Professional Documents
Culture Documents
Immunotherapy For Pulmonary TB
Uploaded by
adrip234Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Immunotherapy For Pulmonary TB
Uploaded by
adrip234Copyright:
Available Formats
1117
REVIEW
ISSN 1750-743X 10.2217/IMT.13.111 2013 Future Medicine Ltd Immunotherapy (2013) 5(10), 11171126
part of part of
Immunotherapy for pulmonary TB:
antimicrobial peptides and their inducers
TB is an infectious disease caused by Mycobac-
terium tuberculosis. TB has existed in humanity
for centuries. Despite this long relationship and
the huge advance in the knowledge of the etio-
logical agent, M. tuberculosis is still at the top of
the list of pathogens that causes huge mortal-
ity worldwide; every time a new anti-TB drug
comes aboard a new multidrug-resistant (MDR)
M. tuberculosis strain emerges. This makes it a
tough task for researchers to nd novel anti-TB
drugs. Vaccination is another strategy used to
eradicate TB; however, the only licensed vac-
cine currently is BCG, which is about 100 years
old and shows variable efcacy ranging from
0 to 80%. Altogether, these data suggest that
present strategies to eradicate TB should be
improved, and one promising approach is the
use of immunotherapeutics, which together with
conventional drugs and vaccines raise new hope.
Within these immunotherapeutic agents, anti-
microbial peptides (AMPs) are a very important
group due to their versatile activity. This article
will focus on the advances made in research of
AMPs and AMP inducers, and their use in TB
treatment.
Basic facts
AMPs are small cationic molecules of a vari-
able length. These peptides mainly constitute
polar-hydrophilic, nonpolar-hydrophobic and
positively charged amino acids. This special
conformation gives the molecule amphipathic
and cationic properties, which are very impor-
tant for their bactericidal activity [1]. AMPs are
broadly distributed in nature and all of them
share fundamental structural characteristics
that are very important for their broad-spectrum
antimicrobial activity, such as length (less than
60 amino acids), amphipathic structure and the
presence of cationic amino acids in their struc-
ture, providing them with a partial positive
charge. However, due to their secondary struc-
tural characteristics, AMPs could be divided into
subcategories that include: a-helical, peptides
enriched with repetition of one amino acid, and
peptides with intramolecular bonding formed
by cysteines. These features allow the AMPs to
interact with most microorganisms lipid bilayer
and eliminate them through membrane disrup-
tion or by translocating across the membrane
and inhibiting cytosolic targets [2,3].
Recent ndings show that the immunoregula-
tory activity is quite efcient since most of these
activities have an effect at the nanomolar scale,
acting over several innate immune response
receptors. Although at the beginning it was
thought that these functions were only focused
to promote proinammatory conditions, it is
now well known that some peptides, such as
cathel icidin have ambiguous functions pro-
moting, in certain cases, an anti-inammatory
response as well [47].
Antimicrobial activity of AMPs
As described above, AMPs share key biophysi-
cal properties that confer strong antimicrobial
activity, such as the presence of a positive or
cationic charge that permits chemoattraction
and electrostatic attachment to the bacterial
membrane. When the peptides are at a high
TB is an infectious disease that still has an enormous impact on public health worldwide. With the
continuous increasing epidemic of multidrug-resistant TB, new drugs and vaccines are urgently needed.
In the last decade there has been a broad advance in the knowledge of innate immunity in TB. Together
with the growing research regarding immunomodulators, new promising insights have been developed
that can contribute in the control of TB. This is the case of antimicrobial peptides, which can be potential
therapeutic or adjuvant agents. The current high cost of antimicrobial peptide synthesis may be a current
deterrent for treatment; antimicrobial peptide-inducers can be an alternative for low-cost treatment
and/or adjuvants.
KEYWORDS: antimicrobial peptides n defensins n HNP-1 n IDRs n L-isoleucine n LL-37
n TB immunotherapy n vaccines n vitamin D
Cesar Enrique
RivasSantago
1
, Rogelio
HernndezPando
2
& Bruno
RivasSantago*
3
1
Rutgers University School of Public
Health, Department of Environmental
& Occupatonal Health, Center for
Global Public Health, Piscataway,
NJ, USA
2
Department of Experimental
Pathology, Natonal Insttute of
Medical Sciences & Nutriton Salvador
Zubirn, Mexico City, Mexico
3
Medical Research Unit Zacatecas,
Mexican Insttute of Social
Security-IMSS, 45 Zacatecas,
cp.98000, Mexico
*Author for correspondence:
Tel.: +52 4929 226 019
rondo_vm@yahoo.com
For reprint orders, please contact: reprints@futuremedicine.com
Immunotherapy (2013) 5(10)
1118 future science group
REVIEW Rivas-Santiago, Hernndez-Pando & Rivas-Santiago
concentration, they can insert into the bacterial
membrane perpendicularly, causing alterations
in the lipid bilayer, making it permeable and
triggering bacterial death [3,8,9]. However, this
is not the only mechanism of action known for
AMPs; for example, it has been demonstrated
that members of the buforines and cathelicidins
family are able to cross the membrane and, in
the cytosol, they can bind to DNA and RNA
by electrostatic charges, interfering with vital
processes [10]. However, nucleic acids are not
the only intracellular target of AMPs; there are
peptides such as mersacidin that inhibits cell
wall synthesis by interaction with peptidogly-
can precursors [11]. Some other peptides, such
as PR-39, HNP-1 and -2, inhibit the synthesis
of very important proteins for bacterial viability
[12]. Finally, there is a group of AMPs described
recently, such as hepcidin, that not only pro-
duce damage in the bacterial cell membrane [13],
but also decrease the iron levels by negatively
regulating its intestinal absorption [14].
Immune regulatory functions
n Proinammatory
AMPs have been shown to act as chemoattract-
ants for cells of innate and adaptive immunity,
and in fact, many authors consider them as a
bridge between innate and adaptive immunity
[1518]. One of the most studied peptides has
been human cathelicidin LL-37 because of its
regulatory functions and being the only member
of the cathelicidin family present in humans.
LL-37 is capable of attracting neutrophils,
monocytes, T cells and mast cells using formyl
peptide receptor-like 1, and a distinct Gi-cou-
pled receptor at nanomolar concentrations [19,20].
Besides the remarkable chemotactic activity, it
also induces several other responses in leuko-
cytes and epithelial cells, modifying gene expres-
sion in order to improve or modulate immune
response. It has been reported that stimulation
of primary human monocytes and macrophages
with LL-37 led to the induction of a wide range
of chemokines, chemokine receptors and other
genes involved in cell adhesion, communication
and motility [21]. In fact, most of the encounters
between pathogenic microorganisms and cells
lead to LL-37 production, which in turn pro-
motes proinammatory chemokine production.
Along with cathelicidin, defensins have a wide
range of immuno regulatory activities owing
to their ability to engage several cell surface
receptors promoting chemotaxis, such as the
recruitment of immature dendritic cells (DCs)
and T lymphocytes after hbD-2 engagement to
the CCR6 receptors [22]. Moreover, hbD-3 can
downregulate CXCR4, which in certain condi-
tions, such as HIV-1 infection, may contribute to
avoiding virus infection [23]. In addition, APCs
undergo maturation in the presence of hbD-3
via Toll-like receptors (TLRs)-1 and -2. Fur-
thermore, murine b-defensin and hbD-3 have
been shown to act directly on immature DCs
as an endogenous ligand for TLR-4, -2 and -3,
inducing upregulation of costimulatory mole-
cules and DC maturation, triggering robust Th1
polarized adaptive immune responses in vivo
[24,25]. hbD-3 also has a high afnity for inter-
action with CCR2 on myeloid cells resulting in
chemoattraction in the absence of the natural
ligand-1/CCL2 [26]. Finally, hbD-3 can com-
pete with melanocyte-stimulating hormone a,
the natural ligand of melanocortin (MC1R) in
myeloid cells [27], which suggests that hbD-3
may inhibit anti-inammatory activity pro-
moted by melanocyte-stimulating hormone a
since this ligand has been shown to induce IL-10
in cells expressing the ligand of melanocortin.
