Professional Documents
Culture Documents
20 Prism Info
Uploaded by
kjnsdnCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
20 Prism Info
Uploaded by
kjnsdnCopyright:
Available Formats
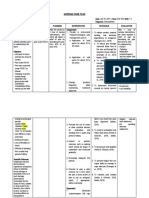
Useful Facts about Ophthalmic Prism
Opt 562, Behavioral Optometric Science
Bradley Coffey, O.D., FAAO
Pacific Optometry
A Few Things You Should Know About . . .
PRISM !
Prism is a useful tool in the behavioral optometric practice. Response of an
individual to a prism prescription is determined by both sensory and motor factors.
If sensory fusion is not present, as in strabismus or suppression, the individual will
not typically respond to prism by means of a vergence (motor) response. If sensory
fusion is intact, the individual will typically respond to small values of lateral prism
(for discussion purposes, 8 or less; sometimes more, sometimes less depending
upon the individual) by making a vergence movement (convergence in response to
base-out; divergence in response to base-in). Motor vergence responses to vertical
prism also occur, but the fusional range is much less (typically 1-3 base-up or
base-down). When sensory fusion is present, prism may be prescribed in three
forms: compensating/relieving, training, or yoked. These types of prism Rx are
discussed below.
1. Compensation of vergence conditions. When using prism to
compensate a condition in order to facilitate binocular sensory fusion, it is assumed
that the individual will NOT respond to the prism with a motor fusional movement of
vergence. Compensating prism allows the individual to maintain the deviant
vergence posture; the prism(s) refracts (bends) the incoming light so as to enable
sensory fusion in the absence of proper motor vergence alignment: Move the
image to the eye. This is the same concept that is used when you are measuring
the vergence posture with alternate cover testing: You continue adding
compensating prism until the cover test is neutralized. The thoughtful practitioner,
when using compensating prisms, also prescribes anti-suppression training and
endeavors to gradually reduce the needed prism power over time, ideally to zero.
The most common use of prism in this regard is the partial or full
compensation of excessive vertical phorias or vertical tropias. These conditions can
give rise to extreme asthenopia and/or diplopia. Prism is prescribed to relieve or
fully compensate the measured tropia or phoria, and is usually split between the two
lenses to provide better cosmesis. In some cases, usually when there exists a
paresis of a single extraocular muscle, the prism may be incorporated into only one
lens of the spectacle Rx. Base-down for a hyper condition, base-up for a hypo
condition.
Prism info, B Coffey, PUCO, p2
Prism may also be used to relieve or compensate an extreme horizontal
phoria or tropia. Base-in for exo conditions, base-out for eso conditions.
Prescribing prism for horizontal phorias or tropias can be risky to the careless
optometrist due to the phenomenon of prism adaptation, in which the individual
adapts to the prism by increasing the manifest deviation. If the deviation increases,
the initially prescribed prism loses its effectiveness, and larger amounts of prism
must be prescribed to relieve symptoms. Many phoric individuals have been
converted into strabismics by well-intentioned practitioners unaware of prism
adaptation. This creates a major patient management dilemma, and may place the
practitioner at risk for litigation. Prism adaptation is most likely to occur with baseout prism, but may also occur with vertical or base-in prism. This is a real danger
and should be borne in mind anytime a compensating prism prescription is being
considered. Prism adaptation is thought to occur within the adaptive or tonic
vergence controller.
Relieving prism refers to a partial compensating prism. For example, if an
individual measures 20 esophoria, a 10 base-out prism might be prescribed to
relieve the excessive eso posture, and thereby improve the individual's ability to
maintain constant fusion and heterophoria.
2. Training of vergence ability. It is frequently desirable to improve an
individual's ability to converge or diverge the eyes. One technique that may be
employed in this treatment approach is the use of temporary introduction of prism
before the eyes to change the vergence demand of the incoming light. In this
regard, for individuals with normal binocular vision, base-out prism stimulates a
convergence response; base-in prism stimulates a divergence response. For this
type of training to be effective, it is imperative that the individual have intact sensory
fusion ability; if a tendency is present to suppress one eye, the introduction of the
prism will likely cause suppression rather than the desired vergence response.
