Professional Documents
Culture Documents
Gambaran Patologis Pada Otoskopi Telinga, Hidung, Tenggorok
Uploaded by
Merlein Uviarty0 ratings0% found this document useful (0 votes)
38 views7 pagesGranulation tissue is found in the meatus infected with Pseudomonas and anaerobic organisms. If uncontrolled, the condition may be fatal. "Malignant" indicates the serious clinical nature.
Original Description:
Original Title
Gambaran Patologis Pada Otoskopi Telinga, Hidung,Tenggorok
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentGranulation tissue is found in the meatus infected with Pseudomonas and anaerobic organisms. If uncontrolled, the condition may be fatal. "Malignant" indicates the serious clinical nature.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
38 views7 pagesGambaran Patologis Pada Otoskopi Telinga, Hidung, Tenggorok
Uploaded by
Merlein UviartyGranulation tissue is found in the meatus infected with Pseudomonas and anaerobic organisms. If uncontrolled, the condition may be fatal. "Malignant" indicates the serious clinical nature.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 7
1
Gambaran Patologis Pada Telinga
Malignant Otitis Externa
Malignant otitis externa is a rare and serious form of otitis externa to which elderly
diabetics are particularly susceptible. Granulation
tissue is found in the meatus infected with
Pseudomonas and anaerobic organisms. This
granulation tissue tends to erode deeply, involving
the middle and inner ear, the bone of the skull base
with extension to the brain, and also the great vessels
of the neck. If uncontrolled, the condition may be
fatal. Intense antibiotic therapy sometimes
associated with surgical drainage of the affected
areas is necessary. It is not a malignant condition
in the histological sense, for the biopsies of
granulation tissue show inflammatory changes only.
Necrotizing otitis externa may be more accurate,
but malignant indicates the serious clinical nature.
Otitis Externa Secondary
Otitis externa secondary to discharge via a drum perforation is initially treated (an ear
swab having been taken for culture and sensitivity) with cleaning of the meatus and the
instillation of the appropriate antibiotic and corticosteroid drops. If the condition persists with
marked irritation and pain, a fungal otitis externa
should be suspected. In persistent infection, the
meatus contains a cocktail of drops, pus, and
desquamated skin. In fungal infections, as shown
here, the dark spores of Aspergillus niger and
white mycelium of Candida albicans can be seen.
Thorough cleaning of the meatus precedes
treatment with a topical antifungal agent. The
meatal skin infection is introduced from outside
usually from the patients finger, or from water,
particularly after swimming. The infection,
however, may be from the middle ear if there is a
perforation, and discharge from chronic otitis
media may be the cause of a persistent otitis
externa. Otitis externa rarely damages the
tympanic membrane. With fungal otitis externa,
however, and the presence of a granular
myringitis, a perforation may ensue.
2
Bullous otitis externa (bullousmyringitis)
This unusual otitis externa frequently follows
influenza or an upper respiratory tract infection. A
complaint of earache followed by bleeding, then
followed by relief of pain is diagnostic of this
condition. Examination shows hemorrhagic blebs
on the drum and meatus, similar to the vesicular
eruption of herpes. If there is pyrexia with a
conductive hearing loss, the otitis externa is
associated with an otitis media, and systemic
antibiotics are necessary. In the absence of
pyrexia and hearing loss, this condition settles
spontaneously without treatment.
Chalk patches
White areas of tympanosclerosis (arrows) are common findings on examination of the drum.
They are of little significance in themselves, and
the hearing is often normal. A past history of
otorrhea in childhood or grommet insertion is
usual. Chalk patches do occur with no apparent
past otitis media. Extensive tympanosclerosis
with a rigid drum is a sequela of past otitis
media, and the ossicles, too, may be fixed or
noncontinuous.
Aural Polip
If the growth of granulation tissue is exuberant, a pedunculated polyp develops, which may
present at the orifice of the meatus (arrow). Granulations and polyps commonly arise from
the tympanic annulus posteriorly, but the
originating site may also be the mucous
membrane of the promontory, eustachian tube
orifice, and antrum and aditus. Careful and
thorough removal of polyps and granulation
tissue to their site of origin is necessary. If the
polyp is associated with cholesteatoma, removal
by mastoid approach is required.
GAMBARAN PATOLOGIS PADA
HIDUNG
3
Granular Rhinitis
Granulation tissues in the nose requires biopsy. Sarcoidosis not infrequently involves the
upper respiratory tract mucosa of the nasal fossae and larynx. In the nose the granulations are
pale, but tuberculosis, malignant granuloma, and neoplasia are among the differential
diagnoses.
Nassal Adhesion
Adhesion or synechiae may follow nasal
trauma (including surgical trauma) and bridge
the lateral wall of the nose, frequently from the
inferior turbinate to the septum, causing nasal obstruction. Recurrence follows surgical
division of the larger adhesions unless an indwelling silastic splint is left in situ until mucosa
underlying the adhesion regenerates.
