Professional Documents
Culture Documents
Opacidades de Vidrio Deslustrado-Guia Diagnostica
Uploaded by
Rahul KashyapCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Opacidades de Vidrio Deslustrado-Guia Diagnostica
Uploaded by
Rahul KashyapCopyright:
Available Formats
GROUND-GLASS OPACITY ON HRCT.
A GUIDE TO
DIAGNOSIS
Herrez Ortega I, Alonso Orcajo N*, Lpez Gonzlez L, Dez Fernndez FL**, Rodrguez Morejn C, Bollo E**. Radiology, Pathology*
and Respiratory Departments**. Complejo Hospitalario Len. Len. SPAIN. iherraez@hleo.sacyl.es
Objectives: To define ground-glass opacity (GGO) and to show how it can be detected on HRCT scans for diffuse lung diseases. To make diagnosis easier, by indicating the findings that narrow down the
ff differential diagnosis. To develop a diagnostic algorithm.
Methods: GGO is the slight increase of pulmonary attenuation, which permits seeing the underlying vessels and walls of the bronchi. It occurs when there is a decrease in pulmonary air for partial filling or partial
collapse of air spaces, moderate thickening of the alveolar interstice or an increase of the capillary volume. Therefore, it is a non-specific finding in which the underlying pulmonary alteration is belowthe limit of
resolutionof the HRCT.
Usually, it indicates active disease that is potentially reversible with the appropriate treatment, but if it is associated with signs of fibrosis, such as honeycomb cysts, traction bronchiectasis, distortion of the
parenchymal architecture and irregular thickening of the interlobular septa, it probably indicates fibrosis.
GGO is a very frequent finding in HRCT scans for diffuse infiltrative lung diseases. Detection is the first problemin its evaluation. GGO was detected by the dark bronchus sign, which is a lower attenuation of air
in the bronchus than in the lung surrounding it, and MinimumIntensity Projection (mIP) reconstructions. False diagnoses of GGO stemfromtechnical errors, respiratory and cardiac movements, poor inspiration
and hypoventilation in the dependent lung areas.
Subsequently, it was determined: 1) whether GGO is the predominant pattern of the disease (when the GGO is an associated finding, the differential diagnosis is based on the other dominant alterations); 2)
whether its distribution is patchy, diffuse or nodular; 3) whether or not it is accompaniedby signs of fibrosis; 4) whether the disease is acute, subacute or chronic.
GGO versus consolidation.
Axial HRCT scan shows bilateral
areas of GGO involving the
posterior regions of lower lobes
(stars). Note the consolidations,
without visible vessels (arrows).
The patient was a 54-year-old
women with cryptogenic organizing
GGO with fibrosis. Axial and coronal mIP
reconstructions help to detect honeycombing (blue
) d t ti b hi t i ( ll ) i
mIP
mIP
Ground-glass opacity (GGO).
a) Axial HRCT scan shows patchy GGO, with
visible vessels (asterisk). Interlobular septal
thickening can also be seen (yellow arrow).
b) The photomicrograph shows alveolar septal
thickening (star) and partial airspace filling by
macrophages and eosinophils (orange arrow).
The patient was a 32-year-old man with chronic
b a a
Dark bronchus sign.
HRCT scan shows diffuse ground-glass
attenuation with the dark bronchus
sign in a patient with nonspecific
interstitial pneumonia. .
Value of mIP reconstructions. Coronal HRCT scans and
mIP reformatted images showdiffuse GGO, predominant in
th iddl l ( t ) i ti t ith
mIP mIP
Results: Four groups were considered in the differential diagnosis of predominant GGO with a diffuse or patchy distribution. Two groups were considered in the differential diagnosis of predominant GGO with a
nodular distribution.
yp g g g
pneumonia.
arrows) and traction bronchiectasis (yellow arrows) in
a patient with idiopathic pulmonary fibrosis.
y
eosinophilic pneumonia.
the middle lung zones (stars) in a patient with
hypersensitivity pneumonitis.
