Professional Documents
Culture Documents
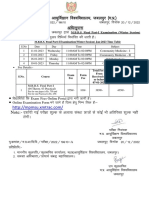
Novel Coronavirus Infection
Uploaded by
Mohamed ShalabiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Novel Coronavirus Infection
Uploaded by
Mohamed ShalabiCopyright:
Available Formats
Dr.
AL ANOUD ABDULLAH AL-JIFRI
Chairman of Infection & Prevention Department
Infectious Diseases Consultant
KFH, Madinah , MOH
CDC continues to work closely with the WHO and other partners
to better understand the public health risk presented by recently
reported cases of infection with a novel coronavirus (nCoV).
As of May 16, 2013, 40 laboratory-confirmed cases have been
reported to WHO :
30 from Saudi Arabia,
2 from Qatar,
2 from Jordan,
3 from the United Kingdom,
one from the United Arab Emirates,
and 2 from France.
Among the 40 cases, 20 were fatal.
Baltimore classification
is a classification system that places viruses into one of
seven groups depending on a combination of their nucleic
acid (DNA or RNA), strandedness (single-stranded or
double-stranded), Sense, and method of replication.
Named after David Baltimore, a Nobel Prize-winning biologist
Virus Family Examples (common names)
Adenoviridae
Adenovirus, Infectious canine hepatitis
virus
Papovaviridae Papillomavirus, Polyomaviridae,
Parvoviridae Parvovirus B19, Canine parvovirus
Herpesviridae
Herpes simplex virus, varicella-zoster
virus, cytomegalovirus, Epstein-Barr
virus
Poxviridae
Smallpox virus, cow pox virus, sheep pox
virus, orf virus, monkey pox virus,
vaccinia virus
Hepadnaviridae Hepatitis B virus
Anelloviridae Torque teno virus
Virus Family Examples (common names)
Reoviridae Reovirus, Rotavirus
Picornaviridae
Enterovirus, Rhinovirus, Hepatovirus,
Cardiovirus, Aphthovirus, Poliovirus,
Parechovirus, Erbovirus, Kobuvirus, Teschovirus,
Coxsackie
Caliciviridae Norwalk virus
Togaviridae Rubella virus, alphavirus
Arenaviridae Lymphocytic choriomeningitis virus
Flaviviridae
Dengue virus, Hepatitis C virus, Yellow fever
virus
Orthomyxoviridae
Influenzavirus A, Influenzavirus B,
Influenzavirus C, Isavirus, Thogotovirus
Virus Family Examples (common names)
Paramyxoviridae
Measles virus, Mumps virus, Respiratory
syncytial virus, Rinderpest virus, Canine
distemper virus
Bunyaviridae California encephalitis virus, Hantavirus
Rhabdoviridae Rabies virus
Filoviridae Ebola virus, Marburg virus
Coronaviridae Corona virus
Astroviridae Astrovirus
Bornaviridae Borna disease virus
Arteriviridae Arterivirus, Equine Arteritis Virus
Hepeviridae Hepatitis E virus
Are species in the genera of virus belonging to the
subfamily Coronavirinae in the family
Coronaviridae.
The name "coronavirus" is derived from the Latin
corona, meaning crown or halo, and refers to the
characteristic appearance of virions under electron
microscopy (E.M.) with a fringe of large, bulbous
surface projections creating an image
reminiscent of the solar corona.
Human coronaviruses were first identified
in the mid 1960s.
Coronaviruses primarily infect the upper
respiratory and gastrointestinal tract of
mammals and birds.
In chickens, the Infectious bronchitis virus (IBV), a
coronavirus, targets not only the respiratory tract
but also the uro-genital tract.
The virus can spread to different organs throughout
the chicken.
4-5 different currently known strains of coronaviruses
infect humans.
The most publicized human coronavirus, SARS-CoV
which causes SARS, has a unique pathogenesis because it
causes both upper and lower respiratory tract infections
and can also cause gastroenteritis.
The five coronaviruses that can infect people are:
alpha coronaviruses 229E and NL63
beta coronaviruses OC43, HKU1,SARS-CoV (the
coronavirus that causes severe acute respiratory
syndrome).
