Professional Documents
Culture Documents
Syok Septik Guidline PD Bayi Anak
Uploaded by
rantiadrianiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Syok Septik Guidline PD Bayi Anak
Uploaded by
rantiadrianiCopyright:
Available Formats
Clinical Pearls for the Crashing Pediatric Patient
Mimi Lu, MD
Clinical Assistant Professor
Department of Emergency Medicine
University of Maryland School of Medicine
Director, Pediatric Emergency Medicine Education
mlu@umaryland.edu
Objectives:
1. Define clinical manifestations of early shock in the pediatric patient.
2. Recognize new trends in pediatric resuscitation.
3. Discuss the new changes made to the pediatric resuscitation guidelines.
Definition
Shock develops when systemic oxygen and nutrient supply become inadequate to meet the
metabolic demands of the bodys organ systems.
Compensated shock
Decompensated shock
Irreversible shock
Pediatric Shock
1) Distributive
e. Septic
i. Antibiotics, IVF
f. Anaphylactic
i. Home-remedies
ii. Formula
g. Neurogenic
i. Seizure
ii. (Non-accidental) Trauma
2) Cardiogenic
e. Heart lesion
i. Obstructive
ii. Cyanotic
1. Hyperoxia test
iii. Prostaglandin
f. Anomalous coronary artery
i. EKG
g. Supraventricular tachycardia (SVT)
3) Hypovolemic
e. Blood loss
i. 10 ml/kg PRBC
f. Fluid loss
i. 10-20 ml/kg normal saline bolus
4) Obstructive
e. Malrotation with volvulus
f. Diaphragmatic hernia
g. Necrotizing enterocolitis
5) Endocrine/ metabolic
e. Congenital adrenal hyperplasia (CAH)
i. Low sodium, high potassium
ii. Hydrocortisone
f. Glucose!!!
i. Rule of 50
g. Inborn error or metabolism
i. Glucose
ii. Lactate
iii. Ammonia
iv. Ketonuria
Ttrauma,nonaccidentaltrauma
Hheartdisease,hypovolemia,hypoxia
Eendocrine(CAH,thyrotoxicosis)
Mmetabolic
Iinbornerrorsofmetabolism
Ssepsis
Fformula(dilutionorconcentration)
Iintestinalcatastrophies
Ttoxins
Sseizures
Pediatric shock: early recognition and management
a. Airway
i. Cuffed tubes okay!
ii. ETT size: (Age/4) +4, decrease by size if using cuffed
Anatomy
Infant Adult
Tongue Relatively large, intraoral Normal
Epiglottis Floppy, anterior, cephalad Firm
Vocal cord angle Inclined Flat
Glottis C3 level C5-C6 level
Cricothyroid Membrane Small, narrowest point Normal
Trachea Small, short, collapsible Large, stationary
b. Breathing
i. Measure RR over 30 seconds
ii. Increase temp by 1C =increase RR by 2-5
Age adjusted rates
Age RR
Infant 30-60
Toddler 24-40
Preschooler 22-34
School-aged 18-30
Adolescent 12-16
c. Circulation
v. (Age x 2) +90 =median 50% percentile for SBP
vi. Early use of intraosseous access
vii. NS bolus (20 ml/kg) EXCEPT neonates or congenital cardiac (10 ml/kg)
viii. PRBC/ FFP 10 ml/kg (5 ml/kg in neonates)
d. Dextrose!!! All ill-appearing infants are hypoglycemic until proved otherwise!
i. Rule of 50-100
1. D
10
5-10 ml/kg (age <1 year)
2. D
25
2-4 ml/kg (age 1 8 year)
3. D
50
1-2 ml/kg (age >8 year)
<60
<30
<15
e. Vital signs
i. Always measure in kilograms!!!
Newborns
Brierley J , Carcillo J A, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and
neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009
Feb;37(2):666-88.
Infants and Children
Brierley J , Carcillo J A, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and
neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009
Feb;37(2):666-88.
SIRS: Age-specific vital signs and laboratory values
Age group Tachycardia Bradycardia Respiratory
rate
WBC
x 10
3
/mm
3
Systolic BP
mmHg
Newborn >180 <100 >50 >34 <65
Neonate >180 <100 >40 >19.5 or <5 <75
Infant >180 <90 >34 >17.5 or <5 <100
Toddler >140 - >22 >15.5 or <6 <94
Child >130 - >18 >13.5 or <4.5 <105
Adolescent >110 - >14 >11 or <4.5 <117
Table 3. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in
pediatrics. Goldstein B, Giroir B, Randolph A; International Consensus Conference on Pediatric Sepsis. Pediatr Crit
Care Med. 2005 J an;6(1):2-8.