Moreover, some peptides are capable of activat-
ing cells of the immune system through TLRs
[22,24,25,28] or inducing the production of chemo-
kines such as IL-8 [28]. In fact, our group, based
on this important characteristic, has found that
b-defensin-2 binds to DCs during early stages
of infection and promotes IFN-g production in
experimental TB [29], which has led us to design
vaccines using defensins as an adjuvant and
applying this vaccine to boost BCG with prom-
ising results [30]. These peptides with anti- and
pro-inammatory properties, such as b defen-
sins, can induce the release of prostaglandin D
2
and histamine in mast cells, which causes vas-
cular permeability triggering the inammatory
process [31,32].
n Anti-inammatory
Although many of the immunoregulatory
effects of AMPs are related to proinf lam-
matory responses, in the past few years the
anti-inammatory aspect of AMPs has been
demonstrated. For instance, defensins have
powerful anti-inammatory effects on human
monocytes, human monocyte-derived macro-
phages and human myeloid DCs [33]. In fact,
after phagocytic cells were treated with HNPs
after exposure to lipopolysaccharides (LPS), it
was observed that HNP-1 blocked the release
of IL-1b from LPS-activated monocytes, but
not the expression and release of TNF-a [34].
It has been demonstrated that apoptotic and
necrotic neutrophils inhibit the secretion of
www.futuremedicine.com 1119 future science group
Immunotherapy for pulmonary TB: antimicrobial peptides & their inducers REVIEW
proinammatory cytokines from macrophages
by releasing HNPs in the presence of both live
and dead whole bacteria; thus, HNPs inhibit
the LPS-mediated activation of macrophages
without affecting the release of proinamma-
tory cytokines by macrophages. Pingel et al.
found that hbD-3 attenuates the IL-6, IL-10,
GM-CSF and TNF-a response of human
myeloid DCs [35].
Similarly, LL-37 modulates host cell responses
to stimuli and also affects the action of endog-
enous immune mediators: IL-1b and GM-CSF.
This activity is dependent on the cell type and
activation status, timing of exposure and the
microenvironment. In certain cells, such as
monocytes, macrophages, DCs and B lympho-
cytes, it inhibits cellular responses to interferon,
showing suppression of cell activation and pro-
liferation, and production of proinammatory
and Th1-polarizing cytokines and antibodies.
It was further demonstrated in monocytes that
the suppressive effects of LL-37 were mediated
through inhibition of STAT1-independent
signaling events, involving both the p65 subunit
of NF-kB and p38 MAPK [7].
Another anti-inf lammatory function of
AMPs is mediated by their ability to bind anti-
genic molecules preventing the activation of
immune responses. One clear example of this
is the binding of cathelicidins and defensins to
LPS to prevent TNF-a secretion [36]. Addition-
ally, HNP-1 binds to Bacillus anthracis lethal
factor, inducing conformational changes that
prevents enzymatic conversion and protects
mice from B. anthracis lethal factor intoxication
and death [37]. HNP-1, HNP-3 and HD-5 bind
to toxin B from Clostridium inhibiting glycosy-
lation in vitro of Rho guanosine triphosphatases
[38]. FIGURE 1 outlines the different mechanisms of
action described for AMPs.
AMPs in TB
The pioneering studies to determine the rela-
tionship between AMPs and TB focused on the
antimycobacterial activity of AMPs. These stud-
ies were performed using nonpathogenic strains,
Direct antimicrobial effect by
pore formation in bacteria
Antimicrobial effect by inhibition of
replication transcription and translation
IFN-
IL-1
TNF-
IL-6
Inhibit cellular
response to
IFN-
Block secretion
of proinflammatory
cytokines in
monocytes and
macrophages
Maturation of
immature DC
Chemoattraction of
immune system cells;
neutrophils,T cells,
monocytes and DCs
AMPs
Proinflammatory effects
Anti-inflammatory effects
Antimicrobial effect
Figure 1. Diverse mechanisms of action of antimicrobial peptides. (A) The different
bactericidal effects observed in AMPs. Left: extracellular action; right: intracellular targets.
(B & C) The inammatory effects demonstrated by AMPs.
AMP: Antimicrobial peptide; DC: Dendritic cell.
Immunotherapy (2013) 5(10)
1120 future science group
REVIEW Rivas-Santiago, Hernndez-Pando & Rivas-Santiago
observing an important decrease in the bacilli
burden in an in vitro model [39]. However, it was
not until the year 2000, when pathogenic strains
were studied and an important effect against the
bacilli was demonstrated [40,41]. Thereafter, Kis-
ich et al. demonstrated that cellular synthesis
of hbD-2 after mRNA transfection to human
macrophages conferred efcient mycobactericidal
and mycobacteristatic activities [41]. Considering
that the rst cells that encounter M. tuberculosis
during primary infection are epithelial cells, our
group sought to determine whether these cells
used AMPs to counterattack infection. Both
in vitro and in vivo results showed that defensins
are very important in killing mycobacteria, and
a mouse strain that was susceptible to develop
TB demonstrated markedly lower levels of defen-
sins compared with the resistant strain. Working
with this murine model, we demonstrated that
during the early stages of disease there was high
expression of b-defensins, and this expression
strikingly decreased during late active infection,
which correlated with the severity of the disease
and the increase of pulmonary bacillary loads in
the mice. In a murine model of TB latent infec-
tion, a constant high production of defensins was
observed, which could be associated with bacil-
lary growth control due to reactivation induced
by corticosterone and the production of defensins
substantially decreased in coexistence with a high
increase of mycobacterial pulmonary loads [42].
Another very important AMP that has been
involved in the immuno pathogenesis of TB is
cathelicidin LL-37, as well as its mice ortholog
CRAMP. In the last few years our group has
studied these peptides, observing that myco-
bacteria induce the production of LL-37 in
human alveolar macrophages and the over-
production of this AMP will lead to bacterial
lysis during in vitro infection [43]; on the other
hand, our studies in the murine model have
shown that during M. tuberculosis infection,
there are three peaks of cathelicidin expression
at 1, 21 and 60 days postinfection. Intriguingly,
cathelicidin is highly expressed once the pneu-
monia is established; however, this high produc-
tion is not reected by a decrease of bacillary
loads in the lung, which probably means that
cathelicidin is acting more as an immunomodu-
lator rather than an anti microbial, promoting an
anti-inammatory response [44]. Similar results
were obtained in TB patients, in which they
showed high production of cathelicidin during
active disease, while in latent infected individuals
LL-37 levels were comparable with those found
in healthy donors [45].
Another important factor related to innate
immunity is that AMPs and TB control vita-
min D and its receptors. It has been shown that
stimulation of TLR-2 and -1 increase the expres-
sion of these receptors as well as the enzyme
Cyp27B1, which catalyzes the conversion to
the active form of vitamin D, and nally leads
to the induction of cathelicidin LL-37, increas-
ing the intracellular killing of the bacilli [46].
This group has also shown the direct partici-
pation of cathelicidin induction by vitamin D
in the intracellular killing of M. tuberculosis,
using interfering RNA specic for this AMP.