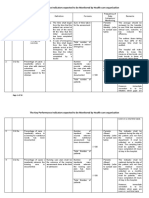
GROUND-GLASS OPACITY
PREDOMINANT PATTERN
PATCHY OR DIFFUSE NODULAR
PATCHY OR DIFFUSE GGO
WITHOUT FIBROSIS, ACUTE DISEASE (1)
Pulmonary oedema
Pulmonary haemorrhage
Neumocystis Jiroveci and viral pneumonias
Acute eosinophilic pneumonia
Radiation pneumonitis (acute phase)
NODULAR GGO
HOMOGENEOUS DISTRIBUTION (5)
Hypersensitivity pneumonitis
Respiratory bronchiolitis
Respiratory bronchiolitis/ILD
Siderosis
Dental technicians pneumoconiosis
Aluminum exposure
NON-HOMOGENEOUS (6)
PATCHY OR DIFFUSE NODULAR
WITHOUT FIBROSIS WITH FIBROSIS
ACUTE (1) SUBACUTE
OR CHRONIC (2)
HOMOGENEOUS (5)
ACUTE (3) SUBACUTE
OR CHRONIC (4)
Permeability pulmonary oedema: ATRA syndrome. Axial and
coronal volumetric HRCT scans show diffuse GGO with the dark
bronchus sign. The same areas show superimposed interlobular
septal thickening and intralobular lines (crazy-paving pattern)
(stars). The patient was a 40-year-old man with acute promyelocytic
l k i t t d ith t ti i id
PATCHY OR DIFFUSE GGO
WITH FIBROSIS ACUTE DISEASE (3)
Aluminum exposure
Respiratory bronchiolitis-
associated ILD: Axial
volumetric HRCT scan and
mIP coronal reformatted
mIP
PATCHY OR DIFFUSE GGO
WITH FIBROSIS
PATCHY OR DIFFUSE GGO
WITHOUT FIBROSIS
SUBACUTE-CHRONIC DISEASE
leukaemia treated with transretinoic acid.
NODULAR GGO
NON HOMOGENEOUS DISTRIBUTION
Infectious bronchiolitis
Pulmonary oedema
Pulmonary haemorrhage
NODULAR GGO
NON-HOMOGENEOUS DISTRIBUTION (6)
WITH FIBROSIS, ACUTE DISEASE (3)
Acute interstitial pneumonia
ARDS
images show centrilobular
nodular areas of GGO with a
homogeneous distribution
throughout both upper lung
zones (arrows). Diffuse GGO
in the lower lung zones can be
also observed. The patient was
smoker.
mIP
WITH FIBROSIS
SUBACUTE, CHRONIC DISEASE (4)
IIPs: Nonspecific interstitial pneumonia
Desquamative interstitial pneumonia
Idiopathic pulmonary fibrosis
Collagen vascular diseases
Hypersensitivity pneumonitis
Radiation pneumonitis (chronic phase)
I I
Hypersensitivity pneumonitis
IIPs: Respiratory bronquiolitis/ILD
Desquamative interstitial pneumonia
Cryptogenic organizing pneumonia
Lymphoid interstitial pneumonia
Collagen vascular diseases
PATCHY OR DIFFUSE GGO
WITHOUT FIBROSIS
SUBACUTE-CHRONIC DISEASE (2)
Vasculitis
Pulmonary haemorrhage
in a patient with right
pulmonary artery
agenesis and hipoplastic
right lung Axial HRCT
Acute interstitial pneumoni a. Axial HRCT scans show diffuse
bilateral GGO. Consolidations, reticular pattern (green arrow),
traction bronchiectasis (yellow arrow) and honeycombing (orange
arrow) are all evident in the posterior lung zones. Bilateral
pneumothorax and pneumomediastine can also be seen.
The photomicrograph
shows airspace filled with
proteinaceous exudate
(star). The alveolar septa
are thickened (arrow) by
fibroblastic tissue. Marked
hyperplasia of type II
pneumocytes can be
observed.
I
IP
E
Bronchoalveolar carcinoma
Chronic eosinophilic pneumonia
Alveolar proteinosis
Sarcoidosis
Expiration Inspiration
REFERENCES
1. Miller WTJ , Shah RM. Isolated diffuse ground-glass opacity in thoracic CT: causes
andclinical presentations. AJ R 2005;184:613-622.
2. Engeler CE, Tashjian J H, Trenkner SW, Walsh J W. Ground-glass opacity of the lung
parenchyma: a guide to analysis with high-resolution CT. AJ R 1993;160:249-251.
3. Collins J , Stern EJ . Ground-glass opacityat CT: theABCs. AJ R 1997;169:355-367.
4. Remy-J ardin M, Giraud F, RemyJ , Copin MC, Gosselin B, DuhamEL a. Importance of
CONCLUSIONS: The dark
bronchus sign and mIP
reconstructions help to detect and
quantify GGO.
