Professional Documents
Culture Documents
Pseudomonas Spp. - Pathogen Safety Data Sheets - Public Health Agency of Canada
Uploaded by
Reg LagartejaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pseudomonas Spp. - Pathogen Safety Data Sheets - Public Health Agency of Canada
Uploaded by
Reg LagartejaCopyright:
Available Formats
Home > Laboratory Biosafety and Biosecurity > Biosafety Programs and Resources > Pathogen Safety Data
Sheets
and Risk Assessment > Pseudomonas spp.
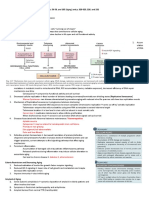
PSEUDOMONAS SPP.
PATHOGEN SAFETY DATA SHEET - INFECTIOUS SUBSTANCES
SECTION I - INFECTIOUS AGENT
NAME: Pseudomonas spp.
SYNONYM OR CROSS REFERENCE: P. aeruginosa, P. stutzeri, P. fluorescens
CHARACTERISTICS: The genus Pseudomonas, of the Pseudomonadaceae family, are motile gram-
negative aerobic bacteria, 2 4 m long plump-shaped rods, with polar flagella which have an important
role in pathogenicity
1 - 3
. They are non-spore forming and can produce pigments, such as pyocyanine
(green-blue) and pyorubrin (yellow-green) fluorescence
1 , 4 - 7
. P. aeruginosa can produce a large
variety of extracellular toxins, including exotoxin A and enterotoxins
8
. Other substances such as
hydrocyanic acid, proteolytic enzymes, toxic surface slime, and haemolytic substances may also
contribute to the pathogenicity of this species. Toxins combined with harmful substances are determinant
factors in the high virulence of P. aeruginosa in a variety of different hosts
9
.
SECTION II - HAZARD IDENTIFICATION
PATHOGENICITY/TOXICITY: As opportunistic pathogens, Pseudomonas spp. often invades the host
tissue and cause infection and bacteremia in immunocompromised hosts (e.g., HIV/AIDS, cystic fibrosis,
bronchiectasis, and severe chronic obstructive pulmonary disease, burns, malignancy, or diabetes
mellitus)
10 , 11
. The common site of infection is the lower respiratory tract, and severity ranges from
colonization without immunological response to severe necrotizing bronchopneumonia; such severe
infection in patients with cystic fibrosis is almost impossible to eradicate once established in the airways
12
. Pseudomonal pneumonia often develops from oro-pharyngeal contamination or secondary
bacteremia, and is also a common cause of nosocomial ventilator-related pneumonia in intensive care
settings. Infections also include endocarditis, osteomyelitis, urinary tract infections, gastrointestinal
infections, meningitis, and, commonly, septicaemia
13
. P. aeruginosa is the most common agent
associated with infection and inflammation during contact lens wear. The bacteria colonize on lenses and
produce proteases to kill or invade corneal cells, an infection that can lead to scarring and vision loss
1
.
The species is also the most virulent with a mortality rate of 30%, which can be higher depending on
predisposing conditions
4
. P. aeruginosa can also readily colonize on open burn wounds, causing
infections, abscesses, and sepsis, with edema and/or discoloration of unburned skin at wound margins
and green pigment in subcutaneous fat
14 , 15
. P. aeruginosa is also associated with swimmers ear
(otitis externa). Other Pseudomonas species are also opportunistic; however, cases of infection are rare
3
.
EPIDEMIOLOGY: Worldwide often a problem in hospitals as it can be found on equipment, increasing
the risk of nosocomial infections
12
. 30 40% of those with cystic fibrosis will acquire chronic
pseudomonal infection. P. aeruginosa infections account for 20% of pneumonia and 16% of urinary tract
infections
16
. Prevalence in the community is less than in the hospital, and cases of severe community-
acquired infection are rare
17
.
HOST RANGE: Humans, animals (wild, domestic, livestock), and plants (flora and fungi)
18
.
Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote
Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote Footnote
INFECTIOUS DOSE: Unknown for humans. Studies with larvae models have found the infectious dose for
the insects to be high
19
.
MODE OF TRANSMISSION: P. aeruginosa have been found to survive within droplet nuclei and can
remain in aerosols for long periods of time, thus there is evidence of potential airborne transmission
20
.