They observed that macrophages with silenced
cathelicidin had a higher bacillary burden com-
pared with macrophages that did not receive
the siRNA [47]. Conversely, M. tuberculosis-
infected mice treated with 1 mg/kg of LL-37
or CRAMP showed a modest decrease of bacilli
burden but pneumonia was increased consider-
ably [48]. Taken together these data suggest that
cathelicidin is essential for innate immunity
against mycobacteria; however, once the infec-
tion has been established cathelicidin promotes
an anti-inammatory response. Thus, LL-37 has
a dual effect in infection: during early infection
it increases phago cytosis, expression of costimu-
latory molecules in DCs and induces a higher
production of type Th1 cytokines [49]; and dur-
ing late infection, it inhibits TNF-a secretion
from monocytes as well as some other proinam-
matory cytokines [21]. Moreover, it reduces the
response of monocytes, macrophages and DC
to IFN-g [7], which is the principal cytokine of
the Th1 response. These characteristics show the
duality of cathelicidin during the infectious pro-
cess by avoiding inammation and contributing
directly to the elimination of the microorganism.
Recently our group demonstrated that the addi-
tion of LL-37 to noninfected macrophages led
to the production of proinammatory cytokines,
but when macrophages were highly infected, it
led to production of cytokines such as IL-10 and
TGF-b [Rivas-Santiago B, Unpublished Data]. These
experiments correlate with previous ndings in
experimental animal models [44].
Another potent AMP that has been stud-
ied in M. tuberculosis infection is hepcidin,
an AMP produced in the liver in response to
inammation and high concentrations of iron,
which is essential for bacilli growth and sur-
vival. Hepcidin is localized in the mycobacteria-
containing phagosome in macrophages and
inhibits M. tuberculosis growth in vitro by caus-
ing bacterial structural damage [13]. However,
macro phages are not the only cell of the innate
www.futuremedicine.com 1121 future science group
Immunotherapy for pulmonary TB: antimicrobial peptides & their inducers REVIEW
immune system that overproduce hepcidin when
infected by M. tuberculosis. Epithelial cells, such
as pneumocytes type 2, or DCs in mice, are able
to overexpress this AMP in response to some
components of the bacilli [50].
There are other kinds of AMPs that are
obtained synthetically by the fusion of dif-
ferent peptides [51], as well as by modication
of some amino acids in the structure of well-
known peptides, with the purpose of increasing
amphiphacity or by increasing their net positive
charge [52]. These modications have increased
the efciency of these AMPs against bacteria and
fungi [51,52]. Recently our group has tested these
semisynthetic peptides as promising antimyco-
bacterial compounds in our mouse TB model.
Some of these peptides showed magnicent
activity to eliminate mycobacteria both in vivo
and in vitro [48,53].
AMPs as therapeutics agents for
pulmonary TB
AMPs can be used as therapeutic agents admin-
istered as recombinant or synthetic protein, as
well as using inductors, which stimulate specic
cells for high AMP production and secretion.
A good example of an inductor is l-isoleucine,
which is an essential amino acid that has been
reported as a strong inductor of b-defensins in
bovine kidney epithelial cells [54]. Our results
showed that l-isoleucine signicantly induced
the production of these peptides in human pneu-
mocyte cultures and this induction was specic
for this amino acid as other amino acids with a
similar structure, such as d-isoleucine, did not
produce the same effects [54,55]. When l-isoleu-
cine was used therapeutically in M. tuberculosis-
infected mice with either a drug-sensitive or a
drug-resistant strain over 2 months, a signi-
cant decrease of pulmonary bacilli burdens and
reduction of tissue damage (pneumonia) was
observed in correlation with high expression of
b-defensins [55].
As mentioned above, vitamin D is a catheli-
cidin inducer not only in TB but also in several
infectious and noninfectious diseases. Indeed, it
has been demonstrated that reduced serum levels
of this vitamin are associated with the develop-
ment of active TB [56,57], and in the presence
of IFN-g and TNF-a, this vitamin induces
the production of AMP and bacilli elimina-
tion [46,58]. Recent meta-ana lysis reports dem-
onstrated that low serum vitamin D levels are
associated with a higher risk of active TB [56].
However, the use of vitamin D as a supplement
to increase the production of AMP was not as
effective as expected owing to a decrease in blood
LL-37 levels after vitamin administration [59].
The controversy among reports highlights the
different doses used for each study. Thus, Mily
et al. performed a dose-nding study and deter-
mined that 5000 IU once-daily vitamin D
3
is
the optimal dose for the induction of LL-37 on
macrophages and lymphocytes with efcient
intracellular M. tuberculosis killing by macro-
phages, and the effect is synergically increased
when vitamin D
3
is coadministered with 500 mg
of phenylbutyrate (PB) twice-daily [60].
The use of vitamin D as an immunomodula-
tor is a promising therapy for the treatment of
pulmonary TB; however, there are some issues
that should be considered before clinical tri-
als can start. As described above, cathelicidin
induced by vitamin D may contribute to the
production of anti-inf lammatory cytokines
during active disease, which could be detri-
mental; however, further studies need to be
carried out.
Although vitamin D is the most signicant
immunotherapeutic candidate to use in TB,
some other candidates have emerged. Previous
experimental studies have shown that down-
regulation of the rabbit cathelicidin (CAP-18) in
the large intestine and lung can be counteracted
by oral treatment with sodium butyrate, a short-
chain fatty acid and PB [61,62].With this back-
ground, Raqib et al. developed a clinical trial in
which sodium butyrate was used as an adjuvant
in the treatment against shigellosis, nding that
treatment with sodium butyrate led to a faster
reduction of inammation and that the decrease
in inammation and clinical illness could be
associated with the induced expression of LL-37
[63]. The same group further demonstrated that
PB can induce LL-37 expression synergistically
with 1,25 dihydroxyvitamin D
3
, at both pro-
tein and mRNA levels in a lung epithelial cell
line [64].
It is likely that an oral supplementation with
PB will boost innate immunity in the lung
mucosa by increasing expression of AMPs, and
M. tuberculosis killing and autophagy, and is
now being tested in a clinical trial of adults with
active pulmonary TB [60]. Owing to the impor-
tance of vitamin D as an immunotherapeutic,
different groups have developed different clinical
trials in pulmonary TB. The results obtained
are very variable; while some studies show the
evident role of vitamin D, in others it is not that
evident. Overal, it is probable that the admin-
istration of vitamin D as an adjuvant is helpful
just for patients with the tt genotype of the TaqI
Immunotherapy (2013) 5(10)
1122 future science group
REVIEW Rivas-Santiago, Hernndez-Pando & Rivas-Santiago
vitamin D receptor polymorphism [65]. Besides
that fact, the application of vitamin D could be
helpful as prophylaxis in latent TB [66]; however,
more clinical trials must be carried out taking
into account the ethnic origin of the group and
stage of the disease.
Another interesting use of AMP is in vac-
cination. Our group recently showed that
DNA vaccines containing coding sequences
for b-defensin-2 induce a strong Th1 adaptive
response against M. tuberculosis antigens, and
when these DNA vaccines were used as a booster
for immunization after BCG vaccination, a
signicant improvement of protection against
M. tuberculosis strains was produced. Since BCG
is the only vaccine for TB and has a reduced
efcacy to protect against pulmonary TB, this
new approach could greatly improve vaccination
efcacy against highly transmissible and virulent
strains. Thus, this study suggests that improve-
ment of BCG vaccination combined with DNA
vaccines in a prime-boost scheme is a good choice
for the rational design of a more efcient vaccine
against TB [30]. Further experiments need to be
carried out to assess the efcacy of this vaccine
as therapeutic rather than prophylactic.
Lantibiotics are AMPs synthetized by Gram-
positive bacteria and these peptides are charac-
terized by the presence of post-translationally
modied amino acids in their structure, such
as lanthionine and/or methyl lanthionine. The
most studied lantibiotic is nisin A, a peptide
produced by Lactococcus lactis, which in 1988
was considered safe for use as a food preserva-
tive. The mechanism of action of this AMP is
joining a cell wall precursor to lipid II, allowing
pore formation and at the same time inhibit-
ing biosynthesis of the bacterial cell wall [67,68].
