Professional Documents
Culture Documents
Nursing Management Child With Cancer
Uploaded by
lisalovCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Management Child With Cancer
Uploaded by
lisalovCopyright:
Available Formats
Nursing Management- Cancer In Children
Nursing Diagnosis Anxiety of parents related to learning of diagnosis Risk for Infection and hemorrhage related to bone marrow suppression caused by chemotherapy and disease Disturbed Body Image related to alopecia associated with chemotherapy Imbalanced Nutrition: Less Than Body Requirements related to anemia, anorexia, nausea, vomiting, and mucosal ulceration secondary to chemotherapy or radiation Acute Pain related to diagnostic procedures, progression of the disease, and adverse effects of treatment Activity Intolerance related to fatigue that results from the disease and treatment Anxiety of child related to hospitalization and diagnostic and treatment procedures
Decreasing Parental Anxiety
Be available to the parents when they want to discuss their feelings. Offer kindness, concern, consideration, and sincerity toward the child and parents; be a source of consolation.
Contact the family's clergyman or the hospital chaplain. Obtain the services of a social worker, as appropriate, to help the family use appropriate community resources.
Offer hope that therapy will be effective and will prolong life. Have parents speak with parents of a child currently on therapy. Encourage parents to participate in activities of daily living to help them feel a part of their child's care.
Assess family dynamics and coping mechanisms and plan interventions accordingly.
Help the parents to deal with anticipatory grief. Help the parents to deal with other family members, especially siblings and grandparents, and friends.
Encourage the parents to discuss concerns about limiting their child's activities, protecting child from infection, disciplining child, and having anxieties about the illness.
Facilitate communication with the clinic nurse or clinical specialist who may interact with the child during the entire course of illness
Preventing Infection
Monitor complete blood count (CBC) as ordered. Provide adequate hydration.
o o
Maintain parenteral fluid administration. Offer small amounts of oral fluids if tolerated.
Observe renal function carefully.
o o
Measure and record urine output. Check specific gravity.
o o
Observe the urine for evidence of gross bleeding. Use labsticks to determine if occult urinary bleeding is present.
Protect the child from infection sources.
o
Never use a rectal thermometer or drugs or enemas when caring for a neutropenic patient.
Family, friends, personnel, and other patients who have infections should not visit or care for the child. Discuss care of siblings while child is on therapy.
o o
Do not place a child with an infection in the room with a child with leukemia. Good hand washing is the most important way to control infection.
Observe the child closely and be alert for signs of impending infection.
o o
Observe broken skin or mucous membrane for signs of infection. Report fever more than 101 F (38.3 C).
Assess central line site for redness or tenderness.
Administer growth factors, such as granulocyte colony-stimulating factor, to stimulate the production of neutrophils and to decrease the incidence of severe infections in the child after intense chemotherapy.
Administer I.V. antibiotics as ordered. Administer prophylaxis Record vital signs and report changes that may indicate hemorrhage, including:
o o o o o
Tachycardia. Lowered blood pressure (BP). Pallor. Diaphoresis. Increasing anxiety and restlessness.
Observe for GI bleeding and Hematemesis Move and turn the child gently because hemarthrosis may occur and may cause pain.
o o o o
Handle the child in a gentle manner. Turn the child frequently to prevent pressure ulcers. Place the child in proper body alignment, in a comfortable position. Allow the child to be out of bed in a chair if this position is more comfortable.
Avoid I.M. injections if possible. Handle catheters and drainage and suction tubes carefully to prevent mucosal bleeding. Protect the child from injury by monitoring activities and environmental hazards. Be aware of emergency procedures for control of bleeding:
o o
Apply local pressure carefully so as not to interfere with clot formation. Administer packed RBCs and platelets as ordered.
Promoting Acceptance of Body Changes
Prepare the patient for potential changes in body image (alopecia, weight loss, muscle wasting) and help child cope with related feelings.
Engage Child Life therapist for medical play and support.