Genus: Alphacoronavirus; type species: Alphacoronavirus 1
Species: Alpaca coronavirus, Alphacoronavirus 1, Human coronavirus
229E, Human Coronavirus NL63, Miniopterus Bat coronavirus 1,
Miniopterus Bat coronavirus HKU8, Porcine epidemic diarrhea virus,
Rhinolophus Bat coronavirus HKU2, Scotophilus Bat coronavirus 512
Genus Betacoronavirus; type species: Murine coronavirus
Species: Betacoronavirus 1, Human coronavirus HKU1, Murine
coronavirus, Pipistrellus Bat coronavirus HKU5, Rousettus Bat
coronavirus HKU9, Severe acute respiratory syndrome-related
coronavirus, Tylonycteris Bat coronavirus HKU4, hCoV-EMC
Genus Deltacoronavirus; type species: Bulbul coronavirus HKU11
Species: Bulbul coronavirus HKU11, Munia coronavirus HKU13, Thrush
coronavirus HKU12
Genus Gammacoronavirus; type species: Avian coronavirus
Species: Avian coronavirus, Beluga whale coronavirus SW1
Coronaviruses cause colds in humans primarily in
the winter and early spring seasons.
In the United States, people usually get infected
with human coronaviruses in the fall and winter.
Most people will get infected with human
coronaviruses in their life time.
Young children are most likely to get
infected.
However, anybody can have multiple
infections in life time , and typically lead to
the common cold in adults and children.
What is the new human coronavirus?
The new virus strain is the human beta-coronavirus
EMC (HCoV-EMC)
It is different from other coronaviruses that have
been found in people before.
This particular novel coronavirus is rare but causes
serious illness, including death.
The virus may have
originated in an animal,
such as bats, but that
investigation is still
ongoing.
CDC is still learning
about this new virus.
The novel coronavirus is not the same virus that
caused severe acute respiratory syndrome (SARS)
in 2003.
However, like the SARS virus, the novel
coronavirus is most similar to those found in bats (
Genetic sequencing to date has determined the
virus is most closely related to coronaviruses
detected in bats).
This novel coronavirus is from the same large
family of viruses that includes the SARS virus.
Both viruses are capable of causing severe disease.
However, one of the key differences between the
two is that this novel coronavirus doesnt seem
to get passed from person to person easily, while
the SARS virus did.
SARS CORONAVIRUS
NCOV
Group: Group IV ((+)ssRNA)
Order: Nidovirales
Family: Coronaviridae
Genus: Coronavirus
Species: SARS coronavirus
Group: Group IV ((+)ssRNA)
Order: Nidovirales
Family: Coronaviridae
Subfamily: Coronavirinae
Genera
Alphacoronavirus
Betacoronavirus
Deltacoronavirus
Gammacoronavirus
The ways that human coronaviruses spread have
not been studied very much, except for SARS.
However, it is likely that human coronaviruses
spread from an infected person to others through:
The air by coughing and sneezing
Close personal contact, such as touching or
shaking hands.
There is clear evidence of human-to-human
transmission, possibly involving different modes of
transmission such as droplet and contact transmission.
In the UK, one infected person likely spread the virus
to two family members.
In Saudi Arabia, two healthcare providers were
infected after caring for patients who had novel
coronavirus.
But further studies are required to better understand the
risks.
These viruses may also spread by touching
contaminated objects or surfaces then
touching mouth, nose, or eyes.
Human coronaviruses usually cause mild
to moderate upper-respiratory tract
illnesses of short duration.
Symptoms may include runny nose,
cough, sore throat, and fever.
These viruses can sometimes
cause lower-respiratory tract
illnesses, such as pneumonia.
This is more common in people
with cardiopulmonary disease
or compromised immune
systems, or the elderly.
(Sudden ,severe, acute
respiratory illness )
Pneumonia has been the most common
clinical presentation.
5 patients developed Acute Respiratory
Distress Syndrome (ARDS).