When this type of training is conducted, suppression should be controlled by means
of anaglyphic or polarized targets and filtering spectacles, or by some other means.
Training of vertical vergence conditions is very difficult and requires extreme
commitment and practice to be effective. Convergence training using base-out
prism is easiest by far; divergence training using base-in prism requires greater
effort, but is less challenging than vertical vergence training.
If the practitioner desires to train an exotrope, for example, it is first
necessary to eliminate suppression tendencies. Once suppression has been
eliminated or controlled, relative convergence training may ensue by asking the
individual to maintain binocular sensory fusion with gradually less base-in
(compensating or relieving) prism. When the exo individual is able to maintain
fusion with no base-in prism present, the practitioner can begin true convergence
training by introducing small amounts of base-out prism, then gradually increasing
the convergence demand with larger amounts of base-out prism, all the while
controlling for suppression by means of anaglyphic or polarizing filter materials.
Prism info, B Coffey, PUCO, p3
3. Yoked prisms represent a distinctly different approach to the use of
prism in the behavioral optometric practice. Yoked prism, prism of equal amounts
placed before each eye with the base in the same direction (up, down, left, right),
stimulates a version, rather than vergence, response on the part of the individual.
Regardless of the orientation of the yoked prism, the response of the individual is to
move the eyes toward the apex of the prisms. For example, yoked base-down prism
stimulates an upward movement (sursumversion or supraversion) of both eyes. In
general, yoked prisms have the same effect regardless of the sensory status of the
individual; yoked prism base-left, for example, will produce the same movement of
the eyes (dextroversion) in the phoric as well as the tropic individual (given no
extraocular muscle paresis).
Vertical yoked prisms are sometimes prescribed to modify postural
characteristics of the individual. Yoked prisms base-down, for example, will usually
yield a more upright posture, and are used by some practitioners as a preventative
strategy in a comprehensive management plan for myopia.
Lateral (horizontal) yoked prisms are most frequently used for individuals
who have eye muscle paralysis or paresis due to trauma or disease. In some cases
these individuals must rotate the head leftward or rightward in order to avoid
diplopia. The use of yoked prisms in these cases enables the individual to keep the
head in a more normal position while allowing the eyes to be in a position of
levoversion or dextroversion. Yoked prisms are also used by neurorehabilitative
optometrists to modify suspected visual perceptual abnormalities concerning the
perception of straight ahead (visual midline shift syndrome).
Horizontal yoked prisms are sometimes a temporary treatment for individuals
with acquired visual field loss. In these cases, the prism is applied with the base
toward the affected visual field: For a left hemianopsia, the prisms would be
prescribed bases-left. The idea of this treatment is to optically move the visual
information in the affected field to a more straight-ahead position so that it can be
more easily viewed. Patients with hemianopsias are usually encouraged to develop
regular scanning eye movements in the direction of the affected field in order to
monitor the area. Once these scanning eye movements have become habitual, the
yoked prism is removed.
Yoked prisms of various orientations are also sometimes used in the
vision therapy practice to modify visual input in order to force an individual to pay
more attention to what s/he is seeing. In this context, eye-hand activities are
usually employed to provide immediate feedback to the individual being treated.
