological variables
can act both as antecedents and consequences, reinforcing the pain problem in a
complex chain of events with feedback loops.
Fear and Pain Disability
249
injury
oilily,
I
Disuse
I
/Depre~l~ _~. _ l
Avoidance
PeJnfulexpedenoes
Recovery
l
ConfrontalJon
+\ / C,4~lTophlzlng
]Fig,2. Cognitive-behaviomodel
ral of fearof movement/(re)injury.
Fear of movement/(re)injury may also influence patterns of performance of
workers with low back pain in an occupational setting. Clinicians are often requested to make judgments about the present and future functional capacity of
patients on the basis of dynamometry. The assumption hereby is that lumbar (isokinetic) dynamometry provides objective and unbiased measures and that it can
quantify maximal functional capacity. Menard et al. (52), for example, found a difference in the pattern of dynamometry in two groups of low back pain patients
who differed only in the propensity of abnormal illness behavior (as indicated by
the Waddell score), and proposed that fear of pain of movement might be one of
the possible explanations. The plausability of this explanation is corroborated by
earlier studies (29, 36) in which a relation between fear of movement/(re)injury
and behavioral performance is demonstrated. This means that a valid assessment
of functional capacity cannot be carried out without controlling for fear-avoidance
beliefs.
In occupational rehabilitation, early identification of catastrophizing and fear
of movement/(re)injury appears to be important in preventing chronic back disability. The TSK-DV has the potential to identify a subgroup of CLBP patients whose
disability is mainly determined by the specific fear of movement/(re)injury and not
by current pain intensity, the underlying organic pathology, or nocieeption. For this
subgroup, a specific treatment might be applied. Although cognitive-perceptual factors, and catastrophizing in particular, are associated with fear of movement, didactic lectures, education, or rational argument will not be as effective as more
behavioral forms of intervention. As Bandura (53) points out, symbolic evidence is
not nearly as credible as first-hand evidence. For a fearful patient, it is far more
convincing to actually see him/herself behaving differently than it is to be told that
he/she is capable of behaving differently. For individuals suffering from phobias,
graded exposure to the feared stimulus has proven to be a most effective treatment
(54). Consequently, for this CLBP subgroup, a more systematic application of
graded exposure to movement, such as described by Fordyce et al. (5) and Lind-
250
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
str6m et al. (55), is warranted. The movements that are chosen for such an exposure
can best be matched with the work-related activities that are needed to resume
the job responsibilities after the sick leave period. Randomized prospective research studies including cost-effectiveness analyses demonstrating the impact of
such a customized approach are likely to be promising, and badly needed. The
available knowledge gained both in the predictors of disability and in developing
behavioral rehabilitation programs should be applied to the field of secondary prevention (56). Waiting until pain problems have fully developed into chronic and
almost irreversable situations is ethically and economically unjustifiable.
ACKNOWLEDGMENTS
The authors wish to thank the staff of the department of Pain Rehabilitation
and Rheumatology of the Lucas Foundation for Rehabilitation, Hoensbroek, who
contributed considerably to the clinical management of the patients included in this
study. We also wish to acknowledge the assitance of Nienke Haga of the Rehabilitation Center "Blixembosch" at Eindhoven, Robert Miihlig of the De Wever Hospital at Heeden, and Huub Vonken and Wil Sillen of the outpatient clinic of the
Lucas Foundation for Rehabilitation for the referrals of patients that were included
in the second study. Thanks are also extended to Arnoud Arntz and Wip Bakx for
their advice at various stages of the study, and to Geert Crombez, Jolanda van
Haastregt, and an anonymous reviewer for their useful comments on an earlier
version of this article. This research was partly supported by Grant O G 91-088 of
the Dutch Insurance Council.
REFERENCES
1. Spitzer WO, LeBlanc FE, Dupuis M. Scientific approach to the assessment and management of
activity-related spinal disorders: Report of the Quebec task Force on Spinal Disorders. Spine 1987;
12 (Suppl. 7): S1-$59.