Contact with contaminated water is also a major route, but since the oral infectious dose is thought to be
very high, routes that pose the greatest health risk are skin exposure (for example, in contaminated hot
tub water) and lung exposure from inhaling aerosols discharged from infected respiratory tracts
13
. The
bacterial can often enter the body through injuries and wounds
3
. The use of contaminated mechanical
respiratory ventilators in hospital settings is also a common source of nosocomial infections
12
.
INCUBATION PERIOD: Varies according to infection, eye infection can appear 24 72 hours after
infection
21
.
COMMUNICABILITY: Spread of infection from person-to-person is speculated to be highly possible
during infection, especially amongst cystic fibrosis patients
22
.
SECTION III - DISSEMINATION
RESERVOIR: Infected humans, animals, contaminated water, soil
18
. Pseudomonas spp. are ubiquitous
in the environment.
ZOONOSIS: None.
VECTORS: None.
SECTION IV - STABILITY AND VIABILITY
DRUG SUSCEPTIBILITY: Pseudomonas spp. are resistant to many antibiotics. Susceptibility to
extended-spectrum penicillins (such as ticarcillin, azlocillin, and piperacillin), aminoglycosides,
cephalosporins, fluoroquinolones, polymixins, and the monobactams
12
.
DRUG RESISTANCE: Multi-drug resistant strains are emerging, such as against carbenicillin,
cephalosporins, ceftazidime, and ciprofloxacin
12
.
SUSCEPTIBILITY TO DISINFECTANTS: Susceptibility has been shown for 1% sodium hypochlorite,
70% ethanol, 2% glutaraldehyde, and formaldehyde
23
; however, it has been found to be resistant to
disinfectants that are used to treat drinking water such as chlorine, chloramines, ozone, and iodine
13
.
Certain adapted stains have been found to be able to grow in disinfectants; however, isopropyl alcohol 4%
v/v or ethyl alcohol 6% v/v are effective disinfectants
24
.
PHYSICAL INACTIVATION: Inactivation and sterilization using moist heat should be at 121C for 15
minutes or longer, dry heat at 170-250 C or higher for 30 minutes or more
25
.
SURVIVAL OUTSIDE HOST: Pseudomonas can survive for months on dry surfaces and inanimate
objects, and are one of the bacteria most frequently isolated from patients with nosocomial infections;
humidity can improve persistence
26
. Growth observed in distilled water can survive up to months with
minimal nutrients
27
.
SECTION V FIRST AID / MEDICAL
SURVEILLANCE: Diagnosis is made by bacteriological culture on selective/non-selective culture media
and laboratory identification
28
.
FIRST AID/TREATMENT: Administer appropriate drug therapy. Aminoglycoside with !-lactam penicillin
is usually the first line of treatment
12
. Aggressive treatment can avoid development of chronic infection.
Wounds should be cleaned with surgical detergent disinfectants and/or topical antibacterial ointments,
such as mupirocin
15
.
IMMUNIZATION: None currently available, although studies have shown that live-attenuated P.
aeruginosa vaccines in mice can protect against corneal infections
15
.
PROPHYLAXIS: Antibiotics such as ciprofloxacin (a fluoroquinolone) can be used in patients with CF, but
constant prophylactic therapy is not recommended as it can lead to drug resistance
12
.
SECTION VI - LABORATORY HAZARDS
LABORATORY-ACQUIRED INFECTIONS: None reported to date.
SOURCES/SPECIMENS: Blood cultures, urine, skin, sputum, soft tissue samples, lower respiratory tract
secretions, wound exudates, contaminated water samples, and mechanical ventilator equipment
4 , 12 , 14 , 27 , 28
PRIMARY HAZARDS: Accidental parenteral inoculation, inhalation of infectious aerosols, accidental
ingestion, or direct skin contact
4 , 13 , 20
.
SPECIAL HAZARDS: None.
SECTION VII EXPOSURE CONTROLS / PERSONAL PROTECTION
RISK GROUP CLASSIFICATION: Risk Group 2. This risk group applies to the genus as a whole, and
may not apply to every species within the genus.
CONTAINMENT REQUIREMENTS: Containment Level 2 facilities, equipment, and operational practices
for work involving infectious or potentially infectious materials, animals, or cultures. These containment
requirements apply to the genus as a whole, and may not apply to each species within the genus.