Therapies adults and children with septic shock
Therapy Children Adults
Volume Usually need more fluid, up to and
over 60 ml/kg
Fluid resuscitation to CVP 12
Antibiotics Early initiation of appropriate
antibiotics within 1 hour
Early initiation of appropriate
antibiotics within 1 hour
Inotropes and vasopressors First line peripheral epinephrine cold
shock, transition to central when able.
Central norepinephrine for warm
shock
First line norepinephrine
dobutamine
Vasopressin for warm shock
Vasodilators Use for pulmonary hypertension
Low CO, high SVR shock
No role
Tight glycemic control Unresolved Harmful
ECMO Survival 80% neonates, 50% children Evolving H1N1 popularizing use
Inhaled NO Neonates with RV failure No role
Hydrocortisone Absolute adrenal insufficiency only;
post ACTH cortisol level <18 g/dL
or baseline <5 g/dL
Use if continue on vasopressors
regardless of adrenal status
Reprinted with permission from Marianne Gausche-Hill, MD
Pediatric Basic Life Support
Change in sequence C-A-B
Eliminated look, listen and feel to assess breathing after opening airway
Lay rescuers: check for response of abnormal breathing (eliminate pulse check)
Health care providers: allows 10 sec for pulse check
o 30 compressions followed by 2 breaths (lone rescuer)
o 15:2 if two providers
Push hard, push fast at least 100 per minute, allowing recoil of chest
o Infant chest compression 1.5 in (4 cm)
o Children 2 in (5 cm)
Defibrillation
o Manual defibrillator >AED with dose attenuator >AED without dose attenuator
o 2-4 J /kg, followed by at least 4 J /kg, up to 10 J /kg
Pediatric Advanced Life Support
BVM recommended over ETI for out-of-hospital setting
o Experienced providers may use LMAs
Cricoid pressure NOT recommended
Cuffed tubes okay!
o Uncuffed: (age/4) +4 =mm ID
o Cuffed: (age/4) +3.5 =mm ID
Capnography recommended to confirm ETT placement and assess adequacy of CPR
Avoid excessive ventilation (8-10 breaths per minute)
Oxygen increasing evidence for harm, especially in neonates
o Avoid hyperoxemia
o Start with 100% O
2
then titrate to maintain SpO
2
>94%
Medications
o Addition of procainamide as possible therapy for refractory SVT
o Routine calcium administration NOT recommended unless clear indication
o Etomidate may be used for RSI but NOT recommended in septic shock
o Atropine may be added for symptomatic bradycardia but not cardio-pulmonary
arrest
Wide-complex tachycardia present of QRS width >0.09 sec
Post-arrest Care
o Therapeutic hypothermia may be considered in children with ROSC (large trial
underway)
Family presence during resuscitation is recommended
New topics:
o Specific guidance for cardiac arrest in infants with single-ventricle anatomy,
Fontan or hemi-Fontan/ bidirectional Glenn physiology and pulmonary
hypertension
o Autopsies recommended for young victims of sudden cardiac arrest
Neonatal resuscitation
Maintain A-B-C sequence
De-emphasis on peripartum suctioning
ET suctioning for nonvigorous neonate in meconium-stained fluid.
Vigorous newborns do not require ET suctioning of meconium regardless of how thick
the meconium is.
Determine degree of oxygenation by pulse ox on the right wrist or arm
Term babies should be resuscitated with room air first, then supplemental oxygen if
needed by blended oxygen-air delivery
o If bradycardic after 90 sec of resuscitation, increased oxygen to 100%
Start CPR for HR <60 bpm despite assisted ventilation for 30 seconds.
Preferred method is thumb-hand technique.
Compression:ventilation ratio 3:1 (90 compressions with 30 ventilations per cycle)
Infants >36 weeks with moderate to severe hypoxic-ischemic encephalopathy should be
offered therapeutic hypothermia
Adults/
Adolescents
Infants/
Children
Neonates
Sequence C-A-B C-A-B A-B-C
Compression rate (bpm) 100 100 90:30 events/min
Depth >2 inches 1.5-2 inches 1/3 AP diameter
Compression:ventilation ratio
1 rescuer
2 rescuers
30:2
30:2
30:2
15:2
3:1
3:1
Pause for ventilation after
intubation?
No No Yes
Key references:
1. Brierley J , Carcillo J A, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and
neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009
Feb;37(2):666-88.
2. Goldstein B, Giroir B, Randolph A, et al. International pediatric sepsis consensus conference: definitions for sepsis and
organ dysfunction in pediatrics. International Consensus Conference on Pediatric Sepsis. Pediatr Crit Care Med. 2005
J an;6(1):2-8.