2. CrookJ, MoldofskyH. The probability of recovery and return to work from work disability as a
function of time. Quality Life Res 1994; 3 (Suppl. 1): 97-109.
3. NachemsonAL. Newest knowledge of low back pain. Clin Orthop 1992; 279: 8-20.
4. FordyceWE. Behavioral methods for chronic pain and illness. St. Louis: Mosby, 1976.
5. FordyceWE, Shelton JL, Dundore DE. The modificationof avoidance learning in pain behaviors.
J Behav Med 1982; 5: 405-414.
6. Waddell G. A new clinical model for the treatment of low back pain. Spine 1987; 12: 632-644.
7. Waddell G, Main CA, Morris EW, DiPaola MP, Gray ICM. Chronic low back pain, psychologic
distress and illness behaviour. Spine 1984; 9: 209-213.
8. Turk DC, Meichenbaum D, Genest M. Pain and behavioral medicine. A cognitive-behavioral
perspective. New York: Guilford Press, 1983.
9. DeyoR, Diehl A, Rosenthal M. How many days of bed rest for acute low back pain? New Engl J
Med 1986; 315: 1064-1070.
10. Philips HC, Grant L. The prevention of chronic pain and disability: A preliminary investigation.
Behav Res Ther 1991; 29: 443-450.
11. Klenerman L, Slade PD, Stanley IM, Pennie B, Reilly JP, Atkinson LE, Troup JDG, Rose MJ.
The prediction of chronicity in patients with an acute attack of low back pain in a general practice
setting. Spine 1995; 4: 478-484.
Fear and Pain Disability
251
12. Vlaeyen JWS, Snijders A_I~J, Schuerman JA, van Eek H, Groenman NH, Bremer JJCB. Chronic
pain and the three-systems model of emotions. A critical examination. Crit Rev Phys Reh Med 1989;
2: 67-76.
13. Flor H, Birbaumer N, Turk DC. The psychobiology of chronic pain. Adv Behav Res Ther 1990; 121:
47-84.
14. Feuerstein M. A multidisciplinary approach to the prevention, evaluation, and management of work
disability. J Occup Rehab 1991; 1: 5-12.
15. Pilowsky I. Pain and illness behaviour: Assessment and management. In: Wall PD, Melzack R, eds.
Textbook of pain. Edinburgh: Churchill Livingstone, 1994.
16. Cioffi D. Beyond attentional strategies: A cognitive-perceptual model of somatic interpretation.
Psychol Bull 1991; 109: 25-41.
17. Ciccone DS, Grzesiak RC. Cognitive dimensions of chronic pain. Soc Sci Med 1984; 12: 1339-1345.
18. Kazdin AE. Behavior modification in applied settings, revised Ed. Homewood, Illinois: Dorsey Press
1980.
19. Kanfer FH, Phillips JS. Learning foundations of behavior therapy. New York: Wiley & Sons, 1970.
20. Bortz WM. The disuse syndrome. West J Med 1984; 141: 691-694.
21. Philips HC, Jahanshahi M. The components of pain behaviour report. Behav Res Ther 1986; 24:
117-125.
22. Philips HC. Avoidance behaviour and its role in sustaining chronic pain. Behav Res Ther 1987; 25:
273-279.
23. Lethem J, Slade PD, Troup JDG, Bentley G. Outline of a fear-avoidance model of exaggerated
pain perceptions. Behav Res Ther 1983; 21: 401-408.
24. McCracken LM, Zayfert C, Gross RT. The Pain Anxiety Symptoms Scale: Development and
validation of a scale to measure fear of pain. Pain 1992; 50: 67-73.
25. McCracken LM, Gross RT. Does anxiety affect coping with pain? Clin J Pain 1993; 9: 253-259.
26. Waddell G, Newton M, Henderson I, Somerville D, Main C. A Fear-Avoidance Beliefs
Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability.
Pain 1993; 52: 157-168.
27. Kori SH, Miller RP, Todd DD. Kinisophobia: A new view of chronic pain behavior. Pain
Management 1990; Jan/Feb: 35-43.