Renal failure, pericarditis and disseminated
intravascular coagulation (DIC) have also
occurred.
clinical syndromes include :
Severe pneumonia
Acute Respiratory Distress Syndrome
Sepsis
Severe sepsis
Septic shock
A person with an acute respiratory infection, which may include history
of fever or measured fever ( 38 C, 100.4 F) and cough;
AND suspicion of pulmonary parenchymal disease (e.g. pneumonia or
ARDS), based on clinical or radiological evidence of consolidation:
AND residence in or history of travel to the Arabian Peninsula or
neighboring countries within 10 days before onset of illness:
AND not already explained by any other infection or aetiology, including
all clinically indicated tests for community-acquired pneumonia according
to local management guidelines.
It is not necessary to wait for test results for other
pathogens before testing for novel coronavirus.
Probable Case
A person fitting the definition above of a Patient Under Investigation,
with clinical, radiological, or histopathological evidence of pulmonary
parenchymal disease (e.g. pneumonia or the Acute Respiratory Distress
Syndrome, ARDS) but no possibility of laboratory confirmation either
because the patient or samples are not available or no testing is available
for other respiratory infections;
AND
Close contact with a laboratory-confirmed case;
AND
Not already explained by any other infection or aetiology, including all
clinically indicated tests for community-acquired pneumonia according to
local management guidelines.
Confirmed Case
A person with laboratory confirmation of infection
with the novel coronavirus.
Close contact includes:
Anyone who provided care for the patient,
including a health care worker or family member,
or who had other similarly close physical contact.
Anyone who stayed at the same place (e.g. lived
with, visited) as a probable or confirmed case
while the case was symptomatic.
In general, SARS begins with high fever (temperature
>100.4F [>38.0C]).
other symptoms may include :headache, an overall feeling
of discomfort ,and body aches.
Some people also have mild respiratory symptoms at the
onset.
About 10-20% of patients have diarreah.
After 2-7 days SARS patient may develop a dry cough.
Most patients develope pnemonia.
Preventing or limiting infection transmission in
health-care settings requires the application of
procedures and protocols referred to as controls.
Include the following:
A. Administrative controls.
B. Environmental and engineering controls.
C. Personal protective equipment (PPE).
These are the first priority of IPC strategies.
They provide the infrastructure of policies and
procedures to prevent, detect, and control infections
during health care.
To be effective, IPC measures must anticipate
the flow of patients from the first point of
encounter until discharge from the facility.
Includes:
1) Establishment of sustainable IPC
infrastructures and activities.
2) Education of HCWs.
3) Prevention of overcrowding in waiting
areas, providing dedicated waiting areas for
the ill and placement of hospitalized
patients.
4) Organization of health-care services for
adequate provision and use of supplies; policies
and procedures for all facets of occupational
health
5) Emphasis on surveillance of ARIs among
HCWs.
6) Importance of seeking medical care.
7) Monitoring of compliance.
Acute Respiratory Infections = ARI
8) Rapid identification of patients with
ARI and patients suspected of nCoV
infection, with prompt application of
appropriate precautions, and
implementation of source control.
Clinical triage should be used for early
identification of all patients with ARIs.
Identified ARI patients should be placed in an area
separate from other patients, and additional IPC
precautions has to be promptly implemented.
Clinical and epidemiological aspects of the cases
should be evaluated as soon as possible.
The investigation should be complemented by
laboratory evaluation.
These include :
basic health-care facility infrastructures
.
1. Ensuring adequate environmental ventilation
in all
areas within a health-care facility
2. Adequate environmental cleaning.
Spatial (locative) separation of at least 1 m should be
maintained between each ARI patient and others,
including HCWs (when not using PPE).
Both controls can help reduce the spread of some
pathogens during health care
Consistent use of available PPE and
appropriate hand hygiene help reduce the
spread of infection.
1 . Standard Precautions:
A cornerstone for providing safe health care and
reducing the risk of further infection.
Most transmissions occur in the absence of basic IPC
precautions and before a specific infection is suspected or
confirmed; hence, the routine application of measures to
prevent spread of acute respiratory infections (ARI)
when
caring for symptomatic patients is essential to reduce
spread of any ARI in health-care settings.
Include :
Hand hygiene.
Use of PPE to avoid direct contact with patients
blood, body fluids, secretions (including respiratory
secretions) and non-intact skin.
PPE should include the use of:
facial protection by means of either a medical mask
and eye-visor or goggles, or a face shield;
&
a gown and clean gloves.
