Professional Documents
Culture Documents
Arterial Blood Gas
Uploaded by
vanita pathareCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arterial Blood Gas
Uploaded by
vanita pathareCopyright:
Available Formats
Arterial blood gas
An arterial blood gas (ABG) is a blood test that is performed using blood
from an artery. It involves puncturing an artery with a thin needle and syringe
and drawing a small volume of blood. The most common puncture site is the
radial artery at the wrist, but sometimes the femoral artery in the groin or
other sites are used. The blood can also be drawn from an arterial catheter.
The test is used to determine the pH of the blood, the partial pressure of
carbon dioxide and oxygen, and the bicarbonate level. ABG testing is mainly
used in pulmonology, to determine gas exchange levels in the blood related to
lung function, but has a variety of applications in other areas of medicine.
Extraction and analysis
Arterial blood for blood gas analysis is usually extracted by a phlebotomist, nurse,
or respiratory therapist. Blood is most commonly drawn from the radial artery
because it is easily accessible, can be compressed to control bleeding, and has less
risk for occlusion. The femoral artery (or less often, the brachial artery) is also
used, especially during emergency situations or with children. Blood can also be
taken from an arterial catheter already placed in one of these arteries.
The syringe is pre-packaged and contains a small amount of heparin, to prevent
coagulation or needs to be heparinised, by drawing up a small amount of heparin
and squirting it out again. Once the sample is obtained, care is taken to eliminate
visible gas bubbles, as these bubbles can dissolve into the sample and cause
inaccurate results. The sealed syringe is taken to a blood gas analyzer. If the
sample cannot be immediately analyzed, it is chilled in an ice bath in a glass
syringe to slow metabolic processes which can cause inaccuracy. Samples drawn
in plastic syringes are not iced and are analyzed within 30 minutes.
Calculations
The machine used for analysis aspirates this blood from the syringe and measures
the pH and the partial pressures of oxygen and carbon dioxide. The bicarbonate
concentration is also calculated. These results are usually available for
interpretation within five minutes.
Reference ranges and interpretation
Analyte
pH
Range
7.357.45
PaO2
9.313.3 kPa
or
80100
mmHg
PaCO2
4.76.0 kPa
or
3545
mmHg
HCO3
H+
2226 m
mol/l
3545 n
mol/l
Interpretation
If pH < 7.35 - acidic.
If pH > 7.45 - alkalemic.
A low O2 indicates that the patient is not
respiring properly, and is hypoxemic.
A high PaCO2 (respiratory acidosis) indicates
under ventilation.
A low PaCO2 (respiratory alkalosis) hyper- or
over ventilation.
PaCO2 levels can also become abnormal
when the respiratory system is working to
compensate for a metabolic issue so as to
normalize the blood pH.
A low HCO3 indicates metabolic acidosis.
A high HCO3 indicates metabolic alkalosis.
HCO3 levels can also become abnormal when
the kidneys are working to compensate for a
respiratory issue so as to normalize the
blood pH.
+
If H >45-acidotic
If H+< 35-alkalemic
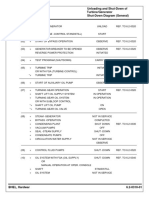
Normal Arterial Blood Gas Values
pH
7.35-7.45
PaCO2
35-45 mm Hg
PaO2
80-95 mm Hg
HCO3
22-26 mEq/L
O2 Saturation 95-99%
BE
Respiratory
Acidosis
Acute
Partly
Compensated
Compensated
Respiratory
Alkalosis
Acute
Partly
Compensated
Compensated
Metabolic
Acidosis
Acute
Partly
Compensated
Compensated
Metabolic
Alkalosis
Acute
Partly
Compensated
Compensated
+/- 1
pH
PaCO2
HCO3
< 7.35
> 45
Normal
< 7.35
> 45
> 26
Normal
> 45
> 26
> 7.45
< 35
Normal
> 7.45
< 35
< 22
Normal
< 35
< 22
< 7.35
Normal
< 22
< 7.35
< 35
< 22
Normal
< 35
< 22
> 7.45
Normal
> 26
> 7.45
> 45
> 26
Normal
> 45
> 26
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Sdre14-5 Ral 1-2-Rev17Document3 pagesSdre14-5 Ral 1-2-Rev17lwin_oo2435No ratings yet
- The Wrist Complex: Vanita A Pathare PG-1Document54 pagesThe Wrist Complex: Vanita A Pathare PG-1vanita pathareNo ratings yet
