Professional Documents
Culture Documents
NCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDS
Uploaded by
Tina LarsenOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP Nursing Care Plan For Acute Respiratory Distress Syndrome ARDS
Uploaded by
Tina LarsenCopyright:
Available Formats
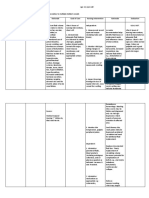
NCP Nursing Care Plan for Acute respiratory distress syndrome ARDS.
Acute respiratory distress syndrome (ARDS) is a form of pulmonary edema that causes acute respiratory failure. Also known as shock, stiff, white, wet, or Da Nang lung. It may follow direct or indirect lung injury. ARDS results from increased permeability of the alveolocapillary membrane. Fluid accumulates in the lung interstitium, alveolar spaces, and small airways, causing the lung to stiffen. Effective ventilation is thus impaired, prohibiting adequate oxygenation of pulmonary capillary blood. Severe ARDS can cause intractable and fatal hypoxemia; however, patients who recover may have little or no permanent lung damage. Causes for Acute respiratory distress syndrome ARDS Trauma is the most common cause of ARDS, possibly because trauma-related factors, such as fat emboli, sepsis, shock, pulmonary contusions, and multiple transfusions, increase the likelihood of microemboli developing. ARDS can result from any one of several respiratory and nonrespiratory causes: Aspiration of gastric contents Sepsis (primarily gram-negative), trauma (lung contusion, head injury, long bone fracture with fat emboli), or oxygen toxicity Viral, bacterial, or fungal pneumonia or microemboli (fat or air emboli or disseminated intravascular coagulation) Anaphylaxis, drug overdose (barbiturates, glutethimide, narcotics) or blood transfusion Smoke or chemical inhalation (nitrous oxide, chlorine, ammonia) Pancreatitis, hypertransfusion, cardiopulmonary bypass Near drowning. Less common causes of ards include coronary artery bypass grafting, hemodialysis, leukemia, acute miliary tuberculosis, pancreatitis, thrombotic thrombocytopenic purpura, uremia, and venous air embolism.
Nursing Assessment Nursing Care Plan for Acute respiratory distress syndrome (ARDS) ARDS initially produces rapid, shallow breathing and dyspnea within hours to days of the initial injury (sometimes after the patient's condition appears stable). Hypoxemia develops, causing an increased drive for ventilation. Because of the effort required to expand the stiff lung, intercostal and suprasternal retractions result. Fluid accumulation may produce crackles and rhonchi, and worsening hypoxemia causes restlessness, apprehension, mental sluggishness, motor dysfunction, and tachycardia (possibly with transient increased arterial blood pressure). Severe ARDS causes overwhelming hypoxemia, which, if uncorrected, results in hypotension, decreasing urine output, respiratory and metabolic acidosis and, eventually, ventricular fibrillation or standstill. In stage I, the patient may complain of dyspnea, especially on exertion. Respiratory and pulse rates are normal to high. Auscultation may reveal diminished breath sounds. In stage II, respiratory distress becomes more apparent. The patient may use accessory muscles to breathe and appear pallid, anxious, and restless. He may have a dry cough with thick, frothy sputum and bloody, sticky secretions. Palpation may disclose cool, clammy skin. Tachycardia and tachypnea may accompany elevated blood pressure. He may have a change or decrease in mental status. Auscultation may reveal basilar crackles. (Stage II signs and symptoms may be incorrectly attributed to other causes such as multiple traumas.) In stage III, the patient struggles to breathe. Vital signs reveal tachypnea (more than 30 breaths/minute), tachycardia with arrhythmias (usually premature ventricular contractions), and a labile blood pressure. Inspection may reveal a productive cough and pale, cyanotic skin. He may demonstrate a change or decrease in mental status. Auscultation may disclose crackles and rhonchi. The patient needs intubation and ventilation. In stage IV, the patient has acute respiratory failure with severe hypoxia. His mental status is deteriorating, and he may become comatose. His skin appears pale and cyanotic. Spontaneous respirations aren't evident. Bradycardia with arrhythmias accompanies hypotension. Metabolic acidosis and respiratory acidosis develop. When ARDS reaches this stage, the patient is at high risk for fibrosis. Pulmonary damage becomes life-threatening.