PROTECTIVE CLOTHING: Lab coat. Gloves when direct skin contact with infected materials or animals is
unavoidable. Eye protection must be used where there is a known or potential risk of exposure to
splashes
29
.
OTHER PRECAUTIONS: All procedures that may produce aerosols, involve high concentrations or large
volumes should be conducted in a biological safety cabinet (BSC). The use of needles, syringes, and other
sharp objects should be strictly limited. Additional precautions should be considered with work involving
animals or large scale activities
29
.
SECTION VIII HANDLING AND STORAGE
SPILLS: Allow aerosols to settle and, wearing protective clothing, gently cover spill with paper towels and
apply an appropriate disinfectant, starting at the perimeter and working towards the centre. Allow
sufficient contact time before clean up
29
.
DISPOSAL: Decontaminate all wastes that contain or have come in contact with the infectious organism
before disposing by autoclave, chemical disinfection, gamma irradiation, or incineration
29
.
STORAGE: The infectious agent should be stored in leak-proof containers that are appropriately labelled
29
.
SECTION IX - REGULATORY AND OTHER INFORMATION
REGULATORY INFORMATION: The import, transport, and use of pathogens in Canada is regulated
under many regulatory bodies, including the Public Health Agency of Canada, Health Canada, Canadian
Food Inspection Agency, Environment Canada, and Transport Canada. Users are responsible for ensuring
they are compliant with all relevant acts, regulations, guidelines, and standards.
UPDATED: December 2011
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
PREPARED BY: Pathogen Regulation Directorate, Public Health Agency of Canada
Although the information, opinions and recommendations contained in this Pathogen Safety Data Sheet
are compiled from sources believed to be reliable, we accept no responsibility for the accuracy, sufficiency,
or reliability or for any loss or injury resulting from the use of the information. Newly discovered hazards
are frequent and this information may not be completely up to date.
Copyright
Public Health Agency of Canada, 2011
Canada
REFERENCES:
Willcox, M. D. (2007). Pseudomonas aeruginosa infection and inflammation during contact lens
wear: a review. Optometry and Vision Science : Official Publication of the American Academy of
Optometry, 84(4), 273-278. doi:10.1097/OPX.0b013e3180439c3e
Dasgupta, N., Arora, S. K., & Ramphal, R. (2000). fleN, a gene that regulates flagellar number
in Pseudomonas aeruginosa. Journal of Bacteriology, 182(2), 357-364.
Kayser, F. H., Bienz, K. A., Eckert, J., & Zingernagel, R. M. (Eds.). (2001). Medical Microbiology
(10th ed.). Stuttgart, Germany: Georg Thieme Verlag.
Enoch, D. A., Simpson, A. J., & Kibbler, C. C. (2004). Predictive value of isolating Pseudomonas
aeruginosa from aerobic and anaerobic blood culture bottles. Journal of Medical Microbiology,
53(Pt 11), 1151-1154.
Young, R. S., Deal, P. H., & Whitfield, O. (1968). The response of spore-forming vs. nonspore-
forming bacteria to diurnal freezing and thawing. Space Life Sciences, 1(1), 113-117.
Shellito, J., Nelson, S., & Sorensen, R. U. (1992). Effect of pyocyanine, a pigment of
Pseudomonas aeruginosa, on production of reactive nitrogen intermediates by murine alveolar
macrophages. Infection and Immunity, 60(9), 3913-3915.
Palumbo, S. A. (1972). Role of iron and sulfur in pigment and slime formation by Pseudomonas
aeruginosa. Journal of Bacteriology, 111(2), 430-436.
Liu, P. V. (1974). Extracellular toxins of Pseudomonas aeruginosa. The Journal of Infectious
Diseases, 130 Suppl(0), S94-9.
Stover, G. B., Drake, D. R., & Montie, T. C. (1983). Virulence of different Pseudomonas species
in a burned mouse model: tissue colonization by Pseudomonas cepacia. Infection and
Immunity, 41(3), 1099-1104.
LIU, P. V., & MERCER, C. B. (1963). Growth, Toxigenicity and Virulence of Pseudomonas
Aeruginosa. The Journal of Hygiene, 61, 485-491.
Feldman, M., Bryan, R., Rajan, S., Scheffler, L., Brunnert, S., Tang, H., & Prince, A. (1998). Role
of flagella in pathogenesis of Pseudomonas aeruginosa pulmonary infection. Infection and
Immunity, 66(1), 43-51.