Nisin A and its synthetic derivatives nisin S
and nisin T are efcient lantibiotics against
M. tuberculosis and non-TB bacteria, and they
constitute interesting compounds for clinical
studies [69].
In the last 5 years, the boom of innate
defense regulator peptides (IDRs) has brought
promising immunoregulatory alternatives for
infectious disease including TB [53]. IDRs are
synthetic immunoregulatory and anti-infective
peptides that are based on the sequences of
natural AMPs. IDRs were originally designed
as antibiotics, but many of them also have
immuno regulatory activities and their in vivo
functions may ultimately be mediated through
a combination of both functions [7072]. In
recent studies, it has been demonstrated that
the protective activity of IDRs could be solely
based on their immuno modulatory properties
and that this protection is functional even in
animals infected with MDR strains [73]. Besides
this immuno regulatory property, the low poten-
tial of microbial resistance, lower toxicity and
requirement of fewer doses, suggest that IDRs
could be used as a treatment and as an adjuvant,
as well as for conventional drug-sensitive, but
Table 1. Relevance of antimicrobial peptides in TB.
Antimicrobial
peptide
Source Activity Importance in TB Ref.
Human neutrophil
peptides
Neutrophils Bactericidal effect, chemotaxis and
activation of DCs and DNA-binding
Possible adjuvant in anti-TB
chemotherapy
[7477]
b-defensin-2 Epithelial cells Bactericidal effect, chemotaxis of a
wide range of leukocytes through
CCR2 and CCR6, and activation
of DCs
Induction of this antimicrobial peptide
reduce mycobacterial loads
[22,25,41,55,78]
b-defensin-3 Epithelial cells Bactericidal effect, and chemotaxis
of monocytes, macrophages and
neutrophils through CCR2
Owing to its chemotactic effect, this
antimicrobial peptide could be used as
immunotherapy
[78,79]
LL-37 Alveolar macrophages,
MDM and alveolar
epithelial cells
Bactericidal effect and modulation
of immune response
A decrease in bacterial load was
observed when applied as a therapy in
infected mice
[7,48]
E2, E6 and CP26 Synthetic peptides Bactericidal effect by disruption in
cell wall of the bacteria
Application of these peptides
signicantly reduces the lung bacillary
loads
[48,80]
Innate defense
regulator peptides
Synthetic peptides Immunomodulatory functions by
the induction of chemokines
In animal models, reduced bacillary
loads as well as inammation by
decreased pneumonia
[53,70,81,82]
DC: Dendritic cell; MDM: Monocyte-derived macrophage.
www.futuremedicine.com 1123 future science group
Immunotherapy for pulmonary TB: antimicrobial peptides & their inducers REVIEW
mainly MDR, strains combining their antimi-
crobial and wound healing properties to treat
deep sores and ulcers [73]. Several in vitro and
in vivo experiments have tested the efcacy of
IDRs in experimental TB with pathogenic and
MDR strains. In a murine model of progres-
sive pulmonary TB, the intratracheal adminis-
tration of the IDR peptides E2, E6 and CP26
during late disease in mice infected with drug-
sensitive M. tuberculosis or MDR strains signi-
cantly reduced lung bacillary loads. However,
there was no reduction in the inammatory
infiltrate (pneumonia) compared with con-
trol nontreated mice [48]. Further experiments
demonstrated that the use of some IDRs, such
as HH2 or 1018, not only decreased bacillary
loads but also pneumonic areas, therefore they
are candidates for testing in humans [53]. TABLE 1
shows a summary of the different AMPs and
their importance in TB.
Potential disadvantages of
immunotherapy using AMPs for TB
Although it seems that AMPs and their inducers
could be used as a treatment against TB and that
these options could help to eradicate this dis-
ease, currently this is quite far off. Even though
there is greater knowledge of the relationship
between TB and AMPs, there are many gaps
that need to be lled before applying clinical
approaches. For instance, it is still unknown
which peptides could be used for each stage
of the disease, since some peptides have anti-
inammatory effects whereas others have proin-
ammatory effects. The induction of inamma-
tion during progressive TB would accelerate the
pneumonic process in the patient. Therefore, the
design of precise AMPs for specic stages of TB
must take place. Furthermore, it is known that
M. tuberculosis develops resistance to antibiotics
under evolutive pressure; AMPs would not be
an exception and this would mainly be seen in
developing countries where a medical prescrip-
tion is not necessary to have access to antibiotics.
In summary, basic investigation and new health
policies are essential before AMPs are used as
immunotherapy.
Future perspective
Although many issues remain to be studied
regarding AMPs and their inducers for the
immunotherapy of TB, this topic is a promising
alternative for the control of M. tuberculosis infec-
tion mainly by MDR strains; therefore, for future
studies it will be necessary to include these kinds
of strains. Another important point to assess is
which peptides could be used for each specic
stage of the pulmonary disease to avoid unnec-
essary inammation that could impair patient
health. In this case, IDRs are a good option, but
further clinical studies are needed. It is widely
demonstrated that vitamin D and l-isoleucine
have undoubted in vitro effects, inducing AMPs
that lead to M. tuberculosis killing. However, both
these molecules must be studied further in clini-
cal trials in people of different ethnic origins and
it will be necessary to determine whether these
molecules have synergic effects with convectional
antimycobacterial drugs. Finally, the way AMPs
or AMP inducers are delivered is likely to inu-
ence their effectiveness, thus efcient routes of
delivery need to be studied.
Conclusion
The possibility of the use of AMPs, AMP induc-
ers and IDRs for the treatment of pulmonary
TB is increasing, partly owing to the exten-
sive research on innate immunity of TB. The
improvement of low-cost peptide synthesis and
peptide development companies are advanc-
ing therapeutic candidates that are relatively
short-sequenced, do not require folding, such
as disulde bonds, and are required in low
concentrations to be effective. The ana lysis of
costbenet when compared with second- and
third-generation antibiotics used for the treat-
ment of MDR and extensively drug-resistant
strains should be also considered.
There is signicant therapeutic potential for
the use of AMPs. The issues that must be over-
come are not trivial and include cost of goods,
stability, toxicity and delivery. However, these
issues are the same for any drug development
candidate, but are likely to be overcome with
advances in drug delivery, and with limitations
as well as the attributes of innate immunity
peptides.
Acknowledgements
The authors thank PA Cantarella IV (Rutgers University
School of Public Health) for reviewing the manuscript.
Financial & competing interests disclosure
The authors have no relevant afliations or nancial
involvement with any organization or entity with a nan-
cial interest in or nancial conict with the subject matter
or materials discussed in the manuscript. This includes
employment, consultancies, honoraria, stock ownership or
options, expert testimony, grants or patents received or
pending, or royalties.
No writing assistance was utilized in the production of
this manuscript.
Immunotherapy (2013) 5(10)
1124 future science group
REVIEW Rivas-Santiago, Hernndez-Pando & Rivas-Santiago
References
Papers of special note have been highlighted as:
n
of interest
nn
of considerable interest
1 Shai Y. Mechanism of the binding, insertion
and destabilization of phospholipid bilayer
membranes by alpha-helical antimicrobial and
cell non-selective membrane-lytic peptides.
Biochim. Biophys. Acta 1462(12), 5570
(1999).
n
Describes the different models that explain
the mechanisms of insertion and pore
formation of antimicrobial peptides (AMPs),
which are fundamental steps for the
destabilization of the phospholipid bilayer.
2 Bi X, Wang C, Ma L, Sun Y, Shang D.
Investigation of the role of tryptophan
residues in cationic antimicrobial peptides to
determine the mechanism of antimicrobial
action. J. Appl. Microbiol. 115(3), 663672
(2013).
