Professional Documents
Culture Documents
tmpBD78 TMP
Uploaded by
FrontiersOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
tmpBD78 TMP
Uploaded by
FrontiersCopyright:
Available Formats
Brief
Communication
The Deadly Ebola Threat in the Midst of an
Overwhelming Dengue Epidemic
Alwi Muhd Besari1, Siti Suraiya Md Noor2, Yeong Yeh Lee1,3
Submitted: 24 Oct 2014
Accepted: 26 Oct 2014
Department of Medicine, School of Medical Sciences, Universiti Sains
Malaysia, 16150 Kubang Kerian, Kelantan, Malaysia
Department of Microbiology, School of Medical Sciences, Universiti Sains
Malaysia, 16150 Kubang Kerian, Kelantan, Malaysia
Sub-Editor (Medical Base), Malaysian Journal of Medical Sciences, Universiti
Sains Malaysia Health Campus, 16150 Kubang Kerian, Kelantan, Malaysia
Abstract
The recent death tolls and morbidities associated with two deadly viral haemorrhagic fevers
(VHFs), i.e., Ebola and dengue, are simply shocking. By the end of August 2014, 65 672 people were
afflicted with dengue fever (DF) in Malaysia, with 9505 from Kelantan, and there were 128 reported
deaths. More astounding are the death tolls associated with Ebola: 3091 deaths from 6574 reported
cases so far. It is not difficult to imagine the potential disaster if Ebola spreads beyond Africa. VHFs
are characterised by an acute onset of fever, vascular disruption and a rapid progression to shock
and death. The revised World Health Organization (WHO) 2012 classification (dengue with and
without warning signs and severe dengue) is more clinically relevant and allows more streamlined
admission. With good administrative support and public health and governmental efforts, the
dengue epidemic in Malaysia is now more contained. However, there should be no laxity with the
imminent lethal Ebola threat. Human-to-human transmission is an important mechanism for the
spread of Ebola, and this calls for strict precautions regarding contact with any suspected cases. In
contrast, the control and elimination of dengue would require successful control of the vectors and
their breeding sites.
Keywords: Ebola, dengue, hemorrhage, fever, virus
The Shocking Numbers
The world has been shaken by the recent
unprecedented morbidity and mortality caused by
two viral haemorrhagic fevers (VHFs), i.e., Ebola
and dengue. The initial triggering of the Ebola
outbreak in West Africa in the beginning of 2014
closely followed the dengue epidemic in Asia.
At one extreme, Ebola viral disease (EVD) has a
fatality rate above 90% (1), whereas dengue fever
(DF), at the other end, is associated with significant
morbidity. The dengue epidemic in Malaysia
this year, especially in the state of Kelantan in
the northeastern region of the Peninsular, has
been the worst ever, stretching the limits of the
national health care system. DF causes significant
economic loss because this disease affects mainly
healthy young people. By the end of August, a total
of 65 672 people were confirmed to have DF in
Malaysia, with 9505 people from Kelantan. So far,
there are 128 reported deaths, based on national
figures, and these numbers have far exceeded
any previous records (2,3). More astounding,
however, are the death tolls associated with the
Ebola outbreak; by the end of September of this
year, there were 3091 deaths from 6574 reported
cases (4). On September 30th, the first travelassociated case of Ebola was announced outside
of West Africa (4), indicating a real danger that
this disease may spread to the rest of the world.
Deadly Viral Haemorrhagic Fevers
(VHFs)
Collectively, VHFs affect more than 100
million people around the world and kill
more than 60 000 annually (5). The diseases
brought about by viruses in the VHF group are
characterised by an acute onset of fever and
vascular dysfunction, with a potential for bleeding
disorders (5,6). These diseases can rapidly
progress to shock and subsequently death. The
23 enveloped RNA viruses associated with VHFs
are grouped into four taxonomic families, i.e.,
Malays J Med Sci. Nov-Dec 2014; 21(6): 9-13
www.mjms.usm.my Penerbit Universiti Sains Malaysia, 2014
For permission, please email:mjms.usm@gmail.com
Malays J Med Sci. Nov-Dec 2014; 21(6): 9-13
Arenaviridae, Bunyaviridae, Filoviridae, and
Flaviviridae (6). These viruses share a number
of common features. First, they are enveloped
viruses with single-stranded ribonucleic acid
(ssRNA) genomes and cytoplasmic replication
(5). Second, they use rodents, bats, or insects
as natural reservoirs or vectors (5). As a result,
their distribution is geographically limited by
the habitats of their natural hosts, and human
beings are incidental hosts. Most of these viruses
show affinity to most bodily cells (pantropism),
but they preferentially target dendritic cells
(DCs), monocytes and/or macrophages (5).
