Professional Documents
Culture Documents
Bacteriology Review
Uploaded by
yachiru121Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bacteriology Review
Uploaded by
yachiru121Copyright:
Available Formats
BACTERIOLOGY LABORATORY REPORTS / TECHNIQUES ASEPTIC TECHNIQUE: In handling bacteria specimens, do everything possible to assure that extraneous bacteria
from you do not contaminate the specimen. This is not sterile technique. Preparation and Staining: Heat Fixing: After air drying a slide, applying gentle heat helps the bacteria to adhere to the slide. Simple Stain (Methylene Blue): Stains all cells and can illuminate morphology. GRAM STAIN: o PRIMARY STAIN: Crystal Violet stains both Gram+ and Gram- and makes all bacterial cells appear purple. Both Gram+ and Gram- will stain with this dye. o CHELATING AGENT: Add Gram's Iodine which will adhere only to cell walls that have a lot of peptidoglycan in them (i.e. Gram+) o DECOLORIZATION: Add Acetone very briefly to wash away the Crystal Violet dye. Gram-: The purple dye will be washed away. Gram+: The purple dye will remain adherent. o COUNTERSTAIN: Then add Safranin which will stain cells pink. GRAM-POSITIVE: Will appear purple (from Crystal Violet) -- Safranin doesn't stain it. GRAM-NEGATIVE: Will appear pink, as it takes up the Safranin. o FALSE GRAM-NEGATIVES: Dead Gram+ cells will appear as though they are Gram-. In antibiotic-treated specimens, a certain portion of such cells is expected. ACID-FAST STAIN: Stains Mycobacteria such as Mycobacterium Tuberculosis. o LIPID cell wall gives them the property of weak initial staining, plus strong retention of initial dye (like Gram+) once stained. o PROCESS: Carbol-Fuscin dye is used initially, with heat, for 20 to 30 minutes (long time) Acid-Alcohol is then used as a decolorizing agent. If the organism resist the decolorization, it is considered acid-fast. FLUORESCENT STAIN: o It has the advantage that you can scan at low power until you find something that fluoresces, then you can hone in on it. IMMUNODIAGNOSTICS o Hemagglutination Inhibition: Certain organisms can agglutinate red blood cells. If you have antibodies to impede that agglutination, then you have a positive test result (antibody is present). o Direct Fluorescent Antibody: Fluoro tagged antibody checks for presence of antigen directly. o Indirect Fluorescent Antibody: First allow antigen-antibody reaction, then use a second Fluoro tagged antibody (anti-antibody) to identify presence of the first antibody. o Complement Fixation: Usually avoided; expensive. o ACUTE and CONVALESCENT TITERS: Take an antibody titer at initial infection (acute), and again four to five weeks later. You would expect a four-fold increase in titer if the suspected organism is indeed the infecting organism. There is usually a baseline level of antibody present with or without infection, because of cross-reactivity with other antigens. Thus you use acute:convalescent titers as a means of comparison. For some organisms, there are also absolute antibody levels that are diagnostic. o Radio-Immunoassay (RISA, ELISA): Take the patient's direct specimen and try to detect residual evidence of the organism's presence. Used when recovery of bacteria itself is not possible. Molecular Probes Polymerase Chain-Reaction (PCR): Can also be used for direct detection but it's expensive.
CULTURE: EXCEPTIONS to the fact that organisms can be cultured in 24 hours. o Mycobacterium Tuberculosis takes up to eight weeks to culture. o Syphilis and Leprosy organisms have never been cultured. Streaking for Isolation: Process of inoculating a plate such that you get single bacterial colonies once you culture the plate.
www.brain101.info
PROCESS: Take an inoculating stick, flame it, dip it into the bacteria (tissue sample), and then streak across the plate. Then flame it again, and streak it again. SUSCEPTIBILITY TESTS: o KIRBY-BAUER METHOD of Antibiotic Susceptibility Testing: Testing is done using the Disk-Diffusion Method PROCEDURE: Grow confluent bacterial colony on plate Add antibiotic disc in center. Measure the Zone of Inhibition (diameter) to determine bacterial susceptibility. RESULTS: The larger the zone of inhibition, the more susceptible are the bacteria. Resistant: No zone of inhibition is found. Intermediate: Intermediate zone of inhibition. Susceptible: Larger zone of inhibition. An interpretive table or computer, along with known concentrations of antibiotic, must be used to interpret results. o E-TEST: ANAEROBE Susceptibility Test. Strict Anaerobes must be cultures under special conditions. Instead of a disk, the antibiotics are contained in capillary disks. o SPIRAL GRADIENT ENDPOINT TEST: Another susceptibility test Line several isolates (can be from different patients) up on a single plate in wheel-spoke fashion. Growth inhibition at each line can then be observed and interpreted by computer. o SERUM BACTERICIDAL TEST: Susceptibility test for patients that are extremely sick. Take serum sample and test amount of antibody actually in patient's serum. Then plate that antibody out onto culture and verify that it actually does kill the bugs at its peak and trough concentrations in the patient's serum. A 1:8 dilution of serum inhibiting growth should be indicative that antibiotics are effective enough to kill bacteria in vivo. MINIMUM INHIBITORY CONCENTRATION (MIC): The minimum amount of antibiotic necessary to inhibit bacterial growth to the point that no bacteria are visible with the naked eye. o This doesn't necessarily mean that no bacteria are there at all. Healthy person should be able to handle this bacterialevel with normal host-defenses. o PROCEDURE: Take test-tubes containing varying concentrations of antibiotic, plus a control tube with no antibiotic. Add growth media and 107 bacteria to each tube. The most dilute tube in which no turbidity is seen is the MIC -- the minimum antibiotic concentration that inhibits bacterial growth. o MINIMUM BACTERICIDAL CONCENTRATION (MBC): Amount of antibiotic necessary to kill 99.9% of all organisms. This value must be used when treating immunocompromised patients. PROCEDURE: To determine MBC, we must take all of our clear tubes from the MIC and culture them onto plates. Then, the plate on which the fewest number of colonies grows is termed the MBC. o Antibiotic Tolerance occurs when an isolate has a serial difference of five tubes between its MIC and MBC. Normally, the difference is only one or two tubes. This translates to a 32-fold difference in concentration. CHOCOLATE AGAR: Heat-lysed red-blood cells in agar. o
HEMOLYSIS: Appearance of culture in blood agar. alpha-HEMOLYSIS: Partial hemolysis, appearing green. beta-HEMOLYSIS: Full hemolysis. A "halo" appears around the colony. gamma-HEMOLYSIS: No hemolysis.
www.brain101.info
EPIDEMIOLOGY / GENERAL STUFF Causes of COMMUNITY-ACQUIRED PNEUMONIA: 1. Streptococcus Pneumoniae
Causes of NEONATAL (less than 3 months old) MENINGITIS and SEPSIS: In order 1. 2. Group-B Strep Escherichia Coli
Causes of INFANTILE (infants 6 - 24 months) MENINGITIS and SEPSIS: In order 1. 2. Haemophilus Influenzae (Hib) Neisseria Meningitidis
Causes of UTI's: In order 1. 2. 3. E. Coli Proteus Vulgaris / Mirabilis: o 10-15% of hospital acquired UTI's. Pseudomonas Aeruginosa
ENTEROBACTERIACEAE: Cause Gastroenteritis, UTI's, Pneumonia, and Bacteremia. GASTROENTERITIS: STRICTLY LUMINAL 1. Enteropathogenic E. Coli (EPEC) 2. Enterotoxigenic E. Coli (ETEC) 3. Vibrio Cholerae 4. Vibrio Parahaemolyticus (mechanism uncertain) GASTROENTERITIS: INVASIVE (DYSENTERY) 1. Enteroinvasive E. Coli (EIEC) 2. Shigellosis 3. Salmonella Enterica 4. Campylobacter Jejuni BACTEREMIA 1. Entero hemolytic E. Coli (EHEC) 2. Salmonella Typhi 3. Salmonella Choleraesuis URINARY TRACT INFECTION 1. E. Coli 2. Proteus 3. Pseudomonas 4. Klebsiella PNEUMONIA 1. Pseudomonas Aeruginosa 2. Klebsiella Pneumoniae
ENTEROBACTERIACEAE ANTIGENIC MARKERS: O-Antigen: Carbohydrate in the cell wall. K-Antigen: Capsular antigen, when present. H-Antigen: Flagellar antigen, when present: o Campylobacter, Helicobacter, Escherichia. F-Antigen: Pili antigen.
www.brain101.info
UTI COLLECTION METHODS: Midstream clean catch Catheterization o Risk of introducing infection o Technique must be aseptic Indwelling Catheter o Infection always results. Suprapubic Aspiration -- done only in males
UTI DIAGNOSTIC GUIDELINES: Asymptomatic Bacteriuria (Female): Greater than 105 bacteria / mL of a single isolate. o Collection: Clean-catch midstream o Symptoms: asymptomatic Uncomplicated Acute UTI: Greater than 103 bacteria / mL of a single isolate. o Collection: Clean-catch midstream o The diagnostic amount is smaller because polyuria is a symptom of UTI's, thus less bugs would tend to be in the urine. o Symptoms: Dysuria, frequency, urgency Uncomplicated Acute Pyelonephritis: Greater than 105 bacteria / mL of a single isolate o Collection: Clean-catch midstream, or catheter o Symptoms: Fever, chills Back pain, flank pain, tenderness of costovertebral angle Dysuria, frequency, urgency Primary UTI (Male): Greater than 105 bacteria / mL of a single isolate o Collection: Clean-catch midstream, or suprapubic aspiration o Cause: Often prostatitis or an enlarged prostate. Complicated UTI: Greater than 102 - 103 (100 - 1000) bacteria / mL of polymicrobic bacteria -- any bugs count. o Collection: Catheter o Diagnostic amount is less because of greater risk-factors and the patient's inability to concentrate the urine. o Risk-Factors: Anatomic Abnormalities Obstructive Uropathy Indwelling Catheters
www.brain101.info
STAPHYLOCOCCI STAPHYLOCOCCUS AUREUS: Gram(+) cocci in pairs or clusters. Name-Derivation: Grape-Like, Yellow-Gold Epidemiology / At Risk: Normal flora of anterior nares, skin, perineum. o Spread by sneeze and direct contact. Manifestations: o Cutaneous: Abscess, boil, carbuncle o Bacteremia: Targets kidneys, lungs, hearts, bone. Possible coagulopathy. The first thing you will see is an isolate abscess in an organ -- a clue that systemic S. Aures infection is occurring. You may also see petechial hemorrhages in fingernails, toes, and digits. o Osteomyelitis used to occur in children. Septic arthritis occurs in adults, associated with heroin IV-needle use. o Pneumonia: Especially in children, secondary to a viral infection. o Scalded Skin Syndrome: Bullous lesions leading to desquamation in infants. It is a result of the toxin -- not the bugs themselves. No bugs are found in the lesion. It will heal without scarring, if treated carefully and not spread. o Toxic Shock Syndrome: Result of TSS-Toxin. High-grade fever, headache, myalgia, hypotension, rash, diarrhea. o Food Poisoning: Abdominal cramps, diarrhea, vomiting, 2-12 hours after eating. Associated with mayonnaise kept at room temperature, such as at a picnic. o Endocarditis Processing: o Specimen: From lung, nose, skin. Can also be taken from a food sample. o Stain: Gram(+) Dead Gram(+) will appear as Gram(-) o Culture: Blood Agar (non-fecal specimen): Smooth colonies are indicative of polysaccharide. White or yellow beta-Hemolytic -- halos or zones of clearance around them. Mannitol Salt Agar (fecal specimen): Specimen from food poisoning. Used to distinguish S. AURES from S. Epidermidis. S. AURES ferments mannitol ------> pigmented colony. Staph likes to grow in the presence of salt, thus it is often found in salty foods. Broth Medium can be used to initially, to amplify the number of bugs collected. Identification: o CATALASE(+): Compare to Strep Pneumoniae. It will break down H2O2 in water to see bubbles. o COAGULASE(+): Free Coagulase Test for SPECIES ID. The bug coagulates blood in the absence of calcium. Place inoculum in rabbit serum with EDTA, to chelate calcium and remove it from reaction. Clot form after 4 or 20 hours (there are multiple coagulase types) ------> species is Aureus No clot forms ------> Epidermidis or Saprophyticus o Mannitol Test: ------> S. AURES ferments mannitol resulting in pigmented colonies, while the others don't. o HOT-COLD HEMOLYSIS TEST: Staph Aureus is the only one that has beta-Hemolysin and thus can damage RBC's at a cold temperature (4C). Other Staph bugs can't. Virulence: o Extracellular Enzymes: Coagulase: Clumps all the bugs up together ------> antiphagocytic. Impedes host defenses early in infection. Human plasma contains coagulase-reacting factor (CRF) which allows it to agglutinate with coagulase in the absence of calcium. Staphylokinase: Activates plasminogen ------> plasmin, which in turn degrades fibrin. Enhances dissemination by allowing bug to escape the fibrous gunk it makes with coagulase. Phage-mediated factor. Catalase: Inhibits killing by PMN's. Hyaluronidase: Enhances dissemination; important early on to establish infection. Lipase: Provides invasive entry. May penetrate sebaceous glands in eyelid and give us a sty. Nucleases: Permits the reuse of bug and host nucleic acids. beta-Lactamase
www.brain101.info
Exotoxins: HEMOLYSINS: alpha-Hemolysin: Leads to beta-Hemolysis, or complete hemolysis of WBC's and RBC's Kills WBC's as well as RBC's Transposon mediated Causes pore formation in blood cell membrane. beta-Hemolysin: Only damages membranes at a cold temperature, 4C; unique to Staph Aureus. At 37 it alone is not sufficient to produce hemolysis. gamma-Hemolysin: not much known delta-Hemolysin: Detergent, or surfactant-like action. Kills WBC's as well as RBC's. Panton-Valentine Leukocidin: Causes WBC lysis and divided into two components. SLOW COMPONENT binds to GM1 ganglioside in PMN membrane. FAST COMPONENT then uses phosphatidylcholine as a receptor to gain entry. EXFOLIATIN: Cleaves the stratum granulosum and causes desquamation in Scalded Skin Syndrome. Protein a: chromosomal. Protein b: plasmid-mediated. ENTEROTOXINS A, B, C1, C2, D: Affects the GI-tract in S. AURES food poisoning. They are heat stable -- heating (or reheating) food does not denature the toxin. Toxic-Shock Syndrome (TSS) Toxin: It is a superantigen. o Cell-Associated: Protein A: Binds the Fc portion of IgG, all four subclasses. It is antiphagocytic, anticomplement, antigenic, and mitogenic for T-Cells. It activates cell-mediated immunity and Type IV hypersensitivity response. Peptidoglycan: Confers hardiness and activates Alternative Complement pathway. Teichoic Acids: They act as a phage receptor. Ribitol Phosphate (Polysaccharide A) results in a lot of antigen-antibody complex formation -----> immediate type hypersensitivity. Surface Polysaccharides: Adhesins, antiphagocytic. Vaccine / Prevention: Wash your hands! Treatment: Antibiotics do not work! o
STAPHYLOCOCCUS EPIDERMIDIS: Gram(+) cocci in pairs or clusters. Epidemiology / At Risk: Normal flora of skin, mucous membranes. o Can be spread via catheters and may lead to bacteremia. We can treat the catheter tips with antibiotics and heparin in order to counteract the S. EPIDERMIDIS surface glycocalyx, and prevent it from interacting with platelets. Manifestations: OPPORTUNISTIC o Endocarditis o Bacteremia o Local infection involving catheters. Processing: o Stain: No hemolysis Does not ferment mannitol. Broth can be used for amplification. Identification: o CATALASE(+) o COAGULASE(-): Use Free-Coagulase Test to distinguish from S. AURES. o MANNITOL(-): Does not ferment mannitol. o NO PROTEIN-A, so it does not capture the Fc portion of IgG. Virulence: o SURFACE GLYCOCALYX: Surface slime is antiphagocytic and interacts with platelets in order to gain entry in IV catheters. Adhesin. o Teichoic Acid
STAPHYLOCOCCI SAPROPHYTICUS: Epidemiology / At Risk: Sexually transmitted.
www.brain101.info
Manifestations: Common pathogen in symptomatic UTI's. It adheres selectively to transitional epithelium. Identification: Same as S. EPIDERMIDIS, except Urease(+) Virulence: o Urease: Enable survival in urinary tract. o Tropic for urinary transitional epithelium. o Lysostaphin is lethal to S. AURES and other bugs.