3 Zasloff M. Antimicrobial peptides of
multicellular organisms. Nature 415(6870),
389395 (2002).
nn
Very interesting recompilation of papers,
describing the characteristics, properties,
mechanisms of action, distribution and
nature of AMPs.
4 Zanetti M. Cathelicidins, multifunctional
peptides of the innate immunity. J. Leukoc.
Biol. 75(1), 3948 (2004).
5 Zheng Y, Niyonsaba F, Ushio H et al.
Cathelicidin LL-37 induces the generation of
reactive oxygen species and release of human
alpha-defensins from neutrophils.
Br. J. Dermatol. 157(6), 11241131 (2007).
6 Brown KL, Poon GF, Birkenhead D et al.
Host defense peptide LL-37 selectively
reduces proinammatory macrophage
responses. J. Immunol. 186(9), 54975505
(2011).
7 Nijnik A, Pistolic J, Wyatt A, Tam S,
Hancock RE. Human cathelicidin peptide
LL-37 modulates the effects of IFN-gamma
on APCs. J. Immunol. 183(9), 57885798
(2009).
8 Brogden KA. Antimicrobial peptides: pore
formers or metabolic inhibitors in bacteria?
Nat. Rev. Microbiol. 3(3), 238250 (2005).
9 Reddy KV, Yedery RD, Aranha C.
Antimicrobial peptides: premises and
promises. Int. J. Antimicrob. Agents 24(6),
536547 (2004).
10 Park CB, Kim HS, Kim SC. Mechanism of
action of the antimicrobial peptide buforin ii:
buforin ii kills microorganisms by penetrating
the cell membrane and inhibiting cellular
functions. Biochem. Biophys. Res. Commun.
244(1), 253257 (1998).
n
Describes a different mechanism of action
for bacterial killing of AMPs that is related
to DNA binding.
11 Brotz H, Bierbaum G, Leopold K,
Reynolds PE, Sahl HG. The lantibiotic
mersacidin inhibits peptidoglycan synthesis
by targeting lipid II. Antimicrob. Agents
Chemother. 42(1), 154160 (1998).
12 Lehrer RI, Barton A, Daher KA, Harwig SS,
Ganz T, Selsted ME. Interaction of human
defensins with Escherichia coli. Mechanism of
bactericidal activity. J. Clin. Invest. 84(2),
553561 (1989).
nn
First report that relates AMPs with the
killing of bacteria. Pore formation as a
mechanism of action is also elucidated.
13 Sow FB, Florence WC, Satoskar AR,
Schlesinger LS, Zwilling BS, Lafuse WP.
Expression and localization of hepcidin in
macrophages: a role in host defense against
tuberculosis. J. Leukoc. Biol. 82(4), 934945
(2007).
14 Yamaji S, Sharp P, Ramesh B, Srai SK.
Inhibition of iron transport across human
intestinal epithelial cells by hepcidin. Blood
104(7), 21782180 (2004).
15 Bowdish DM, Davidson DJ, Hancock RE.
Immunomodulatory properties of defensins
and cathelicidins. Curr. Top. Microbiol.
Immunol. 306, 2766 (2006).
n
Review of articles where the different
immunoregulatory properties that possess
AMPs, including chemotaxis and cellular
activation, are described.
16 Vandamme D, Landuyt B, Luyten W,
Schoofs L. A comprehensive summary of LL-37,
the factotum human cathelicidin peptide. Cell.
Immunol. 280(1), 2235 (2012).
17 Mookherjee N, Lippert DN, Hamill P et al.
Intracellular receptor for human host defense
peptide LL-37 in monocytes. J. Immunol.
183(4), 26882696 (2009).
18 Bowdish DM, Davidson DJ, Scott MG,
Hancock RE. Immunomodulatory activities of
small host defense peptides. Antimicrob. Agents
Chemother. 49(5), 17271732 (2005).
19 Niyonsaba F, Iwabuchi K, Someya A et al.
A cathelicidin family of human antibacterial
peptide LL-37 induces mast cell chemotaxis.
Immunology 106(1), 2026 (2002).
20 De Y, Chen Q, Schmidt Ap et al. LL-37, the
neutrophil granule- and epithelial cell-derived
cathelicidin, utilizes formyl peptide receptor-like
1 (fprl1) as a receptor to chemoattract human
peripheral blood neutrophils, monocytes, and
T cells. J. Exp. Med. 192(7), 10691074 (2000).
21 Mookherjee N, Brown KL, Bowdish DM et al.
Modulation of the TLR-mediated inammatory
response by the endogenous human host defense
peptide LL-37. J. Immunol. 176(4), 24552464
(2006).
22 Yang D, Chertov O, Bykovskaia SN et al.
Beta-defensins: linking innate and adaptive
immunity through dendritic and T cell CCR6.
Science 286(5439), 525528 (1999).
23 Feng Z, Dubyak GR, Lederman MM,
Weinberg A. Cutting edge: human beta
defensin 3 a novel antagonist of the HIV-1
coreceptor CXCR4. J. Immunol. 177(2),
782786 (2006).
24 Funderburg N, Lederman MM, Feng Z et al.
Human-defensin-3 activates professional
Executive summary
TB is one of the most important infectious diseases and is responsible for 1.8 million deaths worldwide annually.
In the last decade new multidrug-resistant strains have emerged, consequently making it a very hard task to eradicate TB.
The use of antimicrobial peptides (AMPs) and AMP inducers are a promising option for the immunotherapy of TB by using them as
direct antimicrobial molecules, as well as immunomodulators.
AMPs possess both pro- and anti-inammatory properties, which can be convenient for the immunotherapy of TB.
The use of defensins as adjuvants in a prime-boost scheme is a good choice for the rational design of more efcient vaccines
against TB.
The use of innate defense regulator peptides can be a good option to promote Mycobacterium tuberculosis elimination; using them as
immunotherapy avoids undesirable effects, such as inammation.
The use of AMP inducers, such as vitamin D and L-isoleucine, are a good option since all in vitro studies demonstrate their efcacy to
induce AMPs and kill M. tuberculosis through several mechanisms; however, clinical studies are controversial, therefore further clinical
studies are needed.
www.futuremedicine.com 1125 future science group
Immunotherapy for pulmonary TB: antimicrobial peptides & their inducers REVIEW
www.futuremedicine.com
antigen-presenting cells via Toll-like receptors 1
and 2. Proc. Natl Acad. Sci. USA 104(47),
1863118635 (2007).
25 Biragyn A, Rufni PA, Leifer CA et al. Toll-
like receptor 4-dependent activation of
dendritic cells by beta-defensin 2. Science
298(5595), 10251029 (2002).
26 Jin G, Kawsar HI, Hirsch SA et al.
An antimicrobial peptide regulates tumor-
associated macrophage trafcking via the
chemokine receptor CCR2, a model for
tumorigenesis. PLoS ONE 5(6), e10993 (2010).
27 Swope VB, Jameson JA, McFarland KL et al.
Dening MC1R regulation in human
melanocytes by its agonist alpha-melanocortin
and antagonists agouti signaling protein and
beta-defensin 3. J. Invest. Dermatol. 132(9),
22552262 (2012).
28 Tjabringa GS, Aarbiou J, Ninaber DK et al.
The antimicrobial peptide LL-37 activates
innate immunity at the airway epithelial
surface by transactivation of the epidermal
growth factor receptor. J. Immunol. 171(12),
66906696 (2003).
29 Rivas-Santiago B, Cervantes-Villagrana A,
Sada E, Hernndez-Pando R. Expression of
beta defensin 2 in experimental pulmonary
tuberculosis: tentative approach for vaccine
development. Arch. Med. Res. 43(4), 324328
(2012).