28. Kole-Snijders AMJ, Vlaeyen JWS, Boeren RGB, Schuerman JA, Eek van H. Validity of the Tampa
Scale for Kinisophobia--Dutch version (TSK--DV) for chronic low back pain patients. Paper
presented at the 7th Worm Congress on Pain, August 22-27, 1993, Paris.
29. Crombez G. Pijnmodulatie Door Anticipatie (Painmodulation Through Anticipation). Doctoral
dissertation, University of Leuven, Belgium, 1994.
30. Rose M, Klenerman L Atchinson L, Slade PD. An application of the fear-avoidance model to
three chronic pain problems. Behav Res Ther 1992; 30: 359-365.
31. Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients:
Relationship to patient characteristics and current adjustment. Pain 1983; 17: 33-44.
32. McCracken LM, Gross RT, Sorg PJ, Edmands TA. Prediction of pain in patients with chronic low
back pain: Effects of inaccurate prediction and pain-related anxiety. Behav Res Ther 1993; 31:
647-652.
33. Vlaeyen JWS. Chronic Low Back Pain. Assessment and Treatment from a Behavioral Rehabilitation
Perspective. Doctoral dissertation. University of Limburg, Maastricht, The Netherlands, 1991.
34. Wolpe J, Lang PJ. A fear schedule for use in behavior therapy. Behav Res Ther 1964; 2: 27-30.
35. Arrindell WA, Solyom C, Ledwidge B, Van der Ende J, Hageman WJJM, Solyom L, Zaitman A.
Cross-national validity of the five-components model of self-assessed fears: Canadian psychiatric
outpatients data vs Dutch target ratings on the Fear Survey Schedule-III. Adv Behav Res Ther 1990;
12: 101-12g.
36. Vlaeyen JWS, Kole-Snijders AMJ, Boeren RGB, van Eek H. Fear of movement/(re)injury in chronic
low back pain and its relation to behavioral performance. Pain 1995; 62: 363-372.
37. Melzack R. The McGill Pain Questionnaire. Major properties and scoring methods. Pain 1975; 1:
277-299.
38. Van der Kloot WA, Vertommen H. De MPQ-DLV. Een standaard Nederlandstalige versie van de
McGill Pain Questionnaire. Achtergronden en handleiding. Lisse: Swets & Zeitlinger, 1989.
39. Vlaeyen JWS, Geurts SM, Kole-Snijders AM J, Schuerman JA, Groenman NH, van Eek H. What
do chronic pain patients think of their pain? Towards a pain cognition questionnaire. Brit J Clin
Psychol 1990; 29: 383-394.
40. Spinhoven Ph, Linssen ACG. Behavioral treatment of chronic low back pain. Relation to coping
strategy use to outcome. Pain 1991; 45: 29-34.
252
Vlaeyen, Kole-Snijders, Rotteveel, Ruesink, and Heuts
41. Rudy TR, Turk DC, Brena SF, Stieg R L Brody MC. Quantification of biomedical findings of
chronic pain patients: Development of an index of pathology. Pain 1990; 42: 167-182.
42. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC,
Melzack R, eds. Handbook of pain assessment. New York: Guilford Press, 1992.
43. Roland M, Morris R. A study of the natural history of back pain. Part I: Development of a reliable
and sensitive measure of disability in low back pain. Spine 1983; 8: 141-144.
44. Rotteveel A. Fear of pain or pain as a consequence of fear. The role of kinesiophobia in the
maintenance of chronic pain. Unpublished manuscript, 1995.
45. Wall PD. On the relation of injury to pain. Pain 1979; 6: 253-264.
46. Turk DC, Holzman AD. Chronic pain: Interfaces among physical, psychological and social
parameters. In: Holzman AD, Turk, DC, eds. Pain management. A handbook of psychological
treatment approaches. New York: Pergamon, 1986.
47. Burton AK, Tillotson KM, Main CA, Hollis S. Psychosocial predictors of outcome in acute and
subchronic low back trouble. Spine 1995; 20: 722-728.