www.brain101.info
ZOONOTIC INFECTIONS All REPORTABLE diseases BACILLUS ANTHRACIS: Gram(+) large rods with square ends. Name-Derivation: Anthracis = of sheep, cattle. Epidemiology / At Risk: o Cutaneous = 95% of infections. o Inhalation = 5% o Ingestion is not seen in the United States. Manifestations: ANTHRAX. o CUTANEOUS: Black Eschar, found on head, hands, forearms. Erythema and induration, but no pus. Any pus present would be a secondary bacterial infection. o PULMONARY: Wool-Sorter's Disease. Wool-spinners are at risk. Inhaled spores are phagocytosed by alveolar macrophages. Replication occurs in macrophage, then macrophage travels to lymph nodes where it disseminates. Fever, edema, and death within 24 hours from toxemia. o Ingestion: Dysentery followed by shock and death; not seen in USA. Processing: o Specimen: Aspirate of blister (eschar) fluid. o Stain: Gram-stain would show large rods, with squared end and no capsule. Methylene Blue, Giemsa stain is required to see the thin capsule. o Culture: It yields ROUGH colonies with no zone of hemolysis. The capsule is not grown in vitro (conditions are not right), so that they have attenuated virulence. Identification: o Bacillus genus is identified by rough, medusa-head colonies. o SPECIES: PENICILLIN: Anthracis species is identified by a String of Pearls formation in penicillin. The colonies are susceptible to penicillin, whereas other Bacillus species are not. gamma-PHAGE: Will attack and lyse Anthracis on a plate, but not other Bacilli. Can also do a Fluorescent Antibody of the cell-wall polysaccharide can be done -- but not the capsule, because the capsule isn't present in vitro! Virulence: o Cell-Associated: CAPSULE: It is composed of protein -- poly-d-Glutamic acid -- not polysaccharide. Antigenic and antiphagocytic. Plasmid-Mediated property, thus we can manipulate it for vaccine use. Cell-Wall Polysaccharide: Composed of N-Acetylglucosamine and d-Galactose. It cross-reacts with the Group-A blood type. Can be used in lab for ID. o Exotoxin: ANTHRAX TOXIN is a plasma-mediated, heat-labile toxin. It has three components. Protective Antigen: Binds to surface receptor. It is antigenic, and host-response yields protective antibodies (protective against toxin -- not against the bug). Edema Factor: Bug-derived adenyl cyclase enters host cell ------> cAMP ------> electrolyte and water loss. Lethal Factor: Metalloprotease enters and kills host cells. Mechanism unknown. Host Immune Response: Antibodies to the capsule and polysaccharide are not protective. Antibody to toxin is protective. Vaccine / Prevention: o CATTLE vaccine: Viable spores from an attenuated strain (they have no capsule), plus an alum precipitate (adjuvant) to improve immunogenicity. Edema factor and Lethal factor are also removed. o Humans: Only at-risk people. We give alum precipitate plus the protective antigen alone. Multiple shots required. Treatment: Penicillin.
www.brain101.info
BACILLUS CEREUS: Epidemiology / At Risk: o Food-Poisoning = refried beans and rice o Bacteremia = OPPORTUNISTIC. Nosocomial, immunocompromised patients. Manifestations: o Food-Poisoning in refried rice and beans is self-limiting to about 24 hrs. Early on (1-6 hrs): Nausea and vomiting Later (24 hrs): Profuse diarrhea o Bacteremia (contaminated catheters) in immunocompromised leads to meningitis, endocarditis, death. Identification: o B. Cereus is penicillin-resistant. They will form chains of rods rather than string of pearls in penicillin suspension. o gamma-PHAGE does not lyse it. Virulence: o Enterotoxins: Emetic Toxin: Heat stable, basis for early symptoms. Diarrheal Toxin: Heat labile, basis for late onset. Stimulates host cell adenyl cyclase ------> cAMP o Chromosomal beta-Lactamase and Cephalosporinase
BACILLUS SUBTILIS: Epidemiology / At Risk: Heroin preparations can be contaminated with it. Manifestations: Environmental contaminant that can cause very destructive lesions associated with heroin use. Identification: It is susceptible to penicillin.
FRANCISELLA TULARENSIS: Gram(-) rod. Name-Derivation: Named after who and where it was discovered. Epidemiology / At Risk: o Endemic to SE Kansas, carried by small mammals (via ticks). o Fewer than 50 organisms can cause a full infection! Manifestations: The bug is a facultative intracellular parasite of macrophages. o Initial infection ------> PMN's can't kill it ------> macrophages phagocytize it but don't kill it ------> travel to lymph nodes ------> very painful, suppurative infection of lymph nodes. o Lymph node clearance may take up to a year. Anorexia is common during this time. Processing: o Stain: Short-rods that are faintly gram-negative. Incorrectly referred to as "coccobacilli." Giemsa: Short-rods that stain more intensely at the poles. Fluorescent Antibody to capsular antigen is available in Kansas. o Culture: CYSTEINE-AGAR must be used. Must communicate with the lab what you're looking for! CO2 is also required for growth. Growth takes up to 3 days -- longer time than usual. Identification: o Smooth, gray colony on culture. o Antibody agglutination test to most virulent Strain A, which is endemic to Kansas. o SEROLOGY: Collect an early and late specimen Early would show 1:40 Ab titer, as Francisella cross-reacts with Yersinia antibodies. Late would show 1:320 titer -- 4X difference minimum to be significant. Virulence: o Intracellular Parasite of macrophages. This is most important property. o Capsule: Polysaccharide is antiphagocytic and confers serum resistance. Patient hypersensitivity to this polysaccharide will remain for years. Skin-tests can be done. Host Immune Response: o Activated (IL-2, cell-mediated) macrophages are necessary for protection. They can kill the organism. o Delayed hypersensitivity develops to cell wall antigens. Vaccine / Prevention: Live attenuated organism is used. Patient will develop antibody and delayed hypersensitivity. o Only used on lab workers.
www.brain101.info
YERSINIA PESTIS: Gram(-) rod. Epidemiology / At Risk: Rats and fleas. o SYLVATIC CYCLE: Infection cycle between carrier rodents and fleas. o URBAN CYCLE: New Yersinia strain kills large numbers of rats, and fleas spread the infection via dead rat carcasses. o BUBONIC CYCLE: Begins when fleas spread the bug to humans. Bacteria reproduce in flea to the point where they clog the proventriculus. Human bite ------> inoculation of bacteria into host. Manifestations: PLAGUE o BUBONIC FORM: Flea bite. Bite become indurated and necrotic. Buboes (swollen lymph node) results from initial flea bite. Bugs undergo large temperature increase from 25C to 37C, which initiates new virulence properties (YOP's and F1 antigen). High fever, bacteremia, pneumonia, sepsis. o PNEUMONIC FORM: Inhalation of aerosolized droplets spread by human to human contact (coughing). Fever, malaise, pulmonary edema, death within 24 hrs. Processing: o Specimen: Lymph node aspirate (painful) for bubonic form. Inject saline into lymph node and then withdraw saline. Pneumonic Form: blood, sputum, or lymph node. Special transport medium is necessary for transfer to protect handlers. o Stain: No gram stain. Wayson's stain shows a short rod. o Culture: Must advise lab. Specimen held at 28C to reduce virulence. Smooth brownish colonies. Iron is required for growth. Identification: o Agglutination test against F1 Capsular-protein o SEROLOGY: F1-Antibody Test after 5 days is diagnostic of plague. o Group classification is made based on the characteristics of the YOP's. Virulence: Plasmid-regulated. The factors themselves are on the chromosome, but the regulatory operons are on plasmids. o REGULATION: The plasmid is activated by signals that come from temperature change of 25C to 37C. o FLEA: Coagulase is produced at 25C, which entraps the bug in fibrinous material in the flea. This is how the proventriculus gets clogged, which leads to the flea regurgitation into humans. o HUMAN Virulence: All of these factors are activated at 37C. Order of events (first line of defense, second line). Fibrinolysin is produced at 37C, to dissolve the clot. F1 Antigen (Envelope): Antiphagocytic and antigenic. Ab is made but it is not protective. The bugs multiply like crazy. PMN's can't handle the sheer number of bugs, so macrophages come along as second line of defense. pH 6 Antigen allows the bug to survive inside the phagolysosomes of blood macrophages. Yersinia Outer Proteins (YOP's): V & W proteins are produced. They allow replication inside fixed macrophages in liver and spleen YOP's are also antiphagocytic for PMN's. o Other factors: Siderophore (iron) and an endotoxin that promotes fever. Host Immune Response: o Antibody to the F1 antigen promotes opsonization, but killing is not effective. o Activated macrophages (CMI) are required to kill the bug. Vaccine / Prevention: Quarantine is required. Rat control to prevent infection. Treatment: Streptomycin + Tetracycline. Tetracycline used prophylactically for at risk folks.
10
www.brain101.info
STREPTOCOCCI GRAM (+) COCCI, LACTOSE (+) STREPTOCOCCUS PYOGENES (GROUP A): Gram (+) Cocci in pairs or chains of 4 to 8. Epidemiology / At Risk: Spread by aerosolized droplets Manifestations: o SUPPURATIVE: Pharyngitis: 5-15 yrs old. Scarlet Fever: Pronounced oropharyngeal infection and rash. Strawberry tongue, with desquamation ------> raspberry tongue. Desquamation of outer skin layer on trunk. Caused by the virulence factor, Erythrogenic Toxin. Toxic-Shock Like Syndrome: Similar to Staph, it occurs as a result of Superantigen Erythrogenic Toxin A (SEA). Pyoderma: IMPETIGO: Cutaneous lesions in kids, usually on face. Very similar to the Staph bullous lesions, except that these are vesicular lesions because these are actually full of bugs. ERYSIPELAS: Cutaneous lesions in adults. Painful. Again contains organisms. Pneumonia: Bacteremia: Can lead to arthritis, osteomyelitis, endocarditis, meningitis. o NON-SUPPURATIVE: Sequelae Rheumatic Fever: 2-3 weeks after soar throat, low-grade fever and polyarthritis. Heart Murmur found, due to inflammatory process in heart. Theories to cause: Antibody to MAP protein cross-reacting with heart muscle. Small Strep protein may bind to cardiac muscle. Strep actually infect the heart valve, exposing our own antigens which are not normally exposed. Acute Glomerulonephritis: Can follow skin or throat infections. Associated with T-Antigen. Presence of DNAse Type B antigen is diagnostic. Renal shutdown, oliguria, and hypertension. Thought to be immune-complex disease. Processing: o Specimen: o Stain: Cannot do smear on throat culture -- normal flora (such as Strep Pneumoniae) would interfere. o Culture: Large zones of beta-Hemolysis seen on blood agar plate. Appearance of colonies goes from mucoid ------> smooth ------> rough. MUCOID: Producing a capsule. SMOOTH: Hyaluronidase attacks the bacteria's own capsules. ROUGH: In chronic patient, lots of protein being made. Todd-Hewitt Broth: Done when few organisms were recovered. Strep: Granular precipitates on sides and bottom of tube. Staph: Diffuse turbidity. Identification: o BACITRACIN: Group-A Strep = SENSITIVE. Group-B Strep is resistant. o OFFICE TEST, SWAB: Agglutination antibody to Group-A antigen. Positive test is diagnostic. Negative test -- get culture. Swab is put in nitrous acid to extract the Group-A antigen. o CATALASE (-): Compare to Staph. o ANTIBODY to STREP-O (ASO) TEST: Streptolysin-O is immunogenic and is found in Strep A, C, and G. Presence of ASO antibodies indicates that we have Strep A, C, or G, but does not indicate which one. Test: RBC's. If antibody is present, then the cells are not hemolytic, and the RBC's will settle at the bottom in the center of the colony, giving it the appearance of a button.
11
www.brain101.info
Virulence: o Cell-Associated: Cell-Wall Carbohydrate: Not an effective human antigen Peptidoglycan: Induces inflammation Lipotechoic Acid: Adheres to buccal mucosa, allowing colonization. Adhesin. M-Protein: Fibers extending from surface. Antigenically diverse (85 types) and immunogenic, to which we make protective antibodies. This means we could get 85 strep-throats in our lifetime. Antiphagocytic: Clumps PMN's and white cells. Interferes with alternate complement by binding Factor H Interferes with classical complement by inhibiting C3B deposition onto cells. M-Associated Protein (MAP): Antigenic, can cause cross-reaction with myocardial sarcolemma. T-Antigen: Associated with Glomerulonephritis. G-Protein: Binds Fc portion of IgG. Streptococcal Chemotactic Factor: Inactivates C5a. Shuts down inflammatory response in host. Capsule: During early inflammation, it is made antiphagocytic due to hyaluronidase. We can't develop antibody to the bugs until the capsule is lost. Capsule accounts for the smooth texture in colony. o Extracellular: Release right outside of cellular environment. DNAase: Four Types Type B: Is antigenic and is diagnostic for glomerulonephritis. Most prevalent in skin infections. Streptokinase: Works with TPA to digest clots. Can be immunogenic. Repeated therapies with streptokinase as a blood-thinner can result in hypersensitivity. Hyaluronidase: Degrades its own capsule, plus host connective tissue. Proteinase: Used to digest its own M-Protein. o Exotoxins Streptolysin O: Oxygen labile and not expressed in vitro. It is hemolytic in vivo. It lyses RBC's and WBC's under reduced oxygen tension. Damages platelets. Antigenic: Basis for the ASO test. Streptolysin S: Oxygen-stable. Hemolytic, but there is no lysis in vivo. Very small and not antigenic. Erythrogenic Toxin: Three types. Causes the rash seen in Scarlet Fever. Type-A also known as Superantigen Erythrogenic Toxin A (SEA), and causes Toxic-Shock Like Syndrome in the elderly. Host Immune Response: o Antibody to M-Protein is protective. o Antibody to Streptolysin O (ASO) is diagnostic for suppurative infection to Strep A, C, or G. o Antibody to DNAse B is diagnostic for non-suppurative sequelae. Vaccine / Prevention: Treatment: Penicillin-G will work. Strep to date is not resistant.
STREPTOCOCCUS AGALACTIAE (GROUP -B): Gram (+) Diplococci Name-Derivation: Agalactiae = associated with milk. Epidemiology / At Risk: Manifestations: o Neonatal Meningitis and Sepsis. Can be infected during birth by asymptomatic (normal flora) vaginal colonies. Processing: o Specimen: CSF or blood. o Stain: o Culture: Small zones of beta-Hemolysis. Larger beta-Hemolytic zones would be Group A Strep. Identification: o BACITRACIN: Group-B Strep = RESISTANT. Group-A Strep - Sensitive. o CAMP TEST: Mix normally non-hemolytic Staph Aureus with specimen, and hemolytic zone is augmented. Staph Aureus is normally only hemolytic at 4C. o SEROTYPES: 5 serotypes Group III is predominant one in meningitis. IgG vaccine for the mother is being worked on.
12
www.brain101.info
Virulence: o Capsular Antigens: Type III is associated with neonatal meningitis. o Can withstand bile in GI tract. Vaccine / Prevention: Under development for mother.
STREPTOCOCCUS EQUI (GROUP C): Name-Derivation: Equi = horse Epidemiology / At Risk: Major pathogen of horses, or person-to-person. Manifestations: o Skin suppuration: Cellulitis from skin breaks. Identification: o Agglutination with Group-C antiserum. Virulence: o Streptolysin O: Oxygen labile hemolysin, ASO (+). o Streptokinase: Antigenically distinct from Strep Group A. This one is used as a blood thinner. It is immunogenic and hypersensitivity can develop.
STREPTOCOCCUS BOVIS (GROUP D): Very similar to E. Faecalis Name-Derivation: Bovis = from cattle. Epidemiology / At Risk: Opportunistic Manifestations: o Respiratory, peritoneal infections. Processing: o Culture: alpha-Hemolysis (partial hemolysis) = green clearing close to the colonies. Source of color unknown. Identification: Compared to Enterococcus Faecalis o Penicillin sensitive.: Treatment: o Sensitive to penicillin.