Cleaning and
disinfection of the
environment (due to the
detection of SARS CoV
RNA by PCR on
surfaces in rooms
occupied by SARS
patients).
Prevention of needle-stick or sharps injury.
Safe waste management.
Cleaning, disinfection and, where applicable,
sterilization of patient-care equipment and
linen.
There are
currently no
vaccines
available to
protect you
against human
coronavirus
infection.
All individuals, including visitors and HCWs, in
contact with patients with ARI should:
1. Perform hand hygiene before and after contact with
the patient and his or her surroundings and
immediately after removal of a medical mask.
2. Wear a medical mask when in close contact (i.e.
within approximately 1 m) and upon entering the
room or cubicle of the patient. (Droplet precautions)
3. Wear eye protection (i.e. goggles or a face
shield)
4. Wear a clean, non-sterile, long-sleeved
gown; and gloves (some procedures may
require sterile gloves)
If any HCW have an illness caused by?
human coronaviruses, he/she can help
protect others by:
Staying home while they are sick.
Avoiding close contact with others.
Covering mouth and nose when coughing or
sneezing.
Limit the number of HCWs, family
members and visitors in contact with a
patient with probable or confirmed nCoV
infection.
Family members and visitors in contact
with a patient should be limited to those
essential for patient support and should be
trained on the risk of transmission and on
the use of the same infection control
precautions as HCWs who are providing
routine care.
All individuals, including visitors and HCWs has
to:
1. Perform hand hygiene before and after contact
with the patient and his or her surroundings and
immediately after removal of PPE.
2. Wear a medical mask
.
3. Wear eye protection (i.e. goggles or a face
shield).
4. Wear a clean, non-sterile, long-sleeved gown;
and gloves (some procedures may require sterile
gloves).
Use either disposable equipment or dedicated
equipment (e.g. stethoscopes, blood pressure cuffs
and thermometers).
If equipment needs to be shared among patients,
clean and disinfect it between each patient use.
HCWs should refrain from touching their eyes,
nose or mouth with potentially contaminated
gloved or ungloved hands.
Place patients with probable or confirmed nCoV infection
in adequately ventilated single rooms or Airborne
Precaution rooms.
if possible, situate the rooms used for isolation (i.e.
single rooms) in an area that is clearly segregated from
other patient-care areas.
When single rooms are not available, put patients with the
same diagnosis together.
If this is not possible, place patient beds at least 1 m
apart.
For patients with probable or confirmed nCoV infection:
a) Avoid the movement and transport of patients out of the
isolation room or area unless medically necessary.
b) Use designated portable X-ray equipment and other
important diagnostic equipment.
c) If transport is required, use routes of transport that minimize
exposures of staff, other patients and visitors.
d) Notify the receiving area of the patient's diagnosis and
necessary precautions as soon as possible before the patients
arrival.
!!!!!!!
e) Clean and disinfect patient-contact
surfaces (e.g. bed) after use.
f) Ensure that HCWs who are transporting
patients wear appropriate PPE and
perform hand hygiene afterwards.
aerosol-generating procedures are
Any medical procedure (tracheal intubation ,
tracheotomy, non-invasive ventilation and manual
ventilation,bronchoscopy) that can induce the
production of aerosols of various sizes, including
small (< 5 mkm) particles.
a) Perform hand hygiene before and after contact with the patient
and his or her surroundings and after PPE removal.
b) Wear a particulate respirator
(always check the seal )
c) Wear eye protection (i.e. goggles or a face shield)
d) Wear a clean, non-sterile, long-sleeved gown and gloves (some of
these procedures require sterile gloves).
e) Wear an impermeable apron for some procedures with expected
high fluid volumes that might penetrate the gown
f) Has to done in a negative pressure room
g) Perform procedures in an adequately ventilated room; i.e.
minimum of 6 to 12 air changes per hour in facilities
with a mechanically ventilated room and at least 60
liters/second/patient in facilities with natural ventilation
h) limit the number of persons present in the room to the
absolute minimum required for the patients care and
support
The duration of infectivity for nCoV infection is
unknown.
Isolation precautions should be used during the
duration of symptomatic illness
and continued for
24 hours after the resolution of symptoms.
Patient information (e.g. age, immune status and
medication) should also be considered in situations
where there is concern that a patient may be
shedding the virus for a prolonged period.