Deviated Nassal Septum
A congenital or traumatic dislocation of the
septal cartilage into one nasal fossa causes
unilateral nasal obstruction. If the obstruction is
marked, or complicated by recurrent sinusitis, a
septal correction is effective surgery. The time-
honored operation for this is a submucous resection (SMR), but a septoplasty in which
cartilage is preserved and repositionedrather than removedis now used. The SMR
operation involves removal of much of the septal cartilage and loss of nasal support with
saddling, and septal perforations are occasional complications.
A B
Deviated nasal septum into the columella. With caudal dislocation of the septum, an
obvious deformity is coupled with nasal obstruction (a). Repositioning or excision of the
septal dislocation is necessary to improve the appearance and
airway (b).
4
Deviated nasal septum. Deviated nasal septum with a spur of septal cartilage and maxillary
bone occluding the inferior meatus and causing nasal obstruction (see over).
Wegeners granuloma
An endoscopic view of the granulomatous tissue seen on nasal endoscopy. Wegeners
granuloma is a rare autoimmune inflammatory disease which often presents with nasal
symptoms of obstruction, crusting, and epistaxis. Damage to the septum may lead to a saddle
deformity.
The granulomas may be limited to the nose, but the
respiratory tract may be involved along with a
generalized vasculitis and glomerulonephritis. The
condition is characterized by periods of remission,
and treatment with oral steroids and cytotoxic drugs
has dramatically improved the prognosis of a
previously fatal condition.
Acute Maxilary Sinusitis
This is a common complication of a head cold. If a
head cold persists beyond four to five days with
continued nasal obstruction, purulent rhinorrhea, and headache, the probable diagnosis is
maxillary sinusitis. Apical infection of the teeth related to the antrum or an oroantral fistula
following dental extraction also cause maxillary sinusitis, as may trauma with bleeding into
the antrum or barotrauma. Frontal or facial pain may be referred to the upper teeth; nasal
obstruction and purulent rhinorrhea are the other symptoms. The antrum is opaque on
computed tomography (CT; Fig. 3.57a). There may be tenderness over the sinus, but swelling
is rare. Pus is seen issuing from the middle meatus (Fig. 3.58a, arrow). Acute infection may
less commonly affect the ethmoid, frontal, and sphenoid sinuses. Systemic antibiotics, a
vasoconstrictor spray, or drops.
A B
5
Maxillary sinusitis with pus (a, arrow) adjacent to the middle turbinate issuing into the
middle meatus, seen with the endoscope
(b).
Gambaran Patologis Tenggorok
Scleroma
Scleroma with scarring of the soft
palate and oropharynx. This is a specific
chronic inflammatory disease of the upper
respiratory tract mucosa predominantly occurring in Eastern Europe, Asia, and South
America. A protracted painless inflammation of the nose (rhinoscleroma), pharynx, or larynx
is followed after many years by extensive scarring, which is particularly apparent in the
oropharynx. Unlike gummatous ulceration, which is a differential
diagnosis, scleroma is not destructive, the uvula is preserved,
although it may be retracted by scarring into the nasopharynx, and
is seen with the postnasal mirror. The histology of the mucosa in
scleroma is characteristic and diagnostic.
Laringitis
Whether acute or chronic, laryngitis presents with hoarseness and
generalized hyperemia of the laryngeal mucous membrane. Acute
laryngitis commonly follows an upper respiratory tract infection, or
is traumatic following vocal abuse. Voice rest is the most effective treatment.
Normal vocal cords. These are ivory colored and smooth with few vessels on the surface.
This is the view obtained through a laryngoscope at direct microlaryngoscopy.
Acute laryngitis showing slight hyperemia
and edema of both vocal cords seen with
the fiberoptic endoscope.
6
Papiloma
These may occur on the uvula (a), fauces, and tonsil. The patient often notices these
papillomas when looking at the throat, or they are found at medical examination. Symptoms
are uncommon. They are usually pedunculated and are easily and painlessly removable in
outpatients. They should be sent for histology to exclude a squamous carcinoma. If ignored, a
papilloma may cause symptoms on account of size. This large papilloma (b) arises from the
base of the right tonsil.
Bifid Uvula
A common minor congenital deformity of the palate. It is of little significance, but it may be
associated with a submucous palatal cleft. Inflammation of the uvula as an isolated entity
may occur, however, and a cherry-like enlargement may be the sole presenting sign of a sore
throat (uvulitis).
Supratonsilar Cleft
7
This recess near the superior pole of the tonsil, if large, tends to collect debris. A mass of
yellow fetid material can be extruded from the tonsil with pressure; discomfort or halitosis
are symptoms with which this condition may present.