The mechanisms of vascular dysfunction in
VHFs include endothelial damage, activation of
mononuclear phagocytes, expression of abnormal
levels of cytokines and other mediators, platelet
aggregation and consumption, initiation of
the coagulation cascade, and insufficiency of
coagulation factors because of severe hepatic
damage (6). Thrombocytopenia and depressed
immune responses are the hallmarks of VHFs (5).
A body of evidence that indicates the importance
of viral replication and host immune responses
in determining the disease severity and clinical
outcomes is available (5).
Overwhelming Dengue Epidemic in
Malaysia
Dengue virus (DENV), from the Flaviviridae
group of viruses, is the most prevalent cause of
arthropod-borne VHFs (5). A third of the worlds
human population is at risk for exposure to
dengue (7). Annually, there are approximately
50 million reported cases of DF, with 500 000
of them requiring hospitalisation, and there are
between 20 000 and 25 000 reported deaths
(7,8). The primary vector for DENV is the
mosquito Aedes aegypti, which has been urban
adapted, and the secondary known vector is Aedes
albopictus, which has expanded its geographical
distribution in more recent years (7). Any of the
four single-stranded, positive-sense RNA virus
serotypes (DENV serotypes 1 to 4) can cause DF
(7,8). DF is one of the most common causes of
acute febrile illness among children in the AsiaPacific region (9) and is among the leading causes
of hospitalisation (10). Although dengue is not as
fatal as the other types of VHFs (namely, yellow
fever or EVD), the mortality rates of complicated
dengue, i.e., dengue haemorrhagic fever (DHF)
and dengue shock syndrome (DSS), have been
reported to be between 1% and 5% at high-volume
centres (10). However, the mortality rates can
reach 44% in the presence of established shock
10
www.mjms.usm.my
(10).
One of the major challenges is to identify the
patients who might develop the severe form of
dengue. Among the risk factors for severe dengue
reported in the recent literature are female
gender, young age, obesity, the virus strain,
genetic variations, and the presence of secondary
dengue infection (two sequential infections by
different serotypes) (8). Recognising the clinical
limitations of earlier classification (classical
dengue fever, DHF and DSS), in 2012, the WHO
revised the classification to include dengue
without warning signs, dengue with warning signs
and severe dengue (11). This newer classification
is meant to simplify the patients categorisation,
to make the criteria more clinically relevant,
and to make it easier to monitor progress at the
bedside. Furthermore, based on this classification,
admission is more streamlined, i.e., those without
warning signs can be managed at home with home
monitoring, those with warning signs should be
admitted to a general ward and those meeting the
criteria for severe dengue should be admitted to
a high-dependency unit (HDU) or intensive care
unit (ICU).
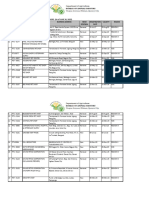
During the dengue outbreak, Hospital
Universiti Sains Malaysia, one of two tertiary
hospitals serving the state of Kelantan, admitted
a total of 1252 patients with DF from January
1st to September 30th of this year. The majority
of patients were admitted to the general ward,
166 (13.3%) of whom had severe dengue. For
the first three quarters of this year, there were
4 (0.3%) dengue-related deaths (Figure 1).
With the alarming growing figures, the hospital
administration, in cooperation with the Ministry
of Health of Malaysia, was quick to take action.
In addition to creating two new general wards
dedicated solely to the outbreak, the whole 6-bed
surgical ICU was readied for any cases of severe
dengue. The wards and ICU were supported by a
dedicated team of doctors, nurses and attendants
who were on duty 24 hours per day, 7 days per
week, for months.