All specimens should be regarded as
potentially infectious
HCWs who collect or transport clinical specimens
should adhere rigorously to Standard Precautions to
minimize the possibility of exposure to pathogens.
1. Wear appropriate PPE
2. Trained in safe handling practices and spill
decontamination procedures.
3. Place specimens for transport in leak-proof specimen bags
(secondary container) that have a separate sealable pocket for
the specimen (i.e. a plastic biohazard specimen bag), with the
patients label on the specimen container (primary container),
and a clearly written request form.
4. Ensure that health-care facility laboratories adhere to
appropriate biosafety practices and transport requirements.
5. Deliver all specimens by hand whenever possible.
6. Do not use pneumatic-tube systems
to transport specimens.
7. State the name of the (suspected) ARI of potential
concern clearly on the accompanying request form.
Notify the laboratory as soon as possible that the
specimen is being transported.
8. After specimens are processed, decontaminate
work surfaces and equipment with appropriate
disinfectants. Use any EPA-registered hospital
disinfectant. Follow manufacturer's
recommendations for use-dilution (i.e.,
concentration), contact time, and care in
handling.
9. All disposable waste should be autoclaved.
Laboratory tests can be done to confirm infection
secondary to human coronaviruses.
Specific laboratory tests may include:
a) Virus isolation in cell culture.
b) Polymerase chain reaction (PCR) assays that are
more practical and available commercially.
c) Serological testing for antibodies to human
coronaviruses.
Nose and throat swabs are the best specimens for detecting
common human coronaviruses.
Serological testing requires collection of blood specimens.
Specimen Type and Priority
To increase the likelihood of detecting infection,
it is recommended to collect multiple specimens
from different sites at different times after
symptom onset, if possible.
As of November 27, 2012, consider lower
respiratory tract and stool specimens a priority
for collection and testing.
For short periods ( 72 hours), most specimens should be
held at 2-8oC rather than frozen
For delays exceeding 72 hrs, freeze specimens at -70oC
as soon as possible after collection (with exceptions noted
below).
Label each specimen container with the patients ID
number, specimen type and the date the sample was
collected.
A. Lower respiratory tract:
Broncheoalveolar lavage, tracheal aspirate, pleural fluid
Collect 2-3 mL into a sterile, leak-proof, screw-cap sputum collection
cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hrs; if exceeding 72 hrs, freeze
at -70oC and ship on dry ice.
Sputum
Have the patient rinse the mouth with water and then expectorate
deep cough sputum directly into a sterile, leak-proof, screw-cap
sputum collection cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hrs; if exceeding 72 hrs, freeze
at -70oC and ship on dry ice.
Nasopharyngeal and oropharyngeal swabs
Use only synthetic fiber swabs with plastic shafts.
Do not use calcium alginate swabs or swabs with wooden shafts, as they may
contain substances that inactivate some viruses and inhibit PCR testing.
Place swabs immediately into sterile tubes containing 2-3 ml of viral transport
media.
Refrigerate specimen at 2-8oC up to 72 hrs; if exceeding 72 hrs, freeze at -
70oC and ship on dry ice.
Nasopharyngeal swabs -- Insert a swab into the nostril parallel to the
palate. Leave the swab in place for a few seconds to absorb secretions. Swab
both nostrils.
Oropharyngeal swabs -- Swab the posterior pharynx, avoiding the tonsils
and tongue.
Nasal Aspirates
Collect 2-3 mL into a sterile, leak-proof, screw-cap
sputum collection cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hrs; if exceeding
72 hrs, freeze at -70oC and ship on dry ice.
Serum
For eventual serum antibody testing: Serum specimens should be collected
during the acute stage of the disease, preferably during the first week after
onset of illness, and again during convalescence, 3 weeks later.
Children and adults
Collect 1 tube (5-10 mL) of whole blood in a serum separator tube. Allow the
blood to clot, centrifuge briefly, and separate sera into sterile tube container.
The minimum amount of serum required for testing is 200 L. Refrigerate
specimen at 2-8oC and ship on ice- pack; freezing and shipment on dry ice is
permissible.
Infants
A minimum of 1 cc of whole blood is needed for testing of pediatric patients.