Contact the school nurse and teacher to help them prepare for the child's return to school. Discuss the bodily changes that have occurred and that may happen in the future.
Promoting Optimal Nutrition
Provide a highly nutritious diet as tolerated by the child.
o o o o o o
Determine the child's food likes and dislikes. Offer frequent, small meals. Offer high-calorie, high-protein supplemental feedings. Encourage the parents to assist at mealtime. Allow the child to eat with a group at a table if his condition allows. Avoid foods high in salt while child is taking steroids.
Give careful oral hygiene; the gums and mucous membranes of the mouth may bleed easily.
o o
Use a soft toothbrush. If the child's mouth is bleeding or painful, clean the teeth and mouth with a moistened cotton swab or sponge-tipped swab.
Use a nonirritating rinse for the mouth (no alcohol-containing mouthwash or hydrogen peroxide).
o o
Apply petroleum to dry, cracked lips. Assess for mucositis and provide appropriate mouth rinse.
Be alert for nausea and vomiting.
o
Administer antiemetic drugs on a round-the-clock, regular schedule (eg, serotonin antagonist, Ativan, dexamethasone).
Become knowledgeable about chemotherapeutic agents and adjust antiemetic therapy for those drugs with delayed nausea and vomiting.
o o
Monitor strict intake and output. Maintain parental fluid administration and assess for signs of dehydration or overhydration.
Administer antiemetic drugs for patients who receive radiation to the chest, abdomen, pelvis, or craniospinal axis.
Suggest relaxation techniques or guided imagery for patients who experience anticipatory nausea and vomiting.
Relieving Pain
Position the child for comfort. Water beds and bean bag chairs are usually helpful. Administer drugs on a preventive schedule before pain becomes intense. Continuous infusion pumps for opioid administration are used.
Manipulate the environment as necessary to increase the child's comfort and to minimize unnecessary exertion.
Prepare the child for treatment and diagnostic procedures
o
Use knowledge of growth and development to prepare the child for such procedures as bone marrow aspirations, spinal taps, blood transfusions, and chemotherapy.
Provide a means for talking about the experience. Play, storytelling, or roleplaying may be helpful.
o o
Convey to the child an acceptance of fears and anger. Use EMLA Cream for local anesthesia at spinal tap, injection, and bone marrow sites to decrease pain.
Administer conscious sedation before procedures and monitor pulse, BP, respirations, and pulse oximetry during and after procedures.
Conserving Energy
Assess the child's energy level and space needed activities accordingly. Allow the child to rest, if necessary.
Encourage the child to lie down and rest after such diagnostic procedures as bone marrow aspirations and spinal taps.
Reducing the Child's Anxiety
Provide for continuity of care. Encourage family-centered care Facilitate play activities for the child and use opportunities to communicate through play.
Maintain some discipline, placing calm limitations on unacceptable behavior. Provide appropriate diversional activities. Encourage independence and provide opportunities that allow the child to control his environment.
Explain the diagnosis and treatment in age-appropriate terms.
Community and Home Care Considerations
Begin to develop a home care plan before the child leaves the hospital. Communicate with health care provider, hospital nurses, family, and others familiar with the case to gather information about the child's illness, treatment plan, and specific needs in the home.
Arrange schedule for blood drawing and how results will be managed. Contact the child's school and arrange a meeting with the school nurse, principal, and appropriate teachers to explain child's diagnosis, treatment, and potential time away from school.
Discuss with patient the possibility of making a visit to the classroom; explain about cancer and the adverse effects of chemotherapy to facilitate school reentry.
Collaborate with primary care provider regarding immunization schedule and the contraindication for children on immunosuppressive therapy who receive live vaccines.
Make sure that parents or caregivers can demonstrate the proper technique for care of venous access, such as dressing changes, flushing, and assessing for infection.