Diagnostic tests for Acute respiratory distress syndrome ARDS Arterial blood gas (ABG) analysis. Serial chest X-rays.
Nursing diagnosis for Acute respiratory distress syndrome ARDS Common Nursing diagnosis found in patient with Acute respiratory distress syndrome ARDS Anxiety Decreased cardiac output Fatigue Fear Impaired gas exchange Impaired physical mobility Impaired verbal communication Ineffective airway clearance Ineffective coping Ineffective tissue perfusion: Cardiopulmonary Risk for impaired skin integrity Risk for infection
Nursing outcomes Nursing Care Plan for Acute respiratory distress syndrome (ARDS)
The patient will express feelings of reduced anxiety. The patient will remain hemodynamically stable. The patient will verbalize the importance of balancing activity with adequate rest periods. The patient will discuss fears or concerns. The patient will maintain adequate ventilation and oxygenation The patient will maintain joint range-of-motion and muscle strength. The patient will use alternate means of communication. The patient will maintain a patent airway. The patient will use support systems to assist with coping. The patient will maintain adequate cardiopulmonary perfusion. The patient will maintain skin integrity. The patient will remain free from signs or symptoms of infection.
Nursing Interventions Nursing Care Plan for Acute respiratory distress syndrome ARDS Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source or anticipated danger Calming Technique: Reducing anxiety in patient experiencing acute distress Hemodynamic Regulation: Optimization of heart rate, preload, afterload, and contractility Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function
Circulatory Care: Mechanical Assist Devices: Temporary support of the circulation through the use of mechanical devices or pumps Energy Management: Regulating energy use to treat or prevent fatigue and optimize function Exercise Promotion: Facilitation of regular physical exercise to maintain or advance to a higher level of fitness and health Nutrition Management: Assisting with or providing a balanced dietary intake of foods and fluids Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source or anticipated danger Security Enhancement: Intensifying a patient s sense of physical and psychological safety Coping Enhancement: Assisting a patient to adapt to perceived stressors, changes, or threats that interfere with meeting life demands and roles Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange Oxygen Therapy: Administration of oxygen and monitoring of its effectiveness Airway Management: Facilitation of patency of air passages Exercise Therapy: [specify]: Use of active or passive body movement to maintain or restore flexibility; use of specific activity or exercise protocols to enhance or restore controlled body movement, etc. Pain Management: Alleviation of pain or a reduction in pain to a level of comfort acceptable to the patient Communication Enhancement: Speech Deficit: Assistance in accepting and learning alternative methods for living with impaired speech Communication Enhancement: Hearing Deficit: Assistance in accepting and learning alternative methods for living with diminished hearing Active Listening: Attending closely to and attaching significance to a patient s verbal and nonverbal messages Airway Management: Facilitation of patency of air passages
Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange Cough Enhancement: Promotion of deep inhalation by the patient with subsequent generation of high intrathoracic pressures and compression of underlying lung parenchyma for the forceful expulsion of air Coping Enhancement: Assisting a patient to adapt to perceived stressors, changes, or threats that interfere with meeting life demands and roles Decision-Making Support: Providing information and support for a person who is making a decision regarding healthcare Fluid/Electrolyte Management: Promotion of fluid/electrolyte balance and prevention of complications resulting from abnormal or undesired fluid/serum electrolyte levels Cerebral Perfusion Promotion: Promotion of adequate perfusion and limitation of complications for a patient experiencing or at risk for inadequate cerebral perfusion Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function Circulatory Care: Arterial/Venous Insufficiency: Promotion of arterial/venous circulation Skin Surveillance: Collection and analysis of patient data to maintain skin and mucous membrane integrity Pressure Management: Minimizing pressure to body parts Pressure Ulcer Prevention: Prevention of pressure ulcers for a patient at high risk for developing them Infection Protection: Prevention and early detection of infection in a patient at risk Infection Control: Minimizing the acquisition and transmission of infectious agents Surveillance: Purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision making
You might also like
- Nursing Care PlanDocument11 pagesNursing Care Planaycee0316100% (1)
- NCP Copd4Document15 pagesNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- Ards NCPDocument5 pagesArds NCPgopscharanNo ratings yet
- Nursing Care Plan - Pulmonary EmbolismDocument3 pagesNursing Care Plan - Pulmonary EmbolismPui_Yee_Siow_6303100% (10)
- Impaired Breathing PatternDocument1 pageImpaired Breathing PatternHanya Bint PotawanNo ratings yet
- Ineffective Breathing PatternDocument8 pagesIneffective Breathing PatternJansen Arquilita Rivera100% (2)
- Ineffective Breathing PatternDocument3 pagesIneffective Breathing PatternTrixie Anne Gamotin100% (3)
- Asthma Impaired Gas ExchangeDocument2 pagesAsthma Impaired Gas ExchangeNedeve Ozned100% (5)
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 pagesNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNo ratings yet
- NCP 1 Ineffective Airway ClearanceDocument2 pagesNCP 1 Ineffective Airway ClearanceDivine Jane PurciaNo ratings yet
- Nursing Care Plan (Septick Shock)Document6 pagesNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- NCP Tissue PerfusionDocument4 pagesNCP Tissue PerfusionLisa Tandog100% (1)
- Nursing Care Plan For AIDS HIVDocument3 pagesNursing Care Plan For AIDS HIVFARAH MAE MEDINA100% (2)
- Cues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalDocument4 pagesCues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalKei Cruz100% (1)
- Covid NCPDocument6 pagesCovid NCPNathalia Cabalse100% (2)
- To Maintain Patent Airway. (-: Surgical Nursing: Clinical Management For Positive Outcomes (Vol. 1)Document3 pagesTo Maintain Patent Airway. (-: Surgical Nursing: Clinical Management For Positive Outcomes (Vol. 1)Clint Delacruz50% (4)
- Assessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveDocument3 pagesAssessment Diagnosis Planning Implementation Evaluation No Subjective Cues ObjectiveMaverick LimNo ratings yet
- Ncp-Ineffective Breathing PatternDocument4 pagesNcp-Ineffective Breathing PatternRoxanne Ganayo Claver100% (1)
- Ineffective Breathing PatternDocument2 pagesIneffective Breathing PatternJoy Arizala CarasiNo ratings yet
- Improve Activity Tolerance Through Rest and RelaxationDocument7 pagesImprove Activity Tolerance Through Rest and RelaxationKrisJane Ratilla Abiva100% (2)
- NCP HemothoraxDocument3 pagesNCP Hemothoraxroseonabreeze0% (2)
- San Francisco St. Butuan City 8600, Region XIII Caraga, PhilippinesDocument3 pagesSan Francisco St. Butuan City 8600, Region XIII Caraga, Philippineskuro hanabusaNo ratings yet