ENTEROCOCCUS FAECALIS (GROUP D): Very similar to Strep Bovis Name-Derivation: feces. Epidemiology / At Risk: Normal GI flora. Manifestations: Multiple infections. Often a complication of cholecystitis. o GI obstruction may lead to bacteremia and endocarditis, due to bacterial resistances. Processing: o Stain: GRAM-VARIABLE -- both Gram (+) and Gram (-) found, alive. o Culture: Use blood agar with 40% bile and 6.5% NaCl. All three types of hemolysis found in culture. Identification: Compared to Strep Bovis (Group D) o Grows in the presence of bile. o Penicillin resistant. Virulence: o LIPOTECHOIC acid, very lipid rich, leads to gram-variable appearance. Treatment: Penicillin resistant, strongly, due to altered Penicillin-binding proteins. o Also have acquired vancomycin and gentamycin resistance.
GROUP G STREPTOCOCCI: Epidemiology / At Risk: Major animal pathogen, minor cause of human infections. Manifestations: o Cellulitis. o Synovium. o Bacteremia, endocarditis. Processing: o Specimen: o Stain:
13
www.brain101.info
o Culture: Identification: ASO (+) Virulence: o Streptolysin O: Oxygen labile hemolysin. o DNAse: Invasive. o Streptokinase: Antigenically unique.
STREPTOCOCCUS PNEUMONIAE (PNEUMOCOCCUS, DIPLOCOCCUS): Epidemiology / At Risk: #1 cause of community-acquired pneumonia. o Normal flora of oropharynx. o Viral flu, smoking, alcohol, old age, CHF predispose to infection. Manifestations: o Pneumonia: Lobar pneumonia with diffuse widespread consolidation. Sudden onset of symptoms. Productive cough, with mucopurulent rusty sputum. o Pericarditis and Pleurisy: Continuous spread from lungs can cause empyema and invasion of pericardium. o Bacteremia: 15-25% of cases. o Otitis Media: Infants. Processing: o Specimen: Sputum sample is very fragile. o Stain: Gram (+) lancet-shaped Diplococci. o Culture: Very large capsule gives a halo appearance to the colonies. Smooth colonies. Smooth colonies; alpha-hemolysis. Autolysis occurs after continued incubation -- center of colony becomes sunken inward. Identification: o Counter-Immune Electrophoresis (CIE): Can be done to look for capsular antigens. The capsule is not degraded and shows up in blood, urine, and sometimes CSF. o OPTOCHIN SENSITIVE: Compare to Strep Viridans. o Quellung Reaction: Would show positive Quellung with specific antisera against the sputum sample. Test not done anymore, 85 different serotypes are too many. o SEROTYPES: 85 serotypes; They are immunogenic, and antibodies are protective. Virulence: o Polysaccharide Capsule: #1 virulence factor. 85 different types. Type 3 can stick around post-infection and cause damage in lungs via antigen-antibody reactions. It is the most virulent and makes tons of capsule. o Extracellular Enzymes: Amidase: Causes autolysis, which releases Pneumo lysin-O. Neuraminidase: Helps to penetrate mucin and thus colonize the nasopharynx. Protease: Digest antibodies. o PNEUMO LYSIN-O: Factor released upon autolysis. Oxygen-labile hemolysin. Inhibits respiratory burst when inside PMN's. Cytotoxic for epithelial cells. o Cell-Associated: Forssman (F) Antigen: Inhibits amidase, therefore inhibits autolysis in vivo. M-Protein: Antigenic, but not protective. C-Polysaccharide: In cell wall. In acute infection, it induces inflammation. Promotes release of host CReactive Protein, which then acts with IgG to induce complement. Peptidoglycan Fragments: Induce inflammation and chronic necrosis. Host Immune Response: Vaccine / Prevention: PNEUMO-VAC VACCINE. It only includes the most virulent 25 or so serotypes -- those that cause bacteremia. o Given to at-risk folks: Splenectomy, old, HIV, diabetes, COPD, CVD. Latest recommendation says every 6 years. Flu shot is also recommended for prevention. o Kids under 2 can't get the pure vaccine (preventative for otitis media) -- must be conjugated to protein. Kid's vaccine is under development. Treatment: Penicillin is effective. Little resistance developed yet, but it is due to PBP's when present.
14
www.brain101.info
VIRIDANS STREPTOCOCCUS: Name-Derivation: Viridans = green, as it appears in culture. Manifestations: Important opportunistic organism in periodontal disease. o Bacteremia will lead to endocarditis, especially if heart valves were already damaged. Processing: o Culture: alpha-Hemolysis, appearing green. Identification: o OPTOCHIN-RESISTANT: Compare to Strep. Pneumoniae. Treatment: Penicillin-resistant. Combination therapy (aminoglycoside) required.
15
www.brain101.info
Bugs of Childhood HAEMOPHILUS INFLUENZAE: Short Pleomorphic Gram (-) Rods. Name-Derivation: o Haemophilus = blood-loving o Influenzae = discovered as part of flu epidemics. Epidemiology / At Risk: Infantile Meningitis. Manifestations: There are typable (encapsulated) and non-typable strains o TYPABLE: Haemophilus Type-B infections Infantile Meningitis: #1 cause in kids older than 3 months. Epiglottitis in kids 2 - 5, possibly with sepsis. Cellulitis in kids. Bacteremia: Can either be serum-sensitive (serum + complement lyse the bugs) or serum-resistant (serum + complement can't lyses the bug). Serum sensitivity is conferred by the LOS coat. The higher the molecular weight of the LOS, the worse is the bacteremia. High molecular weight LOS: Serum resistant. Low molecular weight LOS: Serum sensitive. o NON-TYPABLE: Otitis Media Bronchitis and pneumonia Processing: o Specimen: CSF from infants. o Stain: Gram (-) rods, but the poles tend to remain purple. Thus distinguishing with Strep Group-B can be a problem. o Culture: Both Smooth and rough colonies seen in culture. ABSOLUTE GROWTH REQUIREMENTS: Both derived from RBC's. Factor X: Hemin precursor. Factor V: NAD, used for organism pyridine synthesis. Chocolate Agar: Heat-lysed red blood cells. Fildes's Agar: Enzymatically (rather than heat) lysed RBC's. Satellite Growth: Put the bugs in blood agar with Staph Aureus, they will grow around the perimeter of the Staph. This is because the Staph Aureus lyses the RBC's and provides the needed nutrients for the Hib to grow around perimeter. Identification: o TYPABLE: Types a thru f, but Type b is the only important one. Other strands are not typable. QUELLUNG REACTION: Can be done on CSF to identify Hib. Add methylene blue to visualize: Positive test shows rod-shaped organisms with halo, due to swelling of the capsule. Can use CIE, ELISA, or Latex Agglutination to look for residual antigens left in blood, CSF, or urine. o NON-TYPABLE: Pleomorphic appearance on stain, still with intensity at the poles. Virulence: o Capsule: When present, it is the basis for typing. Type-B is made out of poly-ribitol phosphate. We don't really make antibodies to it, thus it is more virulent. We do make antibodies after repeated exposure. Presence of Ab is AGE-DEPENDENT: Infants younger than 3 months are protected by maternal IgG. Infants older than 3 months have lost maternal IgG immunity, thus they become susceptible to Hib meningitis. Immunity is re-acquired by age 10 due to cross-reactivity with Staph Aureus and E. Coli ribitol moieties. o Outer Membrane Proteins: Looking at them for a vaccine. Various ones are antiphagocytic and invasive. P2, porin protein is most promising candidate. o Lipo-oligosaccharide (LOS): Differs from LPS in that it has less sugar. Bacteremia does not result in the serious endotoxic shock of E. COLI, for example. The LOS coat inhibits movement of cilia in the airway and helps to establish infection. Molecular weight of LOS determines serum-resistance in bacteremia. o IgA Protease: Allows Hib to establish in upper airway. o beta-Lactamase: Plasmid-mediated. Host Immune Response: Antibodies are protective. IgG is the most protective.
16
www.brain101.info
Vaccine / Prevention: DPT Vaccine contains the Hib Conjugate -- Diphtheria Toxoid plus Poly-Ribitol Phosphate. 100% effective. o Vaccine administered at 2 months, 4 months, and 6 months. o PRP by itself can only be given to kids older than 2 years. PRP by itself is not as effective. The conjugate tends to elicit more of an IgG response (rather than IgM), which is what we want. Treatment: Treated based on antibiotic susceptibility test results. o Penicillin-Resistant. o Chloramphenicol-Resistant, via Chloramphenicol Acetyl-Transferase (which inactivates the drug).
BORDETELLA PERTUSSIS: Pleomorphic Gram (-) Rods Name-Derivation: Named after researcher Epidemiology / At Risk: Highly communicable and REPORTABLE. Manifestations: o WHOOPING COUGH: Bugs adhere to cilia up and down the airway. Systemic infection from a toxemia -- not a bacteremia. The organisms are non-invasive. Incubation Stage: (7-10 days). Mild respiratory manifestations. Catarrhal Stage: (1-2 weeks). More serious respiratory infections. This is the best time to collect the bugs, when the bugs are in the greatest number. Paroxysmal Stage: (2-4 weeks). Paroxysmal, rapid coughs, anoxia, followed by the "Whoop" sound to recover breath. Intense lymphocytosis is found, unusual for bacterial infection -- more common with viral infection. Vomiting Convalescent Stage: (3-4 weeks or longer). Pneumonia, convulsions from anoxia, other complications. o Subconjunctival Hemorrhaging found in the eyes (red around iris) in babies who have had Whooping Cough. Processing: o Specimen: Must use special Nasopharyngeal Swab, which contains no cotton. Cotton contains fatty acids that are lethal to the bug. Specimen is immediately inoculated at the bedside, either into transport broth or on a plate. o Stain: Gram Stain is of no value. Toluidine Blue stain used to visualize bugs. Look for small rods with bipolar intensity. Appearance is similar to Hemophilus. o Culture: Bordet-Gangeau Plate required -- must notify laboratory. Colonies become rough and lose virulence as they lose envelope, then can subculture for Gram stain. Identification: o Obligate Aerobe o Direct Agglutination or Direct FA can be done on cultured bugs. It is only reliable on the culture -- not on the original specimen. Virulence: o Cell-Associated: Polysaccharide Capsule: Essential for virulence. Filamentous Hemagglutinin (FHA): Filaments sticking out are adhesins to ciliated cells. Also immunogenic (protective) and hemolytic. Pertactin: Outer Membrane Protein, is an adhesin and is immunogenic. Antibody is protective, as it interrupts adhesion to cells. o Pertussis Toxin: AB-Toxin. Structure and Mode of Action: Fragment-B: Complex Hexamer, binds readily to ciliated cells. Fragment-A: ADP-ribose Transferase, transfers to Gi subunit to block Gi ------> cAMP. Effects of Pertussis via raised cAMP: Causes Histamine sensitization which causes us to cough. Turns on a lot of IL-4 production, which causes Isotype switching to IgE. This also will lead to increased vascular permeability. Lymphocytosis Hypoglycemia due to activation of pancreatic beta-cells. Toxin can also block some immune effector cells. o Adenylate Cyclase: Bug-derived, two isotypes. 70 kDa: Results in elevation of host cell cAMP.
17
www.brain101.info
100 kDa: Interferes with PMN phagocytosis and respiratory burst; hinders chemotaxis; hemolysin; impairs alveolar macrophage metabolism. o Other Toxins: Heat-Labile Toxin: Released upon lysis of the bug. Causes dermonecrosis (or surface necrosis) of ciliated epithelial cells upon release. Remember that B. Pertussis is not invasive. Heat-Stable Toxin: Endotoxin with Lipid-A, similar to LPS. Also contains Lipid X which stimulates protective antibodies. Tracheal Cytotoxin: A small peptidoglycan fragment. Ciliastatic. Vaccine / Prevention: DPT vaccine, at 2, 4, and 6 months. o Initial shots: DPT. Pertussis component is methiolate-killed whole organisms. o Booster Shots: DTaP. At 15 months and preschool, we use an acellular vaccine for a booster of FHA + Pertussis Toxoid. o Side-Effect: Risk of 1/300,000+ of encephalopathy. Treatment: Erythromycin.
CORYNEBACTERIUM DIPHTHERIAE: Gram (+) slender Rod. Epidemiology / At Risk: Communicable. Person-person contact. Manifestations: DIPHTHERIA primarily affects respiratory tract and skin. o Skin: Not systemic disease. Local cutaneous pseudomembranous necrosis of hands and feet. Host response contributed to damage. o Bull neck: Characteristic appearance found (similar to Mono), with enlargement of cervical lymph nodes. o Pseudomembranous Necrosis: Found in oropharynx in initial respiratory infection. o Systemic Toxemia: Diphtheria toxin affects three organs, in order: Heart: Nerves: Polyneuritis, anesthesia of palate Kidney: Only late course. DIFFERENTIAL: Vincent's Disease can be confused with this disease. Vincent's Disease is pseudomembranous pharyngitis, and is caused by poor oral hygiene. o Vincent's will show halitosis and signs of gingivitis (swelling, bleeding). o Stain with Vincent's disease will show a whole mess of bacteria -- both Gram (+) and Gram (-), while Diphtheria will show only slender Gram (+) rods. Processing: o Specimen: The Pseudomembrane must be cut with a surgical scissors -- not by tugging or pulling, as that will spread infection. o Stain: Methylene Blue: Pleomorphic slender rods, with Ernst-Babes bodies (granules) stained purple-red. o Culture: Must culture for toxin. Not every strand produces toxin (which is phage-mediated). Blood-Tellurite Agar: Special medium selective for Corynebacterium and Staph. Either bug will give rise to grey black colonies. Then do a Gram stain to differentiate the two. Coagulated Serum (Loeffler's) Agar: Can be used to determine presence of toxin. Supports both the bug and the toxin. Positive test will show creamy colonies. Identification: o TOXIN ID: Two alternatives. Precipitin Reaction: Take agar from above that is not completely hard. Apply filter paper containing antitoxin. Streak isolates of known positive and negatives across it. Look for Ab-Ag precipitation. Guinea Pig Rxn: Innoculate at Site A Administer antitoxin 5 hours later. Reinject at Site B 5 minutes later (antitoxin having been administered) Positive test occurs when only slight reddening occurs at Site B, while Site A undergoes necrosis. Virulence: o Diphtheria Toxin: The Tox Gene encodes for this toxin and is carried in a lysogenized beta-Phage. Iron Regulation: C. Diphtheriae codes for a gene called the Aporepressor. Aporepressor complexes with Iron (Fe+2) to successfully bind the beta-phage tox operon ------> inhibit toxin production. Absence of iron ------> disinhibition ------> toxin production ensues. AB-Toxin: Antitoxin works against Fragment-B to prevent binding. Once the toxin is inside the cell, the cell is doomed. Fragment-B binds to heart, nerve, and kidney cells.
18
www.brain101.info
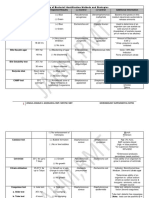
Fragment-A is an ADP-Ribose Transferase which binds to a His residue on Elongation Factor 2 (EL-2) ------> EL-2 can no longer accept amino acids from tRNA ------> inhibit protein synthesis -----> eventual cell death. o Lipase: Important in cutaneous lesions. o Neuraminidase: Acts on respiratory tract mucosa. o Siderophore: As long as iron levels are high, toxin level remains low. Unfortunately, inflammation and fibrinous exudate cut off iron supply. o Cornymycolic Acid: Cell wall glycolipids, contribute to invasiveness. o K-Antigens: Heat-labile, able to induce hypersensitivity. o O-Antigens: Heat-Stable polysaccharides. Hypersensitivity. Host Immune Response: Vaccine / Prevention: DPT Vaccine. Huge success story. o Children: Formyl-inactivated toxoid. Alum is added as an adjuvant. The additional antigens trapped in with the alum can be a source of hypersensitivity. o Adults: Same vaccine, but ammonium is used as the adjuvant. This eliminates some possible contaminating antigens that can cause hypersensitivity. o SHICK-TEST: Used to determine (1) whether or not your are susceptible to Diphtheriae (and need the vaccine) and (2) whether or not you will show hypersensitivity (and thus would need the special vaccine) TOXIN TOXOID Used to check for hypersensitivity 36 hrs Neg 120 hrs Neg Shick-Positive: Patient is susceptible to Diphtheria toxin, and can be immunized with regular vaccine. REPORT
Used to check for presence of antibody 36 hrs Neg 120 hrs Pos erythema and inflammation found Neg Neg Neg Neg
Neg Pos
Neg Neg
Shick-Negative: Antibodies to Diphtheria toxin were present. Patient doesn't need vaccine. Hypersensitive: Patient is hypersensitive to toxoid. He is Shick-negative and doesn't currently need a vaccine, but would need the adult vaccine if one is ever needed in the future. Cross-Reaction: Patient is both susceptible to diphtheria toxin, and hypersensitive. Adult vaccine is required.