The Imminent Worldwide Threat of
Ebola
The onslaught of dengue has barely settled,
and a potentially imminent wave of Ebola is
threatening to hit the Malaysian shore. On
August 8th, 2014, the WHO declared the Ebola
epidemic to be a public health emergency of major
international concern (12). This declaration was
made after the realisation that an international
spread of Ebola could have serious implications
Brief communication | Ebola threat
(12). This concern is not exaggerated and should
not be ignored by any governments, including the
Malaysian government. There is unpredictable
and continuing disease transmission and high
case fatality rates for Ebola in West African
countries (Guinea, Liberia, Sierra Leone, and
Nigeria), and the weak health services in these
and other neighbouring countries would not
be able to contain the epidemic without any
international support (12). The current outbreak
of Ebola has much similarity to the 1976 outbreak.
Both were caused by Zaire ebolavirus and began
in rural forest communities where wild animals
were hunted for food. Acutely ill patients started
to come to district hospitals in large numbers,
with initial symptoms resembling more common
infections, including malaria, typhoid, Lassa
fever, yellow fever, and influenza. In addition
to unknowing relatives, families and friends,
unprepared hospital staff members who were in
contact with the patients blood and bodily fluids
then became ill themselves. The disease quickly
spread to the cities, and chains of transmission
were then established (13).
A member of the Filovirus family, Ebola
viruses are pleomorphic, negative-sense RNA
viruses with genomic organisation similar to that
of the Paramyxoviridae. Of the four identified
strains, three, or the Zaire, Ivory Coast, and Sudan
strains, have resulted in diseases in both humans
and nonhuman primates, with the Zaire strain
being the most lethal (14). This virus replicates
at abnormally high rates that overwhelm the
protein synthesis engine of infected cells and
easily defeat the host immune defences (14).
Direct infection of monocytes and macrophages
and the resultant host immune responses cause
the release of cytokines commonly associated
with inflammation and fever. Additionally, the
direct cytopathic effect on the endothelial linings,
together with abnormal cytokine effects, results
in loss of the vascular barrier, haemorrhage and
subsequent total vasomotor collapse (14). These
effects on the vessels are the causes of the high
mortality rates observed for Ebola.
Ebola vs Dengue: The Conclusion
Figure 1: Patients admitted into Hospital
Universiti Sains Malaysia from
January to September 2014:
(a) total number of admitted
patients with confirmed dengue
and (b) number of patients with
severe dengue (green bar) including
number of deaths (red bar).
Although EVD shares a number of similarities
with other VHFs, there are differences that
set them apart (Table 1). One of the important
differences between EVD and dengue is the
mode of transmission. Whereas there is humanto-human transmission via contact with blood
or bodily fluids for EVD, there is no humanto-human transmission of dengue. Therefore,
a major intervention to control the spread and
dissemination of EVD would be strict observation
of precautions regarding contacts when handling
patients under investigation or any confirmed
cases of EVD. In contrast, the control and
elimination of dengue would require successful
control of the vectors and their breeding sites.
Acknowledgement
None.
Funds
None.
www.mjms.usm.my
11
Malays J Med Sci. Nov-Dec 2014; 21(6): 9-13
Table 1: Comparison between dengue hemorrhagic fever and Ebola viral disease
Dengue hemorrhagic fever
Ebola viral disease
Family
Flaviviridae
Filoviridae
Mode of transmission
Anthropod-born
Direct Contact with Blood/Body fluid
Human-human transmission No
Yes
Incubation period
3 to 7 days
2 to 21 days
Mortality
0.04 to 0.05 %
50 to 90 %
Fever
Common
Common15
Headache
Common
Common15
Muscles ache and pain
Common
Common15
Vomiting
Common
Common15
Diarrhea
Uncommon
Common15
Bleeding
Unusual
Usual15
Platelet
Low
Low16
White cells counts
Low
Low16
Hematocrit
High
Low16
Hemoglobin
High
Low16
Aspartate transferase
Elevated
Elevated16
Supportive
Supportive
Typical Symptoms:
Typical blood Abnormalities:
Treatment
Conflict of Interest
References
None.
1.
World Health Organization. Ebola and Marburg
virus disease epidemics: preparedness, alert,
control, and evaluation. Geneva (CH): World Health
Organization; 2014. p. 12. Report no.: INTERIM
version 1.2.
2.
