Professional Documents
Culture Documents
Imaging in Brain Meningioma
Uploaded by
Bramanda Sml TobingOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Imaging in Brain Meningioma
Uploaded by
Bramanda Sml TobingCopyright:
Available Formats
Imaging in Brain Meningioma
Author: German C Castillo, MD, FACR. FICS; Chief Editor: James G Smirniotopoulos, MD
Radiography
In most patients, no findings of meningiomas are present on plain radiographic examination. Plain skull images may demonstrate calcification in meningiomas of the skull base or convexity. Meningiomas displayed reactive hyperostosis without connection to the size of the tumor. Rare osteolysis is associated with the benign and aggressive meningiomas.
Degree of confidence
Most plain skull radiographs do not depict signs of meningiomas. Meningiomas en plaque have diffuse hyperostosis, more frequently observed over the sphenoid wing and pterion. This finding results in a high degree of confidence.
False positives/negatives
Calcification within the tumor is a considerably less frequent plain radiographic manifestation; therefore, false-negative results occur. Most patients with brain meningiomas do not undergo radiographic imaging because the diagnosis has been made directly with CT scanning or MRI.
Computed Tomography
CT scanning has several advantages in the imaging of meningiomas.[15, 16, 17, 18, 19, 20, 21, 22] Invasion of surrounding dura frequently provokes an osteoblastic response, causing hyperostosis.[23] This imaging modality is used best for demonstrating calcification of meningiomas (see the images below). The CT nature of the calcification may be nodular, fine and punctate, or dense.
Brain meningioma. Nonenhanced computed tomography scan demonstrates a middle fossa meningioma. The calcified mass is attached to the anterior ridge of the
right petrous bone. Ring and punctate calcification are depicted. Edema is not appreciated.
Two different cases. A, B: Computed tomography (CT) scans depict calcified meningiomas from the parietal convexity. C: Nonenhanced axial CT image shows homogeneous calcified mass attached to the right parietal bone. Soft-tissue tumor is seen at the posterior aspect of the calcification (large arrow). Other minor calcifications on the left cerebral hemisphere are caused by a parasitic disease. D: Coronal T2-weighted magnetic resonance image demonstrates calcium deposit (star) surrounded by solid tissue (small arrow); edema is not seen in this case.
CT scanning is effective in showing hyperostosis, bone destruction, and erosion at the site of the dural attachment (see the following images). Hyperostosis is seen in 15-20% of patients.
Brain meningioma. Nonenhanced computed tomography scan shows a malignant meningioma in the frontal convexity that appears as a spontaneously hyperattenuating mass. The cystic cavity may be tumor necrosis, old hemorrhage, cystic degeneration, or trapped cerebrospinal
fluid. Edema and midline shift to the left anterior aspect is observed.
Brain
meningioma. Nonenhanced computed tomography scan shows a malignant meningioma in the frontal convexity. The hyperattenuating and inhomogeneous enhancing mass and a ring-shaped enhancement
is shown. Brain meningioma. Malignant frontal-convexity meningioma. Computed tomography scan of the frontal internal table and diploe shows erosion and bone infiltration.
CT scanning can also show acute tumor hemorrhage and widened vascular grooves in the calvarium. In addition, homogeneous masses with attenuation similar to the surrounding brain make up 25-33% of meningiomas. The remainder are hyperattenuating compared with the brain. Meningiomas can exhibit extensive edema. Inhomogeneous enhancement can result due necrosis or rare hemorrhage. Edema is absent in 50% of patients because of slow growth, but it may be extensive. Edema predominantly affects white matter, and it resembles fingers of low attenuation units. See the images below.
Brain meningioma. Nonenhanced computed tomography scan shows an isoattenuating sphenoid-wing meningioma. The left sylvian fissure is partially collapsed.
Brain meningioma. Computed tomography scan shows an isoattenuating
sphenoid-wing meningioma. The contrast-enhancing mass is attached to the major sphenoid wing and was demonstrated only after the intravenous injection of contrast material.
