Professional Documents
Culture Documents
Anatomy and Physiology of The Conducting System
Uploaded by
Francesca Li0 ratings0% found this document useful (0 votes)
26 views5 pagesAnatomy of cardiac myocytes and physiology of conduction in the heart
Original Title
Anatomy and Physiology of the Conducting System
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAnatomy of cardiac myocytes and physiology of conduction in the heart
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
26 views5 pagesAnatomy and Physiology of The Conducting System
Uploaded by
Francesca LiAnatomy of cardiac myocytes and physiology of conduction in the heart
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
The anatomy and physiology of the conducting system
(including the central mechanisms controlling cardiac rate)
Anatomy
The myocardium is made up of cardiac muscles cells called myocytes.
These cells connect to adjacent cells via a membrane known as the intercalated disc.
This provides both structural support (via desmosomes) and electrical connection to pass
between the neighbouring cells through gap junctions.
The myocytes contain a large number of mitochondria, which provides ATP for the contractile
function to occur.
Myocytes are able to contract due to the action of specialised contractile proteins that are
arranged in organised structural units known as sarcomeres.
Each sarcomere is made up of thick and thin filaments
Thick filaments are mainly composed of myosin molecules
Thin filaments are mainly composed of actin subunits that are arranged in a double helix
(tropomyosin and troponin)
Sarcomeres also consist of M lines, Z discs and the A, H and I bands.
The myocytes cell membrane is known as the sarcolemma it has a specialised structure with
long transverse tubules (T tubules) that extend between myofibrils that facilitates rapid
calcium influx during depolarisation.
His-Purkinje system (bundle of His) are other specialised cells found in the myocardium. They
are involved with rapid transmission of electrical signals through the heart
T tubules and sarcoplasmic reticulum (SR) is similar the ones of the skeletal muscles but in
skeletal muscles, the T tubules are wider and less common and the SR is less well developed.
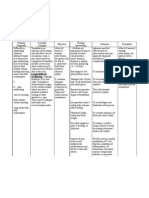
Electrical Conducting System Anatomy
Specialised cardiac myocytes form the conducting system of the heart and are localised to specific
regions. They initiate the normal cardiac cycle and co-ordinate the contractions of the cardiac
chambers.
1. The sinoatrial node is the
pacemaker of the heart, located at
the junction of the superior vena
cava and right atrium in the upper
part of the crista terminalis.
2. It is thought that there are 3 intra-
atrial pathways.
(These groups of internodal tissue
are better referred to as
internodal atrial myocardium (not
tracts) as they do not appear to be
histologically discrete specialised
tracts)
a. Anterior internodal
pathway
b. Middle internodal tract
c. Posterior internodal tract
The anterior internodal pathway begins at the anterior margin of the SAN and curves anterior
around the SVC to enter the anterior interatrial band called the Bachmann bundles. This band
continues down to the left atrium with the anterior internodal pathway ending at the superior
margin of the AVN.
The middle internodal tract begins at the superior and posterior margins of the SAN, travels
behind the SVC to the crest of the interatrial septum and decends in the interatrial septum to the
superior margin of the AVN.
The posterior internodal tract starts at the posterior margin of the sinus node and travels
posteriorly around the SVC and along the crista terminalis to the eustacian ride and then into the
interatrial septum above the coronary sinus where it joins the posterior part of the AVN.
3. The cardiac impulse then propagates across both atria to the atrioventricular node. Which is
located at the base of the right atrium just above the septal cusp of the tricuspid valve. This is the
only electrical connection with the ventricles due to the interposition of the fibrous
atrioventricular rings that restrict impulses from travelling straight from the atria to the ventricles.
4. The bundle of His descends from the atrioventricular node down the membraneous
intraventricular septum to the muscular septum where it divides into the left and right branches.
The left branch divides into anterior and posterior fascicles.
5. The terminal Purkinje fibres then distribute the cardiac impulse almost simultaneously to the
endocardium of the entire left and right ventricles.
Physiology
Contraction
During excitation-contraction coupling
(ECC) a series of processes occur for an
action potential to occur, triggering the
myocyte to contract.
Cardiac contraction when there is a
depolarization of the cell membrane
(Phase A).
This occurs when there is a rise in Ca
2+
concentration inside the myocyte. The
contraction of the myocytes is triggered
by action potentials that run across the
surface of the myocytes down the T
tubules.
These are mediated by voltage-
dependent sodium channels that allow sodium influx to produce depolarization.