Important criteria for narrowing
down the differential diagnosis are:
The predominance and distribution
right lung. Axial HRCT
scans show ill-defined
centrilobular and acinar
nodules (orange arrow)
with a non-homogeneous
distribution. Some patchy
GGO areas (green arrow )
can be observed.
Acute exacerbation of familial idiopathic pulmonary fibrosis.
Axial volumetric HRCT scans (I) and expiratory image (E) show
patchy GGO (green arrows) and crazy-paving pattern (yellow
arrows), irregular septal thickening (orange arrow), traction
bronchiectasis and honeycombing (blue arrow). Patchy air
trapping is also observed (star). Coronal volumetric HRCT scan
(C) and mIP reformatted image showbilateral, patchy air trapping
(predominant in left upper lobe) (star), patchy GGO (green arrow)
and peripheral bronchiectasis (white arrow), without predominant
basal distribution.
C
mIP
mIP
p
Hypersensiti vity
pneumonitis. Axial inspiratory
HRCT scans show patchy
GGO (mosaic attenuation),
predominantly involving the
upper and middle lung zones.
The expiratory HRCT scan
shows patchy air trapping
(star).
p
y , , y , p , , p
ground-glass attenuation in chronic diffuse infiltrative lung disease: pathologic-CT
correlation. Radiology1993;189:693-698.
5. American Thoracic Society; European Respiratory Society. The American Thoracic
Society/European Respiratory Society International multidisciplinary consensus
classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med
2002;165:227-304.
6. Beigelman-Aubry C, Hill C, Guibal A, Savatovsky J , Grenier PA. Multidetector rowCT
and postprocessing techniques in the assessment of diffuse lung disease. Radiographics
2005; 25:1639-1652.
7. Elliot T, Lynch DA, Newell J D J r, Cool C, Tuder R, Markopoulou K, Veve R, Brown K.
High-Resolution Computed Tomography features of nonspecific interstitial pneumonia
andusual interstitial pneumonia. J ComputAssist Tomogr 2005; 29(3):339-345.
8. Hansell DM. High-resolution CT of diffuse lung disease. Value and limitations. Radiol
ClinNAm2001; 39(6):1091-1113.
9. Gotway MB, ReddyGP, WebbWR, Elicker BM, Leung J WT. High-resolution CT of the
lungs: patterns of disease and differential diagnoses. Radiol Clin N Am 2005; 43:513-
542.
10. Nowers K, Rasband J D, Berges G, Gosselin M. Approach to ground-glass
opacificationof the lung. SeminUltrasound CT MRI 2002; 23(4):302-323.
11. Dalal PU, Hansell DM. High-resolution computed tomography of the lungs: the
borderlands of normality. Eur Radiol 2006; 16:771-780.
p
of GGO, the presence or absence
of fibrosis and clinical information.
Progressi ve systemic sclerosis: interstitial pneumonitis and
fibrosis. Axial volumetric HRCT scans and mIP images show
diffuse GGO with fibrosis: traction bronchiectasis (blue arrows) and
honeycombing (orange arrows), in a predominant basal
distribution.
mIP
Sarcoidosis stage II. Axial and coronal volumetric HRCT scans
show round and patchy GGO in the upper lung zones (yellow
arrow). A coronal Maximum Intensity Projection (MIP) image
shows small superimposed centrilobular and subpleural nodules
(orange arrow). Note the mediastinal and hiliar lymphadenopaties
(star).