Fariz Safhan M.N, Tee HP, Abu Dzarr GA, Sapari S,
Lee YY. Bleeding outcome during a dengue outbreak in
2005 in the East-coast region of Peninsular Malaysia:
a prospective study. Trop BioMed. 2014;31(2):270
280.
3.
Ministry of Health. Demam denggi dan
chikungkunya. Putrajaya (MY): Ministry of Health;
2014 [cited 2014 Oct 20]. Available from: http://
www.moh.gov.my/index.php/database_stores/
store_view_page/17/568.
4.
Centers for Disease control and Prevention (CDC).
2014 Ebola outbreak in West Africa. Atlanta (US):
CDC; 2014 [cited 2014 Oct. 20]. Available from:
http://www.cdc.gov/vhf/ebola/outbreaks/2014west-africa/index.html.
5.
Zapata JC, Cox D, Salvato MS. The Role of Platelets
in the Pathogenesis of Viral Hemorrhagic Fevers.
PLoS Negl Trop Dis. 2014;8(6):e2858. doi: 10.1371/
journal.pntd.0002858.
6.
Paessler S, Walker DH. Pathogenesis of the Viral
Hemorrhagic Fevers. Annu Rev Pathol. 2013;8:411
40. doi: 10.1146/annurev-pathol-020712-164041.
Authors Contribution
Conception and design, analysis and interpretation
of the data, drafting of the article, critical revision
of the article for the important intellectual
content, final approval of the article, provision of
study materials or patient, statistical expertise,
obtaining of funding, administrative, technical or
logistic support, collection and assembly of data:
AMB, SSMN, YYL
Correspondence
Dr Lee Yeong Yeh
MD (USM), MMed (Internal Medicine) (USM), PhD
(Glasgow), FACP, FRCP, FACG
Malaysian Journal of Medical Sciences
Universiti Sains Malaysia
Health Campus, 16150 Kubang Kerian
Kelantan, Malaysia
Tel: +609-767 6571
Fax: +609-767 3949
Email: yylee@usm.my
12
www.mjms.usm.my
Brief communication | Ebola threat
7.
Rogers DJ, Suk JE, Semenza JC. Using global maps to
predict the risk of dengue in Europe. Acta Trop. 2014;
129:114. doi: 10.1016/j.actatropica.2013.08.008.
8.
Simmons CP, Farrar JJ, Nguyen vV, Wills B. Dengue.
N Engl J Med. 2012;366(15):1423-32. doi: 10.1056/
NEJMra1110265.
9.
Capeding MR, Chua MN, Hadinegoro SR, Hussain
II, Nallusamy R, Pitisuttithum P, et al. Dengue and
other common causes of acute febrile illness in Asia:
an active surveillance study in children. PLoS Negl
Trop Dis. 2013;7(7):e2331. doi: 10.1371/journal.
pntd.0002331.
10. Ngo TN, Cao XT, Kneen R, Wills B, Nguyen VM,
Nguyen TQ, et al. Acute Management of Dengue
Shock Syndrome. A randomized Double-blind
Comparison of 4-intravenous fluid regime. Clin Infect
Dis. 200;32(2):204213. doi: 10.1086/318479.
11. Chai LSL, Guzman MG, Martinez E, Tan LH, Nguyen
TH. Handbook for clinical management of dengue.
Geneva (CH): World Health Organization; 2012 [cited
2014 Oct 20]. Available from: http://www.wpro.
who.int/mvp/documents/handbook_for_clinical_
management_of_dengue.pdf.
12. Briand S, Bertherat E, Cox P, Formenty P, Kieny MP,
Myhre JK, et al. The International Ebola Emergency.
N Engl J Med. 2014;371(13):11801183. doi: 10.
1056/NEJMp1409858.
13. Breman JG, Johnson KM. Ebola Then and Now. N
Engl J Med. 2014;371(18):16631666. doi: 10.1056/
NEJMp1410540.
14. Sullivan N, Yang Zy, and Nabel GJ. Ebola Virus
Pathogenesis: Implications for Vaccines and
Therapies. J Virol. 2003;77(18):97339737. doi: 10.
1128/JVI.77.18.9733-9737.2003.