Banerjee, D., & Stableforth, D. (2000). The treatment of respiratory pseudomonas infection in
cystic fibrosis: what drug and which way? Drugs, 60(5), 1053-1064.
Mena, K. D., & Gerba, C. P. (2009). Risk assessment of Pseudomonas aeruginosa in water.
Reviews of Environmental Contamination and Toxicology, 201, 71-115. doi:10.1007/978-1-
4419-0032-6_3
Pruitt, B. A.,Jr, McManus, A. T., Kim, S. H., & Goodwin, C. W. (1998). Burn wound infections:
current status. World Journal of Surgery, 22(2), 135-145.
Zaidi, T. S., Priebe, G. P., & Pier, G. B. (2006). A live-attenuated Pseudomonas aeruginosa
vaccine elicits outer membrane protein-specific active and passive protection against corneal
infection. Infection and Immunity, 74(2), 975-983. doi:10.1128/IAI.74.2.975-983.2006
Date Modified: 2012-04-30
16
17
18
19
20
21
22
23
24
25
26
27
28
29
Nadeem, S. G., Qasmi, S. A., Afaque, F., Saleem, M., & Hakim, S. T. (2009). Comparison of the
in vitro susceptibility of Clinical isolates of Pseudomonas aeruginosa in a local hospital setting in
Karachi, Pakistan. British Journal of Medical Practitioners, 2(4), 35-39.
Ishihara, S., Takino, M., Okada, Y., & Mimura, K. (1995). Septic shock due to Pseudomonas
aeruginosa in a previously healthy woman. Intensive Care Medicine, 21(3), 226-228.
Pirnay, J. P., Bilocq, F., Pot, B., Cornelis, P., Zizi, M., Van Eldere, J., Deschaght, P., Vaneechoutte,
M., Jennes, S., Pitt, T., & De Vos, D. (2009). Pseudomonas aeruginosa population structure
revisited. PloS One, 4(11), e7740. doi:10.1371/journal.pone.0007740
Banerjee, A., & Dangar, T. K. (1995). Pseudomonas aeruginosa, a facultative pathogen of red
palm weevil, Rhynchophorus ferrugineus. World Journal of Microbiology and Biotechnology, 11,
618-620.
Clifton, I. J., & Peckham, D. G. (2010). Defining routes of airborne transmission of
Pseudomonas aeruginosa in people with cystic fibrosis. Expert Review of Respiratory Medicine,
4(4), 519-529. doi:10.1586/ers.10.42
Ziady, L. E., & Small, N. (Eds.). (2004). Prevent and Control Infection. Cape Town, South
Africa: Juda and Co Ltd.
Speert, D. P., Campbell, M. E., Henry, D. A., Milner, R., Taha, F., Gravelle, A., Davidson, A. G.,
Wong, L. T., & Mahenthiralingam, E. (2002). Epidemiology of Pseudomonas aeruginosa in cystic
fibrosis in British Columbia, Canada. American Journal of Respiratory and Critical Care
Medicine, 166(7), 988-993.
Laboratory Safety Manual (1993). (2nd ed.). Geneva: World Health Organization.
Burdon, D. W., & Whitby, J. L. (1967). Contamination of hospital disinfectants with
Pseudomonas species. British Medical Journal, 2(5545), 153-155.
Nail, S. L., & Akers, M. J. (Eds.). (2002). Development and Manufacture of Protein
Pharmaceuticals. New York, NY, USA: Kluwer Academic / Plenum Publishers.
Kramer, A., Schwebke, I., & Kampf, G. (2006). How long do nosocomial pathogens persist on
inanimate surfaces? A systematic review. BMC Infectious Diseases, 6, 130. doi:10.1186/1471-
2334-6-130
Leung, D. K. C., Mok, W. F. M., Yu, D. M. W., & Au, T. C. (2001). Use of distilled white vinegar
dressing supplemental to oral antibiotics in the management of Pseudomonas aeruginosa exit
site infection in continuous ambulatory peritoneal dialysis patients. Hong Kong Journal of
Nephrology, 3(1), 38-40.