48. Council JR, Ahem DK, Follick MJ, Kline CL. Expectancies and functional impairment in chronic
low back pain. Pain 1988; 33: 323-331.
49. Romano JM, Turner JA. Chronic pain and depression. Does the evidence support a relationship?
Psyehol Bull 1985; 97: 18-34.
50. McQuade KJ, Turner JA, Buchner DM. Physical fitness and chronic low back pain. Clin Orthop
Rel Res 1988; 233: 198-204.
51. Gamsa A. Is emotional disturbance a precipitator or a consequence of chronic pain? Pain 1990;
42: 183-195.
52. Menard MR, Cooke C, Locke SR, Beach GN, Butler TB. Pattern of performance in workers with
low back pain during a comprehensive motor performance evaluation. Spine 1994; 2: 1359-1366.
53. Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev 1977, 84:
191-215.
54. Butler G. Phobic disorders. In: Hawton et al., eds. Cognitive behaviour therapy for psychiatric
problems. A practical guide. Oxford: Oxford Medical Publications, 1989.
55. Lindstrfm I, Ohlund C, Eek C, Wallin L, Peterson L Fordyce WE, Nachemson AL. The effect of
graded activity on patients with sub-acute low back pain: A randomized prospective clinical study
with an operant conditioning behavioral approach. Phys Ther 1992; 72: 279-290.
56. Linton SJ. Chronic pain: The case for prevention. Behav Res Ther 1987; 4: 313-317.
You might also like
- Role of Kinesiophobia On Pain, Disability and Quality LUQUEDocument44 pagesRole of Kinesiophobia On Pain, Disability and Quality LUQUECelia CaballeroNo ratings yet
- Management L Low Back PainDocument7 pagesManagement L Low Back PainelsyamelindaNo ratings yet
- Environmental Modifications: Nakul RangaDocument42 pagesEnvironmental Modifications: Nakul Rangataniamahapatra1No ratings yet
- Spinal Cord DisordersDocument50 pagesSpinal Cord DisordersIsaac Mwangi100% (1)
- Patterns of Triangular Fibrocartilage Complex (TFCC) Injury Associated WithDocument7 pagesPatterns of Triangular Fibrocartilage Complex (TFCC) Injury Associated WithCésarLópezNo ratings yet
- Stroke Rehab, Info Proving PNF To Improve Upper Limb Function - FullDocument6 pagesStroke Rehab, Info Proving PNF To Improve Upper Limb Function - FullThomas CorbettNo ratings yet
- Malignant Spinal Cord Compression - Dealing The Most Common - MetsDocument60 pagesMalignant Spinal Cord Compression - Dealing The Most Common - MetsDr Sasikumar Sambasivam100% (2)
- 268 Full PDFDocument1 page268 Full PDFRamkeshmaraviNo ratings yet
- JOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFDocument33 pagesJOSPT Shoulder Pain and Mobility Deficitis Adhesive Capsulitis PDFAbdul Wahid ShaikhNo ratings yet
- Michael W. Whittle BSC MSC MB BS PHD - An Introduction To Gait Analysis, 4th Ed. (2007)Document30 pagesMichael W. Whittle BSC MSC MB BS PHD - An Introduction To Gait Analysis, 4th Ed. (2007)Andrew NarridoNo ratings yet
- Neurogenic BowlDocument21 pagesNeurogenic BowlFaridatul IsniyahNo ratings yet
- Pathomechanics of the Shoulder: Factors, Causes, EffectsDocument27 pagesPathomechanics of the Shoulder: Factors, Causes, EffectsVenkat RamanaNo ratings yet
- The Timed Up & Go - A Test of Basic Functional Mobility For Frail Elderly Persons. lAGSDocument7 pagesThe Timed Up & Go - A Test of Basic Functional Mobility For Frail Elderly Persons. lAGSJose Fernando Díez ConchaNo ratings yet