Neg
Pos
Pos
Neg
Treatment: Use antitoxin to collect up free toxin in blood. Erythromycin.
19
www.brain101.info
GRAM-NEGATIVE PNEUMONIAS KLEBSIELLA PNEUMONIAE: Gram (-) Rod Name-Derivation: Klebs was a researcher. Epidemiology / At Risk: Male, malnourished, alcoholic pneumonia. "VA pneumonia." o Transient normal flora of throat. Manifestations: o Pneumonia: Acute lobar pneumonia with highly productive cough. Productive cough. Thick, mucinous, messy, bloody sputum. Focal lung abscesses in late infection lead to bacteremia. o Bacteremia with secondary Meningitis o Wound Infections o UTI Processing: o Culture: Blood Agar: Difficult to define boundaries because the bugs are so mucinous. Selective Medium: Used to inhibit Gram (+) growth; will yield smooth and mucinous colonies. Identification: o Lactose (+) o Serotypes: 77 Virulence: o Capsule: THICK capsule is antiphagocytic. Confers serum resistance ------> bacteremia. o beta-Lactamase o Enterotoxin: Plasmid-mediated. Causes vomiting and diarrhea. o Endotoxin: LPS, fever, hypotension. Treatment: Penicillin-Resistant. Use cephalosporins and broad-spectrum.
LEGIONELLA PNEUMOPHILA: Faintly staining Gram (-) rods. Part of its own family, Legionellaceae. Name-Derivation: Named after American Legion convention, site of initial outbreak. o Family classification based on unique lipid in cell wall. Epidemiology / At Risk: Legionella are abundant in water, particularly at cool temperatures. They are natural intracellular parasites of non-pathogenic amoebae in rivers in lakes. o Aerosolized mist colonizes upper airways. o Associated with air conditioners. o Non-communicable Manifestations: Legionnaire's Disease o Pneumonia: Non-productive cough. Pulmonary fibrinous exudate. Multifocal necrotic lesions. Pulmonary infiltrates on X-Ray. o Toxemia (toxin unidentified) gives us liver dysfunction and CNS toxicity. Also forms the basis for serology tests. o Pontiac Fever: Milder form of disease. Self-limiting, headache, myalgia, fever. Processing: o Specimen: Trans-Tracheal Aspiration; Broncho-alveolar lavage. o Stain: Dieterle Silver Stain shows rod shaped bacteria within macrophages. NO STAIN with Gram Stain, Acid-Fact Stain, or H&E. o Culture: CYSTEINE is absolutely required for growth. Must notify lab! 3-5 days required for growth. Identification: o 14 Serogroups Group 1 accounts for the majority of cases. o Direct Fluorescent Antibody (FA) to Group-1 is diagnostic. If negative, must try to culture. o ELISA or RIA test for polysaccharide antigen in urine. o Serology: Backup tests when culture fails. Tested antibodies are non-protective. Acute:Convalescent titer of 4X, or absolute titer of 1:256 is diagnostic. False negatives common; some never develop antibodies.
20
www.brain101.info
Can test for Serum antibody to heat-shock antigens. o Catalase (+) Virulence: o Facultative Intracellular Parasite of macrophages and PMN's. Inhibits phagolysosome formation. Catalase prevents killing once inside, similar to Francisella. Macrophages take in the bug by a process known as Coiling Phagocytosis -- they wrap a finger around the bug. Macrophage-Infectivity Potentiator (mip): o Lipids in Cell-Wall: gives organisms thermal resistance. o Catalase o Metalloprotease: Hemolysin, sequestering iron for growth. Degrades Fc receptors and complement receptors, impairing opsonization. Cleaves IL-2, impeding cell-mediated response. Impedes T-Cell activation. o beta-Lactamase Host Immune Response: It's an intracellular parasite, so cell-mediated immunity (activated macrophages) are required for protection. Vaccine / Prevention: Hyperchlorination of tap-water. Treatment: Erythromycin.
PSEUDOMONAS AERUGINOSA: See UTI's section.
21
www.brain101.info
MYCOBACTERIA Facultative Intracellular Parasites Catalase (+) MYCOBACTERIUM TUBERCULOSIS, MYCOBACTERIUM BOVIS: Acid-Fast Rods Name-Derivation: Forms tubercles in lung. Epidemiology / At Risk: COMMUNICABLE during primary infection. o Approx. 10 million new cases every year. o Low treatment compliance and thus multi-drug resistance is a big problem. o Urban / HIV / poverty / AIDS o Caring for a single TB patient is extremely expensive. Manifestations: TUBERCULOSIS o Primary Pulmonary Tuberculosis: Very small number of bugs needed to infect. Bugs live intracellularly in macrophages. They are strict aerobes and thus prefer the apical lobe of the lung. Hilar Lymphadenopathy: Macrophages carry the bugs to the hilar lymph nodes. Unproductive cough, low-grade fever, anorexia, night sweats, fatigue. Localized granulomas, tubercles, formed in lung. o Miliary Tuberculosis: Disseminated tuberculosis that results from bacteremia. Likes to go to kidneys, bones, meninges. o Reactivation Tuberculosis: Occurs when quiescent granuloma reactivates. You never get rid of the bug. Seen in immuno-compromised cases, or just spontaneously. Processing: o Specimen: Not easy to get bugs. Collected by spraying warm saline and withdrawing, right when patient awakes. Use N-Acetyl-L-Cysteine, an anti-mucus agent, to free bugs from the macrophages in the sputum. Then apply NaOH to remove contaminants. Then centrifuge and resuspend the sediment in a phosphate buffer. o Stain: Acid-Fast Smear is done on the suspension from the prepared specimen above. Acid-Fast rods is not diagnostic, as it may be some other Mycobacterium species. o Culture: Must be obtained to verify M. Tuberculosis. Takes 3-8 weeks for culture results. Lowenstein-Jensen Medium: Selective medium inhibits growth of normal flora. Penicillin added. Rough Colonies = More Virulent! This is just like with B. Anthracis. Liquid Bactec: Faster method, 1-2 weeks. Look for radioactive byproduct of metabolism. Luciferase gene in phage is used for antibiotic susceptibility testing. Luciferase product releases light when bug is alive and replicating. Thus, loss of light = susceptible. Identification: o Strict Aerobes o NIACIN: M. TUBERCULOSIS: Niacin(+) M. bovis: Niacin(-) Virulence: o Obligate Intracellular Parasite: Thus cell mediated immunity is required for defense. Can only replicate within macrophages. o Catalase, Peroxidase o Cord Factor: Lipid. Causes serpentine arrangement of growth. Inhibits PMN migration Activates Complement damages mitochondria Protect against dessication. o Sulfatides: Glycolipids in cell wall. Wax-D: Mycolic acid with a little peptidoglycan. Acts as an adjuvant. It is a component of Freund's adjuvant. Freund's Incomplete Adjuvant: Contains Wax-D. Freund's Complete Adjuvant: Simple dead M. TUBERCULOSIS, used in animals only. o Siderophores: Exochelin = extracellular factor released to get Fe+2 from environment.
22
www.brain101.info
Mycobactin: Membrane bound, binds to the exochelin to bring it in. Proteins: Tuberculin is antigenic and immunogenic (but not protective). Peptidoglycans: arabinagalactans. Antigenic, responsible for hypersensitivity reaction, and contributes to caseous necrosis. Host Immune Response: Antibodies not protective. Cell-mediated immunity required. Vaccine / Prevention: BCG Vaccine only administered to high-risk folks. Protection is relative -- not absolute. It prevents bacteremia and dissemination. o Innoculate with live, attenuated M. Bovine strain. o Must be TB-free before getting the vaccine: 100 TU skin test must come back negative. If positive, then we assume the patient has already been exposed. 3 months later, test for hypersensitivity. Test again. Then you can give vaccine. o The BCG vaccine renders the PPD skin test useless. PPD SKIN TEST: Indicates whether or not you have been exposed to Tuberculosis before. o The BCG vaccine renders the test useless. o 1 TU: Very dilute, used with young people, people with demonstrated hypersensitivities, or people showing ocular tuberculosis. o 5 TU: TINE Screening Test. Injected intradermally. If positive after 48 hrs, then do a Mantoux to verify. Mantoux Test: Diagnostic for TB. Use pen to outline the zone of induration. > 10 mm: Positive TB test. Has been exposed before. 5-9 mm: Cross-reacting. May be infected with another Mycobacterium. < 5 mm: Negative TB test. HIGH-RISK: > 5 mm is positive. For immunocompromised. LOW-RISK (health-care workers): > 10 mm is positive. NO-RISK: Healthy businessman having no situational exposure. > 15 mm is positive. o 250 TU: Used for prognostic purposes only, to check for adequate cell-mediated response. High amount required in order to elicit a response above baseline presence of the antigen. Treatment: Multi-Drug Resistance is a big problem! Common to treat with 4 antibiotics. MDR has an 80% mortality rate. o Popular drug-combo: Isoniazid, Rifampin, Pyrazinamide, Ethambutol. o Primary Resistance: Primary infection shows resistance. o Secondary Resistance: Resistance arises in a reactivation disease. o o
MYCOBACTERIUM AVIUM COMPLEX (MAC): RUNYON GROUPING: Individual manifestations. o GROUP I: Photochromogenic M. Kansasii: Pulmonary disease with single cavitation. Number one mycobacterium in Nebraska. PPD: Kansasii is cross-reacting, thus a cross-reacting PPD test does not preclude this organism. M. Marinum: Likes water and pools, swimming pools. Cutaneous skin lesions. PPD: Marinum is cross-reacting, thus a cross reacting PPD test does not preclude this organism. o GROUP II: Scotochromogenic M. Scrofulaceum: Produces cervical lymphadenitis in kids. Lymph node is usually removed. PPD: Usually a negative PPD test, i.e. < 5 mm. o GROUP III: Non-Chromogenic M. AVIUM-INTRACELLULARE: Emerged from HIV epidemic. ORAL portal of entry with AIDS, usually ------> GI Tract ------> Bacteremia, with concurrent severe anemia, although it is evidently not due to the MAI. Fatal in AIDS patients. Usually from liver dysfunction. Pulmonary manifestations identical to Tb. SENSITIN SKIN TEST: Can be used for MAI. It cross reacts with Tb, but you want to look for the one that yields the larger diameter. If MAI yields the larger diameter, then it is Tb that is cross reacting and the infection is actually MAI. o GROUP IV: Rapid Growers M. Fortuitum: Cutaneous lesions resembling more of an abscess than an ulcer. o NON-RUNYON: M. Ulcerans, slow-grower.
23
www.brain101.info
Epidemiology / At Risk (GENERAL): Ubiquitous in nature. o A high dose of the bug is needed for infection. Processing: o Stain: Acid Fast o Culture: Require two to three weeks at least to grow out. Virulence: o Obligate intracellular parasites o Catalase Treatment: Generally resistant organisms. Multiple antibiotics required for treatment.
MYCOBACTERIUM LEPRAE: Epidemiology / At Risk: Manifestations: LEPROSY o Tuberculoid Leprosy: Small, organized tuberculoid lesions (granulomas) on skin. Hypopigmented lesions. Cannot be distinguished from contact dermatitis. Skin, nerves. Cutaneous anesthesia results from occupations of nerves. o Lepromatous Leprosy: Unable to mount cellular response (anergic) to the bugs, resulting in much worse skin lesions. No granulomas are formed. "Lepra" cells can be seen. Affects skin, nerves, eyes. Processing: o Specimen: o Stain: Acid-Fast o Culture: Has never successfully been grown up in culture! Can use Armadillo or Mouse footpad models for live hosts. Identification: Virulence: o Obligate Intracellular Parasite inside Macrophages. Can inhibit macrophage phagolysosome fusion. o CD8+ Suppressor Cells prevent Granuloma formation in Lepromatous form. o Phenolic glycolipid appears to be key antigen. Host Immune Response: Vaccine / Prevention: o SKIN TEST: Antigen was sequestered from Armadillos, who are quite affected Leprosy. Skin Test can be used only for prognosis. A good (> 10 mm) response indicates that patient can mount a good response, so lepromatous form should result. Treatment: Sulfa drugs.
24
www.brain101.info
ENTEROBACTERIACEAE YERSINIA ENTEROCOLITICA: Gram-Negative Rod Epidemiology / At Risk: Infected from animals especially during cold season. Manifestations: Outcome of disease depends on age o Less than 5: Acute watery diarrhea that goes on for about a week. o 5-15 years old: Acute mesenteric adenitis. Can be mistaken for appendicitis. o 10-20 years old: Acute terminal ileitis,"Pseudo-Crohn's" disease. o Adult: Diarrhea. Liver disease can predispose to sepsis. o HLA B27 gene: Post-infectious arthritis. Processing: o Specimen: Feces, joint fluid (for HLA B27), lymph. o Stain: Must first be put in enrichment broth before staining. o Culture: Enrichment Broth: Bugs are put in enrichment broth before staining, as number of collected organisms is low. COLD TEMP: 28C Identification: Biochemical tests for species. Virulence: o Invasin Gene: Adhesin and invasion. Attachment-Invasin Loci: Genes that control the invasin gene. o Yersinia factors: shared in common with, or similar to, Y. Pestis. Yersinia Outer Proteins (YOP's): Adhesin proteins, regulated by presence of calcium and temperature. YOP-1: Four important properties Confers serum resistance Autoagglutinates the bug, which makes it harder to phagocytose. Mannose-resistance Hemagglutination (not attracted to mannose) Adhesin Yersinia Adherence Protein (Yad-A): Adhesin, binds to fibronectin, fibrinogen, collagen. Blocks both alternate and classical complement. V & W Antigens: Lipoprotein, antiphagocytic. o Arthritogenic Factor: Factor important in arthritis in HLA B27 patients. beta-subunit of urease. Stimulates TH1 CD4+ cells. o Enterotoxin: Stimulates cGMP to cause diarrhea.
CAMPYLOBACTER JEJUNI: Wavy Gram (-) Rod Name-Derivation: Campylobacter = curved bacterium Epidemiology / At Risk: From cattle. Manifestations: o Invasive gastroenteritis, causing ulcers, crypt abscesses, hemorrhagic necrosis. o Blood and pus found in feces. Processing: o Specimen: Feces or rectal swab. o Stain: Gram-negative rod with spiral or helical appearance, due to heavy tuft of flagella at one end. o Culture: Campy Agar HIGH TEMP 42C -- must notify lab! Identification: Microaerophilic Virulence: o Antigenic Diversity is key virulence property. They are hard to type epidemiologically. Constant change of O and H antigen types. o Flagellum for motility and propulsion into mucosa. o Enterotoxin: Stimulates cAMP. Heat-labile, denatured by boiling the milk. o Cytotoxin: Injurious to enterocytes. Host Immune Response: Fairly easily killed by PMN's if they can be phagocytosed.
25
www.brain101.info
CAMPYLOBACTER FETUS: Wavy Gram (-) Rod Name-Derivation: Campylobacter = curved bacterium Epidemiology / At Risk: Contaminated food, milk, or water. Manifestations: Bacteremia -- no diarrhea symptoms, even though the initial infection is via GI tract. o Bacteremia disseminates to, in order of importance: Meninges, aided by propulsion of flagella. Lungs, with contiguous spread to pleura Joints Suppurative Arthritis early on; specimen can be collected. Rheumatoid Arthritis can occur post-infection. Heart Valves, causing endocarditis. o C. Fetus like to get inside vascular endothelial cells, causing hemorrhagic necrosis. It isn't essential, but they like it. Processing: o Specimen: Blood, CSF if you suspect meningitis, joint fluid when suppurative. o Stain: Gram-negative rod with spiral or helical appearance, due to heavy tuft of flagella at one end. o Culture: Campy Agar. LOW TEMP 25C -- must notify lab! Identification: Microaerophilic Virulence: o Antigenic Diversity is key virulence property. They are hard to type epidemiologically. Constant change of O and H antigen types. o Protein Capsule: Unique among Gram (-)'s. Antiphagocytic, confers serum resistance. o Tropic for endothelial cells. It likes to live inside vascular endothelial cells. Host Immune Response: Fairly easily killed by PMN's if they can be phagocytosed.