Xu, J., Moore, J. E., Murphy, P. G., Millar, B. C., & Elborn, J. S. (2004). Early detection of
Pseudomonas aeruginosa--comparison of conventional versus molecular (PCR) detection
directly from adult patients with cystic fibrosis (CF). Annals of Clinical Microbiology and
Antimicrobials, 3, 21. doi:10.1186/1476-0711-3-21
Public Health Agency of Canada. (2004). In Best M., Graham M. L., Leitner R., Ouellette M. and
Ugwu K. (Eds.), Laboratory Biosafety Guidelines (3rd ed.). Canada: Public Health Agency of
Canada.
You might also like
- Virology MnemonicsDocument2 pagesVirology MnemonicsReg Lagarteja100% (3)
- Comprehensive Exam Recall QuestionsDocument6 pagesComprehensive Exam Recall QuestionsReg LagartejaNo ratings yet
- Drug Database - Potassium CitrateDocument2 pagesDrug Database - Potassium CitrateReg LagartejaNo ratings yet
- CEISDocument5 pagesCEISReg LagartejaNo ratings yet
- Analytic Studies in EpidemiologyDocument3 pagesAnalytic Studies in EpidemiologyReg LagartejaNo ratings yet
- Pedia Clinical Encounter FormDocument11 pagesPedia Clinical Encounter FormReg LagartejaNo ratings yet
- DS SampleDocument3 pagesDS SampleReg LagartejaNo ratings yet
- Ethics Angeles MatrixDocument2 pagesEthics Angeles MatrixReg LagartejaNo ratings yet
- Letter of AuthorizationDocument3 pagesLetter of AuthorizationReg LagartejaNo ratings yet
- Drug Database - Potassium CitrateDocument2 pagesDrug Database - Potassium CitrateReg LagartejaNo ratings yet
- AcSU Endorsement WorksheetDocument2 pagesAcSU Endorsement WorksheetReg LagartejaNo ratings yet
- CASE: Electronic Timing, IncDocument4 pagesCASE: Electronic Timing, Inclee_syah50% (2)
- Bemonc FlowchartDocument1 pageBemonc FlowchartReg LagartejaNo ratings yet
- Epidemiology BooksDocument4 pagesEpidemiology BooksReg LagartejaNo ratings yet
- Nutrition Worksheet For Clerks 2018Document4 pagesNutrition Worksheet For Clerks 2018Reg LagartejaNo ratings yet
- TVM Exercises Chua H, Dijamco G, Legrateja R, Piad RDocument3 pagesTVM Exercises Chua H, Dijamco G, Legrateja R, Piad RReg LagartejaNo ratings yet
- Health and Safety of People Engaged in Work or EmploymentDocument7 pagesHealth and Safety of People Engaged in Work or EmploymentReg LagartejaNo ratings yet
- Epidemiology BooksDocument5 pagesEpidemiology BooksSrinivas RajanalaNo ratings yet
- Final Practice KeyDocument8 pagesFinal Practice KeyReg LagartejaNo ratings yet
- Background On Nutrition and History of CTCDocument67 pagesBackground On Nutrition and History of CTCReg LagartejaNo ratings yet
- Antenatal Care ServicesDocument1 pageAntenatal Care ServicesReg LagartejaNo ratings yet
- Parasite BiologyDocument1 pageParasite BiologyReg LagartejaNo ratings yet
- Chap 006Document15 pagesChap 006Neetu RajaramanNo ratings yet
- Bios TatDocument20 pagesBios TatmunendrajainNo ratings yet
- Chap 001Document17 pagesChap 001Neetu RajaramanNo ratings yet
- Nutri AnthropometryDocument11 pagesNutri AnthropometryReg LagartejaNo ratings yet
- 4 Practice Key 1Document2 pages4 Practice Key 1Reg LagartejaNo ratings yet
- Quiz Bowl Reg NotesDocument8 pagesQuiz Bowl Reg NotesReg LagartejaNo ratings yet
- Emerging and Re-EmergingDocument14 pagesEmerging and Re-EmergingReg LagartejaNo ratings yet
- Schedule Planner - Reg PDFDocument1 pageSchedule Planner - Reg PDFReg LagartejaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- GJRMI - Volume 1, Issue 10, October 2012Document98 pagesGJRMI - Volume 1, Issue 10, October 2012Windi Ayu AprillianiNo ratings yet