30 Cervantes-Villagrana AR, Hernndez-
Pando R, Biragyn A et al. Prime-boost bcg
vaccination with DNA vaccines based in
beta-defensin-2 and mycobacterial antigens
esat6 or ag85b improve protection in a
tuberculosis experimental model. Vaccine
31(4), 676684 (2013).
nn
For the rst time, defensin is used as an
adjuvant for Bacillus CalmetteGurin, with
results suggesting its future use for TB
vaccination.
31 Chen X, Niyonsaba F, Ushio H et al.
Antimicrobial peptides human beta-defensin
(hbd)-3 and hbd-4 activate mast cells and
increase skin vascular permeability.
Eur. J. Immunol. 37(2), 434444 (2007).
32 Niyonsaba F, Someya A, Hirata M, Ogawa H,
Nagaoka I. Evaluation of the effects of
peptide antibiotics human beta-defensins-1/-2
and LL-37 on histamine release and
prostaglandin d(2) production from mast
cells. Eur. J. Immunol. 31(4), 10661075
(2001).
33 Kohlgraf KG, Pingel LC, Dietrich DE,
Brogden KA. Defensins as anti-inammatory
compounds and mucosal adjuvants. Future
Microbiol. 5(1), 99113 (2010).
34 Shi J, Aono S, Lu W et al. A novel role for
defensins in intestinal homeostasis: regulation
of IL-1beta secretion. J. Immunol. 179(2),
12451253 (2007).
35 Pingel LC, Kohlgraf KG, Hansen CJ et al.
Human beta-defensin 3 binds to
hemagglutinin b (rhagb), a non-mbrial
adhesin from porphyromonas gingivalis, and
attenuates a pro-inammatory cytokine
response. Immunol. Cell Biol. 86(8), 643649
(2008).
36 Motzkus D, Schulz-Maronde S, Heitland A
et al. The novel beta-defensin defb123
prevents lipopolysaccharide-mediated effects
in vitro and in vivo. FASEB J. 20(10),
17011702 (2006).
37 Kim C, Gajendran N, Mittrucker HW et al.
Human alpha-defensins neutralize anthrax
lethal toxin and protect against its fatal
consequences. Proc. Natl Acad. Sci. USA
102(13), 48304835 (2005).
n
Emphasizes the importance of AMPs, not
only for their antimicrobial and
immunoregulatory activities, but also for
their capability to neutralize toxins.
38 Giesemann T, Guttenberg G, Aktories K.
Human alpha-defensins inhibit Clostridium
difcile toxin B. Gastroenterology 134(7),
20492058 (2008).
39 Ogata K, Linzer BA, Zuberi RI, Ganz T,
Lehrer RI, Catanzaro A. Activity of defensins
from human neutrophilic granulocytes against
Mycobacterium aviumMycobacterium
intracellulare. Infect. Immun. 60(11),
47204725 (1992).
40 Sharma S, Verma I, Khuller GK. Antibacterial
activity of human neutrophil peptide-1 against
Mycobacterium tuberculosis h37rv: in vitro and
ex vivo study. Eur. Respir. J. 16(1), 112117
(2000).
41 Kisich KO, Heifets L, Higgins M,
Diamond G. Antimycobacterial agent based
on mRNA encoding human beta-defensin 2
enables primary macrophages to restrict
growth of Mycobacterium tuberculosis. Infect.
Immun. 69(4), 26922699 (2001).
42 Rivas-Santiago B, Schwander SK, Sarabia C
et al. Human {beta}-defensin 2 is expressed
and associated with Mycobacterium tuberculosis
during infection of human alveolar epithelial
cells. Infect. Immun. 73(8), 45054511 (2005).
43 Rivas-Santiago B, Hernndez-Pando R,
Carranza C et al. Expression of cathelicidin
LL-37 during Mycobacterium tuberculosis
infection in human alveolar macrophages,
monocytes, neutrophils, and epithelial cells.
Infect. Immun. 76(3), 935941 (2008).
44 Castaneda-Delgado J, Hernndez-Pando R,
Serrano CJ et al. Kinetics and cellular sources
of cathelicidin during the course of
experimental latent tuberculous infection and
progressive pulmonary tuberculosis. Clin. Exp.
Immunol. 161(3), 542550 (2010).
45 Gonzalez-Curiel I, Castaeda-Delgado J,
Lopez-Lopez N et al. Differential expression of
antimicrobial peptides in active and latent
tuberculosis and its relationship with diabetes
mellitus. Hum. Immunol. 72(8), 656662
(2011).
46 Liu PT, Stenger S, Li H et al. Toll-like receptor
triggering of a vitamin d-mediated human
antimicrobial response. Science 311(5768),
17701773 (2006).
47 Liu PT, Stenger S, Tang DH, Modlin RL.
Cutting edge: vitamin d-mediated human
antimicrobial activity against Mycobacterium
tuberculosis is dependent on the induction of
cathelicidin. J. Immunol. 179(4), 20602063
(2007).
48 Rivas-Santiago B, Rivas-Santiago CE,
Castaeda-Delgado JE, Leon-Contreras JC,
Hancock RE, Hernndez-Pando R. Activity of
LL-37, cramp and antimicrobial peptide-
derived compounds e2, e6 and cp26 against
Mycobacterium tuberculosis. Int. J. Antimicrob.
Agents 41(2), 143148 (2013).
n
Use of synthetic AMPs as treatment against
TB in a murine model using drug-sensitive
and multidrug-resistant strains, obtaining an
important decrease in lung bacillary loads.
49 Davidson DJ, Currie AJ, Reid GS et al.
The cationic antimicrobial peptide LL-37
modulates dendritic cell differentiation and
dendritic cell-induced T cell polarization.
J. Immunol. 172(2), 11461156 (2004).
50 Sow FB, Nandakumar S, Velu V et al.
Mycobacterium tuberculosis components
stimulate production of the antimicrobial
peptide hepcidin. Tuberculosis (Edinb.) 91(4),
314321 (2011).
51 Friedrich C, Scott MG, Karunaratne N,
Yan H, Hancock RE. Salt-resistant
alpha-helical cationic antimicrobial peptides.
Antimicrob. Agents Chemother. 43(7),
15421548 (1999).
52 Hilpert K, Volkmer-Engert R, Walter T,
Hancock RE. High-throughput generation of
small antibacterial peptides with improved
activity. Nat. Biotechnol. 23(8), 10081012
(2005).
53 Rivas-Santiago B, Castaeda-Delgado JE,
Rivas-Santiago CE et al. Ability of innate
defence regulator peptides IDR-1002,
IDR-HH2 and IDR-1018 to protect against
Mycobacterium tuberculosis infections in
animal models. PLoS ONE 8(3), e59119
(2013).
54 Fehlbaum P, Rao M, Zasloff M,
Anderson GM. An essential amino acid
induces epithelial beta-defensin expression.
Proc. Natl Acad. Sci. USA 97(23),
1272312728 (2000).
55 Rivas-Santiago CE, Rivas-Santiago B,
Leon DA, Castaeda-Delgado J, Hernndez
Pando R. Induction of beta-defensins by
l-isoleucine as novel immunotherapy in
Immunotherapy (2013) 5(10)
1126 future science group
REVIEW Rivas-Santiago, Hernndez-Pando & Rivas-Santiago
experimental murine tuberculosis. Clin. Exp.
Immunol. 164(1), 8089 (2011).
nn
First report on the induction of AMPs as
immunotherapy against TB in vivo, using
drug-sensitive strains, as well as
multidrug-resistant strains.
56 Nnoaham KE, Clarke A. Low serum
vitamin D levels and tuberculosis:
a systematic review and meta-ana lysis.
Int. J. Epidemiol. 37(1), 113119 (2008).