Contrast-enhanced CT scanning displays moderate to strong homogeneous enhancement in most tumors. Steinhoff et al observed a nodular blush in 97%, a mixed inhomogeneous blush in 0.5%, and a ring blush in 1.5%.[24] In a study by Naidich et al, tumor blush was nodular and nearly homogeneous in 70% of patients, inhomogeneous in 24% of patients, and ringlike in 2% of patients.[25] Cystic components of the meningiomas may be present inside the tumor or between the tumor and the adjacent brain, so-called trapped CSF. Peripheral cysts resulting from trapped CSF can also be present. See the image below.
Brain meningioma. Posterior tentorial meningioma on a coronal contrastenhanced computed tomography scan. A hyperattenuating and well-marginated mass is adjacent to the tentorium. Pooling of cerebrospinal fluid, subtle edema, homogeneous enhancement, and ventricular dilatation are demonstrated. Degree of confidence
Meningiomas are well-circumscribed peripheral or falcine masses that deform the brain. About 90% of meningiomas are demonstrated on CT scans. The main role of CT scanning, as opposed to other imaging modalities, is the demonstration of adjacent bone changes and calcification within the lesion. Atypical CT scan features are the primary reason for preoperative misdiagnosis. Posterior fossa meningiomas may be missed by this imaging modality, as will be some en plaque lesions. CT scanning can fail to demonstrate cystic changes in intracranial meningiomas. CT scan features, such as irregular areas of nonenhancing mass and well-defined regions of persistent low attenuation, are the reason for preoperative misdiagnosis.
False positives/negatives
False-negative findings can occur with cystic changes in brain meningiomas; false-positive findings can occur with large dural calcification, which can mimic the disease.
Magnetic Resonance Imaging
An important advantage of MRI in the imaging of meningiomas is its superior resolution of different types of soft tissue, multiplanar capability, and 3-dimensional (3-D) reconstruction (see the images below).[17, 18]
Parasagittal meningioma. A: Nonenhanced Sagittal T1-weighted magnetic resonance image (MRI) shows a solid dural isointense mass with bone invasion and compression against the parietal cortex. B: Contrast-enhanced sagittal T1-weighted MRI demonstrates partially intense enhancement of the tumor. C: Coronal T2-weighted image shows isointense mass meaning hard tissue. This finding is observed on fibroblastic meningiomas. D: Contrast-enhanced T1weighted axial MRI shows hyperintense image located within the bony marrow.
A: Noncontrast angio-magnetic resonance image (MRI) on lateral view demonstrates occluded superior sagittal sinus due to meningioma invasion. B: MRI reconstruction shows sagittal venous obstruction and 3-dimensional (3-D) appearance of the tumor.
MRI can demonstrate tumor vascularity, arterial encasement, venous sinus invasion, and the relationship between the tumor and surrounding structures. This modality is particularly advantageous in depicting the juxtasellar area and the posterior fossa and in demonstrating the rare presence of disseminated disease via the CSF. The multiplanar capability is often the best means to visualize the broad contact of tumors to the meninges, tumor capsules, and meningeal contrast enhancement adjacent to the tumor.[26, 27, 28] See the following images.
Brain meningioma. Nonenhanced T1-weighted sagittal magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous, long-T1, round mass with thin capsule is present. The tumor is attached to the left sagittal dura. Mass effect is noted
against the ventricular trigone. Brain meningioma. Nonenhanced axial magnetic resonance image demonstrates a typical parasagittal meningioma. T1-weighted image shows a homogeneous, long-T1, round mass with thin capsule. The tumor is attached to the left side of the falx.
Mass effect is noted on the adjacent gyri. Brain meningioma. Coronal T2weighted magnetic resonance image demonstrates a typical parasagittal meningioma. Isointense and inhomogeneous tumor without peripheral edema indicates a more fibrous and harder character (ie, a
fibroblastic meningioma). Brain meningioma. Contrast-enhanced T1-weighted axial magnetic resonance image demonstrates a typical parasagittal meningioma. A homogeneous,
enhancing, globose mass is depicted. Brain meningioma. Contrast-enhanced T1-weighted coronal magnetic resonance image shows a typical parasagittal meningioma. A homogeneous, enhancing, globose mass is depicted.
