Professional Documents
Culture Documents
Hydro Ureter o Nephrosis
Uploaded by
Lutfi AuliaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hydro Ureter o Nephrosis
Uploaded by
Lutfi AuliaCopyright:
Available Formats
Hydroureteronephrosis is the most significant renal alteration during pregnancy.
Physiologic
dilatation of the collecting system begins in the first trimester at 6-10 weeks' gestation and
persists until 4-6 weeks following delivery.[5] Early theories suggest that hydronephrosis of
pregnancy may be a hormonally induced phenomenon whereby ureteral smooth muscles
relax in response to high levels of circulating progesterone. In early pregnancy, increased
progesterone secretion dilates the ureters and reduces ureteral peristalsis, causing
hydronephrosis. Alternatively, the predominant theory ascribes ureteric dilatation to
compression of the ureter by the enlarging gravid uterus at the level of the pelvic brim, where
the ureter crosses the iliac vessels.
Dilatation is greater on the right side than on the left because of pressure due to physiologic
engorgement of the right ovarian vein and dextrorotation of the uterus.[4] Swanson and
associates (1995) observed that hydroureteronephrosis was not routinely found below the
pelvic brim and was altogether absent in patients who had undergone urinary diversion.[5]
Volume changes during pregnancy
Glomerular filtration rate (GFR) and renal plasma flow (RPF) increase by as much as 25-50%
during pregnancy. Both of these changes are attributable to increases in cardiac output,
decreases in renal vascular resistance, and increases in serum levels of progesterone,
aldosterone, deoxycorticosterone, placental lactogen, and chorionic gonadotropin. GFR and
RPF enhancements also contribute to the increase in glucose, amino acid, protein, and
vitamin secretion. As a result of the GFR and RPF modulations, which peak at 9-11 weeks'
gestation, renal volume increases during pregnancy by as much as 30% above the reference
range. The sustained elevation of prolactin levels in the pregnant patient has a growth
hormonetype effect by increasing the glomerular surface area, which also contributes to an
increase in renal volume.
Along with increases in GFR and RPF, the filtered load of sodium, calcium, and urate
increases. Although calcium and urate excretion increases, sodium excretion remains
unchanged. The urinary excretion rate of calcium stone inhibitors, such as citrate and
magnesium, also increases in the pregnant patient; likewise, increased glycosaminoglycans
and acidic glycoproteins inhibit oxalate stone formation (eg, nephrocalcin). This explains
why pregnancy is not associated with a net increase in the rate of stone formation relative to
nonpregnant patients. The net effect of these physiologic changes is a stable relative
supersaturation of important ions such as calcium oxalate, urate, and phosphate.
Uric acid stone formation
The formation of uric acid stones requires continued and excessive oversaturation of urine
with uric acid or extreme aciduria. Dehydration, hyperuricosuria, and significantly acidic
urine contribute to uric acid supersaturation and stone formation. However, during gestation,
urine tends to be more alkaline, probably because of greater intrinsic purine use and increased
urinary citrate excretion. Thus, renal units are generally protected against uric acid stone
formation during pregnancy.
Calcium oxalate and calcium phosphate stone formation
Although pathologic calcium oxalate supersaturation has been identified in the urine of
pregnant women, the incidence of crystalluria is no higher than in women who are not
pregnant. In the pregnant patient, physiologic absorptive hypercalciuria is due to elevated
levels of serum 1,25 dihydroxycholecalciferol (1,25 vitamin D). This hormone, which is
secreted by the placenta, augments calcium absorption in the GI tract and suppresses
parathormone production, increasing renal excretion of calcium. Additionally, dietary
supplementation of calcium during gestation further augments calcium excretion. Some
reports suggest that calcium excretion increases 200-300% compared with that in healthy
patients who are not pregnant. However, increased concentration of the aforementioned
urolithiasis inhibitors present in urine during gestation and increased urine fluid output
counters the increased risk imposed by any hypercalciuria.