If possible, collect 1 cc in an EDTA tube and in a serum separator tube. If only
1cc can be obtained, use a serum separator tube.
EDTA blood (plasma)
Collect 1 tube (10 mL) of heparinized (green-top) or
EDTA (purple-top) blood.
Refrigerate specimen at 2-8oC and ship on ice-pack; do
not freeze.
Collect 2-5 grams of stool specimen (formed
or liquid) in sterile, leak-proof, screw-cap
sputum collection cup or sterile dry container.
Refrigerate specimen at 2-8oC up to 72 hrs; if
exceeding 72 hrs, freeze at -70oC and ship on
dry ice.
Respiratory
Specimens
Test for other
respiratory pathogens
If POSITIVE for other
respiratory pathogens:
1.Testing for novel CoV
may not be required
2.Contact CDC for
consultation
If NEGATIVE for other respiratory
pathogens:
1.Prepare multiple sample aliquots
(200 L) for retention at -70C and
shipping to CDC
2.Notify your local/state health
department and CDC
3.Contact CDC for approval to send
specimen aliquot for novel CoV
testing
Respiratory pathogens to be considered for testing by molecular
or antigen detection methods (not by viral culture) include:
1) influenza A, influenza B, respiratory syncytial virus,
human metapneumovirus, human parainfluenza viruses,
adenovirus, human rhinovirus and other respiratory viruses.
2) Streptococcus pneumoniae, Legionella pneumophila, and
other pathogens that cause severe lower respiratory infections.
Routine confirmation of cases of novel
coronavirus infection will be based on
detection of unique sequences of viral RNA
by real-time reverse-transcriptase
polymerase chain reaction (RT-PCR) and
sequencing.
To consider a case as laboratory-confirmed, one of
the following conditions must be met:
Positive PCR assays for at least two different
specific targets on the novel coronavirus genome
OR
One positive PCR assay for a specific target on
the novel coronavirus genome and an additional
different PCR product sequenced, confirming
identity to known sequences of the new virus
A positive PCR assay for a single specific target
without further testing is considered presumptive
evidence of novel coronavirus infection.
INTERPRETATION OF LABORATORY RESULTS
No virus-specific prevention or treatment (e.g. vaccine
or antiviral drugs) is available.
Only supportive management of patients who have acute
respiratory failure and septic shock as a consequence of
severe infection.
Because other complications have been seen (renal
failure, pericarditis, DIC) clinicians should monitor for
the development of these and other complications of
severe infection and treat them according to local
management guidelines.
Section 1 focuses on the early recognition and management of
patients with SARI and includes early initiation of supportive
and infection prevention and control measures, and therapeutics.
Section 2 focuses on management of patients who deteriorate
and develop severe respiratory distress and ARDS.
Section 3 focuses on the management of patients who
deteriorate and develop septic shock.
Section 4 focuses on ongoing care of the critically ill patient
and best practices to prevent complications.
Clinical management of severe acute respiratory
infections when novel coronavirus is suspected: What to
do and what not to do. Geneva, World Health
Organization, 2013. Available at
http://www.who.int/csr/disease/coronavirus_infections/Int
erimGuidance_ClinicalManagement_NovelCoronavirus_
11Feb13u.pdf
Yes.