Family Education and Health Maintenance
Teach parents about normal CBC values and expected variations caused by therapy. Instruct parents about leukemia and adverse effects of chemotherapy. Tell parents to call the health care provider if child has a fever more than 101 F (38.3 C), bleeding, signs of infections, and exposure to chickenpox if the child has not had it. Immunosuppressed children are in danger of developing disseminated varicella and may be treated prophylactically with varicella immune globulin.
Teach parents the importance of detecting and reporting fever in the child with leukemia. A fever over 101 F may indicate overwhelming infection and impending septic shock.
Teach preventive measures, such as hand washing and isolation from children with communicable diseases.
Reinforce that parents never use a rectal thermometer
You might also like
- Lifeskills PresentationDocument50 pagesLifeskills PresentationlisalovNo ratings yet
- Lifeskills PresentationDocument50 pagesLifeskills PresentationlisalovNo ratings yet
- Drugs To Watch With WARFARINDocument3 pagesDrugs To Watch With WARFARINRajendra RaiNo ratings yet
- Pediatric Advanced Life Support: Instructor Essentials Faculty GuideDocument56 pagesPediatric Advanced Life Support: Instructor Essentials Faculty GuideFajarPradhanaPutra100% (1)
- Ethical Legal IssuesDocument29 pagesEthical Legal IssueslisalovNo ratings yet
- Disturbances in OxygenationDocument10 pagesDisturbances in OxygenationjenrylNo ratings yet
- Types of AnemiaDocument11 pagesTypes of AnemiaCHRISTIE MONTANO50% (2)
- Ethical Issues in PhlebotomyDocument6 pagesEthical Issues in Phlebotomylisalov100% (1)
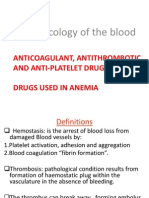
- Pharmacology of The BloodDocument63 pagesPharmacology of The BloodSawsan Z. JwaiedNo ratings yet
- 12-17-2012 Powerpoint Privilege SpeechDocument16 pages12-17-2012 Powerpoint Privilege SpeechMarge MateoNo ratings yet
- DOH Programs EEINC Newborn Screening BEmONC CEmONC NutritionDocument46 pagesDOH Programs EEINC Newborn Screening BEmONC CEmONC NutritionKRISTINE ANGELIE PANESNo ratings yet
- PartographDocument6 pagesPartographYep Yep100% (2)
- Essentials of Primary Health CareDocument40 pagesEssentials of Primary Health CareSpislgal PhilipNo ratings yet
- Dialysis BrochureDocument13 pagesDialysis BrochureRaffy FlorentinoNo ratings yet
- Pediatric RemediationDocument5 pagesPediatric RemediationAlvin L. Rozier67% (3)
- Concepts of Infection Prevention and ControlDocument21 pagesConcepts of Infection Prevention and Controllisalov100% (2)
- Topic 5 Nursing Care of The High-Risk Post-Partal ClientsDocument51 pagesTopic 5 Nursing Care of The High-Risk Post-Partal ClientsMarissa A AquinoNo ratings yet
- Acute EpiglottisDocument20 pagesAcute EpiglottissuciNo ratings yet
- Suspected Ovarian Cancer with Ascites Case ReportDocument18 pagesSuspected Ovarian Cancer with Ascites Case ReportToby MarshallNo ratings yet
- Emergency Care in NursingDocument32 pagesEmergency Care in NursingPauline Añes100% (1)
- Hellp SyndromeDocument40 pagesHellp SyndromeChairunnisa Sitorus100% (2)
- Vital Signs ModuleDocument10 pagesVital Signs ModulelisalovNo ratings yet
- Domiciliary Midwifery RDocument16 pagesDomiciliary Midwifery Rswillymadhu83% (6)
- Medication AdministrationDocument12 pagesMedication AdministrationDinah RealNo ratings yet