MIP
You might also like
- Semi Comprehensive With Coil Amc - Air ConditionerDocument2 pagesSemi Comprehensive With Coil Amc - Air ConditionerRahul KashyapNo ratings yet
- Siemens CT Emotion Dual - 2003 (2 Slice) CT Scanner For SaleDocument1 pageSiemens CT Emotion Dual - 2003 (2 Slice) CT Scanner For SaleRahul KashyapNo ratings yet
- 12958-Brivo CT385 Tigre Bro - v16 12Pgs - 100nos 220GsMattDocument12 pages12958-Brivo CT385 Tigre Bro - v16 12Pgs - 100nos 220GsMattRahul KashyapNo ratings yet
- jnm046045 1920.Document3 pagesjnm046045 1920.Rahul KashyapNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 4020 Assessment 4 Instructions - Improvement Plan Tool Kit - ..Document4 pages4020 Assessment 4 Instructions - Improvement Plan Tool Kit - ..Sabahat BashirNo ratings yet
- Food Safety 3Document22 pagesFood Safety 3Syarahdita Fransiska RaniNo ratings yet
- Assessed Conference Presentations ScheduleDocument2 pagesAssessed Conference Presentations ScheduleAna Maria Uribe AguirreNo ratings yet
- A Medical Outreach Elective CourseDocument11 pagesA Medical Outreach Elective CourseRobert SmithNo ratings yet
- Function: What Is The Skeletal System?Document6 pagesFunction: What Is The Skeletal System?Mr. Christian ParabuacNo ratings yet
- Introduction To Public Health... 1stDocument37 pagesIntroduction To Public Health... 1stNELSONJD20195100% (3)
- Research Paper About EpilepsyDocument4 pagesResearch Paper About EpilepsyHazel Anne Joyce Antonio100% (1)
- Lester Desjarlais Inquest Parts I and IIDocument108 pagesLester Desjarlais Inquest Parts I and IIJames Turner100% (1)
- VetcareDocument18 pagesVetcareMy binNo ratings yet
- OPD Network ListDocument354 pagesOPD Network ListSHAIKH ABDUL AZIZ salim bashaNo ratings yet
- Week 4-Physical Fitness TestDocument38 pagesWeek 4-Physical Fitness TestCatherine Sagario OliquinoNo ratings yet
- Symbols On PackegingDocument3 pagesSymbols On PackegingsakibarsNo ratings yet
- Digestive System PowerpointDocument33 pagesDigestive System PowerpointThomas41767% (6)
- College of Physicians and Surgeons of Alberta QB1803-01472 Certified Record of Proceedings - Illegal sabotage of Alberta Cancer Therapy Programs and abuse (physical violence, harassment, verbal abuse) of frontline healthcare staff by Alberta NDP and their AHS and CPSA Officials, covered-up by CPSADocument908 pagesCollege of Physicians and Surgeons of Alberta QB1803-01472 Certified Record of Proceedings - Illegal sabotage of Alberta Cancer Therapy Programs and abuse (physical violence, harassment, verbal abuse) of frontline healthcare staff by Alberta NDP and their AHS and CPSA Officials, covered-up by CPSAWilliam MakisNo ratings yet
- Remote Working A Dream Job British English Advanced c1 c2 GroupDocument5 pagesRemote Working A Dream Job British English Advanced c1 c2 GroupNick ManishevNo ratings yet
- Hazard Identification Risk Assessment Risk ControlDocument3 pagesHazard Identification Risk Assessment Risk Controle cubeNo ratings yet
- Practical Research 2 Quarter 1 Activity SheetsDocument8 pagesPractical Research 2 Quarter 1 Activity SheetsJonnis Estillore100% (1)
- Laboratory Hygiene and SafetyDocument34 pagesLaboratory Hygiene and SafetyResmiNo ratings yet
- Dowtherm TDocument3 pagesDowtherm Tthehoang12310No ratings yet
- Oet Reading Part A Additional - GlucomaDocument8 pagesOet Reading Part A Additional - Glucomaafacean25% (8)
- The Cell Cycle and Cancer WorksheetDocument3 pagesThe Cell Cycle and Cancer WorksheetAngie Pyatt KarrakerNo ratings yet
- NCP Gastric CancerDocument7 pagesNCP Gastric CancerAnonymous XvwKtnSrMR100% (4)
- MDR Guideline Medical Devices LabelingDocument7 pagesMDR Guideline Medical Devices Labelingarade43100% (1)
- Incident Reports 2017-2019Document8 pagesIncident Reports 2017-2019Buddzilla FranciscoNo ratings yet
- KPI - Foruth EditionDocument30 pagesKPI - Foruth EditionAnonymous qUra8Vr0SNo ratings yet
- Come Back To Your Senses Use Your Body: Psychologyt LsDocument1 pageCome Back To Your Senses Use Your Body: Psychologyt LsMarina Moran100% (1)
- Mindvalley - Superbrain Quest - SummaryDocument17 pagesMindvalley - Superbrain Quest - SummaryMagdy El ID100% (3)
- Biology 3rd ESO Full DossierDocument54 pagesBiology 3rd ESO Full DossierNinaNo ratings yet
- Brett Stolberg 100112479 - ResumeDocument1 pageBrett Stolberg 100112479 - Resumeapi-193834982No ratings yet
- Anthrax (Woolsesters Disease, Malignant Edema) What Is Anthrax?Document3 pagesAnthrax (Woolsesters Disease, Malignant Edema) What Is Anthrax?rvanguardiaNo ratings yet