On nonenhanced T1-weighted images, most meningiomas have no signal intensity difference compared with cortical gray matter. Fibromatous meningiomas may be more hypointense than the cerebral cortex. Meningiomas are hyperintense on T2-weighted images, and T2-weighted images also show the extent of edema. See the images below.
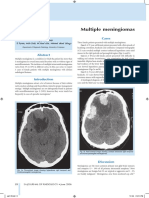
Multiple meningiomas. A: Sagittal T1-weighted magnetic resonance image (MRI) demonstrates posterior fossa and parietal meningiomas. B: Gadolinium enhancement on sagittal T1-weighted MRI shows intense enhancing of the masses. C: T2-weighted coronal MRI shows stable hypointense appearance of the posterior mass after endovascular embolization.
Malignant and multiple meningiomas. A 47-year-old white male underwent gamma knife surgery due to left convexity meningioma, followed by microsurgical removal of the tumor in 2001. A, B: Four years later, in 2005, MRI showed a stable residual parietal/occipital mass. The left sigmoid sinus is occluded. C, D: One small right frontal meningioma also underwent radiosurgery at the same time. Edema and intense enhancing after gadolinium injection is demonstrated.
On MRI and CT, meningiomas exhibit the same enhancement appearance after the injection of contrast medium. Intense enhancement is seen in 85% of tumors. A ring appearance may represent a capsule. Meningiomas have a collar of thickened, enhancing tissue that surrounds their dural attachment; this is also known as a dural tail. This sign represents thickened dura, which may be either reactive or neoplastic. A dural tail occurs in approximately 65% of meningiomas and 15% of other peripheral tumors; therefore, it is a good predictor of lesion identity. Although this radiographic feature is not specific for meningiomas, it is highly suggestive of the diagnosis. Histologic subtypes may have different MRI appearances, but this does not suffice for a histologic diagnosis by using MRI. Hyperintensity on T2-weighted images indicates soft-tumor consistency and microhypervascularity. This is seen more often in aggressive, angioblastic, or meningothelial tumors. T2-weighted signal intensity is best correlated with both the histology and consistency of the meningioma. Generally, low-intensity portions of the tumor on T2-weighted images indicate a more fibrous and harder character (eg, fibroblastic meningiomas), whereas higher-intensity portions indicate a softer character (eg, angioblastic tumor).[29, 30, 31] A typical meningioma is a homogeneous, markedly enhancing extra-axial mass. It may show meningeal cysts, ring enhancement, fatty transformation, and en plaque morphology. Malignant meningiomas may invade the calvarium and cerebral parenchyma (1%). Most meningiomas can be diagnosed by MRI.[17, 18, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41] MRS reveals lactate in embolized areas of the meningioma immediately after embolization. Lipids are not observed before the third day after embolization and are always associated with avascular and soft tissue at the time of surgery.
Gadolinium warning
Gadolinium-based contrast agents (gadopentetate dimeglumine [Magnevist], gadobenate dimeglumine [MultiHance], gadodiamide [Omniscan], gadoversetamide [OptiMARK], gadoteridol [ProHance]) have been linked to the development of nephrogenic systemic fibrosis (NSF) or nephrogenic fibrosing dermopathy (NFD). For more information, see the eMedicine topic Nephrogenic Systemic Fibrosis. The disease has occurred in patients with moderate to endstage renal disease after being given a gadolinium-based contrast agent to enhance MRI or MRA scans. NSF/NFD is a debilitating and sometimes fatal disease. Characteristics include red or dark patches on the skin; burning, itching, swelling, hardening, and tightening of the skin; yellow spots on the whites of the eyes; joint stiffness with trouble moving or straightening the arms, hands, legs, or feet; pain deep in the hip bones or ribs; and muscle weakness. For more information, see the FDA Public Health Advisory or Medscape.