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- NCP For HemothoraxDocument12 pagesNCP For HemothoraxroseonabreezeNo ratings yet
- Hypertonic SolutionsDocument4 pagesHypertonic SolutionsVanessa PaguiriganNo ratings yet
- NCP Increased IcpDocument2 pagesNCP Increased IcphelloaNo ratings yet
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- St. Anthony's Nursing Care Plan for Acute Chest PainDocument1 pageSt. Anthony's Nursing Care Plan for Acute Chest PainjoegeNo ratings yet
- CAD NCP Decreased Cardiac OutputDocument3 pagesCAD NCP Decreased Cardiac OutputLeizel Apolonio100% (3)
- 6639burn NCPDocument18 pages6639burn NCPDivina Grace Renon Camba100% (1)
- Cva NCP AnxietyDocument1 pageCva NCP AnxietyQueenElsaDeVeraNo ratings yet
- NCP Impaired Gas Exhange CHEST INJURYDocument4 pagesNCP Impaired Gas Exhange CHEST INJURYMa. Elaine Carla Tating100% (2)
- NCP PneumoniaDocument28 pagesNCP PneumoniaW'ton Borbe83% (6)
- Breathing Difficulties Pleural EffusionDocument3 pagesBreathing Difficulties Pleural EffusionErickson OcialNo ratings yet
- Impaired Tissue PerfusionDocument2 pagesImpaired Tissue PerfusionLyka Mae Imbat - PacnisNo ratings yet
- NCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsDocument3 pagesNCP Ineffective Airway Clearance Related To The Accumulation of Secretions As Evidence by Decrease in Respiratory Rate and NGT and ET Tube Attached and Crackles at The Left Base of The LungsSarah Ann Jamilla FaciolanNo ratings yet
- Nursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDocument4 pagesNursing Care for Impaired MobilityTITLEPreventing Peripheral Neurovascular Issues TITLERelieving Acute Pain from InflammationDaniel Garraton0% (1)
- NCP For InfectionDocument1 pageNCP For InfectionNathaniel EllanoNo ratings yet
- Managing Acute Renal PainDocument22 pagesManaging Acute Renal PainMaricris S. Sampang100% (1)
- Nursing ManagementDocument16 pagesNursing ManagementNica Marie LumbaNo ratings yet
- CJ C J CJ CJ Cî CJ CJ C C ! "! Cî C Ë # C Ë # CJ$ C C 0 "% C C & C C C Ë Î C "' (C Ëj "ËjDocument105 pagesCJ C J CJ CJ Cî CJ CJ C C ! "! Cî C Ë # C Ë # CJ$ C C 0 "% C C & C C C Ë Î C "' (C Ëj "ËjShirin Forbes Aquino100% (2)
- Lumunok at Huminga, Nabibilaukan Din Ako Madalas" AsDocument4 pagesLumunok at Huminga, Nabibilaukan Din Ako Madalas" AsPatricia Ortega100% (1)
- Ineffective Breathing PatternDocument5 pagesIneffective Breathing PatternruguNo ratings yet
- Knowledge DeficitDocument3 pagesKnowledge DeficitInigo Miguel DulayNo ratings yet
- Acute Confusion Nursing DiagnosisDocument4 pagesAcute Confusion Nursing Diagnosisasmika danaNo ratings yet
- Nanda NCP BasedDocument14 pagesNanda NCP Baseddeliejoyce100% (1)
- Decreased Cardiac OutputDocument3 pagesDecreased Cardiac OutputTiffany Mathis100% (1)
- Impaire Spontaneous VentilationDocument4 pagesImpaire Spontaneous VentilationSkyla FiestaNo ratings yet
- Pneumonia Nursing Care Plans: Assessment, Interventions & OutcomesDocument1 pagePneumonia Nursing Care Plans: Assessment, Interventions & Outcomesjustin_saneNo ratings yet
- Care Plan Prep May 13 Rheumatic FeverDocument16 pagesCare Plan Prep May 13 Rheumatic Feverapi-256360167No ratings yet
- Pneumonia Case Study: Toddler Diagnosis and TreatmentDocument5 pagesPneumonia Case Study: Toddler Diagnosis and TreatmentcrisolandNo ratings yet
- ARDSDocument55 pagesARDSSandhya HarbolaNo ratings yet
- Acute Respiratory Failure-PRINTDocument5 pagesAcute Respiratory Failure-PRINTJan SicatNo ratings yet
- Acute Respiratory Failure in AdultDocument19 pagesAcute Respiratory Failure in AdultFatima Love Ariate-ArcasetasNo ratings yet
- CopdDocument47 pagesCopdNingshesil Ny HermantNo ratings yet
- ARDSDocument31 pagesARDSRaymund Christopher Dela PeñaNo ratings yet