3. Arikan AA, Citak A. Pediatric shock: review. Signa Vitae. 2008; 3(1):13-23.
4. Dellinger RP, Levy MM, Carlet J M, et al. Surviving Sepsis Campaign: international guidelines for management of
severe sepsis and septic shock: 2008. Crit Care Med 2008;36:296-327.
5. Kleinman ME, Chameides L, Schexnayder SM, et al. Part 14: pediatric advanced life support: 2010 American Heart
Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010
Nov 2;122(18 Suppl 3):S876-908.
6. Berg MD, Schexnayder SM, Chameides L, et al. Part 13: pediatric basic life support: 2010 American Heart Association
Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010 Nov 2;122(18
Suppl 3):S862-75.
7. Kattwinkel J , Perlman J M, Aziz K, et al. Part 15: neonatal resuscitation: 2010 American Heart Association Guidelines
for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010 Nov 2;122(18 Suppl
3):S909-19.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
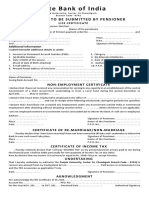
- SBI - Certificate To Be Submitted by Pensioner - ChandigarhDocument1 pageSBI - Certificate To Be Submitted by Pensioner - ChandigarhMsinghNo ratings yet
- Navajo Hearing ProgramDocument3 pagesNavajo Hearing Programjamesmith100000% (1)
- Peugeot 206 Fuse Diagram PDFDocument6 pagesPeugeot 206 Fuse Diagram PDFDedi dwi susanto100% (2)
- Objection HandlingDocument3 pagesObjection HandlingNabin GaraiNo ratings yet
- ASTM IndexDocument34 pagesASTM IndexJimmy Chan67% (3)
- Isolation and Characterization of Galactomannan From Sugar PalmDocument4 pagesIsolation and Characterization of Galactomannan From Sugar PalmRafaél Berroya Navárro100% (1)
- Break Free - Nathaniel BrandenDocument16 pagesBreak Free - Nathaniel Brandennbckudxtkudkuf50% (2)
- Inspection and Test Plan: Flow Chart Start IncomingDocument1 pageInspection and Test Plan: Flow Chart Start IncomingSinden AyuNo ratings yet
- Aslmualaikum WR WBDocument6 pagesAslmualaikum WR WBrantiadrianiNo ratings yet
- Rajapakse Dengue ShockDocument9 pagesRajapakse Dengue ShockrantiadrianiNo ratings yet
- AbstractDocument10 pagesAbstractrantiadrianiNo ratings yet
- Practice Tracing D PrekDocument1 pagePractice Tracing D PrekrantiadrianiNo ratings yet
- Pang Imunopathogenesis Dss PDFDocument3 pagesPang Imunopathogenesis Dss PDFrantiadrianiNo ratings yet
- GipsDocument13 pagesGipsrantiadrianiNo ratings yet
- Handbook: For Clinical Management of DengueDocument124 pagesHandbook: For Clinical Management of DengueraattaiNo ratings yet
- Practice Tracing e PrekDocument1 pagePractice Tracing e PrekrantiadrianiNo ratings yet
- Preterm Birth - WHO RecommendationDocument108 pagesPreterm Birth - WHO RecommendationBonifacius Bayu Erlangga KusumaNo ratings yet
- Practice Tracing B Prek PDFDocument1 pagePractice Tracing B Prek PDFrantiadrianiNo ratings yet
- Learn to Write the Letter C with Curved LinesDocument1 pageLearn to Write the Letter C with Curved LinesrantiadrianiNo ratings yet
- Daftar Pustaka Sepsis Tugas UjianDocument2 pagesDaftar Pustaka Sepsis Tugas UjianrantiadrianiNo ratings yet
- Managing Immune Thrombocytopenic Purpura: An UpdateDocument7 pagesManaging Immune Thrombocytopenic Purpura: An UpdateApriliza RalasatiNo ratings yet
- Practice Tracing B Prek PDFDocument1 pagePractice Tracing B Prek PDFrantiadrianiNo ratings yet
- MRI in MTDocument13 pagesMRI in MTrantiadrianiNo ratings yet
- YUVARAJAN-DeNGUE Pulmonal ComplicationDocument6 pagesYUVARAJAN-DeNGUE Pulmonal ComplicationrantiadrianiNo ratings yet
- Daftar Pustaka RadiologiDocument1 pageDaftar Pustaka RadiologirantiadrianiNo ratings yet
- 6 PDFDocument5 pages6 PDFUgaugaaNo ratings yet
- GipsDocument13 pagesGipsrantiadrianiNo ratings yet
- European ConsensusDocument19 pagesEuropean ConsensusEdgar Quelex VicenteNo ratings yet
- Eficacy Surfactant 2016Document13 pagesEficacy Surfactant 2016rantiadrianiNo ratings yet