- Mirror Box Presentation Handout EditedDocument4 pagesMirror Box Presentation Handout Editedapi-364398898No ratings yet
- Magee 6th Edition - OPA - Copyright PageDocument1 pageMagee 6th Edition - OPA - Copyright PageRonny Araya AbarcaNo ratings yet
- Chapter 1 - Intro Current Concepts and Clinical Decision Making in Electrotherapy PDFDocument7 pagesChapter 1 - Intro Current Concepts and Clinical Decision Making in Electrotherapy PDFTracy Magpoc0% (1)
- The Effectiveness of Trunk Training On Trunk Control, Sitting and Standing Balance and Mobility Post-Stroke: A Systematic Review and Meta-AnalysisDocument11 pagesThe Effectiveness of Trunk Training On Trunk Control, Sitting and Standing Balance and Mobility Post-Stroke: A Systematic Review and Meta-AnalysisMarcela NunesNo ratings yet
- PDF Document PDFDocument8 pagesPDF Document PDFDhruv AgrawalNo ratings yet
- De Quervain SyndromeDocument5 pagesDe Quervain Syndromebangla018No ratings yet
- Cyriax IntroDocument14 pagesCyriax IntrodrrajmptnNo ratings yet
- Scales To Assess Gross Motor Function in Stroke Patients: A Systematic ReviewDocument10 pagesScales To Assess Gross Motor Function in Stroke Patients: A Systematic ReviewAngie TarazonaNo ratings yet
- Therapeutic Management of Knee Osteoarthritis: BY PT H N AbdullateefDocument96 pagesTherapeutic Management of Knee Osteoarthritis: BY PT H N AbdullateefMaida FitrianiNo ratings yet
- MUHS - BPT - 2017 - 4 - Winter - B.P.TH - 51411 Musculoskeletal PhysiotherapyDocument2 pagesMUHS - BPT - 2017 - 4 - Winter - B.P.TH - 51411 Musculoskeletal PhysiotherapyYuvraj AtholeNo ratings yet
- PathomechanicsDocument8 pagesPathomechanicsMike B AndersonNo ratings yet
- PNF Techniques 3rd SessionDocument59 pagesPNF Techniques 3rd SessionBasma T. Zewar100% (1)
- Physiotherapy Scope of Practice-Article PDFDocument3 pagesPhysiotherapy Scope of Practice-Article PDFeins_mptNo ratings yet
- OT Code of Ethics 2015Document8 pagesOT Code of Ethics 2015Ays OlarteNo ratings yet
- Low Back PainDocument8 pagesLow Back PainLev KalikaNo ratings yet
- A Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureDocument14 pagesA Proposed Evidence-Based Shoulder Special Testing Examination Algorithm - Clinical Utility Based On A Systematic Review of The LiteratureAfonso MacedoNo ratings yet
- Rehabilitation AmbulationDocument14 pagesRehabilitation AmbulationDeborah SalinasNo ratings yet
- Rehab of Patients With HemiplegiaDocument2 pagesRehab of Patients With HemiplegiaMilijana D. DelevićNo ratings yet
- Classification of Upper Limb Orthosis: Presented To: Miss Soonhan Rani Presented By: Syeda Zoha Hassan TaqviDocument16 pagesClassification of Upper Limb Orthosis: Presented To: Miss Soonhan Rani Presented By: Syeda Zoha Hassan Taqvizoha hassanNo ratings yet
- Intro To Physical AgentsDocument21 pagesIntro To Physical AgentsPaula ColeenNo ratings yet
- Role of Occupational Therapists in CBRDocument16 pagesRole of Occupational Therapists in CBRFEBIN RAJU100% (1)
- Pain and Pain Gate Control MechanismDocument17 pagesPain and Pain Gate Control MechanismKapil LakhwaraNo ratings yet
- PREVENT NEUROMUSCULAR CONDITIONSDocument37 pagesPREVENT NEUROMUSCULAR CONDITIONSArham ShamsiNo ratings yet
- Pre-Prosthetic Rehabilitation Involving Strength and Positional TDocument13 pagesPre-Prosthetic Rehabilitation Involving Strength and Positional TditaNo ratings yet