- Breast Cancer (Research Paper)Document12 pagesBreast Cancer (Research Paper)Katrina Arnaiz100% (3)
- Kenya ARV Guidelines 2018Document230 pagesKenya ARV Guidelines 2018Felix Wafula MusibiNo ratings yet
- Postnatal Care PDFDocument9 pagesPostnatal Care PDFYanti PoltekkesNo ratings yet
- Practicum Report: Pauline Jean F. Anoba BS Accountancy 4 YearDocument7 pagesPracticum Report: Pauline Jean F. Anoba BS Accountancy 4 YearPauline Figueras AnobaNo ratings yet
- Prepared By: P2Lt Joyce Angeline D Valencia NCDocument23 pagesPrepared By: P2Lt Joyce Angeline D Valencia NCJoan ErbelecNo ratings yet
- ETHICO OutlineDocument5 pagesETHICO Outline'emotera' Gudbai DotaNo ratings yet
- Malnutritiom and Anemia ImciDocument30 pagesMalnutritiom and Anemia ImcibaridacheNo ratings yet
- Course in The WardDocument4 pagesCourse in The WardNejie Zarrah DiazNo ratings yet
- NCM 107Document7 pagesNCM 107Jose Jumamoy100% (1)
- Report - For MaamDocument7 pagesReport - For MaamSherchen Antonio-CortesNo ratings yet
- John Q EthicsDocument2 pagesJohn Q EthicsChristianDominicTigasNo ratings yet
- Ch01Document19 pagesCh01Bridget Shienne DaculaNo ratings yet
- FluidDocument3 pagesFluidcruzjuan58No ratings yet
- Medical Indemnity InsuranceDocument2 pagesMedical Indemnity InsuranceSandeep Bansal100% (1)
- Why Do We Need To Adopt The I.M.C.I. Approach or The Integrated Management of Childhood Illness in The Philippines ?Document15 pagesWhy Do We Need To Adopt The I.M.C.I. Approach or The Integrated Management of Childhood Illness in The Philippines ?Mae DoctoleroNo ratings yet
- Newborn Hearing Screening GuidelinesDocument2 pagesNewborn Hearing Screening GuidelinesAileen A. MonaresNo ratings yet
- Pregnant Woman Diabeties ComplicationsDocument3 pagesPregnant Woman Diabeties ComplicationsAdvanced Research PublicationsNo ratings yet
- DOH Maternal Health ProgramDocument5 pagesDOH Maternal Health ProgramErwin Jake TagubaNo ratings yet
- Fundal Height DefinedDocument2 pagesFundal Height Definedervin0122No ratings yet
- Status AsthmaticusDocument6 pagesStatus AsthmaticusMae Azores100% (1)
- Family Nursing Care PlanDocument5 pagesFamily Nursing Care PlanStephen Joshua PlazaNo ratings yet
- A Review On Otitis Media (Karnapaka) : Ayurvedic Aspects and TreatmentDocument4 pagesA Review On Otitis Media (Karnapaka) : Ayurvedic Aspects and TreatmentEditor_IAIMNo ratings yet
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoNo ratings yet
- Abruptio Placenta Risks, Signs, and TreatmentDocument10 pagesAbruptio Placenta Risks, Signs, and TreatmentDoc DudayNo ratings yet
- Newborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesDocument7 pagesNewborn Screening Policy Catarman Doctors Hospital, Inc.: University of Eastern PhilippinesGenn Medrano GirayNo ratings yet
- COMMUNITY HEALTH DIAGNOSISDocument22 pagesCOMMUNITY HEALTH DIAGNOSISkuruvagadda sagarNo ratings yet
- ChikungunyaDocument2 pagesChikungunyaEagleTribNo ratings yet
- Nurs 05: Community Health Nursing 1 Community Health Nursing of Individual and Family As ClientDocument23 pagesNurs 05: Community Health Nursing 1 Community Health Nursing of Individual and Family As ClientToyour EternityNo ratings yet
- Department of Health: History, Policy, Budget, Programs For HealthDocument57 pagesDepartment of Health: History, Policy, Budget, Programs For HealthAngelica Cassandra VillenaNo ratings yet