HELICOBACTER PYLORI: Wavy Gram (-) Rod Name-Derivation: Originally part of Campylobacter, then given its own genus. Helical = wavy. Epidemiology / At Risk: Manifestations: o Type-B Gastritis: Inflammatory, pyogenic infection of antrum and goblet cells. pH remains normal. o Type-A Gastritis: Autoimmune disease against parietal cell resulting in pernicious anemia. pH is high due to damaged parietal cells. Processing: o Specimen: Must be taken by gastric endoscopy. No specimen is usually collected. o Stain: o Culture: Campy Agar NORMAL TEMP 37, as compared to the Campylobacter Identification: Microaerophilic o UREASE (+) o Catalase (+) o UREA BREATH TEST: Give patient radiolabeled 14C urea, then monitor for the appearance of the 14C in their breath or blood, indicating that it has been broken down. Quick and easy test. Virulence: o Flagellum: Number one property allowing it to invade gastric mucosa. o Mucinase helps penetrate mucin layer. o Fibrillar Hemagglutinin: Adhesin. It hooks to a glycero lipid in host cell membrane. o Catalase: Can survive (not replicate) inside PMN's. o Urease: Thought to create a basic microenvironment which damages intracellular junctions in stomach. o Oxidase Treatment: Three antibiotics, plus Bisthmus (Pepto-Bismol) as a coating against acid damage.
CLOSTRIDIUM DIFFICILE: Gram (+) Rod, Spore-former. Not an Enterobacteriaceae. Epidemiology / At Risk: Spores found in soil and are usually ingested. Can be opportunistic. o Endogenous Infection: Spores that were otherwise silent become activated when normal flora is depressed by antibiotics. o Exogenous Infection: Nosocomial infection in the hospital.
26
www.brain101.info
Manifestations: Processing: o Specimen: Fecal filtrate is taken for toxin assay. o Stain: o Culture: Egg-yolk agar with antibiotics. Identification: o Obligate anaerobe o Serogroups A - G o Can be identified through Gas Liquid Chromatography. o Toxin Test: Toxin is present only in some of the strains. Must determine whether it is present. Put feces specimen filtrate in two dishes. Add antitoxin to one of the dishes. Positive Test: One dish remains toxic, while the other dish is neutralized. Negative Test: Neither dish is toxic. Low Specificity: The antitoxin can cross react with other toxins. o ELISA can identify C. Difficile toxin. Virulence: o Exotoxin A: Protein that damages the intestinal mucosa. It attracts PMN's and causes them to degranulate, resulting in more damage. o Exotoxin B: AB-Toxin that disrupts the cytoskeleton of enterocytes. Fragment-A gets inside with the help of a host-cell protease. Mechanism of damage unknown. Treatment: Treatment has a high relapse rate. o Discontinue broad-spectrum antibiotic therapy. Replace lost fluid and electrolytes. o Do not interfere with diarrhea. Let it run its course. o Vancomycin (some resistance has shown) or metronidazole is used when necessary.
ESCHERICHIA COLI (ENTERIC): Gram (-) Rods Epidemiology / At Risk: o UTI's o Gastroenteritis o Wound Infections o Pneumonia o Meningitis in Infants o Sepsis Manifestations: GI manifestations depends on strain. Virulence factors included. o Enteropathogenic E. COLI (EPEC): Cause Travelers's Diarrhea -- loose stools, plus mild GI complaints, such as nausea, vomiting, or even tenesmus. Has also been called Entero-Aggregative E. COLI (EAEC) because of their tendency to aggregate. o Enterotoxigenic E. COLI (ETEC): Watery diarrhea, as opposed to loose stools. Diarrhea acts on the small intestine. Labile Toxin (LT): Heat labile AB-toxin kicks water out by up-regulating cAMP. Fragment-B: Binds GM1 Ganglioside in small intestinal enterocytes. Fragment-A: ADP-Ribose Transferase. Transfers ADP to a Gs Stimulatory subunit ------> cAMP. LT is also a large molecule and a potent antigen. LT-IIa and Iib: Antigenic variants of labile toxin. Stable Toxin (ST): Heat stable AB-Toxin, prevents water from being reabsorbed in small intestine. Fragment-A: Up regulated cGMP ------> inhibit reabsorption of Na, Cl, and water in brush border. o Enteroinvasive E. COLI (EIEC): Causes dysentery in addition to the watery diarrhea. The new cytotoxin acts in the colon, while watery diarrhea continues to occur from the small intestine. Verotoxin: Phage-mediated Shiga-Like Toxin is cytotoxic to colonic enterocytes. It inactivates protein synthesis at the 60s ribosome and kills the cell, resulting in hemorrhagic necrosis. Invasin: Gene allows the E. COLI to live intracellularly inside colonic enterocytes. o Entero hemolytic E. COLI (EHEC): Causes Hemolytic Uremic Syndrome (HUS). In addition to the dysentery, it has a hemolysin and is tropic for transitional epithelial cells. Symptoms: Hemolytic Crisis Thrombocytopenia Disseminated Intravascular Coagulopathy (DIC) Acute Renal Failure Hemolysin: Plasmid-mediated factor that lyses red-blood cells. It is also a nephrotoxin.
27
www.brain101.info
Processing: o Specimen: o Stain: Gram-Stain is not done on fecal specimens. o Culture: Selective Medium (always used on Enterics), which inhibits Gram (+) and contains lactose, in order to differentiate lactose-fermenting genera. Identification: Lactose-Fermenting o Motile o Huge Antigenic Diversity: Flagellar H-Antigen is divided L, A and B subtypes. With Neonatal sepsis and meningitis, lab will report a B-subtype as it is associated with prognosis. The LAB subtypes indicate how easily the flagellar antigens come off with heat. o Mannose-sensitive hemagglutination, because of F1 pilus antigen. Virulence: Only cell-associated factors. o Pili (F-Antigen): Fimbriae. 10 F Antigen types. Adhesin. F1 Antigen is found in all E. Coli. (chromosomally coded). It is Mannose-Sensitive, i.e. does not agglutinate RBC's in the presence of mannose (because it prefers to stick to the mannose). Mannose sensitive is important to us as normal carriers of E. COLI. It helps E. COLI stick to mucosal (vaginal, GI, buccal) surfaces and protect them. F2 - F10 Antigens: They are all mannose-resistant. One of them is the P-Antigen, associated with Pyelonephritis. o Capsule (K-Antigen): Important in UTI's and Meningitis. Antiphagocytic, serum resistance. o Outer Membrane Proteins: Protein-A confers serum resistance. o Siderophore: Aerobactin o LPS: Lipid-A is the specific component which is a superantigen and makes up endotoxin. Vaccine / Prevention: o The Core Polysaccharide, common to all strands, has been looked at. But whenever we target it, E. COLI respond by making new surface (O-Antigen) polysaccharides. Treatment: Run the risk of inducing endotoxic shock when treating bacteremia.
SHIGELLOSIS: Different Species: o S. Sonnei: Found in U.S. o S. Flexneri: Found in U.S. o S. Boydii: Found in U.S. o S. Dysenteriae: Found mostly abroad, and contains the extra Shiga Toxin. Epidemiology / At Risk: Communicable. Very low infective dose of only 200 - 500 bugs. Manifestations: Ulcerative colitis. Invasive disease. o Children in U.S. with Shigellosis can experience bacteremia and CNS toxicity. Processing: o Specimen: Ulcer swab or feces. Special transport medium required. The organic acid by-products of other normal flora are toxic to the Shigella bugs. o Stain: o Culture: Selective Medium Identification: Non-Lactose Fermenting o Non-Motile, thus no H-Antigen. Virulence: o Surface Polysaccharide: Plasmid-mediated, adhesin and invasin. o Outer Membrane Proteins: Invasin allows mucosal penetration by receptor-mediated endocytosis. Details uncertain. o Hemolysin: Plasmid-mediated (only some strains have it). Disrupts phagolysosome formation and allows intracellular replication in PMN's. They can also actually infect neighboring cells, eventually leading to an ulcer. o SHIGA TOXIN: Only present in the S. Dysenteriae strain, making it the most virulent. In the small intestine, it blocks absorption of NaCl, glucose, and water. In the colon, AB-Toxin. Fragment-B binds a glycolipid on colonic enterocyte. Fragment-A gets internalized and is then known as Fragment-A1, which is an N-Glycosidase. It removes adenine from the 28s rRNA and irreversibly in activates protein synthesis at the 60s ribosomal subunit.
28
www.brain101.info
Some of the U.S. bugs produce a Shiga-Like toxin that produces similar effects -- not but Shiga toxin, and details are not characterized. Treatment: Shigellosis is a public health issue. Antibiotic treatment is required.
SALMONELLA ENTEROCOLITICA (ENTERICA GROUP 1): Gram negative rods. Epidemiology / At Risk: Communicable o Animal to human transmission. o There are over 2000 species of Salmonella. Ubiquitous in environment and many people act as carriers (bugs live in bile duct). o Large infective dose is required for infection. Manifestations: Enterocolitis self limiting to 2-7 days. o Nausea, vomiting, non-bloody diarrhea, fever, abdominal cramps, headache. o Can be asymptomatic. o Can penetrate mucosa but doesn't cause much damage. o No Bacteremia Processing: o Specimen: Feces or blood. o Stain: Not on the feces; direct microscopy not helpful. o Culture: Selective Medium, including bile and lactose. These bugs really love bile. Identification: o Non-lactose fermenting o Motile: Compare to Shigella. o Serogrouping: Very high antigenic diversity. O-Antigen: 4 serogroups DNA Hybridization: 6 groups. Type 1 is most common in U.S. Biphasic expression of the flagellar (H) antigen. Changes throughout growth. Virulence: o Flagellum (H-Antigen): Motility. Biphasic antigen expression in early and late growth makes the bugs hard to fingerprint. o Polysaccharide (O-Antigen): Adhesin to mucosa. o Capsule (K-Antigen) o Outer Membrane Proteins: Adhesin helps them adhere to neighboring cells in the lamina propria. Causes degeneration of the brush border (diarrhea) and fever. o Pili: Mannose-Sensitive hemagglutinins. Adheres to intestinal epithelium. o LPS Endotoxin: Common to all the serogroups. o Enterotoxin: Cause diarrhea, similar to the E. COLI enterotoxins. o Cytotoxin: In the colon, inhibits protein synthesis. Host Immune Response: Vaccine / Prevention: Treatment: Do NOT treat. It only prolongs the carrier state. Only treat symptomatically.
SALMONELLA TYPHI: Epidemiology / At Risk: Human to human transmission only. o Large infective dose. o Mortality Rate: 2-10% o Relapse Rate: 20% Manifestations: Typhoid Fever o Symptoms: First Week: Constipation with step-wise fever and malaise. Second week: Bacteremia. Sustained fever. Rose Spot Rashes are discrete rashes on the trunk. Diarrhea: Intestinal necrosis, severe bleeding, thrombophlebitis, cholecystitis, pneumonia, focal abscesses. Carrier State following resolution -- may last up to a year. Bugs localize to the bile ducts. o PATHOGENESIS: Organisms multiple in the lamina propria, lymphatics, and monocytes of the small intestine. They then invade and disseminate to reticuloendothelial system, leading to sustained bacteremia. At the liver, organisms re-invade the GI-Tract via the gallbladder.
29
www.brain101.info
COMPLICATIONS: Intestinal perforations Thrombophlebitis. Cholecystitis and gallstones Patchy necrosis caused by complement fixation and PMN inflammation. DIC and focal abscesses. Processing: o Specimen: Blood can be taken in early in infection. Feces can be taken in late infection (when diarrhea starts) o Stain: Not useful. o Culture: Enteric Selective Culture containing lactose and bile. Culture under aerobic conditions 1- 7 days. Will show motile bugs with smooth colonies. Identification: o Non-Lactose fermenting o Motile o Facultative intracellular parasite. Virulence: o Capsule Antigen (Vi): Polysaccharide, antiphagocytic, serum resistance. This enhances survival inside monocytes. Immunogenic and basis for partial-vaccine. o Intracellular in Monocytes: Facultative intracellular parasites of monocytes. The capsule protects them from destruction. o Flagellar (H) Antigen: Biphasic antigenic expression. o Outer Membrane Proteins (O-Antigens): Antiphagocytic inside monocytes. Enhances resistance to non-oxidative cationic proteins (defensins) inside PMN's. o Endotoxin. Vaccine / Prevention: o TAB Vaccine: For travelers, short-term temporary protection. Passive antibody to the Vi antigen, allowing for phagocytosis and good complement response. o Prevention: Chlorinate water, sewage disposal, cook your food. Treatment: Carrier state may be prolonged by antibiotic treatment. Cholecystectomy may be needed. o
VIBRIO CHOLERAE: Halophilic (salt-loving) Gram-negative rod. Epidemiology / At Risk: Highly communicable in areas of poor sanitation. o Cholera tends to spread in epidemics. o Humans are host; crustaceans are a vector. Infection via seafood or infected water. Manifestations: o Cholera: Very watery profuse diarrhea. Rice-water stools. o Vomiting and muscular cramps o Dehydration can lead to oliguria and collapse. o Non-invasive. No damage to intestinal epithelium. Diarrhea is strictly via the exotoxin. Processing: o Specimen: Food, water, stool. Transport medium at pH > 8, which suppresses contaminating organisms. o Stain: Dark-field stain only, will see small curving rods with darting motility. It's a comma-shaped bug with long flagellum. o Culture: Identification: o Motile o Oxidase (+) o Non-lactose fermenting o SEROLOGY: Test for O1 serotype to identify presence of Tox gene. If positive, we test for the Cholera El Tor strain via a hemolysis test. Cholera el Tor properties: beta-hemolytic. Endemic to U.S. and South America. Less virulent, as it has only one copy of the Tox gene. If negative, then the Tox gene probably isn't present, although another strain is supposed to have acquired it.
30
www.brain101.info
Virulence: o Polar Flagellum: Provides motility and penetration through mucin. o Pilus: Along with an accessory colonizing protein, this is an adhesin that allows adhesion to brush border. o Mucinase: Aids invasiveness -- but not beyond the intestinal lumen. o Cholera Toxin: Exotoxin causes diarrhea. AB-Mechanism: B-Fragment binds GM1-ganglioside of enterocyte. A-Fragment enters the cell, and a disulfide bond is broken so that it cleaves into two parts. A1 Fragment transfers ADP-Ribose to the Gs-subunit, making it permanently activated ------> perpetually high cAMP, diarrhea. Cholera toxin also prevents absorption of water in the brush-border. Double-duty diarrhea. Vaccine / Prevention: Live attenuated vaccine currently provides short-term protection. Treatment: o Oral Rehydration Therapy: Glucose and water. IV replacement fluids are only used in most severe cases. o Tetracycline may be used, but can also produce resistant strains. Use with caution.
VIBRIO PARAHAEMOLYTICUS: Halophilic Gram-negative rod. Epidemiology / At Risk: o Associated with raw shellfish. o High infective dose. o People with underlying liver disease are at risk. Manifestations: o Self-limiting diarrhea + GI symptoms lasting 3 days. o Wound infections in fisherman. Processing: o Specimen: o Stain: Small gram (-) rods with single large flagellum. o Culture: Salty (3% NaCl) selective medium. No hemolysis in vitro -- only in vivo. Identification: o V. Parahaemolyticus grows in 8% NaCl whereas V. Cholera does not. o Facultative Anaerobe. Virulence: o Hemolysins: they only act in vivo. Treatment: Not usually treated.