- Ards 2Document7 pagesArds 2LUCIBELLOT1No ratings yet
- Chronic Obstructive Pulmonary DiseaseDocument4 pagesChronic Obstructive Pulmonary DiseaseSeraphina SolanNo ratings yet
- ARDSDocument23 pagesARDSDumora FatmaNo ratings yet
- Jurnal Internasional 3Document10 pagesJurnal Internasional 3rina adriyaniNo ratings yet
- Vocal LessonDocument61 pagesVocal LessonLonnie Marlin100% (1)
- Cardiovascular and Respiratory SystemDocument44 pagesCardiovascular and Respiratory SystemKlaudette Collin PaynorNo ratings yet
- Golden Rules For Everyday Life - Omraam Mikhael AivanhovDocument191 pagesGolden Rules For Everyday Life - Omraam Mikhael AivanhovPedro Ribeiro100% (7)
- Vital Signs Guide Key FeaturesDocument17 pagesVital Signs Guide Key FeaturesEvello Mercano100% (1)
- Resmed - Philips Script Convert.Document28 pagesResmed - Philips Script Convert.Diabestes-stuff100% (1)
- App j.1 Guided Self Regulation AprilDocument29 pagesApp j.1 Guided Self Regulation Aprilda_reaper_dasNo ratings yet
- How To Use A Vogel CrystalDocument5 pagesHow To Use A Vogel CrystalJorge100% (1)
- Penis-Massage GuideDocument19 pagesPenis-Massage GuideSubhajit Ghosh100% (3)
- LungsDocument3 pagesLungspinopinguinNo ratings yet
- Care of Clients With Physiologic and Psychosocial AlterationsDocument34 pagesCare of Clients With Physiologic and Psychosocial AlterationsChloie Marie RosalejosNo ratings yet
- Understanding Holistic DevelopmentDocument35 pagesUnderstanding Holistic DevelopmentAdeline PascualNo ratings yet
- Shinryukan Stretching ProgramDocument28 pagesShinryukan Stretching Programwilera100% (1)
- Alcomer 123 LADocument8 pagesAlcomer 123 LAsajad gohariNo ratings yet
- Oxygen Therapy Guide for COVID PatientsDocument44 pagesOxygen Therapy Guide for COVID PatientsISHITA VYASNo ratings yet
- Clinical Guidelines (Nursing) : Tracheostomy ManagementDocument19 pagesClinical Guidelines (Nursing) : Tracheostomy ManagementbarbiemeNo ratings yet
- Mantra Yoga: A Tool For A Healthy Mind: Dr. Kamakhya KumarDocument7 pagesMantra Yoga: A Tool For A Healthy Mind: Dr. Kamakhya KumarKalosoiretrotchgmail.com KalosoNo ratings yet
- Carnatic - Singing Tips Carnatic Music Lessons - ANURADHA MAHESHDocument3 pagesCarnatic - Singing Tips Carnatic Music Lessons - ANURADHA MAHESHhemasundarNo ratings yet
- Power For Every HourDocument10 pagesPower For Every HourmarnesiaNo ratings yet
- Newborn CareDocument120 pagesNewborn CareMike CalipayanNo ratings yet
- Nursing Care Plan (Septick Shock)Document6 pagesNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- Hypnobirthing The Mongan Method Parent Manual v2Document46 pagesHypnobirthing The Mongan Method Parent Manual v2Alma AcostaNo ratings yet
- 0654 IGCSE Coordinated Science 2019-2021 SyllabusDocument49 pages0654 IGCSE Coordinated Science 2019-2021 SyllabusYuhao LuNo ratings yet
- 7 Day Juice Cleanse Work BookDocument18 pages7 Day Juice Cleanse Work Bookgojanmajkovic100% (4)
- Respiratory Ventilation Products Critical Care: United States CatalogDocument37 pagesRespiratory Ventilation Products Critical Care: United States CatalogKatabalwa EricNo ratings yet
- NCP For Ineffective Airway ClearanceDocument3 pagesNCP For Ineffective Airway ClearanceJennelyn BayleNo ratings yet
- Science Class 8 Respiration and CirculationDocument9 pagesScience Class 8 Respiration and Circulationamnakazmi100% (1)
- Strength Training For WomenDocument146 pagesStrength Training For WomenLoreMariaNo ratings yet
- Kindergarten: Quarter 1: Week 4 Learning ExperiencesDocument24 pagesKindergarten: Quarter 1: Week 4 Learning ExperiencesHanzel NietesNo ratings yet
- Neuro Estructural Integracion Tecnica PDF en InglesDocument10 pagesNeuro Estructural Integracion Tecnica PDF en InglesLuulaa Minguin GarciaNo ratings yet