This triggers calcium entry into the cytoplasm in two ways:
In the sarcolemma (especially in T tubules) there are voltage-sensitive calcium channels that
are sensitive to a group of drugs known as dihydropyridines; so these calcium channels are
known as L-type calcium channels. These channels open at a slower rate than sodium channels
and they produce a sustained depolarization known as the plateau phase of the action
potential.
Some calcium that enters through the through the L-type calcium channel binds to receptors
on the SR known as ryanodine receptors. This releases calcium from the SR my a process
known as calcium-induced calcium release. This process accounts for 80% of calcium required
for muscle contraction.
The calcium inside the myocyte interacts with troponin C in a similar way to that of a skeletal muscle
to cause muscle contraction.
Relaxation
The repolarization of the action potential is caused by the opening of potassium channels that
allows potassium efflux to return the membrane potential to its resting level.
The sodium channels are inactive until the resting membrane potential is restored.
The myocyte cannot be re-excited until after the refractory period.
This ensures that each heart beat is separate from the previous one and that there is enough
blood to refill the heart again.
Calcium has to be removed from the cytoplasm and this occurs by two types of calcium
transporter:
o Calcium-ATPase located on the SR and plasma membrane, returning about 80% of
calcium into the SR and remove a small amount from the cell
o Na
+
/Ca
2+
cotransporters on the plasma membrane that removes excess calcium in exchange
for sodium.
Change in the contractility of cardiac muscle are known as ionotropic effects
Drugs can affect the contractility of the cardiac muscle and do so by changing the levels of
intracellular calcium levels.
Some endocrine and renal disorders can change the plasma concentrations of potassium and
calcium which can affect the cardiac action potential
E
Phase A, B, C, D, E can also be commonly
written as Phase 0, 1, 2, 3, 4.
Cardiac Conducting System and the Central Mechanisms Controlling Cardiac Rate
The co-ordinated contraction of the heart is due to an action potential that is initiated at one region
of the heart, which is then conducted through a specialised, conducting system.
Cardiac myoctes are known to have a property known as autorhythmicity, which means they can
spontaneously fire action potentials in a regular pattern without the need for nervous inputs
(therefore cardiac contraction is known to be myogenic).
The most important place that this occurs is at the sinoatrial node. The SA node is normally
responsible for the initial depolarization and subsequent contraction of the whole heart. This is
because the rate of firing is higher than other areas in the heart. The resting membrane potential is
usually -60mV which is much less polarized than normal ventricular myocytes (-90mV). This means
that the SA node myocytes are unstable and is likely to drift towards the threshold for firing an action
potential, which is about -40mV.
The SA node has this ability
(pacemaker potential) due to the
action of different populations of
ion channels in these cells. The SA
node myocytes have both sodium
and calcium channels that allow
slow, inward, background currents
to gradually depolarize the cells.
At the same time the background
potassium current is reduced, this
increases the net depolarization
until the threshold is reached. These cells do not have any voltage-dependent sodium channels so the
depolarisation phase of the action potential is exclusively due to the influx of calcium (compared to
neurons which need voltage-dependent sodium channels for depolarisation to occur).
The gradient of the pacemaker potential determines the rate of firing of the SA node cells this
pattern is known as the sinus rhythm (the normal rhythm of the heart).
Increased gradient = increased rate
Decreased gradient = decreased rate
The SA node normally fires at about 100 times per min, but the normal resting heart rate is about
70bpm. This is because there is the influence of the autonomic nervous system that reduces the
resting rate.
Chronotropic effects are changes in the heart rate.
Many drugs can affect the heart rate and does this by changing the gradient of the pacemaker
potential.