- A Dede Ji 422017 Aj Mah 32627Document9 pagesA Dede Ji 422017 Aj Mah 32627rantiadrianiNo ratings yet
- Pang Imunopathogenesis Dss PDFDocument3 pagesPang Imunopathogenesis Dss PDFrantiadrianiNo ratings yet
- Cardiac Anomali ResearchDocument5 pagesCardiac Anomali ResearchrantiadrianiNo ratings yet
- Shock Risk FactorDocument4 pagesShock Risk FactorrantiadrianiNo ratings yet
- Handbook: For Clinical Management of DengueDocument124 pagesHandbook: For Clinical Management of DengueraattaiNo ratings yet
- Devarajan, Dss DGN ArdsDocument4 pagesDevarajan, Dss DGN ArdsrantiadrianiNo ratings yet
- Hematologic Scoring for Early Neonatal Sepsis DiagnosisDocument5 pagesHematologic Scoring for Early Neonatal Sepsis DiagnosisrantiadrianiNo ratings yet
- Clinical Presenyation Dengue in ChildrenDocument4 pagesClinical Presenyation Dengue in ChildrenrantiadrianiNo ratings yet
- Role of Hematologic Scoring System in Early Diagnosis of Neonatal SepticemiaDocument6 pagesRole of Hematologic Scoring System in Early Diagnosis of Neonatal SepticemiarantiadrianiNo ratings yet
- Eltra Cs 530Document122 pagesEltra Cs 530ahalonsoNo ratings yet
- Batson Et All - 2007 - Anger and Unfairness - Is It Moral Outrage?Document15 pagesBatson Et All - 2007 - Anger and Unfairness - Is It Moral Outrage?Julia GonzalezNo ratings yet
- Jeffrey Ansloos - Indigenous Peoples and Professional Training in Psychology in CanadaDocument17 pagesJeffrey Ansloos - Indigenous Peoples and Professional Training in Psychology in CanadaleoNo ratings yet
- Introduction To Integrative Homeopathy - Bob LeckridgeDocument16 pagesIntroduction To Integrative Homeopathy - Bob LeckridgeBob LeckridgeNo ratings yet
- Acute Coronary Syndrome Guidelines 2020Document79 pagesAcute Coronary Syndrome Guidelines 2020Γιώργος ΕλευθεριάδηςNo ratings yet
- Regional Ecology Test ScoringDocument14 pagesRegional Ecology Test Scoringaisyah Wardah201No ratings yet
- EMI InstructionsDocument2 pagesEMI InstructionsAKSHAY ANANDNo ratings yet
- The Role of Play Therapists in Children's Transitions: From Residential Care To Foster CareDocument11 pagesThe Role of Play Therapists in Children's Transitions: From Residential Care To Foster Caresherry_hoang_1No ratings yet
- NMC Confirmation FormDocument3 pagesNMC Confirmation FormGianina AvasiloaieNo ratings yet
- Buhos SummaryDocument1 pageBuhos Summaryclarissa abigail mandocdocNo ratings yet
- Edna Adan University ThesisDocument29 pagesEdna Adan University ThesisAbdi KhadarNo ratings yet
- Mri 7 TeslaDocument12 pagesMri 7 TeslaJEAN FELLIPE BARROSNo ratings yet
- Indg 449Document12 pagesIndg 449Nissam SidheeqNo ratings yet
- Marital Satisfaction in Dual Earner FamilyDocument4 pagesMarital Satisfaction in Dual Earner FamilyInternational Organization of Scientific Research (IOSR)No ratings yet
- Borri Ups b9000 Ups Service Manual - CompressDocument180 pagesBorri Ups b9000 Ups Service Manual - CompressArun SNo ratings yet
- Bibie Evana OsmanDocument6 pagesBibie Evana OsmanStabat Jaya TrademarkNo ratings yet
- Rise School of Accountancy Test 08Document5 pagesRise School of Accountancy Test 08iamneonkingNo ratings yet
- Partial Defoliation of Vitis Vinifera L. Cv. Cabernet SauvignonDocument9 pagesPartial Defoliation of Vitis Vinifera L. Cv. Cabernet Sauvignon1ab4cNo ratings yet
- Sampling & Data AssayDocument22 pagesSampling & Data AssayFerdinand SiahaanNo ratings yet
- Cement Evaluation CAST-CBL HalliburtonDocument36 pagesCement Evaluation CAST-CBL HalliburtonrezaNo ratings yet
- Final TLE9 Nail Care9 Q1 Module 3Document20 pagesFinal TLE9 Nail Care9 Q1 Module 3Ma. Andrea LagmanNo ratings yet
- Experiment Report Basic Physics "Total Internal Reflection"Document10 pagesExperiment Report Basic Physics "Total Internal Reflection"dita wulanNo ratings yet