- Industrial HealthDocument22 pagesIndustrial HealthPraveen Kumar RNo ratings yet
- Design of A Hand OrthosisDocument251 pagesDesign of A Hand OrthosisIsrael BlancoNo ratings yet
- Lower Back Pain: Healthshare Information For Guided Patient ManagementDocument12 pagesLower Back Pain: Healthshare Information For Guided Patient Managementkovi mNo ratings yet
- PANat - Thetrical - Air Splints - Talas Pneumaticas Margaret JohnstoneDocument44 pagesPANat - Thetrical - Air Splints - Talas Pneumaticas Margaret JohnstonePedro GouveiaNo ratings yet
- CAMERON - Physical Agents in Rehabilitation-231-236Document6 pagesCAMERON - Physical Agents in Rehabilitation-231-236deasyNo ratings yet
- Introduction of Physical MedicineDocument39 pagesIntroduction of Physical MedicineDrMd Nurul Hoque MiahNo ratings yet
- Orthosisofhandppt 181202162551Document65 pagesOrthosisofhandppt 181202162551Khageswar SamalNo ratings yet
- Basic of Geriatrics and Internal Medicine For PhysiotherapistDocument128 pagesBasic of Geriatrics and Internal Medicine For PhysiotherapistDoha EbedNo ratings yet
- TyrosolutionDocument20 pagesTyrosolutioneva5ochabauerNo ratings yet
- Hemispatial Neglect LDHDocument20 pagesHemispatial Neglect LDHAldersleyNo ratings yet
- Shoulder Impingement SyndromeDocument21 pagesShoulder Impingement SyndromeivannaOctavianiNo ratings yet
- Functional Assessment in PhysiotherapyDocument0 pagesFunctional Assessment in PhysiotherapyDibyendunarayan BidNo ratings yet
- Rehabilitation Engineering Fact Sheet PDFDocument2 pagesRehabilitation Engineering Fact Sheet PDFYahya AlkamaliNo ratings yet
- IVDP & Spinal SurgeriesDocument7 pagesIVDP & Spinal Surgeriesbbpanicker67% (3)
- Kaltenborn 1993Document5 pagesKaltenborn 1993hari vijayNo ratings yet
- Walking AidsDocument38 pagesWalking AidsMurad KurdiNo ratings yet
- Occupational Therapy Rehabilitation Paraplegic PatientDocument7 pagesOccupational Therapy Rehabilitation Paraplegic PatientAlina PasăreNo ratings yet
- Pediatrics FracturesDocument14 pagesPediatrics Fracturesخالد الغامديNo ratings yet
- Ataxia Physical Therapy and Rehabilitation Applications For Ataxic PatientsDocument19 pagesAtaxia Physical Therapy and Rehabilitation Applications For Ataxic PatientsAnastasios ChortisNo ratings yet
- Amputee Activity Score PDFDocument5 pagesAmputee Activity Score PDFLydia MartínNo ratings yet
- StrokeDocument16 pagesStrokeFahmi AbdullaNo ratings yet
- Citadel Journal 36Document100 pagesCitadel Journal 36Wilbur Whateley100% (1)
- Sanctus Reach The Red WaaaghDocument186 pagesSanctus Reach The Red WaaaghWilbur Whateley100% (3)
- Dred MobDocument17 pagesDred MobTeister100% (2)
- PalmerDD's Lifeline ChronoDocument42 pagesPalmerDD's Lifeline ChronoWilbur WhateleyNo ratings yet
- ShravanDocument8 pagesShravanSachin KulkarniNo ratings yet
- Student Learning Outcome #1Document12 pagesStudent Learning Outcome #1api-384606877No ratings yet
- Research ProposalDocument5 pagesResearch ProposalAngel Jose100% (1)
- Form Use:: Study GuideDocument2 pagesForm Use:: Study GuideANDRES IBARRA COSSIONo ratings yet
- Cognitive Code Method and Cognitive Anti-MethodDocument14 pagesCognitive Code Method and Cognitive Anti-MethodCarola Pinto Clavijo100% (2)