- IJCRR Comparison of Acapella and RC Cornet For Airway Clearance in BronchiectasisDocument12 pagesIJCRR Comparison of Acapella and RC Cornet For Airway Clearance in Bronchiectasisvanita pathareNo ratings yet
- The Wrist Complex: Vanita A Pathare PG-1Document54 pagesThe Wrist Complex: Vanita A Pathare PG-1vanita pathareNo ratings yet
- Wrist StabilityDocument9 pagesWrist Stabilityel_mekawyNo ratings yet
- IJCRR Comparison of Acapella and RC Cornet For Airway Clearance in BronchiectasisDocument12 pagesIJCRR Comparison of Acapella and RC Cornet For Airway Clearance in Bronchiectasisvanita pathareNo ratings yet
- FINS 2624 Quiz 2 Attempt 2 PDFDocument3 pagesFINS 2624 Quiz 2 Attempt 2 PDFsagarox7No ratings yet
- The Ultimate Life GuideDocument12 pagesThe Ultimate Life GuideNLPCoachingNo ratings yet
- Mastercam 8.1 Beta 4: New Verification Engine in Beta 4! Sub-Programs Post ChangesDocument48 pagesMastercam 8.1 Beta 4: New Verification Engine in Beta 4! Sub-Programs Post ChangesSaul Saldana LoyaNo ratings yet
- Design and Development of Manually Operated ReaperDocument8 pagesDesign and Development of Manually Operated ReaperIOSRjournalNo ratings yet
- A7670 Series Hardware Design v1.03Document69 pagesA7670 Series Hardware Design v1.03Phạm NamNo ratings yet
- Kathrein 80010375Document2 pagesKathrein 80010375klamar5No ratings yet
- Gas Exchange in Plants and AnimalsDocument7 pagesGas Exchange in Plants and AnimalsMarvin MelisNo ratings yet
- GHT 2001 Chino 12 Point Temperature Recorder EH3127 001Document1 pageGHT 2001 Chino 12 Point Temperature Recorder EH3127 001gawaNo ratings yet
- HYKDDocument15 pagesHYKDAri RamadhanNo ratings yet
- JJ309 Fluid Mechanics Unit 6Document30 pagesJJ309 Fluid Mechanics Unit 6Adib AzharNo ratings yet
- Lea 2 PDFDocument21 pagesLea 2 PDFKY Renz100% (1)
- PENERAPAN ARSITEKTUR TROPIS PADA HOTEL RESORT DI PANTAI KRAKALDocument12 pagesPENERAPAN ARSITEKTUR TROPIS PADA HOTEL RESORT DI PANTAI KRAKALleo adoNo ratings yet
- داينمك الملزمة كاملةDocument79 pagesداينمك الملزمة كاملةarno assassin33% (3)
- Everything You Need to Know About Centrifugal FansDocument65 pagesEverything You Need to Know About Centrifugal Fansahmed100% (1)
- Fundamentals of SwimmingDocument7 pagesFundamentals of SwimmingSheila Mae Lira100% (1)
- 2019 Torch and Consumables Catalog: For Mechanized Plasma SystemsDocument64 pages2019 Torch and Consumables Catalog: For Mechanized Plasma SystemsRaj DomadiyaNo ratings yet
- Dr. Ghusoon Mohsin Ali: Al-Mustansiriya University College of Engineering Electrical Engineering DepartmentDocument89 pagesDr. Ghusoon Mohsin Ali: Al-Mustansiriya University College of Engineering Electrical Engineering Departmentهمام الركابي100% (1)
- HTTP Verbs GET POST PUT PATCH DELETE (39Document12 pagesHTTP Verbs GET POST PUT PATCH DELETE (39Jefferson EducacionNo ratings yet
- Durango GS 6-7 Helitack OutreachDocument4 pagesDurango GS 6-7 Helitack OutreachdcgmNo ratings yet
- Steam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)Document1 pageSteam Turbine Unloading and Shut-Down of Operation Turbine/Generator Shut-Down Diagram (General)parthibanemails5779No ratings yet
- BR A Consumables Catalog ElecDocument31 pagesBR A Consumables Catalog Elecdweil1552No ratings yet
- Operating Systems: Chapter 3: DeadlocksDocument46 pagesOperating Systems: Chapter 3: DeadlocksManoel Katlib100% (1)
- Unit-I EsDocument53 pagesUnit-I Eschethan.naik24No ratings yet
- DA1 Learning - Ans KeyDocument4 pagesDA1 Learning - Ans KeyDolon DasNo ratings yet
- DOCUMENT guides the way with VLB-44 LED Marine BeaconDocument4 pagesDOCUMENT guides the way with VLB-44 LED Marine BeaconbenNo ratings yet
- Dialyser Reprocessing Machine Specification (Nephrology)Document2 pagesDialyser Reprocessing Machine Specification (Nephrology)Iftekhar AhamedNo ratings yet
- Real Talk GrammarDocument237 pagesReal Talk GrammarOmar yoshiNo ratings yet
- FLIGHT CONTROLS: TROUBLESHOOTING AND COMPONENTSDocument3 pagesFLIGHT CONTROLS: TROUBLESHOOTING AND COMPONENTSBernardino Ferreira JúniorNo ratings yet
- Volvo g900 Modelos PDFDocument952 pagesVolvo g900 Modelos PDFAdrianDumescu100% (3)