- Case Report SwotDocument31 pagesCase Report Swotanon_252045180No ratings yet
- Concept For Abdominal BloatingDocument1 pageConcept For Abdominal BloatingChiomaDabrinze-AmosNwankwoNo ratings yet
- MaternalDocument347 pagesMaternalJosefa Capuyan100% (1)
- 10 Doh Programs: Prepared By: Dhonnalyn A. Caballero, RNDocument28 pages10 Doh Programs: Prepared By: Dhonnalyn A. Caballero, RNAnne Geleen BariasNo ratings yet
- Pertussis Case Definition and Investigation PresentationDocument62 pagesPertussis Case Definition and Investigation PresentationMuhammad Jahari Supianto100% (1)
- Cultural Factor/ethnicity Such As Regard For Elders, Perception of HealthDocument3 pagesCultural Factor/ethnicity Such As Regard For Elders, Perception of HealthQueency Jane Ursulum100% (1)
- Family Care PlanDocument3 pagesFamily Care PlanAngie MandeoyaNo ratings yet
- NCM 107-A Nursing Leadership & Management ConceptsDocument241 pagesNCM 107-A Nursing Leadership & Management ConceptsMichael Anthony Ermita50% (2)
- Post Mortem CareDocument5 pagesPost Mortem CareTaqwantrih SandiNo ratings yet
- Maternal and Child Health CareDocument7 pagesMaternal and Child Health CareNessa Layos MorilloNo ratings yet
- Breast Feeding Teaching PlanDocument2 pagesBreast Feeding Teaching Planapi-355719147No ratings yet
- LaborDocument94 pagesLaborLany Cardente PascuaNo ratings yet
- ETIC211 Moral RelativismDocument1 pageETIC211 Moral RelativismNadineNo ratings yet
- 10 Golden Rules for Safe Drug AdministrationDocument17 pages10 Golden Rules for Safe Drug AdministrationBien OcampoNo ratings yet
- Postpartum Nursing PowerpointDocument3 pagesPostpartum Nursing PowerpointAntonella VitaleNo ratings yet
- Ch03Document26 pagesCh03Bridget Shienne DaculaNo ratings yet
- Nursing considerations for clients on loop diuretics and beta blockersDocument59 pagesNursing considerations for clients on loop diuretics and beta blockersGil Raphael GanibanNo ratings yet
- Current Investment in the United Kingdom: Part One of The Investors' Guide to the United Kingdom 2015/16From EverandCurrent Investment in the United Kingdom: Part One of The Investors' Guide to the United Kingdom 2015/16No ratings yet
- Seizure Care PLNDocument9 pagesSeizure Care PLNAkhil Paul Kuriakose ManalelNo ratings yet
- S.No. Nsg. Assessment Nsg. Diagnosis Expected Outcome Nursing Interventions Evaluation Planning ImplementationDocument6 pagesS.No. Nsg. Assessment Nsg. Diagnosis Expected Outcome Nursing Interventions Evaluation Planning ImplementationgopscharanNo ratings yet
- Arterial Blood SamplingDocument11 pagesArterial Blood SamplinglisalovNo ratings yet
- LAb SectionsDocument2 pagesLAb SectionslisalovNo ratings yet
- COMMUNICATION SKILLS FOR PHELEBOTOMISTSDocument8 pagesCOMMUNICATION SKILLS FOR PHELEBOTOMISTSlisalov0% (1)
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Alzhiermiers DIseaseDocument42 pagesAlzhiermiers DIseaselisalovNo ratings yet
- Blood PanelsDocument7 pagesBlood Panelslisalov100% (1)
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Alzhiermiers DIseaseDocument42 pagesAlzhiermiers DIseaselisalovNo ratings yet
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Lesson 2 Nursing ScienceDocument9 pagesLesson 2 Nursing SciencelisalovNo ratings yet