15. Bwaka MA, Bonnet MJ, Calain P, Colebunders R, De
Roo A, Guimard Y, et al. Ebola hemorrhagic fever in
Kikwit, Democratic Republic of the Congo: clinical
observations in 103 patients. J Infect Dis. 1999;179
(Suppl 1):S17. doi: 10.1086/514308.
16. Kortepeter MG, Bausch DG, Bray M. Basic clinical
and laboratory features of filoviral hemorrhagic fever.
J Infect Dis. 2011;204 (Suppl 3):S810S816. doi:
10.1093/infdis/jir299.
www.mjms.usm.my
13
You might also like
- tmp3CAB TMPDocument16 pagestmp3CAB TMPFrontiersNo ratings yet
- tmpCE8C TMPDocument19 pagestmpCE8C TMPFrontiersNo ratings yet
- tmp80F6 TMPDocument24 pagestmp80F6 TMPFrontiersNo ratings yet
- tmpF3B5 TMPDocument15 pagestmpF3B5 TMPFrontiersNo ratings yet
- tmpE3C0 TMPDocument17 pagestmpE3C0 TMPFrontiersNo ratings yet
- tmpEFCC TMPDocument6 pagestmpEFCC TMPFrontiersNo ratings yet
- tmp6F0E TMPDocument12 pagestmp6F0E TMPFrontiersNo ratings yet
- Tmpa077 TMPDocument15 pagesTmpa077 TMPFrontiersNo ratings yet
- tmpF178 TMPDocument15 pagestmpF178 TMPFrontiersNo ratings yet
- Tmp1a96 TMPDocument80 pagesTmp1a96 TMPFrontiersNo ratings yet
- tmpFFE0 TMPDocument6 pagestmpFFE0 TMPFrontiersNo ratings yet
- tmpE7E9 TMPDocument14 pagestmpE7E9 TMPFrontiersNo ratings yet
- tmp998 TMPDocument9 pagestmp998 TMPFrontiersNo ratings yet
- tmp6382 TMPDocument8 pagestmp6382 TMPFrontiersNo ratings yet
- tmpF407 TMPDocument17 pagestmpF407 TMPFrontiersNo ratings yet
- Tmp75a7 TMPDocument8 pagesTmp75a7 TMPFrontiersNo ratings yet
- tmp72FE TMPDocument8 pagestmp72FE TMPFrontiersNo ratings yet
- tmp60EF TMPDocument20 pagestmp60EF TMPFrontiersNo ratings yet
- tmp9D75 TMPDocument9 pagestmp9D75 TMPFrontiersNo ratings yet
- tmp8B94 TMPDocument9 pagestmp8B94 TMPFrontiersNo ratings yet
- tmp4B57 TMPDocument9 pagestmp4B57 TMPFrontiersNo ratings yet
- tmpC0A TMPDocument9 pagestmpC0A TMPFrontiersNo ratings yet
- tmp37B8 TMPDocument9 pagestmp37B8 TMPFrontiersNo ratings yet
- tmpB1BE TMPDocument9 pagestmpB1BE TMPFrontiersNo ratings yet
- tmpD1FE TMPDocument6 pagestmpD1FE TMPFrontiersNo ratings yet
- tmp27C1 TMPDocument5 pagestmp27C1 TMPFrontiersNo ratings yet
- tmpA0D TMPDocument9 pagestmpA0D TMPFrontiersNo ratings yet
- tmp2F3F TMPDocument10 pagestmp2F3F TMPFrontiersNo ratings yet
- tmpC30A TMPDocument10 pagestmpC30A TMPFrontiersNo ratings yet
- tmp3656 TMPDocument14 pagestmp3656 TMPFrontiersNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cysticercosis Is The Most Common Parasitic Infection of The CNSDocument16 pagesCysticercosis Is The Most Common Parasitic Infection of The CNScgclarkNo ratings yet
- Immunization RecordDocument1 pageImmunization RecordJordan Simmons ThomasNo ratings yet
- Negative COVID-19 PCR ReportDocument2 pagesNegative COVID-19 PCR ReportSaurabh SinghNo ratings yet
- Equine-Welfare GuidelinesDocument76 pagesEquine-Welfare Guidelinesapi-391604222No ratings yet
- Fernando - Sico - Elo - (181111010) Bahasa InggrisDocument2 pagesFernando - Sico - Elo - (181111010) Bahasa InggrisAsicoNo ratings yet
- MCQ Tropmed 2Document1 pageMCQ Tropmed 2Dapot SianiparNo ratings yet