Degree of confidence
In general, the sensitivity and specificity of MRI are high in the diagnosis of meningiomas. MRI has proved to be superior in delineation of the tumor and its relation with surrounding structures. However, MRI is unreliable for recognition of tumor calcification, and acute hemorrhage is often difficult to image with this modality.
False positives/negatives
False-negative findings of tumor calcium must be considered. Delineation of acute hemorrhage into tumor with conventional sequences is a disadvantage of MRI and may generate false findings
Ultrasonography
The location of intratumoral hemorrhage, cystic changes inside or outside of the tumor mass, calcifications, invasion of the parenchyma by malignant meningiomas, and lobulated or multilobulated masses is demonstrable only with intraoperative ultrasonography.
Angiography
Although magnetic resonance angiography (MRA and magnetic resonance venography [MRV]) have decreased the role of classical angiography, the latter remains a powerful tool for embolization and planning surgery. Angiography is still indispensable if embolization of the tumor is deemed necessary (see the image below).[39, 42, 43]
A: Noncontrast angio-magnetic resonance image (MRI) on lateral view demonstrates occluded superior sagittal sinus due to meningioma invasion. B: MRI reconstruction shows sagittal venous obstruction and 3-dimensional (3-D) appearance of the tumor.
Meningiomas are supplied by meningeal branches of the internal and external carotid artery (see the following images). Basal meningiomas of the anterior and middle cranial fossa and meningiomas of the wings of the sphenoid bone are commonly supplied by the internal carotid artery. Other supratentorial meningiomas are supplied by the internal and external carotid arteries.
Brain meningioma. Middle fossa meningioma. Internal carotid artery demonstrates considerable supply from petrous branch. The external carotid artery provided the main
blood supply to the tumor. Brain meningioma. Parasellar meningioma. Lateral projection from internal carotid angiography shows multiple opacified tumoral vessels in a radial distribution. Circumferential narrowing of the supraclinoid carotid portion is depicted.
Tumors that arise along the falx, the sphenoidal ridge, and the convexity are supplied by the middle meningeal artery. Falcine meningiomas can be supplied additionally by the anterior meningeal artery. Parasellar and tentorium tumors are supplied by the hypophyseal meningeal artery. Direct meningeal arteries from the cavernous sinus can supply meningiomas of the middle cranial fossa. Intraventricular tumors are supplied by anterior and posterior choroidal arteries. See the images below.
Brain meningioma. Parietal-convexity meningioma. Selective injection of the left middle meningeal artery shows inhomogeneous enhancing tumor. Intense vascularity is appreciated on the posterior aspect of the mass. Drainage veins are not seen.
External carotid and vertebral branches supply tumors of the posterior fossa. Large meningiomas can be supplied by pia vessels around the tumor. Meningeal arteries penetrate to a meningioma through its dural attachment with inside branches radially distributed like sunrays. Homogeneous sharp tumor staining is seen early and remains late. Usually, meningiomas do not exhibit drainage veins, but angioblastic types can display it. In summary, angiography is useful in delineating the blood supply of the external versus internal carotid arteries and can show encasement of intracranial vessels. Angiography demonstrates an arterial map for preoperative embolization (see the image below).
Brain meningioma. Cerebellopontine angle meningioma. Selective angiogram of right occipital artery shows focal hypervascularity through the auricular artery. Early and
delayed staining is seen.
Brain meningioma. Cerebellopontine angle
meningioma. Right occipital artery embolized with polyvinyl alcohol particles before surgery.
Digital subtraction angiography. A, B: Left external carotid artery shows early and delayed stain of the mass through media meningeal, superficial temporal arteries. C: Occipital artery. D: The branches were embolized before the surgical procedure. The tumor was partially
removed due to cranial base involvement. Embolization may be the only treatment required in older or high-risk patients. Meningeal vessels from the internal carotid artery should supply the tumor. Mass effect should persist after embolization of the middle meningeal artery.
As an alternative to traditional catheter angiography, 3-D CT angiography may depict the relationship between skull base meningiomas and neighboring bony and vascular structures clearly, quickly, and with minimal risk to the patient.
Degree of confidence
Angiography has a high degree of confidence in recognizing the arterial source of the meningioma. Tumor feeding can be identified with a low rate of false-positive and/or falsenegative findings.
False positives/negatives
Arterial findings have a high sensitivity and specificity in the diagnosis of meningiomas. Angiography shows an arterial map for preoperative embolization with a low false-finding rate.
You might also like
- Brain Tumor: Clinical Imaging Center, 1 Affiliated Hospital of Jinan University. Liu XiaodanDocument31 pagesBrain Tumor: Clinical Imaging Center, 1 Affiliated Hospital of Jinan University. Liu XiaodanWai Kwong ChiuNo ratings yet
- Extra Aksial Brain TumorsDocument15 pagesExtra Aksial Brain TumorsPPDSNeuroUnsri RSMH0% (1)
- Meu Artigo MeningiomaDocument8 pagesMeu Artigo MeningiomapeddrohNo ratings yet
- Magnetic Resonance Imaging of Meningiomas: A Pictorial ReviewDocument10 pagesMagnetic Resonance Imaging of Meningiomas: A Pictorial ReviewKevin EdroNo ratings yet
- Ginsberg 1996Document10 pagesGinsberg 1996husna fitriaNo ratings yet
- TMP BCFFDocument3 pagesTMP BCFFFrontiersNo ratings yet
- Bacterial MeningitisDocument21 pagesBacterial MeningitisMeLonk Oh MeLonkNo ratings yet
- Braib TumorDocument16 pagesBraib TumorPPDSNeuroUnsri RSMHNo ratings yet
- Ecr2015 C-1092Document21 pagesEcr2015 C-1092irsyad120No ratings yet
- Imagerie Des TumeursDocument14 pagesImagerie Des TumeursOuma TaziNo ratings yet
- Meningioma TentorialDocument9 pagesMeningioma TentorialFiorella Alexandra HRNo ratings yet
- DR - Ign Purna Putra, Sps (K)Document64 pagesDR - Ign Purna Putra, Sps (K)Sheryl ElitaNo ratings yet
- Case Report on Chondrosarcoma of the Temporomandibular JointDocument9 pagesCase Report on Chondrosarcoma of the Temporomandibular JointCatalina Soler LioiNo ratings yet
- Imaging Findings in Bacterial MeningitisDocument27 pagesImaging Findings in Bacterial MeningitisMelvy RozaNo ratings yet
- Kelompok 6 Mri For Pituitary GlandDocument23 pagesKelompok 6 Mri For Pituitary GlandAndahZantman AsmirandahNo ratings yet
- MeningiomaDocument19 pagesMeningiomaRavanno Fanizza HarahapNo ratings yet
- Cns Tuberculosis: K Mohamed RafiDocument55 pagesCns Tuberculosis: K Mohamed RafiThiyagarajan ShanmugamNo ratings yet
- Imaging The Temporal Bone: NeuroradiologyDocument15 pagesImaging The Temporal Bone: NeuroradiologyMaulidianaIndahNo ratings yet
- Mature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportDocument5 pagesMature Cystic Teratoma of The Right Cerebellopontine Angle A Rare Case ReportHaribabuBabuNo ratings yet
- Intradural Extramedullary Spinal Tumors GuideDocument4 pagesIntradural Extramedullary Spinal Tumors Guideabishek22No ratings yet
- Seizures, Headaches, and Right Hemiparesis: MeningiomaDocument2 pagesSeizures, Headaches, and Right Hemiparesis: MeningiomacazecageNo ratings yet
- JURNAL SEMANGAT Edit 1Document44 pagesJURNAL SEMANGAT Edit 1Usman Agus PrasetyoNo ratings yet
- Surgical Neurology International: Unusual Growth Pattern of A MeningiomaDocument3 pagesSurgical Neurology International: Unusual Growth Pattern of A MeningiomaJamie NicholsNo ratings yet
- Infection CNS ImagingDocument55 pagesInfection CNS ImagingAndika PradanaNo ratings yet
- Deep Sylvian Meningioma: A Case Report and Review of LiteratureDocument4 pagesDeep Sylvian Meningioma: A Case Report and Review of LiteratureLINA ESTRADA DUQUENo ratings yet
- The Dural Tail Sign-Beyond Meningioma: A. Guermazi, F. Lafitte, Y. Miaux, C. Adem, J.-F. Bonneville, J. ChirasDocument18 pagesThe Dural Tail Sign-Beyond Meningioma: A. Guermazi, F. Lafitte, Y. Miaux, C. Adem, J.-F. Bonneville, J. ChirasKhương Hà NguyễnNo ratings yet
- Promotion of Well Being During Treatment For.12Document17 pagesPromotion of Well Being During Treatment For.12Nica SalazarNo ratings yet
- Malak 2021Document19 pagesMalak 2021Firmansyah FirmansyahNo ratings yet
- Imaging of OrbitDocument69 pagesImaging of OrbitFaisal ShembeshNo ratings yet
- MeningiomaDocument7 pagesMeningiomaLili HapverNo ratings yet
- Yuh2009 Article ImagingOfEpendymomasMRIAndCTDocument11 pagesYuh2009 Article ImagingOfEpendymomasMRIAndCTHuyen NguyenNo ratings yet
- Cerebellopontine Angle TumorsDocument75 pagesCerebellopontine Angle TumorsNiveditha Mariam AbrahamNo ratings yet
- Imaging Features of Salivary Gland TumoursDocument11 pagesImaging Features of Salivary Gland TumourskaryndpNo ratings yet
- Imaging in OtorhinolaryngologyDocument38 pagesImaging in OtorhinolaryngologyNurin AlifatiNo ratings yet
- MR Spectroscopy-Aided Differentiation: "Giant" Extra-Axial Tuberculoma Masquerading As MeningiomaDocument3 pagesMR Spectroscopy-Aided Differentiation: "Giant" Extra-Axial Tuberculoma Masquerading As Meningiomaselvie87No ratings yet
- Painful Suprapatellar Mass: DiscussionDocument4 pagesPainful Suprapatellar Mass: DiscussionGabriela Serra del CarpioNo ratings yet
- (10920684 - Neurosurgical Focus) Olfactory Groove MeningiomasDocument5 pages(10920684 - Neurosurgical Focus) Olfactory Groove Meningiomasnithin shenoiNo ratings yet
- Causas de Isquemia Na MedulaDocument12 pagesCausas de Isquemia Na MeduladianaNo ratings yet
- Malignant Mesothelioma ImagingDocument5 pagesMalignant Mesothelioma ImagingPriskila LiaNo ratings yet
- CPA Lesion Imaging Guide: Enhancing Extra-Axial MassesDocument11 pagesCPA Lesion Imaging Guide: Enhancing Extra-Axial MassesKhương Hà NguyễnNo ratings yet
- ResearchDocument10 pagesResearchdrdannybmcNo ratings yet
- Intracranial CystsDocument9 pagesIntracranial CystsjosephNo ratings yet
- Multiple Cranial Nerve PalsiesDocument11 pagesMultiple Cranial Nerve PalsiesVijay BabuNo ratings yet
- Imaging in Brain TumorDocument142 pagesImaging in Brain TumorMagrinov AzaniaNo ratings yet
- Diagnostic Imaging ENTDocument8 pagesDiagnostic Imaging ENTjdecker78No ratings yet
- Meningioma in The Lumbar SpineDocument12 pagesMeningioma in The Lumbar Spinemex487No ratings yet
- Pembimbing: Dr. Partodji, SP - Rad Oleh: 1. Ira Rahmawati 2. Pradnya Ayu 3. LimastaniDocument32 pagesPembimbing: Dr. Partodji, SP - Rad Oleh: 1. Ira Rahmawati 2. Pradnya Ayu 3. Limastaniira rahmaNo ratings yet
- (10920684 - Neurosurgical Focus) Meningiomas - The Role of Preoperative Angiography and EmbolizationDocument4 pages(10920684 - Neurosurgical Focus) Meningiomas - The Role of Preoperative Angiography and EmbolizationBesseMarwah AgusHusainNo ratings yet
- Multiple MeningiomasDocument3 pagesMultiple Meningiomasarun gowdaNo ratings yet
- MR of CNS Tumors and Tumor Mimics PDFDocument10 pagesMR of CNS Tumors and Tumor Mimics PDFhimadriNo ratings yet
- Vasc Lesions H & NDocument6 pagesVasc Lesions H & Nإسلام الجزيريNo ratings yet
- KLP 10 - Jurnal - MeningiomaDocument11 pagesKLP 10 - Jurnal - Meningiomawahy udiNo ratings yet
- Case Report: Anaplastic Meningioma: A Case Report and Literature ReviewDocument7 pagesCase Report: Anaplastic Meningioma: A Case Report and Literature Reviewprabowoaji12No ratings yet
- Meningioma Quístico, Un Desafío DiagnósticoDocument4 pagesMeningioma Quístico, Un Desafío DiagnósticoPamela WheelockNo ratings yet
- Extracranial Metastases of Anaplastic Meningioma: Case ReportDocument6 pagesExtracranial Metastases of Anaplastic Meningioma: Case ReportRizky AdriansahNo ratings yet
- Head-Neck Schwannoma: Presenting As A Huge Posterior Neck SwellingDocument3 pagesHead-Neck Schwannoma: Presenting As A Huge Posterior Neck SwellingTareq MohammadNo ratings yet
- Spinal En-Plaque Meningioma Case ReportDocument7 pagesSpinal En-Plaque Meningioma Case ReportArif Susilo RahadiNo ratings yet
- MR CT ParanasalSinusDocument21 pagesMR CT ParanasalSinusYongNo ratings yet
- Calcaneal Lytic Lesions LeslieDocument31 pagesCalcaneal Lytic Lesions Leslielesliejose1995No ratings yet
- Lion Air Eticket Itinerary / ReceiptDocument2 pagesLion Air Eticket Itinerary / ReceiptBramanda Sml TobingNo ratings yet
- PDUI SeminarDocument1 pagePDUI SeminarBramanda Sml TobingNo ratings yet
- Adult Sinusitis GuidelineDocument31 pagesAdult Sinusitis Guidelineralu33No ratings yet
- JyhfjfuhthgdhgdhdghgdhDocument1 pageJyhfjfuhthgdhgdhdghgdhBramanda Sml TobingNo ratings yet
- AaosDocument8 pagesAaosBramanda Sml TobingNo ratings yet
- Abdominal TraumaDocument60 pagesAbdominal TraumaBramanda Sml TobingNo ratings yet
- Dasar-Dasar Metodologi Penelitian Klinis. Edisi 3. Jakarta: Sagung SetoDocument2 pagesDasar-Dasar Metodologi Penelitian Klinis. Edisi 3. Jakarta: Sagung SetoBramanda Sml TobingNo ratings yet
- Paper Bramanda Tobing PDFDocument7 pagesPaper Bramanda Tobing PDFBramanda Sml TobingNo ratings yet
- Bells PalacyDocument6 pagesBells PalacyBhushan VichareNo ratings yet
- Bell's Palsy Pathophysiology LongDocument4 pagesBell's Palsy Pathophysiology LongJad Paulo Gatera50% (2)
- ANTIBIOTIC PK PD THE ART of ANTIBIOTIC (Dr. RI)Document22 pagesANTIBIOTIC PK PD THE ART of ANTIBIOTIC (Dr. RI)Dedek PutrawanNo ratings yet
- Agnikumara Rasa A Herbo Mineral Formulation ReviewDocument3 pagesAgnikumara Rasa A Herbo Mineral Formulation ReviewEditor IJTSRDNo ratings yet