57 Yamshchikov AV, Kurbatova EV, Kumari M
et al. Vitamin D status and antimicrobial
peptide cathelicidin (LL-37) concentrations
in patients with active pulmonary
tuberculosis. Am. J. Clin. Nutr. 92(3),
603611 (2010).
58 Denis M. Killing of Mycobacterium
tuberculosis within human monocytes:
activation by cytokines and calcitriol.
Clin. Exp. Immunol. 84(2), 200206 (1991).
59 Larcombe L, Orr P, Turner-Brannen E,
Slivinski CR, Nickerson PW, Mookherjee N.
Effect of vitamin D supplementation on
Mycobacterium tuberculosis-induced innate
immune responses in a Canadian Den First
Nations cohort. PLoS ONE 7(7), e40692
(2012).
60 Mily A, Rekha RS, Kamal Sm et al. Oral
intake of phenylbutyrate with or without
vitamin D3 upregulates the cathelicidin
LL-37 in human macrophages: a dose nding
study for treatment of tuberculosis. BMC
Pulm. Med. 13, 23 (2013).
61 Raqib R, Sarker P, Bergman P et al. Improved
outcome in shigellosis associated with
butyrate induction of an endogenous peptide
antibiotic. Proc. Natl Acad. Sci. USA 103(24),
91789183 (2006).
62 Sarker P, Ahmed S, Tiash S et al.
Phenylbutyrate counteracts Shigella mediated
downregulation of cathelicidin in rabbit lung
and intestinal epithelia: a potential
therapeutic strategy. PLoS ONE 6(6), e20637
(2011).
63 Raqib R, Sarker P, Mily A et al. Efcacy of
sodium butyrate adjunct therapy in
shigellosis: a randomized, double-blind,
placebo-controlled clinical trial. BMC Infect.
Dis. 12, 111 (2012).
n
Report of a clinical trial where the induction
of AMPs (cathelicidins) as an adjuvant in
treatment of shigellosis is described, nding
signicant improvements in patients that
received the adjuvant treatment.
64 Steinmann J, Halldorsson S, Agerberth B,
Gudmundsson GH. Phenylbutyrate induces
antimicrobial peptide expression. Antimicrob.
Agents Chemother. 53(12), 51275133 (2009).
65 Martineau AR, Timms PM, Bothamley GH
et al. High-dose vitamin D(3) during
intensive-phase antimicrobial treatment of
pulmonary tuberculosis: a double-blind
randomised controlled trial. Lancet
377(9761), 242250 (2011).
66 Ganmaa D, Giovannucci E, Bloom BR et al.
Vitamin D, tuberculin skin test conversion,
and latent tuberculosis in mongolian school-
age children: a randomized, double-blind,
placebo-controlled feasibility trial.
Am. J. Clin. Nutr. 96(2), 391396 (2012).
67 Asaduzzaman SM, Sonomoto K. Lantibiotics:
diverse activities and unique modes of action.
J. Biosci. Bioeng. 107(5), 475487 (2009).
68 Breukink E, Wiedemann I, van Kraaij C,
Kuipers OP, Sahl H, de Kruijff B. Use of the
cell wall precursor lipid ii by a pore-forming
peptide antibiotic. Science 286(5448),
23612364 (1999).
69 Carroll J, Field D, OConnor PM et al. Gene
encoded antimicrobial peptides, a template
for the design of novel anti-mycobacterial
drugs. Bioeng. Bugs 1(6), 408412 (2010).
70 Kindrachuk J, Jenssen H, Elliott M et al.
A novel vaccine adjuvant comprised of a
synthetic innate defence regulator peptide and
cpg oligonucleotide links innate and adaptive
immunity. Vaccine 27(34), 46624671
(2009).
71 Cao D, Li H, Jiang Z et al. Synthetic innate
defence regulator peptide enhances in vivo
immunostimulatory effects of cpg-odn in
newborn piglets. Vaccine 28(37), 60066013
(2010).
72 Yang J, Mao M, Zhang S et al. Innate defense
regulator peptide synergizes with cpg odn for
enhanced innate intestinal immune responses
in neonate piglets. Int. Immunopharmacol.
12(2), 415424 (2012).
73 Hancock RE, Nijnik A, Philpott DJ.
Modulating immunity as a therapy for
bacterial infections. Nat. Rev. Microbiol.
10(4), 243254 (2012).
74 Kalita A, Verma I, Khuller GK. Role of
human neutrophil peptide-1 as a possible
adjunct to antituberculosis chemotherapy.
J. Infect. Dis. 190(8), 14761480 (2004).
75 Sharma S, Verma I, Khuller GK. Therapeutic
potential of human neutrophil peptide 1
against experimental tuberculosis. Antimicrob.
Agents Chemother. 45(2), 639640 (2001).
76 Presicce P, Giannelli S, Taddeo A, Villa ML,
Della Bella S. Human defensins activate
monocyte-derived dendritic cells, promote the
production of proinammatory cytokines, and
up-regulate the surface expression of CD91.
J. Leukoc. Biol. 86(4), 941948 (2009).
77 Sharma S, Khuller G. DNA as the
intracellular secondary target for antibacterial
action of human neutrophil peptide-i against
Mycobacterium tuberculosis h37ra. Curr.
Microbiol. 43(1), 7476 (2001).
78 Rohrl J, Yang D, Oppenheim JJ, Hehlgans T.
Human beta-defensin 2 and 3 and their
mouse orthologs induce chemotaxis through
interaction with CCR2. J. Immunol. 184(12),
66886694 (2010).
79 Soruri A, Grigat J, Forssmann U, Riggert J,
Zwirner J. Beta-defensins chemoattract
macrophages and mast cells but not
lymphocytes and dendritic cells: CCR6 is not
involved. Eur. J. Immunol. 37(9), 24742486
(2007).
80 Spindler EC, Hale JD, Giddings TH Jr,
Hancock RE, Gill RT. Deciphering the mode
of action of the synthetic antimicrobial
peptide bac8c. Antimicrob. Agents Chemother.
55(4), 17061716 (2011).
81 Nijnik A, Madera L, Ma S et al. Synthetic
cationic peptide idr-1002 provides protection
against bacterial infections through
chemokine induction and enhanced leukocyte
recruitment. J. Immunol. 184(5), 25392550
(2010).
82 Achtman AH, Pilat S, Law CW et al.
Effective adjunctive therapy by an innate
defense regulatory peptide in a preclinical
model of severe malaria. Science Transl. Med.
4(135), 135ra164 (2012).
Reproduced with permission of the copyright owner. Further reproduction prohibited without
permission.