- ParkinsonDocument157 pagesParkinsonMassiel Alvarado100% (1)
- Placenta and Fetal Membrane-6614Document45 pagesPlacenta and Fetal Membrane-6614Incredible DivineNo ratings yet
- Patent EsDocument10 pagesPatent Esalcorrea2009No ratings yet
- General Pathology (Lecture-1) - 3Document14 pagesGeneral Pathology (Lecture-1) - 3Usman AkramNo ratings yet
- Parallel Evolution of Cannabinoid Biosynthesis: Nature PlantsDocument31 pagesParallel Evolution of Cannabinoid Biosynthesis: Nature PlantsPaulo EdsonNo ratings yet
- BS2001 Tutorial 1Document3 pagesBS2001 Tutorial 1cherlynNo ratings yet
- Cell Biology Product and Research Guide PDFDocument164 pagesCell Biology Product and Research Guide PDFBasma Al-KershNo ratings yet
- Primary Lymphoid Organs Generate Immune CellsDocument10 pagesPrimary Lymphoid Organs Generate Immune CellsKarthigaNo ratings yet
- 10 1126@science Aau3644Document14 pages10 1126@science Aau3644nicolasNo ratings yet
- Independent Expansion of The Keratin Gene Family in Teleostean Fish and Mammals An Insight From Phylogenetic Analysis and Radiation Hybrid Mapping of KeratinDocument9 pagesIndependent Expansion of The Keratin Gene Family in Teleostean Fish and Mammals An Insight From Phylogenetic Analysis and Radiation Hybrid Mapping of KeratinHabosha LoloNo ratings yet
- Plant Kingdom (L2) - 2nd JuneDocument43 pagesPlant Kingdom (L2) - 2nd JuneUpal PramanickNo ratings yet
- Julian Huxley and The Continuity of Eugenics in Twentieth-Century Britain'Document13 pagesJulian Huxley and The Continuity of Eugenics in Twentieth-Century Britain'Natalina Dass Tera Lodato100% (1)
- ICSE Class 10 Biology Previous Year Question Paper 2012Document10 pagesICSE Class 10 Biology Previous Year Question Paper 2012Bmt KingNo ratings yet
- Cell Structure Function2Document28 pagesCell Structure Function2Ritesh SinghNo ratings yet
- Delta Green - Autopsy of A ByakheeDocument4 pagesDelta Green - Autopsy of A ByakheeLuca LiperiNo ratings yet
- Definition of Cell CultureDocument36 pagesDefinition of Cell CultureGladys AilingNo ratings yet
- Revision For Mid Term Test 2.: Module: C - Importance of PlantsDocument10 pagesRevision For Mid Term Test 2.: Module: C - Importance of Plantsvenice tranNo ratings yet
- Cell MembraneDocument6 pagesCell MembraneÖmer KhanNo ratings yet
- Unit3 Lab DNAReplication Bio1Document6 pagesUnit3 Lab DNAReplication Bio1DuckyRoblox YTNo ratings yet
- Pathology of Diabetic Ketoacidosis - Romeo Rivera Jr.Document1 pagePathology of Diabetic Ketoacidosis - Romeo Rivera Jr.romeo riveraNo ratings yet
- Human Body Organs GuideDocument4 pagesHuman Body Organs GuideGMSUNDARINo ratings yet
- Test I. Blood Puzzle: Find The Words Listed Below in The Word SearchDocument2 pagesTest I. Blood Puzzle: Find The Words Listed Below in The Word SearchPilarieBernalNo ratings yet
- Q.P. Code: 684884Document1 pageQ.P. Code: 684884Priyanjali SainiNo ratings yet
- 04 Macromolecules-1Document53 pages04 Macromolecules-1keikisboyNo ratings yet
- GPB201 Unit-5 FullDocument51 pagesGPB201 Unit-5 FullAman MidhaNo ratings yet
- Pharmacology NotesDocument4 pagesPharmacology NotesKristoffer VelezNo ratings yet
- Tetracycline IntroductionDocument8 pagesTetracycline IntroductionNarendra Kumar S.No ratings yet
- HUMAN PHYSIOLOGY KEY FUNCTIONSDocument17 pagesHUMAN PHYSIOLOGY KEY FUNCTIONSplsssssNo ratings yet
- Robbins Notes: Aging, Radiation, and Inflammation Self StudyDocument44 pagesRobbins Notes: Aging, Radiation, and Inflammation Self StudyJustine HungNo ratings yet