- Educ 108 Reflection For PortfolioDocument2 pagesEduc 108 Reflection For PortfolioqtkosuperNo ratings yet
- Organizational Structure and CultureDocument32 pagesOrganizational Structure and Cultureamr369100% (1)
- 720 Degree Performance AppraisalDocument42 pages720 Degree Performance AppraisalMayank Baheti50% (2)
- What Is GrammarDocument52 pagesWhat Is Grammarkhatipah ghaniNo ratings yet
- Speakout Elementary PunctuationDocument3 pagesSpeakout Elementary PunctuationKaterina PolonskayaNo ratings yet
- Employee Engagement JRADocument4 pagesEmployee Engagement JRAUday Kumar100% (1)
- Short Review of "Two KindsDocument19 pagesShort Review of "Two KindsEisya Abdullah100% (1)
- Book Review of The Self and Its Brain by Popper and EcclesDocument4 pagesBook Review of The Self and Its Brain by Popper and EcclesKai MöllNo ratings yet
- EmoTrance Introduction Exercise PDFDocument1 pageEmoTrance Introduction Exercise PDFCharles Teixeira SousaNo ratings yet
- Coping With Toxic Managers, Subordinates and Other Difficult PeopleDocument402 pagesCoping With Toxic Managers, Subordinates and Other Difficult Peoplejiggycheng91% (11)
- Machine Learning With Python: Amin ZollanvariDocument457 pagesMachine Learning With Python: Amin Zollanvari方士豪No ratings yet
- Eapp-Handout1: From Various Disciplines". Read and Study The EntireDocument1 pageEapp-Handout1: From Various Disciplines". Read and Study The EntireJanine TurlaNo ratings yet
- Project Code:: A Comparative Study of Traditional and Contemporary Nigerian DancesDocument10 pagesProject Code:: A Comparative Study of Traditional and Contemporary Nigerian DancesMorrison Omokiniovo Jessa SnrNo ratings yet
- Journal ON Social and Emotional Intelligence: Submitted By: Sriprakash PG20112085 Sec-EDocument16 pagesJournal ON Social and Emotional Intelligence: Submitted By: Sriprakash PG20112085 Sec-EAryan SpNo ratings yet
- LS-CHECKLISTDocument9 pagesLS-CHECKLISTravindran85No ratings yet
- Solving the Evolutionary Paradox: Understanding Attraction Beyond LooksDocument15 pagesSolving the Evolutionary Paradox: Understanding Attraction Beyond LooksSamin Afnan0% (1)
- Machine Learning by SahilDocument15 pagesMachine Learning by SahilNaman SharmaNo ratings yet
- English 1Document6 pagesEnglish 1Gabriela75% (8)
- PerPerDev - Q1 - 3 - Developing The Whole Person Evaluate One - S PersonalityDocument17 pagesPerPerDev - Q1 - 3 - Developing The Whole Person Evaluate One - S PersonalityJamil JalloresNo ratings yet
- Week V RC Ss G WC Week 1 En4V-Iiia-13.2: List of CompetenciesDocument2 pagesWeek V RC Ss G WC Week 1 En4V-Iiia-13.2: List of CompetenciesMa Francia BulacanNo ratings yet
- Physiological Arousal - Emotional Arousal - Cognitive Arousal - Environmental ArousalDocument33 pagesPhysiological Arousal - Emotional Arousal - Cognitive Arousal - Environmental ArousalWaris AshrafNo ratings yet
- Foundation of Educ - ReportDocument7 pagesFoundation of Educ - ReportJemelyn Aguilar100% (2)
- Self and Self PresentationDocument46 pagesSelf and Self PresentationReizelNo ratings yet
- Pramanasamuccaya Potter Summary (NEW)Document37 pagesPramanasamuccaya Potter Summary (NEW)khnum02100% (2)
- The Empath Healer and Intuitive Training GuideDocument15 pagesThe Empath Healer and Intuitive Training GuideLaura Whalen Jones67% (6)