You might also like
- Intestinal Absorption of Vitamin D 2018Document17 pagesIntestinal Absorption of Vitamin D 2018adrip234No ratings yet
- Emotional Tears TIMINGDocument8 pagesEmotional Tears TIMINGadrip234No ratings yet
- Bolus-Dose Vitamin D and Prevention of Childhood PneumoniaDocument4 pagesBolus-Dose Vitamin D and Prevention of Childhood Pneumoniaadrip234No ratings yet
- Hypophosphatasia The Disease in AdultsDocument6 pagesHypophosphatasia The Disease in Adultsadrip234No ratings yet
- VITAMIN D Vitamin D Immunomodulatory Actions and New Potentialities FileDocument2 pagesVITAMIN D Vitamin D Immunomodulatory Actions and New Potentialities Fileadrip234No ratings yet
- Vitamin D An Overview of Vitamin D Status EUROPEDocument29 pagesVitamin D An Overview of Vitamin D Status EUROPEadrip234No ratings yet
- DSM 42e 09 DSM Nutrition Award 2009Document2 pagesDSM 42e 09 DSM Nutrition Award 2009adrip234No ratings yet
- Y2012-074 Nutrition and The Healthy Heart With An ExerciseDocument10 pagesY2012-074 Nutrition and The Healthy Heart With An Exerciseadrip234No ratings yet
- Vitamin D and Chronic Obstructive Pulmonary DiseaseDocument4 pagesVitamin D and Chronic Obstructive Pulmonary Diseaseadrip234No ratings yet
- Adult Hypophosphatasia and A Low RBC Tiamine PyrophosphateDocument4 pagesAdult Hypophosphatasia and A Low RBC Tiamine Pyrophosphateadrip234No ratings yet
- Contents 2017 Endocrinology and Metabolism Clinics of North AmericaDocument4 pagesContents 2017 Endocrinology and Metabolism Clinics of North Americaadrip234No ratings yet
- Vitamin D in Health and DiseaseDocument1 pageVitamin D in Health and Diseaseadrip234No ratings yet
- Adult Hypophosphatasia and A Low RBC Tiamine PyrophosphateDocument4 pagesAdult Hypophosphatasia and A Low RBC Tiamine Pyrophosphateadrip234No ratings yet
- Caveolin 1 Regulates 5-MediatedDocument14 pagesCaveolin 1 Regulates 5-Mediatedadrip234No ratings yet
- Internalsecretio00gley PDFDocument264 pagesInternalsecretio00gley PDFadrip234No ratings yet
- Life Is A Huge CompromiseDocument5 pagesLife Is A Huge CompromiseAnonymous wvs8SG65No ratings yet
- Varlberg Carsten 2014 IntroducereDocument2 pagesVarlberg Carsten 2014 Introducereadrip234No ratings yet
- Chronology of Advances Neuroendocrine ImmunomodulationDocument11 pagesChronology of Advances Neuroendocrine Immunomodulationadrip234No ratings yet
- The Mitochondrion As A Primary Site NEUROIMMUNOMODULATIONDocument11 pagesThe Mitochondrion As A Primary Site NEUROIMMUNOMODULATIONadrip234No ratings yet
- The Coinage of The Genoese SettlementsDocument12 pagesThe Coinage of The Genoese SettlementsMarco GianasiNo ratings yet
- Vitamin D An Innate Antiviral Agent SuppressingDocument10 pagesVitamin D An Innate Antiviral Agent Suppressingadrip234No ratings yet
- The Agathyrsi Were Hun-Scythians 2013.Document5 pagesThe Agathyrsi Were Hun-Scythians 2013.SzkitaHunMagyarNo ratings yet
- Archeology Ancient Egypt Hawass - Fs - Oconnor-1Document28 pagesArcheology Ancient Egypt Hawass - Fs - Oconnor-1adrip234No ratings yet
- BMJ Grant 2015Document5 pagesBMJ Grant 2015adrip234No ratings yet
- Vitamin D Status and Spine Surgery OutcomesDocument12 pagesVitamin D Status and Spine Surgery Outcomesadrip234No ratings yet
- Vitamin D Status and Spine Surgery OutcomesDocument12 pagesVitamin D Status and Spine Surgery Outcomesadrip234No ratings yet
- Vitamin D Prevents Cognitive Decline and EnhancesDocument8 pagesVitamin D Prevents Cognitive Decline and Enhancesadrip234No ratings yet
- Vitamin D and Neurocognitive FunctionDocument10 pagesVitamin D and Neurocognitive Functionadrip234No ratings yet
- The Agathyrsi Were Hun-Scythians 2013.Document5 pagesThe Agathyrsi Were Hun-Scythians 2013.SzkitaHunMagyarNo ratings yet
- An Overview and Management of OsteoporosisDocument11 pagesAn Overview and Management of Osteoporosisadrip234No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Characteristics of NewbornDocument28 pagesCharacteristics of NewbornChandu Raj100% (4)
- Serologic Chart V 8Document1 pageSerologic Chart V 8Olga CîrsteaNo ratings yet
- Herpetologists and the Study of Amphibians and ReptilesDocument20 pagesHerpetologists and the Study of Amphibians and ReptilesJamie BagundolNo ratings yet
- Alowerquiz4 6Document6 pagesAlowerquiz4 6sandroedaniNo ratings yet
- Nurul Farhanah BT Rosli: HumidityDocument3 pagesNurul Farhanah BT Rosli: HumidityfahnacircleNo ratings yet
- B.I Paper 1 2017 Tahun 6Document11 pagesB.I Paper 1 2017 Tahun 6Faridah Abd HalimNo ratings yet
- Molecular Basis of Circadian RhythmDocument1 pageMolecular Basis of Circadian RhythmNigarNo ratings yet
- Nasogastric Tube Insertion: Notes: ComplicationsDocument2 pagesNasogastric Tube Insertion: Notes: ComplicationsAlyssandra LucenoNo ratings yet
- ProtozoaDocument31 pagesProtozoaBio SciencesNo ratings yet
- Connective Tissues and Their FunctionsDocument3 pagesConnective Tissues and Their FunctionsSenNo ratings yet
- Z+blood Groups....Document36 pagesZ+blood Groups....ilhamaminsyaputraNo ratings yet
- AustraliaDocument4 pagesAustraliaOana PopaNo ratings yet
- Miko SisDocument90 pagesMiko SisFahlevi QalbiNo ratings yet
- Anatomy & Physiology Digestive System Exam ReviewDocument13 pagesAnatomy & Physiology Digestive System Exam Reviewhugomiso100% (3)
- Phylum Nematoda (Ascaris) : RoundwormsDocument14 pagesPhylum Nematoda (Ascaris) : RoundwormsLuisa San SebastianNo ratings yet
- 2015-2016 Patient records from local hospitalDocument47 pages2015-2016 Patient records from local hospitalElvis Olivera EgasNo ratings yet
- PERIOPERATIVE MANAGEMENT OF BRAIN TRAUMADocument52 pagesPERIOPERATIVE MANAGEMENT OF BRAIN TRAUMAKimbek BuangkeNo ratings yet
- ResearchDocument4 pagesResearchEmmanuel Isaac GohNo ratings yet
- Alchemist ExtractsDocument17 pagesAlchemist ExtractsCa KZNo ratings yet
- Lista Me Cmimet CIF Dhe EXW Te BarnaveDocument1,070 pagesLista Me Cmimet CIF Dhe EXW Te BarnaveAgron Spahija100% (1)
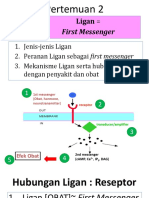
- 2 Ligan First MassengerDocument32 pages2 Ligan First MassengerikhararaNo ratings yet
- Pharmacology of Renal SystemDocument125 pagesPharmacology of Renal SystemBirhanu GetaNo ratings yet
- Handy Health Guide To DiabetesDocument49 pagesHandy Health Guide To DiabetesDiabetes Care100% (1)
- Blood PressureDocument9 pagesBlood Pressuregenevieve kryzleiNo ratings yet
- 10 Science Ncert Ch6Document10 pages10 Science Ncert Ch6Sharan KNo ratings yet
- Needle Prick Injury & PreventionDocument17 pagesNeedle Prick Injury & Preventioniman zainuddinNo ratings yet
- Congenital Heart Disease Sounds MP3sDocument2 pagesCongenital Heart Disease Sounds MP3ssra1_103No ratings yet
- Lai2015 Patogenitas AHPND Toksin PirDocument9 pagesLai2015 Patogenitas AHPND Toksin PirSuminiNo ratings yet
- Animal Life Cycle Unit Test - 2012Document9 pagesAnimal Life Cycle Unit Test - 2012Caitlin AblettNo ratings yet
- Respiratory Failure Nursing Care and ManagementDocument19 pagesRespiratory Failure Nursing Care and ManagementYudionoNo ratings yet