You might also like
- Large IntestineDocument22 pagesLarge IntestineLutfi AuliaNo ratings yet
- What Are The Symptoms of Diabetes Insipidus?Document5 pagesWhat Are The Symptoms of Diabetes Insipidus?Lutfi AuliaNo ratings yet
- Small Intestine and PancreasDocument52 pagesSmall Intestine and PancreasLutfi AuliaNo ratings yet
- BPHDocument1 pageBPHLutfi AuliaNo ratings yet
- BPHDocument1 pageBPHLutfi AuliaNo ratings yet
- Dengue Is A Common Viral Infection Spread by Mosquitoes. It Is Widespread in Tropical and Sub-Tropical RegionsDocument2 pagesDengue Is A Common Viral Infection Spread by Mosquitoes. It Is Widespread in Tropical and Sub-Tropical RegionsLutfi AuliaNo ratings yet
- Signs and Symptoms: Dengue Fever, Also Known As Breakbone Fever, Is ADocument8 pagesSigns and Symptoms: Dengue Fever, Also Known As Breakbone Fever, Is ALutfi AuliaNo ratings yet
- Essential Update: Dengue May Be Underrecognized in The United StatesDocument4 pagesEssential Update: Dengue May Be Underrecognized in The United StatesLutfi AuliaNo ratings yet
- Retention Urine During PragnancyDocument1 pageRetention Urine During PragnancyLutfi AuliaNo ratings yet
- A Collection of Related DiseasesDocument2 pagesA Collection of Related DiseasesLutfi AuliaNo ratings yet
- KankerDocument3 pagesKankerLutfi AuliaNo ratings yet
- Pic. PituitaryDocument2 pagesPic. PituitaryLutfi AuliaNo ratings yet
- Diagnosing and Treating Kidney Stones During PregnancyDocument1 pageDiagnosing and Treating Kidney Stones During PregnancyLutfi AuliaNo ratings yet
- Meningoenchepalitis BacterialDocument3 pagesMeningoenchepalitis BacterialLutfi AuliaNo ratings yet
- Pic. PituitaryDocument2 pagesPic. PituitaryLutfi AuliaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Seminars in Pediatric Surgery: Immediate Versus Staged Repair of OmphalocelesDocument6 pagesSeminars in Pediatric Surgery: Immediate Versus Staged Repair of OmphalocelesGufi GeorgeNo ratings yet
- DRUG STUDY TITLEDocument2 pagesDRUG STUDY TITLEpretty_mary100% (4)
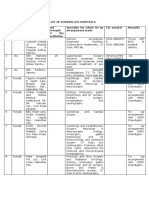
- LIST OF EMPANELLED HOSPITALSDocument38 pagesLIST OF EMPANELLED HOSPITALSChandan ChatterjeeNo ratings yet
- Case AnalysisDocument3 pagesCase AnalysisDebi Bahinting Ouano-RotaNo ratings yet
- Test 7Document7 pagesTest 7Sayani BanerjeeNo ratings yet
- Nurses TraitsDocument3 pagesNurses TraitsGeorge Michael LimNo ratings yet
- Klinefelter SyndromeDocument12 pagesKlinefelter SyndromeYob YnnosNo ratings yet
- KC DataDocument7 pagesKC DataDeepa YadavNo ratings yet
- Guidelines for Starting X-Ray InstallationDocument3 pagesGuidelines for Starting X-Ray InstallationmansooracNo ratings yet
- A New Look at The Safety of Breastfeeding During Pregnancy - KellyMomDocument11 pagesA New Look at The Safety of Breastfeeding During Pregnancy - KellyMomdoggydogNo ratings yet
- Board Exam 3Document26 pagesBoard Exam 3Kira100% (1)
- Case Study The Gambia A Youthful PopulationDocument2 pagesCase Study The Gambia A Youthful PopulationJunior MirandaNo ratings yet
- Ini Cet - Online Seat Allocation - 1st Round Mdms Mds Final Net 2Document109 pagesIni Cet - Online Seat Allocation - 1st Round Mdms Mds Final Net 2jai patelNo ratings yet
- Pelvic Planes Dimensions and ContractionTITLEDocument12 pagesPelvic Planes Dimensions and ContractionTITLEDavid Eka PrasetyaNo ratings yet
- Faculty of Medical Sciences PDFDocument114 pagesFaculty of Medical Sciences PDFAriey MaQueenNo ratings yet
- Clinical Practice Guideline for Diagnosing and Treating Sudden Hearing LossDocument45 pagesClinical Practice Guideline for Diagnosing and Treating Sudden Hearing Lossvania fatmaNo ratings yet
- Pages From ASHRAE HVAC Design Manual For Hospitals & Clinics-2013 (Orignal)Document1 pagePages From ASHRAE HVAC Design Manual For Hospitals & Clinics-2013 (Orignal)3obaydoofNo ratings yet
- Neonatal JaundiceDocument14 pagesNeonatal Jaundicewewewwe memeNo ratings yet
- Antenatal AssessmentDocument53 pagesAntenatal AssessmentAaron Wallace100% (1)
- Genitourinary SystemDocument23 pagesGenitourinary SystemRisma ZulfianiNo ratings yet
- DR ActivityDocument2 pagesDR ActivityVia Teresa AtienzaNo ratings yet
- Twin to twin transfusion syndrome الدكتور ماهر معايطةDocument7 pagesTwin to twin transfusion syndrome الدكتور ماهر معايطةjordanmedicsNo ratings yet
- Logiq S8: Simply AmazingDocument6 pagesLogiq S8: Simply AmazingOswaldo FilhoNo ratings yet
- Prelim TFNDocument5 pagesPrelim TFNjokazelNo ratings yet
- Endocrinology, