Professional Documents
Culture Documents
Chapter 27
Uploaded by
monster40lbsCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 27
Uploaded by
monster40lbsCopyright:
Available Formats
Chapter 27: Pulmonology
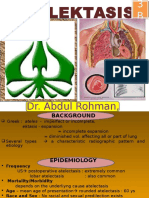
Pulmonology- study of the respiratory system. COPD (Chronic Obstructive Pulmonary Disease)- a disease characterized by a decreased ability of the lungs to perform the function of ventilation. Process of Gas Exchange Ventilation- the mechanical process of moving air in and out of the lungs. Diffusion- the movement of molecules through a membrane from an area of greater concentration to an area of lesser concentration. Perfusion- the circulation of blood through the capillaries. o Lung perfusion is dependent on 3 conditions Adequate blood volume Intact pulmonary capillaries Efficient pumping of blood by the heart Hemoglobin (Hb)- the transport protein that carries O2 in the blood. Oxygen dissociation curve- as fully oxygen-bound hemoglobin begins to release oxygen, it more readily sheds additional oxygen. Basically, the more Hb the more O2 can be transported. Changes in body temperature, blood pH, and the PCO2 can all alter the Oxygen dissociation curve. Bohr effect- phenomenon in which a decrease in PCO2/acidity causes an increase in the quantity of O2 that binds w/ the hemoglobin and, conversely, an increase in PCO2/acidity causes the hemoglobin to give up a greater quantity of O2. CO2 is transported from the cells to the lungs in one of three ways. 1. as bicarbonate ion- is predominantly what CO2 is converted to 2. bound to the globin portion of the hemoglobin molecule 3. dissolved in plasma (measured as PCO2) Respiration- the exchange of gases between a living organism and its environment. Pathophysiology Disruption in Ventilation o Upper and Lower Respiratory Tract Obstruction o Chest Wall & Diaphragm Pneumothorax- a collection of air in the pleural space, causing a loss of the negative-pressure that binds the lung to the chest wall. Hemothorax- a collection of blood in the pleural space. Flail chest- one or more ribs fractured in two or more places, creating an unattached rib segment. o Nervous System- certain abnormal respiratory patterns are produced by specific brain injury or illness. Kussmauls respirations- deep, slow or rapid, gasping breathing. Associated w/ diabetic ketoacidosis Cheyne-Stokes respirations- progressively deeper, faster breathing alternating gradually w/shallow, slower breathing, indicating brain stem injury.
Biots respirations- irregular pattern of rate and depth w/ sudden, periodic episodes of apnea, indicating increased ICP. Central neurogenic hyperventilation- deep, rapid respirations, indicating increased ICP. Agonal respirations- shallow, slow or infrequent breathing, indicating brain anoxia. Disruption in Diffusion- any disruption in diffusion can cause Hypoxia o Hypoxia- state in which insufficient O2 s available to meet the O2 requirements of the cells. Disruption in Perfusion- any state that reduces the normal circulating blood volume, such as trauma, hemorrhage, dehydration, shock or other causes of Hypovolemia, will limit normal perfusion or the lungs. o Pulmonary shunting- when an area of lung tissue is appropriately ventilated but no capillary perfusion occurs, available O2 is not moved into the circulatory system. Assessment of the Respiratory System Scene Size Up1. Is the Scene Safe to approach the patient? 2. Are there visual clues that might provide information regarding the patients medical complaint? Initial Assessment o General impression Position?- tripod, usually respiratory distress will be upright Color ?1. Pallor- paleness 2. Diaphoresis- sweatiness 3. Cyanosis- bluish discoloration of the skin due to an increase in reduced hemoglobin in the blood. The condition is directly related to poor ventilation. Mental status- AVPU Ability to speak- possibly can only speak 1-2 word sentences Respiratory effort4. Nasal flaring- excessive widening of the nares w/respiration 5. Accessory muscle- use indicates significant breathing effort. 6. Pursed lips 7. Tracheal tugging- retraction of the tissues of the neck due to airway obstruction or Dyspnea. o Airway- Principals to assessing the airway Noisy breathing nearly always means partial airway obstruction Obstructed breathing is not always noisy The brain can survive only a few minutes in asphyxia.
8. Asphyxia- a decrease in the amount of O2 & an increase in the amount of CO2 as a result of some interference w/respiration. Artificial respiration is useless if the airway is blocked. A patent airway is useless if the patient is apneic. If you note airway obstruction, fix it immediately. o Breathing- suggested signs of possible life-threatening respiratory problems in adults. 1) Alterations in mental status 2) Severe central cyanosis 3) Absent breath sounds 4) Audible Stridor 5) 1-2 word Dyspnea 6) Tachycardia 130bpm 7) Pallor and diaphoresis 8) Accessory muscle use during labored breathing Focused History & Physical Examination o History SAMPLE OPQRST ? Orthopnea- Dyspnea while lying supine ? Paroxysmal Nocturnal Dyspnea- short attacks of Dyspnea that occur at night and interrupt sleep. ? Hemoptysis- expectoration of blood from the respiratory tree. o Physical Examination Head Neck Chest Inspection Palpation o Crepitus- crackling sounds o Subcutaneous Emphysema- presence of air in the subcutaneous tissue. o Tactile fremitus- vibratory tremors felt through the chest by palpation. o Tracheal deviation- any position of the trachea other that midline Percussion Auscultation o Snoring- partial obstruction of upper airway by tongue o Stridor- associated w/laryngeal edema or constriction o Wheezing- associated w/bronchiolar constriction
o Crackles (Rales)- associated w/ fluid in the smaller bronchioles o Rhonchi- associated w/inflammation, mucus, or fluid in the bronchioles o Pleural Friction Rub- sounds like dried pieces of leather rubbing together; occurs when the pleura becomes inflamed, as in pleurisy. Extremities o Vital Signs Blood Pressure Pulsus paradoxus- a drop in the systolic blood pressure of 10mmHg or more w/each respiratory cycle. It is associated w/COPD and Cardiac Tamponade. Diagnostic Testing Pulse Oximetry Peak Flow Capnometry- normal 35-45% PCO2 Management of Respiratory Disorders Management Principals 1. Airway is the 1st Priority 2. Always Provide O2 to Patients w/respiratory distress or possible hypoxia o Never withhold O2 from a patient suspected of suffering hypoxia. Specific Respiratory Diseases Upper-Airway Obstruction o Causes Tongue- most common cause of Airway obstruction Foreign matter Trauma Burns Allergic reactions Infection o Management Conscious Adult- Hymlick Maneuver (5 Abdominal thrusts) Unconscious Adult- Head-tilt chin-lift, jaw-thrust, or modified jaw-thrust to attempt to open the airway. Then Abdominal thrusts. ARDS (Adult Respiratory Distress Syndrome)- form of pulmonary edema that is caused by fluid accumulating in the interstitial space within the lungs. o Causes Drowning Seizure activity or hypoventilation High altitude exposure Toxins related to septic shock o Management
Use positive pressure ventilation to support and ARDS patient who demonstrates signs of respiratory failure. BVM, ETT, C-PAP Obstructive Lung Diseaseo COPD (Chronic Obstructive Pulmonary Disease) Emphysema (Pink Puffers)- destruction of the alveolar walls distal to the terminal bronchioles. The Alveolar walls grow thick and scar due to the damage of external influences (i.e. Cigarette smoke, toxins). Cigarette smoking is the major factor contributing to emphysema in our society. Patient is barrel chested and breaths backward by trying to hold air in the lungs to keep air passages open. Chronic Bronchitis (Blue Bloaters)- is a build up of mucus in the lungs plugs the airways and obstructs airflow and gas exchange. o Asthma- is a chronic inflammatory disorder of the airways. Triggers or Inducers initiate the inflammatory reaction causing a narrowing of the bronchioles (bronchospasm) and obstruction of the airway. Intrinsic triggers predominantly affect children Extrinsic triggers predominantly affect adults Common Signs of Asthma Dyspnea Wheezing Cough Asthma Management Goals: Correct hypoxia Reverse bronchospasm Reduce inflammation Upper Respiratory Infection (URI)- an interference w/air movement through the upper airway. o The best defense against spread of upper respiratory infection is common practices such as good hand washing and covering the mouth during coughing and sneezing. o Viruses are responsible for a vast majority of URIs, and bacteria also produce infection as well. o 30% of URIs are Strep Throat from the bacteria Group A streptococcus. Pneumonia- acute infection of the lung, including alveolar spaces and interstitial tissue. Lung Cancer (Neoplasm)- is the leading cause of cancer-related death in the US in both & . Toxic Inhalation- of toxic substances into the respiratory tract can cause pain, inflammation, or destruction of the pulmonary tissue. o Products that can result in the formation of corrosive acids or alkalis Ammonia (ammonium hydroxide) Nitrogen oxide (nitric acid) Sulfur dioxide (sulfurous acid)
Sulfur trioxide (sulfuric acid) Chlorine (hydrochloric acid) Carbon Monoxide (CO) Inhalation- CO is an odorless, tasteless, colorless gas produced from the incomplete burning of fossil fuels and other coarboncontaining compounds. o CO has an affinity for hemoglobin 200 times that of O2. Pulmonary Embolism- is a blood clot (thrombus), air or fat embolism or some other particle that lodges in a pulmonary artery, effectively blocking blood flow through that vessel. Spontaneous Pneumothorax- a Pneumothorax that occurs spontaneously, in the absence of blunt or penetrating trauma. Hyperventilation Syndrome- is characterized by rapid breathing, chest pains, numbness, and other symptoms usually associated w/anxiety or a situational reaction. o Popedal spasm- cramping of the muscles of the feet and hands CNS (Central Nervous System) Dysfunction- due to head trauma, stroke, brain tumors, & various drugs. Dysfunction of the Spinal Cord, Nerves, or Respiratory Muscles- numerous disorders can interfere w/ respiratory function; including spinal cord trauma, polio, ALS or Lou Gehrigs Disease, viral infections, and myasthenia gravis.
You might also like
- Neurotransmitter chart functions effects drugsDocument1 pageNeurotransmitter chart functions effects drugsmonster40lbs100% (2)
- Ageism PowerpointDocument11 pagesAgeism Powerpointapi-254132646No ratings yet
- Schizophrenia PowerpointDocument53 pagesSchizophrenia Powerpointmonster40lbsNo ratings yet
- Respiratory Nursing #1Document19 pagesRespiratory Nursing #1shenric16100% (12)
- Care of A Child With RespiratoryDocument185 pagesCare of A Child With RespiratoryVanessa Lopez100% (1)
- Obstructive Disease of Lung and Physiotherapy ManagementDocument76 pagesObstructive Disease of Lung and Physiotherapy Managementphysio43100% (1)
- Abnormal Psychology Study GuideDocument243 pagesAbnormal Psychology Study GuideAllissa Michelle Kimker83% (23)
- Respiratory System-Review PathoDocument100 pagesRespiratory System-Review PathoSadiePartington-RiopelleNo ratings yet
- Breathing and Exchange of Gases ExplainedDocument40 pagesBreathing and Exchange of Gases ExplainedPranesh ShandilyaNo ratings yet
- Lower Respiratory Disorders Part 1Document70 pagesLower Respiratory Disorders Part 1Joseph Krafft100% (1)
- Respiratory SystemDocument19 pagesRespiratory Systemtheodore_estradaNo ratings yet
- Patho Respiratory - KatherineDocument9 pagesPatho Respiratory - KatherineKayla MayerNo ratings yet
- Diseases of The Respiratory System Diseases of The Respiratory System Principles of Respiratory InsufficiencyDocument9 pagesDiseases of The Respiratory System Diseases of The Respiratory System Principles of Respiratory InsufficiencyJaafar AlzuheiriNo ratings yet
- Respiratory SystemDocument18 pagesRespiratory SystemYoussef ElhamamyNo ratings yet
- Blue Bloaters and Pink PuffersDocument2 pagesBlue Bloaters and Pink PuffersAlmir SaraciNo ratings yet
- Oxygenation 1Document155 pagesOxygenation 1Khatlen BagaresNo ratings yet
- Reviewer For Management of Common IllnessDocument27 pagesReviewer For Management of Common Illnessmarie vennis hamchawanNo ratings yet
- Resp Medicine NotesDocument95 pagesResp Medicine Noteshugolucas182100% (1)
- Pulmonary SystemDocument75 pagesPulmonary Systemangeles_robert_71No ratings yet
- Interventions To Promote OxygenationDocument19 pagesInterventions To Promote OxygenationMary Ann SacramentoNo ratings yet
- Pulmonary Examination - Knowledge at AMBOSSDocument1 pagePulmonary Examination - Knowledge at AMBOSSKC Dela RosaNo ratings yet
- patholpgic change in EmphysemiaDocument16 pagespatholpgic change in Emphysemiafenil1194No ratings yet
- Bronchial AsthmaDocument71 pagesBronchial AsthmaHero MondaresNo ratings yet
- Respiratory: Welcome!Document119 pagesRespiratory: Welcome!Majo ParagasNo ratings yet
- Respiratory SystemDocument7 pagesRespiratory SystemxoxogeloNo ratings yet
- Oxygenation NotesDocument23 pagesOxygenation NoteschikaycNo ratings yet
- Lung Examination: AbnormalDocument56 pagesLung Examination: AbnormalBECAREFUL89ANo ratings yet
- Pulmonary Ventilation and OxygenationDocument87 pagesPulmonary Ventilation and Oxygenationபிரேம் குமார் ராஜாமணிNo ratings yet
- Thorax and LungsDocument11 pagesThorax and LungsJoel SantosNo ratings yet
- Respiratory SystemDocument85 pagesRespiratory SystemDr:-Ustaad Aakass Ahmed Junejo SahabNo ratings yet
- Jordan A. Mamalumpong Bsn-3 Clinical Instructor: Ma. Antonietta Edris Assignments For NCM 112 A. GlossaryDocument11 pagesJordan A. Mamalumpong Bsn-3 Clinical Instructor: Ma. Antonietta Edris Assignments For NCM 112 A. GlossaryJordan Abosama MamalumpongNo ratings yet
- Respiratory Dysfunction GuideDocument42 pagesRespiratory Dysfunction GuideHassan DayaxNo ratings yet
- The Thorax and Lungs - BATESDocument4 pagesThe Thorax and Lungs - BATESsitalcoolk100% (2)
- 2300 - Module 4 - Basic Respiratory PathophysiologyDocument26 pages2300 - Module 4 - Basic Respiratory Pathophysiologymegan.abbinkNo ratings yet
- Atelectasis SignsDocument26 pagesAtelectasis SignsArini NurlelaNo ratings yet
- NOTES2Document7 pagesNOTES2Angelica BautistaNo ratings yet
- CopdDocument4 pagesCopdapi-3739910100% (2)
- Respiratory Exam: Lungs, Breathing, CyanosisDocument81 pagesRespiratory Exam: Lungs, Breathing, CyanosisashuNo ratings yet
- Airway CopdDocument16 pagesAirway Copdfaisal alharbiNo ratings yet
- 1.) Anatomy and Physiology of The Respiratory SystemDocument6 pages1.) Anatomy and Physiology of The Respiratory SystemFaith SarmientoNo ratings yet
- Nursing Care Management - 112Document67 pagesNursing Care Management - 112Ong KarlNo ratings yet
- DR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaDocument81 pagesDR Amsalu Bekele Ass - Professor of Medicine Head of Chest Unit Department of Internal Medicine Addis Ababa University, School of Medicine Addis Ababa, EthiopiaBethelhem BirhanuNo ratings yet
- COPD & RLDDocument17 pagesCOPD & RLDhis.thunder122No ratings yet
- Clinical Physiology of Respiration: Dr. M Qathar RF TDocument76 pagesClinical Physiology of Respiration: Dr. M Qathar RF TTiwi Lestari TiwiNo ratings yet
- Assessment of Respiratory System: Submitted by Pankaj Singh Rana Nurse Practitioner in Critical Care, SrhuDocument80 pagesAssessment of Respiratory System: Submitted by Pankaj Singh Rana Nurse Practitioner in Critical Care, SrhuMary Christine Estrada CabactulanNo ratings yet
- Sesak Napas Arimbi (PBL)Document50 pagesSesak Napas Arimbi (PBL)Endik SiswantoNo ratings yet
- resp د. وفاءDocument22 pagesresp د. وفاءProf. Wafaa Mohammed Al-AttarNo ratings yet
- Lung Volumes and CapacitiesDocument9 pagesLung Volumes and CapacitiesMukesh YadavNo ratings yet
- MedSurg Ch30-31Document8 pagesMedSurg Ch30-31Vanessa Da Cruz100% (1)
- Respi Anaphy Day 1Document128 pagesRespi Anaphy Day 1Tracy Megan RusillonNo ratings yet
- Lung Examination Guide: Physical Steps, Pathologies, Dyspnea TypesDocument145 pagesLung Examination Guide: Physical Steps, Pathologies, Dyspnea TypesIrina CornilovNo ratings yet
- LP Dyspnea RevisiDocument12 pagesLP Dyspnea RevisiInsaniNo ratings yet
- Symptoms and Signs of Respiratory Disease Lecture 2: DyspnoeaDocument9 pagesSymptoms and Signs of Respiratory Disease Lecture 2: DyspnoeaShannon RamsumairNo ratings yet
- Respiratory System Anatomy and DiseasesDocument25 pagesRespiratory System Anatomy and DiseasesDaniellaNo ratings yet
- EMPHYSEMADocument2 pagesEMPHYSEMAJerick DaangNo ratings yet
- Anatomy Respiratory SystemDocument5 pagesAnatomy Respiratory SystemSusanne Seynaeve95% (20)
- Respiratory EmergencyDocument14 pagesRespiratory EmergencyThomas SentanuNo ratings yet
- Copd 200412082048Document139 pagesCopd 200412082048Richard ArceNo ratings yet
- Alterations of Pulmonary Function OutlineDocument13 pagesAlterations of Pulmonary Function Outlinemenickel3No ratings yet
- The Process of OxygenationDocument7 pagesThe Process of OxygenationMich CercadoNo ratings yet
- Atelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesFrom EverandAtelectasis, (Lung Collapse) A Simple Guide To The Condition, Diagnosis, Treatment And Related DiseasesNo ratings yet
- Pleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandPleurisy, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Your Family Doctor Asthma: Understanding Asthma / Avoiding Allergies / Proper Use of InhalersFrom EverandYour Family Doctor Asthma: Understanding Asthma / Avoiding Allergies / Proper Use of InhalersNo ratings yet
- Development Through The Lifespan: Cognitive Development in Infancy and ToddlerhoodDocument48 pagesDevelopment Through The Lifespan: Cognitive Development in Infancy and Toddlerhoodmonster40lbsNo ratings yet
- Depression: WWW - Bradfordvts.co - UkDocument28 pagesDepression: WWW - Bradfordvts.co - Ukmonster40lbsNo ratings yet
- Psychometrics NotesDocument6 pagesPsychometrics Notesmonster40lbsNo ratings yet
- Dishwasher: 24 Hours A Day, 7 Days A Week For LG Customer ServiceDocument48 pagesDishwasher: 24 Hours A Day, 7 Days A Week For LG Customer Servicemonster40lbsNo ratings yet
- 0132431564Document40 pages0132431564Rotaru RaduNo ratings yet
- Roll and Write Letters LKU1W8Document1 pageRoll and Write Letters LKU1W8monster40lbsNo ratings yet
- Motivation and EmotionDocument56 pagesMotivation and Emotionmonster40lbsNo ratings yet
- Psych 327 #15807 Sec 01 SchlussmanDocument6 pagesPsych 327 #15807 Sec 01 Schlussmanmonster40lbsNo ratings yet
- Psych 327 #11955 Sec 02 Schnieder - 0001Document8 pagesPsych 327 #11955 Sec 02 Schnieder - 0001monster40lbsNo ratings yet
- Chapter 07-IntelligenceDocument91 pagesChapter 07-Intelligencemonster40lbsNo ratings yet
- Label A SceneDocument4 pagesLabel A Scenemonster40lbsNo ratings yet
- MIT9 00SCF11 Lec20 Psych1 PDFDocument45 pagesMIT9 00SCF11 Lec20 Psych1 PDFmonster40lbsNo ratings yet
- 10 Memory: Reconstructing The Past The Biology of MemoryDocument60 pages10 Memory: Reconstructing The Past The Biology of Memorymonster40lbsNo ratings yet
- Count Tens FrameDocument1 pageCount Tens Framemonster40lbsNo ratings yet
- Developmental Psychology Chapter 1Document77 pagesDevelopmental Psychology Chapter 1monster40lbsNo ratings yet
- Development, Maturation, Aging, and Death: Lecture Presentation by Suzanne Long, Monroe Community CollegeDocument62 pagesDevelopment, Maturation, Aging, and Death: Lecture Presentation by Suzanne Long, Monroe Community Collegemonster40lbsNo ratings yet
- Substance Abuse Power PointDocument54 pagesSubstance Abuse Power Pointmonster40lbsNo ratings yet
- AnxietydisordersDocument82 pagesAnxietydisordersmayshiaNo ratings yet
- Treatment and Healing NotesDocument8 pagesTreatment and Healing Notesashley100% (1)
- Cook Handout AppendixDocument22 pagesCook Handout Appendixmonster40lbsNo ratings yet
- Psychological Disorders ExplainedDocument9 pagesPsychological Disorders Explainedmonster40lbsNo ratings yet
- Lsita de Leitura Ciencias Cognitivas - WWW - Cogsci.ucsd - Edubarragraduate-Studybarraphdbarrareading-ListDocument4 pagesLsita de Leitura Ciencias Cognitivas - WWW - Cogsci.ucsd - Edubarragraduate-Studybarraphdbarrareading-ListLiana MartinsNo ratings yet
- By: Margaret Wise Brown Adapted By: Jessie Moreau, M.Ed., NBCTDocument18 pagesBy: Margaret Wise Brown Adapted By: Jessie Moreau, M.Ed., NBCTmonster40lbsNo ratings yet
- CH 09 Morris11e IPPT FINALDocument99 pagesCH 09 Morris11e IPPT FINALmonster40lbsNo ratings yet
- Chapter Outlines of Psychology 5,6,8,9Document20 pagesChapter Outlines of Psychology 5,6,8,9monster40lbsNo ratings yet
- Lecture On Cognition, Mental Abilities, and Cognitive BiasesDocument100 pagesLecture On Cognition, Mental Abilities, and Cognitive Biasesmonster40lbsNo ratings yet
- Chapter 5 Powerpoint With Extra SlidesDocument111 pagesChapter 5 Powerpoint With Extra Slidesmonster40lbsNo ratings yet
- Muis Kidney Book ENGDocument17 pagesMuis Kidney Book ENGCrystyan CryssNo ratings yet
- Evaluation of Personal Dust Exposure of The Rice Mill Workers in AssamDocument10 pagesEvaluation of Personal Dust Exposure of The Rice Mill Workers in AssamIJAMTESNo ratings yet
- Prosecution and elements of crimes under Philippine lawsDocument14 pagesProsecution and elements of crimes under Philippine lawsNoel Cagigas FelongcoNo ratings yet
- Fetal Products AllDocument1 pageFetal Products AllIon pasterfNo ratings yet
- Excipients As StabilizersDocument7 pagesExcipients As StabilizersxdgvsdgNo ratings yet
- Three Little PigsDocument9 pagesThree Little PigsrNo ratings yet
- Maxicare Individual and Family ProgramDocument43 pagesMaxicare Individual and Family Programbzkid82No ratings yet
- Will BrinkDocument10 pagesWill BrinkJoao TorresNo ratings yet
- Campus Waste Lab Proposal To Substitute Single-Use Plastic With Paper Products and Plastic Utensils For BambooDocument14 pagesCampus Waste Lab Proposal To Substitute Single-Use Plastic With Paper Products and Plastic Utensils For Bambooapi-529878933No ratings yet
- ZV Class Links @Medliferesuscitation-CopyDocument31 pagesZV Class Links @Medliferesuscitation-CopyDebajyoti DasNo ratings yet
- Makalah ThoughtDocument5 pagesMakalah Thoughtifa safiraNo ratings yet
- 1 6Document58 pages1 6Emiliano.Armando Aguilera.Vázquez100% (1)
- Tata Bluescope Steel Limited, Jamshedpur.: Liquefied Petroleum Gas Material Safety Data SheetDocument6 pagesTata Bluescope Steel Limited, Jamshedpur.: Liquefied Petroleum Gas Material Safety Data Sheetsujit5584No ratings yet
- Carte Tehnica Partea IDocument22 pagesCarte Tehnica Partea IadrianNo ratings yet
- History of Medicine - Alexander WilderDocument555 pagesHistory of Medicine - Alexander WilderMark R. JaquaNo ratings yet
- Lesson 1:: Introduction To Science, Technology and SocietyDocument17 pagesLesson 1:: Introduction To Science, Technology and SocietyAlexis A. AguilarNo ratings yet
- Chemistry Tshirt ProjectDocument7 pagesChemistry Tshirt Projectapi-524483093No ratings yet
- Drug Study Pre OpDocument6 pagesDrug Study Pre OpgiaNo ratings yet
- Proceedings of BUU Conference 2012Document693 pagesProceedings of BUU Conference 2012Preecha SakarungNo ratings yet
- Examiner's report on F6 Taxation (UK) December 2010 paperDocument3 pagesExaminer's report on F6 Taxation (UK) December 2010 paperyorcpl200No ratings yet
- CALIS ScoringDocument2 pagesCALIS ScoringIqbal BaryarNo ratings yet
- Ra 9520 Chapter VDocument8 pagesRa 9520 Chapter VLorribelle OcenarNo ratings yet
- JDP Rainbox Attenuation CratesDocument6 pagesJDP Rainbox Attenuation CratesBerat DalyabrakNo ratings yet
- Certificate of Employment Document TitleDocument1 pageCertificate of Employment Document TitleAyni ReyesNo ratings yet
- Rexnord Thomas Flexible Disc Couplings - Series 71 - 8Document2 pagesRexnord Thomas Flexible Disc Couplings - Series 71 - 8Orlando ReisNo ratings yet
- embragues-INTORK KBK14800 Erhsa2013 PDFDocument56 pagesembragues-INTORK KBK14800 Erhsa2013 PDFPablo RuizNo ratings yet
- Product Bulletin - Menopause Balance Complex Cooling LotionDocument2 pagesProduct Bulletin - Menopause Balance Complex Cooling Lotionshaklee480No ratings yet
- UK & India Health Insurance Actuarial ExamDocument4 pagesUK & India Health Insurance Actuarial ExamVignesh SrinivasanNo ratings yet
- Thalassemia WikiDocument12 pagesThalassemia Wikiholy_miracleNo ratings yet