31
www.brain101.info
URINARY TRACT INFECTIONS ESCHERICHIA COLI: UTI's Epidemiology / At Risk: o #1 organism responsible for UTI's. o Organisms originate from endogenous flora. Manifestations: UTI o Dysuria, Frequency, Urgency o Cystitis, Urethritis o Pyelonephritis Processing: o Specimen: Mid-stream clean catch Catheter Suprapubic aspiration o Stain: Gram-stain with one or more organisms per oil-immersion field is diagnostic. o Culture: Enteric Selective Medium (lactose). Identification: o Lactose-Positive o Typical E. COLI Profile: O126:B4:H15:F1,P+ All E. COLI have F1 (mannose-sensitive) pilus P+ means the Pyelonephritis antigen is present. B4 represents subtype of flagellar antigens H15 is another flagellar antigen Virulence: o P-Antigen (Pili): Mannose-resistant F2-10 antigen that is associated with pyelonephritis. o K-Antigen (Capsule): Associated with adherence to transitional epithelium. o O-Antigen: Cell-wall polysaccharide. Treatment: No treatment if asymptomatic
PROTEUS VULGARIS, MIRABILIS: Family Proteaceae, Gram-negative rods Epidemiology / At Risk: Hospital-acquired UTI, catheterized. o Found in soil, water, and decaying organic matter. o 10-15% of hospital-acquired UTI's o Wound infection Manifestations: o UTI: Bacteriuria, dysuria, frequency, urgency, pyelonephritis, prostatitis. Processing: o Specimen: o Stain: o Culture: Swarming Growth, many flagella and highly motile, forming rings of growth. Identification: o Urease(+): Key test. o Weil-Felix Test: Cross-reaction of Proteus with the Rickettsia, to test for a Rickettsial infection. No longer used. o Species: P. Vulgaris: Positive for metabolizing tryptophan ------> indole Ampicillin-resistant. Use aminoglycoside and then wait for sensitivity tests. P. Mirabilis: Negative for metabolizing tryptophan ------> indole Treated with Ampicillin Virulence: o Urease: Key virulence. Makes alkaline urine (more ammonia) ------> calculi and kidney stones. A pH>8 in urine is suspicious for Proteus. o Flagella: Peritrichous flagella enables retrograde invasion of urinary tract. o Pili: Adhesin in renal pelvis. Treatment: o P. Vulgaris: Ampicillin-resistant o P. Mirabilis: May be treated with Ampicillin.
32
www.brain101.info
PSEUDOMONAS AERUGINOSA: Family Pseudomonaceae, Gram (-) Rod. Name-Derivation: Epidemiology / At Risk: 3rd most common cause of UTI's. Manifestations: Opportunistic o UTI's o Burn Infection: Leads to bacteremia and sepsis. o Bacteremia: Immunocompromised Endocarditis o Pneumonia: Especially in Cystic Fibrosis patients. Luminal infection is leads to buildup of mucus and pus. micro-abscesses and necrosis can result. o Otitis Externa: Swimmer's ear o Eye infection: Conjunctivitis, keratitis, endophthalmitis. Processing: o Specimen: Take blood to test for bacteremia Clean-catch urine for UTI Sputum for CF patient Surface swab of burn o Stain: Direct microscopy not helpful. o Culture: Blood agar shows smooth, beta-hemolytic, blue-green (due to pyocyanin) colonies. Sputum colonies from CF patient will be mucoidy, because of the presence of Alginate which sticks to the glycocalyx of epthelial cells. Identification: o Strict Aerobe, thus they are non-fermenting of all sugars. o Oxidase (+) -- cytochrome oxidase; again, strict aerobes. o Juicy-Fruit Smell o Bug-Typing: Pyocins are used in hospitals to type-strains. These are proteins made by one strain of Pseudomonas that is lethal to another strain of Pseudomonas. This property allows for mapping of infections by different strains. Virulence: o Cell-Associated Pigments: Pyocyanin: It is an effective antibiotic against Staph Aureus, thus it overtakes Staph in CF lung infections. Pyoverdin: Helps to acquire iron. Ciliostatic. Flagella: Adhesin in the urinary tract. Pili: Adhesin to skin and upper respiratory tract. o Toxins Exotoxin A: AB-Toxin acts similar to Diphtheria toxin. Especially toxic to liver cells (as compared to Diphtheria which likes heart, nerve, kidneys). Fragment-A: Transfers ADP to Elongation-Factor 2 (EL-2) ------> inhibit protein synthesis. Exotoxin S: General AB-cytotoxin that targets a lot of cells. ADP-ribosyl transferase that interrupts protein synthesis. beta-Hemolysin: Consists of Phospholipase-C and Glycolipid, which act synergistically to lyse RBC's. o Enzymes Alkaline Protease: Ruins PMN interaction with antibodies, thus preventing opsonisation and making a vaccine difficult. Alginate: In CF patients, this sticts to the glycocalyx and is toxic to PMN's, resulting in the mucoidy colony. Elastase: Responsible for the toxic effects of the bug. Attacks elastin in vessels and lung. Damages cornea Causes pinpoint hemorrhages in skin Impairs PMN function. Vaccine / Prevention: Under develpoment, but not much progress. Treatment: Highly drug-resistant. Big problem.
33
www.brain101.info
SEXUALLY TRANSMITTED NEISSERIA GONORRHEA (GONOCOCCUS): Gram-negative reniform Diplococci Name-Derivation: Epidemiology / At Risk: o Sexual Contact o Fomite (inanimate object) may be means of transmission in prepubescent female, but it is highly unlikely. We must investigate for sexual abuse. Manifestations: o Gonorrhea Male: Painful urethritis. Purulent discharge and dysuria. Female: Vaginitis; 80% are asymptomatic. UTI symptoms Vaginal discharge Vaginitis progresses to PID, leading to sterility Common to have coinfection with Chlamydia (one predisposes to the other). Anorectal: From anal sex; rectal discharge and bleeding; usually asymptomatic. Pharyngitis: From oral sex; usually asymptomatic. o Bacteremia: Can result from failed, incomplete, or inadequate treatment. Fever, rash, skin lesions. Rash has no bugs in it. Septic Arthritis: The leading cause of arthritis in people 20-30 years of age! o Neonatal Conjunctivitis: Rapidly invasive. Destroys cornea and leads to blindness. By law, NaNO3 or Tetracycline eyedrops are given prophylactically to neonates at birth. Processing: o Specimen: Urethral exudate preferred, or swab. o Stain: Only useful on urerthral exudate. Sensitive for males but not females. Stain will show lots of variants, but they're from the same isolate. Variation reflects presence or absence of pili. o Culture: Thayer-Martin Medium is Chocolate Agar, with iron and antibiotics added to supress Gram (-)'s, Gram (+)'s, and Candida. It is usually inoculated at the bedside, because the bugs die very easily. Vancomycin gets rid of Gram (+) Colistin gets rid of other Gram (-)'s Nystatin gets rid of Candida. Then subculture to Chocolate Agar to speciate (glucose and maltose fermentation) Identification: o Neisseria: Catalase(+), Oxidase(+) is key factor. o Glucose-fermenting o Non-maltose fermenting (differ from N. Meningiditis). Virulence: o Cell-Surface: Pili Porin Protein: Protein I (PI): Complexes with PIII to form the Porin protein. Structure: Antigenically diverse: N and C termini are within membrane, and central loop sticks out which is highly antigenically diverse. High Molecular Weight: Associated with disseminated disease and increased serum resistance. Low Molecular Weight: Associated with localized (UG) disease and decreased serum resistance. Action: It triggers phagocytosis. Protein III (PIII): Complexes with PI to form the Porin protein. Binds IgG and blocks killing mediated by IgG (serum resistance). Protein II (PII): Adhesin; causes autoagglutination and adherence to epithelium. H8: Immunogenic antigen. Antibody and complement will bind to this and lyse the bug. Penicillin-Binding Protein (PBP): Peptidoglycan: Lipooligosaccharide (LOS): Not endotoxin. It damages fallopian tube mucosa and is ciliostatic.
34
www.brain101.info
Enzymes: IgA Protease: Degrades IgA antibodies; two types beta-Lactamase Intracellular survival: Catalase, Superoxide Dismutase, Peroxidase Host Immune Response: Antibodies are effective, but not protective because of antigenic diversity. Vaccine / Prevention: Tetracycline or NaNO3 eyedrops given to babies prophylactically. Treatment: Completely Penicillin-resistant, due to both beta-Lactamase and altered PBP's. o
HEMOPHILUS DUCREYI: Gram-negative Rod Epidemiology / At Risk: Manifestations: Chancroid. Looks like a Syphillus chancre, but it isn't. o Painful o Purulent Exudate o Non-indurated o Usually found on genitalia, but can be on lip. o Suppurative lymph nodes found; may develop abscess. Processing: o Specimen: Purulent exudate o Stain: Gram-negative rods. If you see bugs on the gram stain, then you have established that it is not Syphillus. o Culture: Chocolate agar, but it is very difficult to grow. Identification: o It stains on the gram-stain. Virulence: o Pili: Adhesin o beta-Lactamase Treatment: Penicillin-resistant. Use erythromycin or bactram.
TREPONEMA PALLIDUM: Spirochete Name-Derivation: Treponema - turning thread Epidemiology / At Risk: Syphillus o PRIMARY SYPHILLUS: Chancre Painless Serous Exudate Indurated (hard) Lymph nodes are slightly enlarged but not tender. o Between primary and secondary phases, there is an asymptomatic spirochetemia, during which the bugs replicate. o SECONDARY SYPHILLUS: Rash all over, including palms and soles. Rashes are also loaded with bugs and highly infectious. Not painful. Lymph nodes enlarged but not too painful. o Latency: Early Latency: Lots of antibodies and symptoms present. Headache, achiness, lethergy, tenderness of lymph nodes. Late Latency: Asymptomatic o TERTIARY SYPHILLUS: Not infectious, due to immune response. Gumma: Cell-mediated hypersensitivity with tremendous necrosis and Giant-cells. Skin: patchy loss of hair. Neurosyphillus: Tabes Dorsalis, dementia, seizures, paresis. Presence of symptoms depends on penetration of blood-brain barrier. To determine likelihood of these symptoms, look for antibodies in the CSF. Cardiovascular: Dissecting Aortic Aneurysm o Congenital Syphillus: Symptoms: Stillbirth, abortion, or structural (but not intellectual) defects if the baby is born. The fetus is protected during the first 16 weeks of pregnancy. Langerhorn cells of placenta act as barrier. Manifestations: Processing: o Specimen: Serous exudate.
35
www.brain101.info
o Stain: Dark-field microscopy shows tiny spirochetes. o Culture: Cannot be grown on agar. Koch's postulates not fulfilled. Identification: o Non-Specific Tests: Used for screening Wasserman: Old complement-fixation test looking for IgG against Cardiolipin (found in mitochondria) + lecithin + cholesterol This IgG is termed Reagin for historical reasons. Venereal Diseases Research Laboratory (VDRL): Has been superseded by RPR Rapid Plasma Reagin (RPR): Rapid card that tests for Reagin in the blood, i.e. IgG against Cardiolipin, lecithin, and cholesterol. Test is highly sensitive but not specific. If you get positive here, than go on and do one of the specific tests such as the FTA. False positives occur with SLE, aging, and other cross-reactions. o Specific Tests Treponema Pallidin Immobilization (TPI): Expensive and difficult. It is limited to people with SLE or for research. Immobilize the bug to make it visible on darkfield microscopy. Fluorescent Treponema Antibody (FTA): Antigen: A uniform strain of the bug itself grown up in rabbits. Antibody: Potentially the patient's serum, if the test is positive. Procedure: Run an indirect FA, using antihuman IgG with a fluorescein tag. FTA-Absorbed: Improved specificity from the FTA test. DEFINITIVE TEST. Eliminate (absorb and centrifuge off) cross-reacting antibodies with the Reiter Strain, which are periodontal spirochetes in the mouth. This gives the test higher specificity. A positive result with this test is an absolute positive for Syphillus. Microhemmaglutination Assay: Similar to Absorbed FTA. Less expensive, more rapid, but not as sensitive. IgM-FTA-Absorbed: Just as reliable as the IgG test if it is positive, but false negatives occur. Thus it is even more specific but not sensitive enough. o Interpretation: Virulence: Little is known because it hasn't been cultured. o Hyaluronidase: invasion Host Immune Response: o Antibody is not protective. o Cell-mediated response is essential. CMI is slow to be activated. T-Supressor cells are involved. Treatment: o Treatment is most effective in secondary phase. o Jarisch-Herxheimer Reaction: Systemic illness resulting from Penicillin treatment given to a patient that wasn't manifesting symptoms. They think it is due to the bug being lysed and killed.
36
www.brain101.info
BACTEREMIAS Only cause disease when in bloodstream NEISSERIA MENINGIDITIS (MENINGEOCOCCUS): Gram-negative diplococcus Name-Derivation: Epidemiology / At Risk: Communicable bia inhaled droplets. o #2 cause of infantile meningitis. o Transient normal flora of throat. Manifestations: o Meningeococcemia: Bugs in the bloodstream leads to a rash with lots of bugs in it. Gram negative DIC and shock are possible complications. o Meningitis: Vomiting and fever may be the only signs in infants. No treatment leads to death. Processing: o Specimen: CSF, rash exudate, blood, synovial fluid. o Stain: Mostly extracellular gram-negative cocci. Because of their thick capsule they are not phagocytosed. Lots of PMN's. o Culture: Smooth colonies. Capsule. Thayer-Martin (chocolate agar with antibiotics) Sterile specimens (CSF, blood) will can be grown on chocolate agar alone. CO2 Subculture for glucose / maltose fermentation tests. Identification: o Catalase(+), Oxidase(+): Neisseria o Glucose-fermenting, Maltose-fermenting (Meningidits) o Serotypes: Based on the capsule antigen. A,B,C,D,29E: Originally known to be virulent W135,X,Y,Z: Orginally thought to be harmless; now it's known otherwise. Type-B is the most virulent because it is not immunogenic -- we cannot make protective antibodies against it. It is made out of alpha-2,8-n-acetylneuraminic acid. It is rapidly degraded and thus not immunogenic. o Quellung Reaction: Add antiserum to look for Type-B. Swelling shows positive test. o CIE, Latex Agglutination: On CSF or urine. Two specific antibody tests to look for capsular antigens. Virulence: o Cell-Associated: Capsule: Thick polysaccahride determining the serogroup. Antiphagocytic. Type-B is not immunogenic. Outer Membrane Proteins: Another basis for serotyping. They are being used to search for a conjugate vaccine. They have homology with the Outer Membrane Proteins (I thru III) of N.Gonorrhea. LPS: Induces the Schwartzman Reaction. Causes the rash and can lead to necrosis. Pili: Adhesins in upper respiratory tract. o Enzymes: IgA Protease: Two types, cleaves bonds at hinge region of IgA1 Oxidase Needs Iron: Iron is taken up by an energy-dependent (not siderophore) mechanism. Host Immune Response: Serological o Antibody is essential to phagocytosis of this bug. o Problem: cross-reacting antigens (E.Coli, E.Fecaelis) stimulate IgA, which blocks IgM, hindering serum immunity. Not good. o Group-B can be phagocytosed but remains serum resistant. Vaccine / Prevention: Given to military recruits. Contains A, C, Y, W135. Naturally it doesn't contain B because Type-B is not immunogenic! o Vaccine can only be given to people older than two. Treatment: Prophylactic antibiotic treatment for kids younger than 6 years old, with documented contact with an index case.
37
www.brain101.info
BRUCELLOSIS: Small gram-negative rod (coccobacillus) Species B. Melitensis goat B. Abortus cattle B. Suis pig B. Canis dog Epidemiology / At Risk: Zoonotic. Cattle ranchers and people who handle cattle. Manifestations: Undulating Fever, Bang's Disease o Infecting organisms go into bloodstream and then are taken up by fixed RES macrophages, where they reside happily. o Organisms are occassionally released from fixed macrophages and go back into the bloodstream. Fever waxes and wanes according to the presence of organisms in the bloodsteam. o Symptoms: Fever, chills, sweats, myalgia, weakness, recurring at 10-day intervals. o Chronic disease causes microabscesses, granulomas, and caseation in the spleen and liver. This results from Type-IV cell mediated response to the bugs. Processing: o Specimen: Blood, bone marrow o Stain: Not useful o Culture: Brucella Agar = Selective Agar containing Erythritol, which the bugs subsist on. Erythritol is found in reproductive tract of cattle, hence these bugs cause abortion in cattle. Humans don't have erythritol so no abortion happens. Identification: o Facultative Intracellular Parasite of macrophages o Catalase (+) o Oxidase (+) o Gas-liquid chromatography can be used to identify the species.0 Virulence: o Catalase o 5'-GMP, Adenine: They inhibit the release of peroxidase by PMN's, thus hindering the halide pathway of killing. o Facultative Intracellular Parasite of macrophages o LPS: Responsible for fever. Host Immune Response: o IgM persists throughout infection. IgG waxes and wanes with fever. o IgG blocks IgM's bactericidal action in the serum. o Acute:Convalescent titer of 1:160. Vaccine / Prevention: Cattle are vaccinated in Kansas. Live attenuated B.Abortus.