- New HSV EraserDocument108 pagesNew HSV EraserDashar WilsonNo ratings yet
- A Comparative Clinical Study ofDocument11 pagesA Comparative Clinical Study ofArter AdamNo ratings yet
- Toacs 8Document305 pagesToacs 8Mobin Ur Rehman Khan100% (2)
- AmpicillinDocument1 pageAmpicillinMichael KuzbytNo ratings yet
- Stress SymptomsDocument3 pagesStress SymptomsZuh KiNo ratings yet
- GE Versana Balance Platinum BrosjyreDocument8 pagesGE Versana Balance Platinum BrosjyreRicky ImranNo ratings yet
- The Treatment For Dengue Fever Is Often Supportive in NatureDocument8 pagesThe Treatment For Dengue Fever Is Often Supportive in NatureJames FabioNo ratings yet
- CH04 PMCTC ALARM - Prof. DR - Dr. Noroyono Wibowo, SpOG (K)Document41 pagesCH04 PMCTC ALARM - Prof. DR - Dr. Noroyono Wibowo, SpOG (K)Putri MahacakriNo ratings yet
- A Guide For Patients and Physicians: The Washington State Medical Marijuana ActDocument4 pagesA Guide For Patients and Physicians: The Washington State Medical Marijuana Actelioom100% (2)
- Critique Presentation: Vaishali Rathava 2 Year M.SC Nursing ROLL NO:-09Document12 pagesCritique Presentation: Vaishali Rathava 2 Year M.SC Nursing ROLL NO:-09VaishaliNo ratings yet
- Assignment 3 (Clerkship)Document11 pagesAssignment 3 (Clerkship)Ataur RahmanNo ratings yet
- 2023 Atrial Fibrillation Guideline-at-a-Glance: Societal StatementDocument5 pages2023 Atrial Fibrillation Guideline-at-a-Glance: Societal StatementMiguel Limaylla ZapataNo ratings yet
- Theorist Task Stage Patient Description 1. Erik Erikson Generativity vs. StagnationDocument8 pagesTheorist Task Stage Patient Description 1. Erik Erikson Generativity vs. StagnationRina CebreroNo ratings yet
- Assingment 1Document2 pagesAssingment 1Natria Hikmatul AminNo ratings yet
- Combustio: DR - Dian SyahputraDocument35 pagesCombustio: DR - Dian SyahputraYulliza Kurniawaty LNo ratings yet
- Safety Tips For Covid-19Document5 pagesSafety Tips For Covid-19Angelo AsoqueNo ratings yet
- BI in Healthcare IndustryDocument14 pagesBI in Healthcare IndustryAnne Chaitanya Venkat100% (1)
- ChemotherapyDocument4 pagesChemotherapyKartik KumarNo ratings yet
- RubellaDocument4 pagesRubellaRose Mary De GuzmanNo ratings yet
- Falls in Older PeopleDocument18 pagesFalls in Older PeoplePabloIgLopezNo ratings yet
- Appelant T10Document19 pagesAppelant T10shreeyasingh0929No ratings yet
- Lesson 4 Infancy by HurlockDocument44 pagesLesson 4 Infancy by HurlockJessica Recaido100% (1)
- Stress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentDocument16 pagesStress Ulcer Ditinjau Dari Aspek Patofisiologi Dan TreatmentJufri NstNo ratings yet
- Para PhimosisDocument9 pagesPara PhimosisNazurah Azmira100% (1)
- Multicultural Approa of Tibetan WindDocument7 pagesMulticultural Approa of Tibetan Windxin chenNo ratings yet
- Lanjutan StrengteningDocument5 pagesLanjutan Strengtening'fanny Quenhita'No ratings yet
- Community Medicine Module Book PDFDocument37 pagesCommunity Medicine Module Book PDFLiya SuwarniNo ratings yet
- Sector409056 PDFDocument467 pagesSector409056 PDFVictor BogdanNo ratings yet