Tonsillectomy may be necessary. The surgeon, however, must
beware of tonsillectomy for halitosis. Although dental or gastric
pathology may cause this symptom (as may a pharyngeal pouch),
the symptom may be imagined by the patient, or by another
person complaining about the halitosis.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 6.variable V Variable F Control - Braking, Closed Loop ControlDocument25 pages6.variable V Variable F Control - Braking, Closed Loop ControlJanani RangarajanNo ratings yet
- Comparing and contrasting inductive learning and concept attainment strategiesDocument3 pagesComparing and contrasting inductive learning and concept attainment strategiesKeira DesameroNo ratings yet
- IB Diploma Maths / Math / Mathematics IB DP HL, SL Portfolio TaskDocument1 pageIB Diploma Maths / Math / Mathematics IB DP HL, SL Portfolio TaskDerek Chan100% (1)
- Presentations - Benefits of WalkingDocument1 pagePresentations - Benefits of WalkingEde Mehta WardhanaNo ratings yet
- Feminism in Lucia SartoriDocument41 pagesFeminism in Lucia SartoriRaraNo ratings yet
- Httpswww.ceec.Edu.twfilesfile Pool10j07580923432342090202 97指考英文試卷 PDFDocument8 pagesHttpswww.ceec.Edu.twfilesfile Pool10j07580923432342090202 97指考英文試卷 PDFAurora ZengNo ratings yet
- 3 QDocument2 pages3 QJerahmeel CuevasNo ratings yet
- Waiver: FEU/A-NSTP-QSF.03 Rev. No.: 00 Effectivity Date: Aug. 10, 2017Document1 pageWaiver: FEU/A-NSTP-QSF.03 Rev. No.: 00 Effectivity Date: Aug. 10, 2017terenceNo ratings yet
- Ck-Nac FsDocument2 pagesCk-Nac Fsadamalay wardiwiraNo ratings yet
- 14 Worst Breakfast FoodsDocument31 pages14 Worst Breakfast Foodscora4eva5699100% (1)
- NDA Template Non Disclosure Non Circumvent No Company NameDocument9 pagesNDA Template Non Disclosure Non Circumvent No Company NamepvorsterNo ratings yet
- Bhushan ReportDocument30 pagesBhushan Report40Neha PagariyaNo ratings yet
- Kina Finalan CHAPTER 1-5 LIVED EXPERIENCES OF STUDENT-ATHLETESDocument124 pagesKina Finalan CHAPTER 1-5 LIVED EXPERIENCES OF STUDENT-ATHLETESDazel Dizon GumaNo ratings yet
- A Chat (GPT) About The Future of Scientific PublishingDocument3 pagesA Chat (GPT) About The Future of Scientific Publishingraul kesumaNo ratings yet
- TDS Tetrapur 100 (12-05-2014) enDocument2 pagesTDS Tetrapur 100 (12-05-2014) enCosmin MușatNo ratings yet
- Climbing KnotsDocument40 pagesClimbing KnotsIvan Vitez100% (11)
- Presidential Decree 1613 Amending The Law of ArsonDocument19 pagesPresidential Decree 1613 Amending The Law of ArsonBfp Atimonan QuezonNo ratings yet
- The Role of Store LocationDocument6 pagesThe Role of Store LocationJessa La Rosa MarquezNo ratings yet
- Rock Art and Metal TradeDocument22 pagesRock Art and Metal TradeKavu RI100% (1)
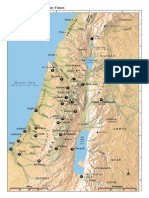
- Israel Bible MapDocument1 pageIsrael Bible MapMoses_JakkalaNo ratings yet
- MyiasisDocument29 pagesMyiasisihsanNo ratings yet
- JDDocument19 pagesJDJuan Carlo CastanedaNo ratings yet
- Basic Principles of Social Stratification - Sociology 11 - A SY 2009-10Document9 pagesBasic Principles of Social Stratification - Sociology 11 - A SY 2009-10Ryan Shimojima67% (3)
- The Hittite Name For GarlicDocument5 pagesThe Hittite Name For GarlictarnawtNo ratings yet
- Operative ObstetricsDocument6 pagesOperative ObstetricsGrasya ZackieNo ratings yet
- A Christmas Carol AdaptationDocument9 pagesA Christmas Carol AdaptationTockington Manor SchoolNo ratings yet
- E Purjee (New Technology For The Sugarcane Farmers)Document4 pagesE Purjee (New Technology For The Sugarcane Farmers)Mohammad Shaniaz IslamNo ratings yet
- Web Design Course PPTX Diana OpreaDocument17 pagesWeb Design Course PPTX Diana Opreaapi-275378856No ratings yet
- TOPIC 12 Soaps and DetergentsDocument14 pagesTOPIC 12 Soaps and DetergentsKaynine Kiko50% (2)
- Asia Competitiveness ForumDocument2 pagesAsia Competitiveness ForumRahul MittalNo ratings yet