LISTERIA MONOCYTOGENES: Gram (+) pleomorphic rods Name-Derivation: Monocytogenes = induces a monocytic response (in animals only). Epidemiology / At Risk: Zoonotic. Ingestion of contaminated cole slaw, raw hot dogs, chicken, cheese, milk. o At Risk: PREGNANT women, young and old, immunocompromised. Manifestations: Listeriosis. Bug has a tropism for the CNS. o Neonatal Disease: Infected at early pregnancy: Abortion or very sick baby. Infected at late pregnancy: Congential diseases. Sepsis, fetal distress, seizures. Delayed-onset meningitis and meningeoencephalitis. o Adult Disease: Bacteremia. Meningitis, endocarditis. o Pregnant Woman: Mild-flu like illness, usually associated with ice cream. o Sequelae: Strictly immunologic -- aseptic meningitis and rash. Processing: o Specimen: CSF, blood, amniotic fluid. o Stain: Rods, both inside and outside cells, tends to filamentous. o Culture: Blood agar. Small colonies with narrow zone of beta-hemolysis. Can grow in cold (4C), therefore it's perfectly happy when refrigerated. Identification: o Catalase (+) o beta-Hemolysis o Facultative Intracellular Parasite of macrophages
38
www.brain101.info
Virulence: o Listerolysin O: Oxygen labile, beta-Hemolytic, like Streptolysin-O Cytotoxic to RBC's, WBC's, PMN's (at low pH intracellularly), and myocardium Disrupts phagolysosome. o Catalase o Facultative Intracellular Parasite of macrophages: actin polymerizes to allow the bugs to travel from cell to cell, like Shigella. o Cell Wall Lipid: Induces granulocytic response in humans. Induces an IgM response. In humans, hemolytic due to cross-reaction with blood-group antigen. It's not gram-negative, but this leads to a hemolytic crisis. Host Immune Response: o Monocytic response in animals. Granulocytic with left-shift (standard) response in humans. o Cross-reaction with Staph and Strep leads to high diagnostic titer of 1:200. o Protective Cell-mediated immunity is induced.
39
www.brain101.info
SPIROCHETEMIAS LEPTOSPIRA INTERROGANS: Spirochete Epidemiology / At Risk: Zoonotic. o Chronic animal carriers disseminate bugs in the urine. o Infection through breaks in skin or mucosa, or by ingestion. Manifestations: Leptospirosis o Bacteremia: bugs circulate and produce disfunction in: Liver: Jaundice, hemorrhage Kidneys: Uremia CNS: Aseptic meningitis (from immune complexes in CSF) o Organisms replicate in endothelial cells in the CSF. o Symptoms: fever, chills, myalgia, headache, vomiting. Last about a week than rash follows. Processing: o Specimen: Blood especially in the first 7 days (during Spirochetemia) Urine after first 7 days CSF o Stain: Dark Microscopy: long, thin spirochetes. Two axial filaments per pole, with a hook or loop at end. o Culture: Takes 1-2 weeks. Identification: o beta-Hemolytic o 19 serogrops. 140 variations. A lot of cross-reactivity. IgM titer therefore must be greater than 1:100. o Serology: Screening (not specific due to cross-reactivity): Check for agglutination between formalin-killed bugs and patient serum. Specific: Use live organisms and check for agglutination. Virulence: o Cell-wall Lipids: ~25% of dry weight of cell. Accounts for endotoxin-like fever, chilld, headache. o Hemolysin: Heat-labile. Anti-phagocytic and responsible for beta-hemolysis. o Surface-Antigens: Induce host antibody and complement. Host Immune Response: o IgM appears after 1 week and lasts for months. o IgG appears after 1 month and lasts for years. Vaccine / Prevention: o Dog: Prevents chronic kidney infection and shedding of organisms in urine. o Sewer-Workers: At-risk population for the serovariety-specific vaccine for humans.
BORRELIA RECURRENTIS: Large spirochete, visible on light microscope Name-Derivation: Recurrentis = relapsing-fever Epidemiology / At Risk: Rodents and small animals are reservoires. o Head-Lice (Louse): Common vector. Prevention = get rid of head lice. Transmitted by crushing lice when we scratch. o Tick: Another vector that carries B.Hermsii, similar to this bug. Bacterium is introduced upon biting by the tick. Manifestations: Relapsing Fever. Bugs go straight to the blood. o Incubation time: 1 week o Spirochetemia: Fever, chilld, headache, myalgia Possible hepatosplenomegaly Flu-like symptoms o Fever returns 1 to 2 weeks later, and cycle repeats 2 to 3 times. Processing: o Specimen: Blood o Stain: Giemsa or Wright stain is most effective.
40
www.brain101.info
However it stains Gram-negative and is visible under light microscope Darkfield: Shows cokscrew motility and 15-20 axial filaments per pole. o Culture: It can be cultured, but it is difficult. 7 - 14 days. Identification: Culture o Microaerophilic Virulence: o Antigenic Shift in vivo is responsible for the Relapsing Fever. Continuous antigenic shift of outer membrane proteins. Host Immune Response: Antibody + Complement is protective. Vaccine / Prevention: Prevention of lice in schools. Treatment: Broad-spectrum
BORRELIA BURGDORFERI: Spirochete Name-Derivation: Lyme = town in CT; Burgdorf = Researcher Epidemiology / At Risk: Zoonotic o Vector = Deer Tick bin nymph (agressive) stage. o Host = Deer o Prevelant in Summer, outdoors. Manifestations: Lyme Disease. Incubation of 3-30 days. o Early: Skin lesions; erythema chronicun migrans. Rash, necrotic in center, and grows. Then it clears. Most common manifestations. o Later: Appear to be immunological sequelae. Neurological: Next most common manifestations in U.S. Headache, encephalitis, Bell's Palsy. Cardiac: Common manifestations in Europe. AV-block, myocarditis Rheumatoid: Non-erosive migratory arthritis (non-supparative) o Systemic spirochetemia symptoms can also be found: malaise, fatigue, fever, etc. Processing: o Specimen: Blood o Stain: Giemsa or Wright stain. Darkfield: Motility Slower than B. Recurrentis 7-11 flagella at each pole -- not axial filaments. o Culture: Enriched Selected Kelly's Medium. Enriched with fatty acids, but it's still difficult to grow. 7 days Identification: o Microaerophilic Virulence: o Outer Membrane Proteins A & B: Polyclonal mitogenic antigens of B-Cells. Antigenic shift seen in vivo. Polyclonal B-Cell activation is probably responsible for the immunological sequelae. Host Immune Response: o Lots of antibodies o Very few PMN's, because the bugs are so long that you cannot suck them up. o Bugs are presumably killed by antibody + complement. Treatment: Penicillin
41
www.brain101.info
ANAEROBES BACTEROIDES FRAGILES: Gram-Negative Pleomorphic Rod Name-Derivation: Epidemiology / At Risk: #1 bacteria of normal GI flora. 1010-1011 bacteria / gram o Can survive on skin and mucosa. o At Risk: Immunocompromised Manifestations: Bugs enter through a compromise in GI-tract. Initial infection is polymicrobic, but as other bugs use up the oxygen, Bacteroides can grow. o Pelvic Inflammatory Disease o Intra-abdominal abscess; peritonitis o Sustained Bacteremia: Not endotoxic, and not transient, but in between. Processing: o Specimen: Exudate. Will be polymicrobic early on. Must use anaerobic transport medium. o Stain: Gram-negative rods contain intracytoplasmic vacuoles. o Culture: Blood agar with antibiotics. Identification: o Strict (Aerotolerant) Anaerobe o Direct-FA on capsule to verify its presence. It is not readily visible in culture. o Gas-Liquid Chromatography of metabolic byproducts. Anaerobes are difficult to culture. Virulence: o Isobutyric and Succinic Acid: Biochemical byproducts are toxic to Salmonella and Shigella. Thus our normal flora are protective against Salmonella. o Capsule: Allows adhesin to peritoneum. Antichemotactic and antiphagocytic for PMN's. Aids to inhibit intracellular killing once the bugs are phagocytosed. o Superoxide Dismutase: makes it aerotolerant o Catalase: induced by hemin, thus produced in the blood. o Enzymes: Hyaluronidase, DNAse, Heparinase contribute to invasiveness. o LPS: Contains Lipid-A, but it is not as toxic as E. Coli endotoxin. Only mild endotoxic effect. o Enterotoxin: Diarrhea. This toxin only carried by a few strains. o beta-Lactamase Treatment: Abscesses must be surgically drained. Metronidazole.
CLOSTRIDIUM PERFRINGES: Gram-Positive rod, spore-former Epidemiology / At Risk: Normal flora; found as spores in the GI-tract. Manifestations: o Food-Poisoning: TYPE-A. Found in meats, gravy. 8-24 hours after meal. Water diarrhea, no perforation, resolves spontaneously. No Vomiting. No fever. Heating doesn't prevent it. It only drives out the oxygen. o Necrotizing Enteritis: TYPE-C. More prevelant in other countries. Necrotizing invasion of small intestine, leading to necrosis, perforation, and death. o Gas Gangrene (Myonecrosis): TYPE-A. Spreading of initial tissue damage. Predisposing Factor: Must have trauma with damage to muscle, and reduced bloodflow. Reduced pH (6.5 or lower) causes autolysis of muscle proteins and release of amino acids ------> spores use them as energy resource and germinate. Fatal without treatment. o Cellulitis: TYPE-A. Subcutaneous damage without muscle damage. Infection spreads along fascial planes. Processing: o Specimen: Exudate, blood, feces. o Stain: Plump Gram(+) rods with square ends and a capsule. No inflammatory cells. o Culture: Egg-Yolk Agar. Lecithin is present to test for Lecithinase activity.
42
www.brain101.info
Double-zone of hemolysis: beta-hemolysis on inside, plus hazy zone of partial hemolysis on outside. Identification: o Strict (Aerotolerant) Anaerobe o SEROTYPING: Based on ability to produce four different exotoxins: alpha, beta, , There are types A-E Type-A is most prevelant in U.S. o Gas-Liquid Chromatography for speciation. Virulence: o Very fast (10 minute) generation time. o Exotoxins: At least 12 are produced. Some main ones Alpha Toxin: Lecithinase. Hydrolyzes lecithin and sphingomyelin, to lyse mitochondria, RBC's, and WBC's. Responsible for the larger zone of incomplete hemolysis. It's an exotoxin so it can go awayfrom the cell. Beta Toxin: Cytotoxin, responsible for necrotizing enteritis. Theta Toxin: Oxygen-labile hemolysin. Responsible for smaller zone of beta-hemolysis. Toxic to heart muscle, leading to myocarditis as a cardiac complication (from toxemia) o Invasiveness: Due to extracellular enzymes; proteases, collegenases, DNAses. o Enterotoxin: Only released upon sporulation and lysis of a vegetative cell. Thus it is not a true exotoxin (only released upon lysis) Causes watery diarrhea, no dysentery. Vaccine / Prevention: Clean and debride wounds for prevention. Treatment: Antibiotics, intermittent hyperbaric oxygen treatment.
CLOSTRIDIUM TETANI: Gram-positive spore-forming rod. Epidemiology / At Risk: Spores are uniquitous in the soil and introduced through puncture wounds. Manifestations: Tetanus. A microgram of toxin is sufficient to kill. o Spore Germination: Once spores introduced, they can lie dormant for years if wound remains well aerated. As aeration is reduced (such as with age, for example), spores germinate and release exotoxin. Exotoxin is taken up by nerve cells ------> retrograde transport to post-synaptic dendrites, where the exotoxin exerts its effect. o Generalized Tetanus: Lockjaw. Toxin may ascend to brain and affect respiratory center. ANS involvement and generalized spasms. Death by respiratory arrest. Symptoms: Dysphagia Drooling ANS involvement: sweating, hyperthermia, cardiac arrhythmias. o Localized Tetanus: Localized spasm in area of infection. It may spread to generalized tetanus. o Cephalic Tetanus: Primary infection in head. Processing: o Specimen: Only a few organisms in the lesions. Diagnosis is clinical -- not by microbiology. o Culture: Swarming Growth in culture. Thin surrounding film and faint beta-hemolysis. Amplified in cooked hamburger broth. Selected for by heat. Identification: o Opportunstic Strict Anaerobe o Genus is identified by colony morphology. o Somatic Antigen O: Fortunately there is only one serotype of Antigen-O, so that a vaccine is easy to make and effective. Virulence: o Tetanospasmin: Heat labile, potent, antigenic exotoxin. AB-Toxin cleaved in light (A) and heavy (B) fragments by an endogenous protease. Fragment-B binds to ganglioside receptor of a nerve cell. Fragment-A is taken up by endocytosis. Acidifcation of the vesicle causes Fragment-A to be release into cytoplasm. Effect: Fragment-A moves up axon retrograde to the post-synpatic receptor. It blocks release of GABA and Glycerine at the post-synaptic terminal. This results in unregulated excitatory post-synaptic potentials on nerve terminal, leading to spastic paralysis of skeletal muscle and respiratory arrest.
43
www.brain101.info
Vaccine / Prevention: o VACCINE: Given against the O-Antigen in cell wall. Alum-precipitated toxoid (more immunogenic but can cause hypersensitivity): given to infants and children, and never-before immunized adults. Children given at age 2, 4, 6, and 15-18 months. Ammonium-precipiated toxoid: Given as a booster shot every ten years thereafter. People are usually over-vaccinated for this bug. o ANTITOXIN: Given prophylactically if someone is potentially exposed (has a puncture wound) and has not been vaccinated within 5 years. Tetanus toxin itself is not inherently immunogenic. If a documented vaccine has been administered in last 5 years, no antitoxin is necessary. Treatment: To someone who has never been vaccinated, the antitoxin is given in one arm, and a vaccine is given in the other arm, simultaneously. The two will not intermix if given in separate arms.
CLOSTRIDIUM BOTULINUM: Gram-positive spore forming rod. Epidemiology / At Risk: Spores are in soils and sediment. Found in foods preserved at home at room temperature; old canned foods or self-canned foods. Manifestations: o Food-Born Botulism: Usually found in alkaline foods, consumed without heating. Initial Symptoms: Weakness, diziness, constipation. Toxin is then absorbed from small intestine into blood and nerve cells. Terminal Symptoms: Blurred vision, dry mouth, peripheral and respiratory flaccid paralysis. Death. o Infant Botulism: Infant at risk up to 1 year of age. After 1 year, GI ingestion of spores is not a problem. Cause: Ingestion of spores, usually in unpasteurized honey. Organisms replicate in GI tract and release toxin. Toxin is not readily absorbed through mucosa, but it can be absorbed if the problem is neglected. Presents as failure to thrive, but can progress to flaccid paralysis. o Wound Botulism: Rare, similar clinical presentation as food botulism. Processing: o Specimen: Blood, gastric contents, or food. Feces for children. Serology: Do an assay for the toxin in the blood. o Stain: On infant feces, will find gram-positive rods. o Culture: Blood agar. Heat to boiling for 10 minutes to induce sporulation. Smooth colonies, beta-hemolysis. Identification: o ELISA can be used on culture for detection of toxin. o Oppotunstic Strict Anaerobe o Serotypes: 8 serologic types of toxin: A, B, C1, C2, D, E, F, G. All of them act the same. Only types A, B, E affect humans. Virulence: o Botulin Exotoxin: The most potent toxin known to man, i.e. lowest amount required to kill. Phage-mediated, heat labile toxin. Antigenic. The toxin is released upon cell lysis. MECHANISM: AB-Toxin. Fragment-A is translocated up neuron and blocks release of Acetylcholine -----> Flaccid Paralysis. Enzyme resistance: Acid stable. Our bodies actually break down the toxin into fragments that are more toxic. Host Immune Response: No persistent antibody to the toxin, therefore no lifelong immunity. o Again, the toxin is not inherently immunogenic. Vaccine / Prevention: Alum-precipitated toxoid, only for lab workers. o PREVENTION: Head food, don't give unpasteurized honey to babies. o Antitoxin is available for types A, B, and E. Treatment: o Ventilatory Support o Administer antitoxin. o Gastric Lavage to wash out any unabsorbed toxin.