The yoked prism will initially cause errors in eye-hand placement activities, and the
individual will have to make an adaptive adjustment within the visual motor system
in order to accurately complete the task.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Lesions of Upper Motor Neurons and Lower Motor NeuronsDocument9 pagesLesions of Upper Motor Neurons and Lower Motor NeuronsAdhitya Rama Jr.No ratings yet
- DK Publishing - Neal's Yard Remedies Complete Massage - All The Techniques, Disciplines, and Skills You Need To Massage For Wellness (2019, DK) PDFDocument248 pagesDK Publishing - Neal's Yard Remedies Complete Massage - All The Techniques, Disciplines, and Skills You Need To Massage For Wellness (2019, DK) PDFSolveig100% (1)
- Characteristics of Children with Learning DisabilitiesDocument4 pagesCharacteristics of Children with Learning DisabilitiesDanilo Siquig Jr.No ratings yet
- Robert MonroeDocument6 pagesRobert MonroelucioNo ratings yet
- SOP NeuroDocument2 pagesSOP NeuroMani100% (2)
- HHS Public Access: How Schizophrenia Develops: Cognitive and Brain Mechanisms Underlying Onset of PsychosisDocument25 pagesHHS Public Access: How Schizophrenia Develops: Cognitive and Brain Mechanisms Underlying Onset of PsychosisNoriNo ratings yet
- Abusive Head Trauma: Information and PreventionDocument19 pagesAbusive Head Trauma: Information and PreventionFahd AltaweelNo ratings yet
- ATLS Page Number Bridge 9th To 10th Edition PDFDocument4 pagesATLS Page Number Bridge 9th To 10th Edition PDFDaniel MirandaNo ratings yet
- Neurologic NCLEX Practice Test Part 1Document10 pagesNeurologic NCLEX Practice Test Part 1mpasague100% (2)
- Module 2.1 Sress and Nervous SystemDocument30 pagesModule 2.1 Sress and Nervous SystemIsha JoshiNo ratings yet
- FOUR Score Coma ScaleDocument32 pagesFOUR Score Coma ScaleAndriawan BramNo ratings yet
- The World of Pediatric NeurologyDocument12 pagesThe World of Pediatric Neurologyapi-321693380No ratings yet
- Articular NeurologyDocument14 pagesArticular Neurologykinj100% (1)
- C9 Discourse On The Logic of LanguageDocument5 pagesC9 Discourse On The Logic of LanguageMihaela TomaNo ratings yet
- 1.1 ANT Callejas, Lupiáñez y Tudela 2004Document4 pages1.1 ANT Callejas, Lupiáñez y Tudela 2004Daniel Londoño GuzmánNo ratings yet
- RPMS DETAILED PRESENTATIONDocument59 pagesRPMS DETAILED PRESENTATIONmageshNo ratings yet
- Ana Phisio Lab Report.Document4 pagesAna Phisio Lab Report.Diana Amor100% (1)
- Sense OrgansDocument12 pagesSense OrgansRon GruellaNo ratings yet
- Brain Fog PDFDocument1 pageBrain Fog PDFRomina Faur CapparelliNo ratings yet
- Psych - Root WordDocument7 pagesPsych - Root Wordarvilla18No ratings yet
- Trace Decay Theory of ForgettingDocument3 pagesTrace Decay Theory of ForgettingJecel Biagan100% (2)
- Neuroplasticity: Presented By: Advincula, Arnina Fortus, Jacyrone Pitpit, MarcusDocument17 pagesNeuroplasticity: Presented By: Advincula, Arnina Fortus, Jacyrone Pitpit, MarcusCLAIRE DENISSE DEVISNo ratings yet
- The Rare and The Unexpected Miller Fisher SyndromeDocument4 pagesThe Rare and The Unexpected Miller Fisher SyndromedoctorebrahimNo ratings yet
- NURSING CARE PLAN FOR OSTEOARTHRITISDocument4 pagesNURSING CARE PLAN FOR OSTEOARTHRITISKian HerreraNo ratings yet
- Neurological Manifestations in Typhoid Fever During The First Week of Illness A Case ReportDocument3 pagesNeurological Manifestations in Typhoid Fever During The First Week of Illness A Case ReportJorge Ramirez RaherNo ratings yet
- Kessler 2005Document11 pagesKessler 2005mccg1478No ratings yet
- Ieee AUTOMATIC NUMBER-PLATE RECOGNITION VNIS.1994.396858-NEURAL NETWORK APPROACHDocument3 pagesIeee AUTOMATIC NUMBER-PLATE RECOGNITION VNIS.1994.396858-NEURAL NETWORK APPROACHEdikan AkpanNo ratings yet
- Primary Brain TumorDocument33 pagesPrimary Brain Tumoriura echin100% (2)
- Chapter 7 - NERVOUS SYSTEM PDFDocument58 pagesChapter 7 - NERVOUS SYSTEM PDFMary LimlinganNo ratings yet
- Hearing Status of Children Under Five Years Old in Jatinangor DistrictDocument5 pagesHearing Status of Children Under Five Years Old in Jatinangor DistricterickNo ratings yet