- Age TheoriesDocument55 pagesAge TheorieslisalovNo ratings yet
- ScabiesDocument16 pagesScabieslisalovNo ratings yet
- From Dependency to Maturation: Child Development StagesDocument6 pagesFrom Dependency to Maturation: Child Development StageslisalovNo ratings yet
- Perception of The ElderlyDocument28 pagesPerception of The ElderlylisalovNo ratings yet
- Alterations in Cardiovascular FunctionDocument103 pagesAlterations in Cardiovascular FunctionlisalovNo ratings yet
- Cleft Lip PalateDocument29 pagesCleft Lip PalatelisalovNo ratings yet
- ScabiesDocument16 pagesScabieslisalovNo ratings yet
- Alterations in Eye, Ear, NoseDocument79 pagesAlterations in Eye, Ear, NoselisalovNo ratings yet
- AgeismDocument49 pagesAgeismlisalov100% (1)
- Gender and WomenDocument4 pagesGender and WomenlisalovNo ratings yet
- Recent Advances in Companion Animal Behavior ProblemsDocument9 pagesRecent Advances in Companion Animal Behavior ProblemsStephen PopeNo ratings yet
- Renal Failure in ChildrenDocument43 pagesRenal Failure in Childrendennyyy175No ratings yet
- Amlodipine Side EffectsDocument6 pagesAmlodipine Side Effects1976gt500No ratings yet
- Rheumatology Quiz.8Document2 pagesRheumatology Quiz.8Ali salimNo ratings yet
- Careers in Medicine CV Sample #4Document3 pagesCareers in Medicine CV Sample #4huyenthanh1807No ratings yet
- FP Form 1Document2 pagesFP Form 1hhhirangNo ratings yet
- Becky Patty ResumeDocument1 pageBecky Patty Resumeapi-510748241No ratings yet
- Stan Drug StudyDocument10 pagesStan Drug StudyIvan Louise Fajardo ManiquizNo ratings yet
- Jisakos 2017 000146 PDFDocument10 pagesJisakos 2017 000146 PDFemilNo ratings yet
- The Perception of Anatomy Teaching Among UK Medical StudentsDocument4 pagesThe Perception of Anatomy Teaching Among UK Medical StudentsPaul AndreasNo ratings yet
- Unresolved Questions in Selection of Therapies For Treatment Naïve Chronic Lymphocytic LeukemiaDocument22 pagesUnresolved Questions in Selection of Therapies For Treatment Naïve Chronic Lymphocytic Leukemiaguzzy235No ratings yet
- TK Heme 13-24Document49 pagesTK Heme 13-24rotat2348No ratings yet
- VSR PDFDocument12 pagesVSR PDFDrkrunal badaniNo ratings yet
- MTB Cardiology NotesDocument7 pagesMTB Cardiology Noteskabal321No ratings yet
- PNP RequirementsDocument22 pagesPNP RequirementsJEREMY WILLIAM COZENS-HARDYNo ratings yet
- Delfinm QsenDocument57 pagesDelfinm Qsenapi-346220114No ratings yet
- Journal Terapi Dermatitis SeboroikDocument4 pagesJournal Terapi Dermatitis SeboroikMohd Faie RamliNo ratings yet
- Cpga002 0Document4 pagesCpga002 0sakif sNo ratings yet
- Nexpro Uae FinalDocument13 pagesNexpro Uae Finalamr ahmedNo ratings yet
- Jonsen SieglerDocument2 pagesJonsen SieglerBramantyo NugrahaNo ratings yet
- Validation of The Filipino-Translated Version of TDocument11 pagesValidation of The Filipino-Translated Version of TRoger Jr BrazilNo ratings yet
- Pre-Existing Conditions Disclosure Form: Page 1 of 2Document2 pagesPre-Existing Conditions Disclosure Form: Page 1 of 2celeenNo ratings yet
- Retinopathy of Prematurity Handout FormatDocument31 pagesRetinopathy of Prematurity Handout FormatkaznielsNo ratings yet
- Sarcopenia - Revised European Consensus On Definition and Diagnosis 2019Document16 pagesSarcopenia - Revised European Consensus On Definition and Diagnosis 2019Matheus MartinsNo ratings yet