- Lengua Extranjera Inglès: Dengue Prevention at SchoolDocument12 pagesLengua Extranjera Inglès: Dengue Prevention at SchoolDionicia MartinezNo ratings yet
- Covid 19: Dennis N. Muñoz, RN, RM, LPTDocument103 pagesCovid 19: Dennis N. Muñoz, RN, RM, LPTDennis Nabor Muñoz, RN,RMNo ratings yet
- Human Blood GroupsDocument29 pagesHuman Blood GroupsKunalNo ratings yet
- 1) Cutaneous LeishmaniasisDocument3 pages1) Cutaneous LeishmaniasisDjdjjd SiisusNo ratings yet
- ICD10 Random StudyDocument752 pagesICD10 Random StudyezzsakrNo ratings yet
- Chandigarh Dental - 148Document12 pagesChandigarh Dental - 148deva nesanNo ratings yet
- Vaccine Formulation, Dosage, Schedule and Protection GuideDocument2 pagesVaccine Formulation, Dosage, Schedule and Protection GuideEricNo ratings yet
- ISH552 Group 2 IC2204D - Legal Concept and Enforcement in Halal Slaughtering ManagementDocument22 pagesISH552 Group 2 IC2204D - Legal Concept and Enforcement in Halal Slaughtering ManagementMEOR ALIFF HAIKAL MOHD NOR ASRADNo ratings yet
- Explanation Text Covid-19Document2 pagesExplanation Text Covid-19Mr ClawNo ratings yet
- What Is A Viral Test For Covid-19?: What Do Your Results Mean?Document2 pagesWhat Is A Viral Test For Covid-19?: What Do Your Results Mean?zakiadaNo ratings yet
- Canine Brucellosis Antibody Test Kit D-Tec CBDocument2 pagesCanine Brucellosis Antibody Test Kit D-Tec CBEdson RiberioNo ratings yet
- Performing The Small Animal Physical Examination: August 2017Document2 pagesPerforming The Small Animal Physical Examination: August 2017Muhammad Fernanda DanuartaNo ratings yet
- Bai Darfo Registered Pet Shops As of June 30 2023Document6 pagesBai Darfo Registered Pet Shops As of June 30 2023itshardtogetauserNo ratings yet
- Epidemiology Modeling With StellaDocument33 pagesEpidemiology Modeling With Stellaqiuyan.yuanNo ratings yet
- Pertussis: PDF, 667kbDocument2 pagesPertussis: PDF, 667kbRaissa DeaNo ratings yet
- 19126-Article Text-68642-1-10-20140611 PDFDocument5 pages19126-Article Text-68642-1-10-20140611 PDFHikmat UllahNo ratings yet
- Uloga Veterinara U ONE HEALTHDocument34 pagesUloga Veterinara U ONE HEALTHlelascepanovicNo ratings yet
- Immunity (Lecture Notes)Document5 pagesImmunity (Lecture Notes)Anisha NishanthNo ratings yet
- 2022 Tuition Fees Tuition Fee Tables For International StudentsDocument31 pages2022 Tuition Fees Tuition Fee Tables For International StudentsAva JosephineNo ratings yet
- Updates On The Epidemiology of Dermatophyte InfectionsDocument19 pagesUpdates On The Epidemiology of Dermatophyte InfectionsAldo NovaNo ratings yet
- Risk Assessment Envirn Mad Cow Disease-2Document9 pagesRisk Assessment Envirn Mad Cow Disease-2api-436969344No ratings yet
- Alexis Wolter ResumeDocument2 pagesAlexis Wolter Resumeapi-610069547No ratings yet
- Ebola Virus Disease (EVD) : Clinical Features Diagnosis Treatment, Prevention and ControlDocument19 pagesEbola Virus Disease (EVD) : Clinical Features Diagnosis Treatment, Prevention and ControlABc abcNo ratings yet
- Addis Ababa University: General InformationDocument15 pagesAddis Ababa University: General InformationRahel EshetuNo ratings yet