44
www.brain101.info
INTRACELLULAR VIRUS-LIKE THINGIES RICKETTSIA RICKETTSIAE: Poorly staining gram-negative pleomorphic rods. Family Properties: RICKETTSIACEAE o Strict Intracellular Parasites o Requirwe NAD and ATP for growth o OTHER SPECIES: Ehrlichia: Arthropod-vectored infection of WBC's. No rash. Coxiella: Q-Fever. Usually carried by farm animals. RES involvement -- hepatosplenomegaly. Maybe no pneumonia. No rash. Epidemiology / At Risk: Found in the Eastern U.S., spread by ticks, in the Summer. Manifestations: Rocky Mountain Spotted Fever is the best known example. o General Properties: Arthropods are vectors. They infect endothelial cells, starting with small capillaries and working their way up, leading to thrombosis and hemorrhage. There is a prominent rash and fever. o Time Course: 4-7 days: Extensive rash, extending from extremities to trunk. Rash resembles Syphillus. 2 weeks: Very sick. High fever, DIC, hypotension, gram-negative shock. Cardiac failure, renal failure, and encephalitis are likely causes of death. o OTHER RICKETTSIAL INFECTIONS: Typhus: Several species and several vectors. Rash spreads from trunk to extremities, rather than RSMF which is the opposite. Rickettsial Pox: From mites. Benign, self-limited rash. Processing: o Specimen: Rash biopsy for RMSF. o Culture: Egg or tissue culture. Identification: o Direct FA on endothelial cells o Serology: Indirect FA to measure antibody levels. Antibody titer of 1:64, or Acute:Convelescent titer of 4X Virulence: o Outer Membrane Proteins o Phospholipase: Acts as an invasin, helping bugs get into endothelial cells. o LPS: Strong endotoxic component. o Actin Polymerization: Making little projection to infect other cells. Some sort of way for the bugs to spread from cell to cell, similar to Shigella. Host Immune Response: Probably combination of antibody plus cell-mediated. Not sure. Vaccine / Prevention: Protective clothing. Treatment: Tetracycline.
CHLAMYDIA TRACHOMATIS: Gram-negative rods. Family Properties: CHLAMYDIACEAE o Obligate intracellular parasite o Tropic for columnar epithelia. o Gram-negative, but no peptidoglycan layer. o Dependent on ATP from host. o LIFE-CYCLE: Elementary Body: Individual bugs living outside the host. They infect the host by endocytosis. They then multiply inside the host, utilizing host ATP. Reticular Body: Cluster of bugs forming an inclusion body inside the cytoplasm of the host cell. They are released from the host-cell, to form more elementary bodies, which then go on to infect other cells. Epidemiology / At Risk: o Leading cause of preventable blindness.
45
www.brain101.info
o Leading cause of PID. Manifestations: o Chronic Keratoconjunctivitis: Types A, B, C Progressive conjunctivitis causes blindness by age 15 or 20. o Chlamydial Urethritis: Types D-K So-called "Non-gonococcal urethritis." PID o Inclusion Conjunctivitis (TRIC): Types D-K. Problem in newborns. Not the same as blindness above. By law, (along with Gonococcus), newborns are treated prophylactically with eyedrops. o Lymphogranuloma Venereum: Types L1-L3. Sexually transmitted, but the primary manifestation is suppurative (and later granulomatous) inflammation of inguinal lymph nodes. Processing: o Specimen: Scrapings are taken for the inclusion conjunctivitis, UG, or rectal. Look for bugs in epithelial cells. o Stain: Giemsa stain. Iodine stain, looking for brown inclusion bodies. o Culture: Identification: o Serotypes A-C: Keratoconjunctivitris, found in Asia and Africa D-K: Most prevelant in U.S. Urethritis and inclusion conjunctivitis. L1-L3: Lymphogranuloma Venereum. Asia and Africa. o Iodine-Positive: Inclusion bodies contain a lot og glycogen and thus stain brown with iodine. Virulence: Mostly focused on the Reticular Body. o ATPase: Helps the bug utilize the host cell's ATP. o ATP-ADP Translocase: In conjunction with the ATPase, this allows the bug to utilize the host cell ATP (high energy phosphate bonds) as a source of energy. o Cylindrical Projections: Little projections that probably help the bugs utilize host-cell nutrients. o LPS: Antigenic, providing a group-antigen for this bug. o Outer Membrane Proteins: Antigenic source for most of the serotyping (Types A-K, L1-L3). Treatment: Tetracycline.
CHLAMYDIA PNEUMONIA: Gram-negative rods. Manifestations: Walking Pneumonia, aka TWAR. o Infection of columnar epithelium of upper respiratory tract. Identification: No processing usually needed. Disease can be treated based on clinical manifestation alone. Treatment: Tetracycline.
CHLAMYDIA PSITTACI: Gram-negative rods. Epidemiology / At Risk: Respiratory droplets inhaled. Found in pet birds (parrots, parakeets), poultry birds. People talking to their birds up close, etc. Manifestations: Psitaccosis. An interstitial pneumonia. o Headache (can be severe), and dry, non-productive, hacking cough. o Sequelae: severe headache, encephalopathy, possible convulsions, coma, and death. Processing: o Specimen: Lung biopsy. Can take sputum late in disease. Blood. o Stain: o Culture: Identification: o Iodine-negative: Does not stain brown with iodine, as the inclusion bodies do not contain glycogen. o Serology: Indirect FA. Test for patient antibodies to the bugs, by using labelled anti-antibodies. o Acute-Convalescent titer of 4X Treatment: Tetracycline.
MYCOPLASMA PNEUMONIA: No gram-stain. Family Properties: MYCOPLASMACEAE o No Cell Wall: Only a triple-layer plasma membrane. Thus they are flexible, pliable, filterable.
46
www.brain101.info
Absolute Growth Requirements: Cholesterol or other sterol for synthesis of plasma membrane. Purines and pyrimidines. Epidemiology / At Risk: o Ubiquitous. Normal flora of respiratory, GI, UG tract. o Infected spreads the organism for up to 14 weeks. Person-to-person spread of pneumonia occurs, and it tends to be found with close-living quarters, such as dorms, families, etc. Manifestations: o Walking Pneumonia Monocytic respose, lots of lymphocytes, which is normally found in a viral infection. Infects ciliated cells in the bronchial region and multiples intracellularly. Thus it is ciliostatic, and it can make the cells lose their cilia altogether. Other bug that infects same cells is B.Pertussis. Non-productive or minimally productive cough. WBC-count is not markedly high, maybe slightly high. o Otitis Media in adults. We can find bullous myringitis (inflammation of tympanic membrane). Processing: o Specimen: Swab, sputum or ear aspirate. o Stain: o Culture: Biphasic Enriched Agar/Broth Medium. Agar with broth on top. 10 days. They divide very slowly. Small fried-egg-like colony can be seen under scanning microscope after two weeks. Absolute Growth Requirements: Cholesterol or other sterol for synthesis of plasma membrane. Purines and pyrimidines. Identification: o Guinea-Pig RBC's: Add guinea-pig RBC's to the agar once the bugs have grown, and they should adhere to these cells (hemagglutination), making them easy to identify. In agar, hemolysis also occurs. o Cold-Agglutination Antibody Titration Not sensitive, but still clinically useful. PROCEDURE: An IgM antibody produced by the host cross-reacts with the I-antigen (type-O) bloodgroup antigen. Take the two and mix them together. ANTIBODY: If found, it is the IgM antibody. ANTIGEN: We use the type-O group-antigen. If antibodies are present, hemagglutination will occur at 4C indicates a positive test. If the agglutination then dissolves when it is heated back up, then we have a positive test. Test has theraputic applications: keep patient warm in order to prevent in-vivo hemagglut-ination with the bug. o Complement-Fixation Test: Specific test. Only useful if the test is positive. If antibody is present, then the lipid component of the bug's membrane will fix complement in the patient's serum. o Diagnostic antibody titer is 1:100, slightly high because it is an ubiquitous organism. Virulence: o P1 Protein: Adhesin attaches to receptors on respiratory, GI, and UG tracts. It also gives the bug a characteristic gliding motility. Host Immune Response: Monocytic. Treatment: Tetracycline. o
MYCOPLASMA HOMINIS: Emerging bug, associated with post-abortal and post-partum fevers, and PID. UREAPLASMA UREALYTICA: Tiny bug. Epidemiology / At Risk: Ubiquitous. Manifestations: Urethritis which can be asymptomatic. Another causative agent of non-gonococcal urethritis. Processing: o Culture: Very small colonies grow very slowly. Identification: Add a pH indicator to medium to verify basic pH, which results from the presence of potent Urease. Virulence: Urease helps bug survive in UG tract. Degrades urea and produces ammonia, yielding higher pH. Treatment: Tetracycline.
47
www.brain101.info
You might also like
- Gram Positive Cocci Sem 1 1Document45 pagesGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- Aerobic Gram PositiveDocument14 pagesAerobic Gram PositiveMickey mg100% (1)
- MycologyDocument26 pagesMycologySkandi43No ratings yet
- ISBB Immunology ReviewDocument9 pagesISBB Immunology ReviewNathan DrakeNo ratings yet
- Myco-Viro Questions GuideDocument14 pagesMyco-Viro Questions GuideDhanimie FayeNo ratings yet
- Acid Fast StainingDocument4 pagesAcid Fast Stainingchaudhary TahiraliNo ratings yet
- Test Bank Exam 3Document81 pagesTest Bank Exam 3Sajjad AhmadNo ratings yet
- Medical Laws and Regulations SummaryDocument16 pagesMedical Laws and Regulations SummaryNeririNo ratings yet
- HistotechniquesDocument9 pagesHistotechniquesDivineGloryMalbuyoNo ratings yet
- Introduction to Mycology: An Overview of Fungal Morphology and ReproductionDocument26 pagesIntroduction to Mycology: An Overview of Fungal Morphology and ReproductionOsannah Irish InsongNo ratings yet
- 3 SEMR421 Bacteriology Part 3Document14 pages3 SEMR421 Bacteriology Part 3Micah Daniel TapiaNo ratings yet
- Summary of Key Microbiology TestsDocument45 pagesSummary of Key Microbiology TestsAtiya HajjajNo ratings yet
- Enterobius Vermicularis: Ciulla Chapter 8 - ParasitologyDocument13 pagesEnterobius Vermicularis: Ciulla Chapter 8 - ParasitologySalve Rachelle BillenaNo ratings yet
- A. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaDocument7 pagesA. Neisseria Gonorrhoeae B. Moraxella Catarrhalis C. Neisseria Meningitidis D. Neisseria LactamicaWynlor AbarcaNo ratings yet
- Clinical Microscopy ExamDocument3 pagesClinical Microscopy ExamKarla GiorlaNo ratings yet
- Anaerobic BacteriaDocument2 pagesAnaerobic BacteriaAbhugz MarceloNo ratings yet
- Microbiology Revision E6.5Document132 pagesMicrobiology Revision E6.5massprithiv58No ratings yet
- Medical Mycology Study Questions PDFDocument4 pagesMedical Mycology Study Questions PDFPauline JoramNo ratings yet
- Intestinal Nematodes Maricelle ManlutacDocument64 pagesIntestinal Nematodes Maricelle ManlutacGlanela ManalotoNo ratings yet
- Microbiology ReviewDocument22 pagesMicrobiology ReviewCassie Von Peenq100% (1)
- Immunology Serology ReviewDocument211 pagesImmunology Serology ReviewRachel Marie M. Gania100% (1)
- Biochemical TestDocument13 pagesBiochemical TestSusi100% (1)
- Biochemical Identification of BacteriaDocument72 pagesBiochemical Identification of BacteriaMaria Jhoyce MagpantayNo ratings yet
- HashbrownDocument22 pagesHashbrownLeomill MendiolaNo ratings yet
- Gram-Negative Rods in Gut FloraDocument2 pagesGram-Negative Rods in Gut FloraJohn TerryNo ratings yet
- 20 MycobacteriaDocument47 pages20 MycobacteriaStephen Jao Ayala UjanoNo ratings yet
- Medical TechnologyDocument13 pagesMedical Technologyangelina buenaNo ratings yet
- Bacteriology LectureDocument38 pagesBacteriology LectureAisle Malibiran Paler100% (1)
- Intro To Mycology Prelims2Document47 pagesIntro To Mycology Prelims2Annika AbadNo ratings yet
- Antigen and Its PropertiesDocument20 pagesAntigen and Its Propertiestusharpremin92% (12)
- 2.medical HelminthologyDocument148 pages2.medical HelminthologyHanifatur Rohmah100% (2)
- Summary of Diagnostic BacteriologyDocument45 pagesSummary of Diagnostic Bacteriologyomaromran100% (3)
- Bacteriology HandoutsDocument30 pagesBacteriology HandoutsMarco Tolentino100% (8)
- Microbiology MnemonicsDocument5 pagesMicrobiology MnemonicsFritzel SusbillaNo ratings yet
- Progress Exam - MicrobiologyDocument75 pagesProgress Exam - MicrobiologyAngelicaNo ratings yet
- Studying Fungi Methods Lab DiagnosisDocument74 pagesStudying Fungi Methods Lab DiagnosisKaycee Gretz LorescaNo ratings yet
- Acts Reinforcement Mar2020 PDFDocument8 pagesActs Reinforcement Mar2020 PDFErika Kate MedadoNo ratings yet
- Mtap - Immunohema Transfusion MedicineDocument9 pagesMtap - Immunohema Transfusion MedicineMoira Pauline LibroraniaNo ratings yet
- Immune Responses: Introduction to Innate and Adaptive ImmunityDocument10 pagesImmune Responses: Introduction to Innate and Adaptive ImmunityArvi MandaweNo ratings yet
- SerologyDocument84 pagesSerologyngsusannasuisum100% (2)
- Bacterial Identification Methods SummaryDocument12 pagesBacterial Identification Methods SummaryLarnie Alejandre100% (1)
- HISTOPATHOLOGYDocument3 pagesHISTOPATHOLOGYYza RysNo ratings yet
- IMMUNOLOGY SEROLOGY OVERVIEWDocument45 pagesIMMUNOLOGY SEROLOGY OVERVIEWJacqueline RoijardNo ratings yet
- MICROBIOLOGY BOARD EXAM QUESTIONSDocument6 pagesMICROBIOLOGY BOARD EXAM QUESTIONSchristinejoan100% (1)
- Microbiology PDFDocument71 pagesMicrobiology PDFDanny Alexander TullumeNo ratings yet
- Bacte Day 2Document24 pagesBacte Day 2Jadey InfanteNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- AUB - Intro To UrinalysisDocument3 pagesAUB - Intro To UrinalysisJeanne RodiñoNo ratings yet
- Student Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentDocument5 pagesStudent Notes: Clinchem1: Davao Doctors College Medical Laboratory Science DepartmentMelody PardilloNo ratings yet
- Microbio Lec 1 - Bacterial Morphology and Ultra StructureDocument8 pagesMicrobio Lec 1 - Bacterial Morphology and Ultra Structureapi-3743217100% (3)
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- Bacteriology Final Coaching Notes 2Document9 pagesBacteriology Final Coaching Notes 2Mylene TamoriteNo ratings yet
- Microbiology Exam - Parasitology Flashcards - QuizletDocument17 pagesMicrobiology Exam - Parasitology Flashcards - QuizletIdrissa ContehNo ratings yet
- Intestinal FlagellatesDocument6 pagesIntestinal FlagellatesRitz Celso100% (2)
- Sterilization and DisinfectionDocument10 pagesSterilization and DisinfectiondrugdrugNo ratings yet
- My CologyDocument25 pagesMy CologyPlasma CarwashNo ratings yet
- Agglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4From EverandAgglutination, Complement, Neutralization, and Inhibition: Methods in Immunology and Immunochemistry, Vol. 4No ratings yet
- Senior Medical Laboratory Technician: Passbooks Study GuideFrom EverandSenior Medical Laboratory Technician: Passbooks Study GuideNo ratings yet
- TBDocument2 pagesTBDeti ParidlahNo ratings yet
- Muscles of Inspiration Muscles of Expiration: Principal Accessory Quiet Breathing Active BreathingDocument2 pagesMuscles of Inspiration Muscles of Expiration: Principal Accessory Quiet Breathing Active BreathingDeti ParidlahNo ratings yet
- Bone Scan PPDocument49 pagesBone Scan PPDeti ParidlahNo ratings yet
- Monro-Kellie Doctrine Volume RelationsDocument1 pageMonro-Kellie Doctrine Volume RelationsDeti ParidlahNo ratings yet