WHO and CDC have not issued travel health
warnings for any country related to novel
coronavirus.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Test Bank Contemporary Behavior Therapy - Michael-Spiegler - 6th EditionDocument12 pagesTest Bank Contemporary Behavior Therapy - Michael-Spiegler - 6th Editionlewisbacha0% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Iveco F4ge PDFDocument142 pagesIveco F4ge PDFHandy Lee67% (3)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Or FlapsDocument5 pagesOr FlapsMohamed ShalabiNo ratings yet
- 10 03 02 Skin Tumors Melanoma 2Document50 pages10 03 02 Skin Tumors Melanoma 2Mohamed ShalabiNo ratings yet
- 10-01 Skin Grafts, Substitutes and Principles of Flaps-1Document78 pages10-01 Skin Grafts, Substitutes and Principles of Flaps-1Mohamed ShalabiNo ratings yet
- Rhinoplasty in Adolescent Cleft PatientsDocument9 pagesRhinoplasty in Adolescent Cleft PatientsMohamed ShalabiNo ratings yet
- Deck Damage and Penetrations: Prepared by Richard B. Heagler, P.EDocument9 pagesDeck Damage and Penetrations: Prepared by Richard B. Heagler, P.ENelzon MamaniNo ratings yet
- ImpetigoDocument31 pagesImpetigoUmmu Insyirah100% (1)
- TDDDocument4 pagesTDDJay VibhaniNo ratings yet
- Heat Affected Zone: Page 1 of 5Document5 pagesHeat Affected Zone: Page 1 of 5sujkubvsNo ratings yet
- ISA CCST Task List Reference GuideDocument13 pagesISA CCST Task List Reference GuideNaseer HydenNo ratings yet
- Mini City Direct Heating SubstationDocument4 pagesMini City Direct Heating SubstationPaul ButucNo ratings yet
- UntitledDocument193 pagesUntitledurosNo ratings yet
- Navi Cure prospectus summaryDocument50 pagesNavi Cure prospectus summaryGaurav SrivastavaNo ratings yet
- Cooking - Sauces and Marinade RecipesDocument96 pagesCooking - Sauces and Marinade Recipesagape_1st7100% (3)
- UntitledDocument77 pagesUntitledVedranL84No ratings yet
- R02.4 Standard III (A) - AnswersDocument11 pagesR02.4 Standard III (A) - AnswersShashwat DesaiNo ratings yet
- Vodafone Idea Limited: PrintDocument2 pagesVodafone Idea Limited: PrintPrakhar KapoorNo ratings yet
- Waste Management: Spoilage of LandscapeDocument7 pagesWaste Management: Spoilage of Landscapeshauryasahu2004No ratings yet
- Nescafe Alegria Nutritional Facts PDFDocument3 pagesNescafe Alegria Nutritional Facts PDFOmarNo ratings yet
- FAQ For Company Law 2013Document24 pagesFAQ For Company Law 2013Archanat07100% (1)
- Plateau Pressure Ventilation MeasurementDocument1 pagePlateau Pressure Ventilation MeasurementImtiaz AliNo ratings yet
- GSR (ROAD) 2015Document74 pagesGSR (ROAD) 2015Gautam RaiNo ratings yet
- Before The Honourable Supreme Court of India: Memorandum On Behalf of PetitonersDocument31 pagesBefore The Honourable Supreme Court of India: Memorandum On Behalf of Petitonerspalkin50% (2)
- Entrenamiento de Fuerza y Salud Pediátrica Ingles PDFDocument9 pagesEntrenamiento de Fuerza y Salud Pediátrica Ingles PDFGiiovanny PardoNo ratings yet
- Post Harvest Value Chainof Carrot AReviewDocument12 pagesPost Harvest Value Chainof Carrot AReviewDave RoneNo ratings yet
- Concept of Health and IllnessDocument24 pagesConcept of Health and IllnessHydra Olivar - Pantilgan100% (1)
- Oral Dislocation Rehabilitation Program - FirstDocument2 pagesOral Dislocation Rehabilitation Program - FirstPriyaki SebastianNo ratings yet
- MBBS Final Part-I (Winter Session) Time Table (Jan 2023)Document1 pageMBBS Final Part-I (Winter Session) Time Table (Jan 2023)crystal mindNo ratings yet
- PRECOMMISSIONING and COMMISSIONING PROCEDURE FOR CARD ACCESS CONTROL SYSTEMDocument3 pagesPRECOMMISSIONING and COMMISSIONING PROCEDURE FOR CARD ACCESS CONTROL SYSTEMHumaid ShaikhNo ratings yet
- Reglas para Añadir Al Verbo Principal: Am Is Are ReadDocument8 pagesReglas para Añadir Al Verbo Principal: Am Is Are ReadBrandon Sneider Garcia AriasNo ratings yet
- Practical Laser Diodes GuideDocument4 pagesPractical Laser Diodes GuideM Xubair Yousaf XaiNo ratings yet
- Properties of X-Rays and Gamma RaysDocument13 pagesProperties of X-Rays and Gamma RaysjishnusajiNo ratings yet
- Asrs For AutomationDocument25 pagesAsrs For AutomationJavedNo ratings yet