Watch - https://www.youtube.com/watch?v=rIVCuC-Etc0
References
Medical Sciences - Naish
Cardiology (An illustrated colour text)
Anatomy of conducting system - http://emedicine.medscape.com/article/1922987-overview
You might also like
- Pathogenesis of Micro and Macrovascular Complications of DiabetesDocument4 pagesPathogenesis of Micro and Macrovascular Complications of DiabetesFrancesca LiNo ratings yet
- Haematinic DeficienciesDocument7 pagesHaematinic DeficienciesFrancesca Li100% (1)
- FBC Interpretation and Function of Blood ComponentsDocument7 pagesFBC Interpretation and Function of Blood ComponentsFrancesca LiNo ratings yet
- Skin DiagramDocument1 pageSkin DiagramFrancesca LiNo ratings yet
- Syncope and ShockDocument2 pagesSyncope and ShockFrancesca LiNo ratings yet
- Clotting Cascade SimplifiedDocument1 pageClotting Cascade SimplifiedFrancesca LiNo ratings yet
- Peripheral Vascular Disease Investigations and Stroke MimicsDocument4 pagesPeripheral Vascular Disease Investigations and Stroke MimicsFrancesca LiNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- CBSE Class 10 Life Processes QuestionsDocument5 pagesCBSE Class 10 Life Processes QuestionsDeepakNo ratings yet
- The Australian Water BuffaloDocument148 pagesThe Australian Water BuffaloFirah MagfirahNo ratings yet
- 10 MOST POPULAR DOGS Doberman PinscherDocument5 pages10 MOST POPULAR DOGS Doberman PinscherMunnau Norman BenNo ratings yet
- 2ND Period 1 PDFDocument2 pages2ND Period 1 PDFRëönärüdö KmpöNo ratings yet
- Document 3Document2 pagesDocument 3Berta EliesNo ratings yet
- Biology ProjectDocument17 pagesBiology ProjectsahilkalraksNo ratings yet
- Full Download Test-Bank-For-Chemistry-12th-0321907140-9780321907141 PDF Full ChapterDocument36 pagesFull Download Test-Bank-For-Chemistry-12th-0321907140-9780321907141 PDF Full Chapterputvicaragewt788100% (17)
- AP Animal Husbandry Assistant Syllabus 2023Document4 pagesAP Animal Husbandry Assistant Syllabus 2023Shaik WazeedNo ratings yet
- Basic Life Support: BLS For Healthcare Providers and Professional RescuersDocument15 pagesBasic Life Support: BLS For Healthcare Providers and Professional RescuersRaja FadhilNo ratings yet
- Congenital AnomaliesDocument22 pagesCongenital Anomaliesjessy100% (1)
- ARDS Berlin Definition UpdateDocument43 pagesARDS Berlin Definition UpdateAgnes Pritama Fahmi100% (1)
- SuturingDocument40 pagesSuturingAldora OktavianaNo ratings yet
- The Mirror Neuron System: Luigi Cattaneo, MD Giacomo Rizzolatti, MDDocument4 pagesThe Mirror Neuron System: Luigi Cattaneo, MD Giacomo Rizzolatti, MDBigBoostingNo ratings yet
- Parvovirus Infection Diagnostic and Therapy Diagnosticul Si Terapia in Infectii Cu Parvovirus La Caini Vaccinati.Document1 pageParvovirus Infection Diagnostic and Therapy Diagnosticul Si Terapia in Infectii Cu Parvovirus La Caini Vaccinati.Dr. Dragos CobzariuNo ratings yet
- Lung AnatomyDocument16 pagesLung AnatomywhyseejoshNo ratings yet
- ICAR JRF/SRF Exam Question Bank for Veterinary StudentsDocument281 pagesICAR JRF/SRF Exam Question Bank for Veterinary StudentsHarish ShindeNo ratings yet
- Medical MnemonicsDocument140 pagesMedical Mnemonicsmir-medicina100% (1)
- Occlusal RadiologyDocument15 pagesOcclusal RadiologySharlene OngNo ratings yet
- Visitors Health Check List: TemperatureDocument1 pageVisitors Health Check List: TemperatureSterben ShouchiNo ratings yet
- HIV AIDS Planning Checklist Sheet1 and Sheet2Document16 pagesHIV AIDS Planning Checklist Sheet1 and Sheet2佐々木 隆典No ratings yet
- Phonetics and PhonologyDocument34 pagesPhonetics and PhonologyFaith Clavaton Morales50% (2)
- Cow Rearing - 19Document47 pagesCow Rearing - 19Imran KhanNo ratings yet
- Difficulty in SwallowingDocument1 pageDifficulty in SwallowingmawelNo ratings yet
- Importance of Zoology - Understanding Animals & Their Role in NatureDocument16 pagesImportance of Zoology - Understanding Animals & Their Role in NatureSaad Akram Chaudhry100% (1)
- Biomechanics Pronation SupinationDocument10 pagesBiomechanics Pronation SupinationProfesseur Christian DumontierNo ratings yet
- Accelerated Orthodontics A ReviewDocument9 pagesAccelerated Orthodontics A ReviewvijayprabugNo ratings yet
- Triage Lecture DR F Mesa GaerlanDocument55 pagesTriage Lecture DR F Mesa Gaerlanapi-19431894100% (1)
- Black Cobra Tablets in PakistanDocument3 pagesBlack Cobra Tablets in PakistanBlack Cobra Tablets in PakistanNo ratings yet
- 452l Simulation 6 Pre SimulationDocument9 pages452l Simulation 6 Pre Simulationapi-307439819No ratings yet
- MalariaDocument5 pagesMalariaRina KhazarenNo ratings yet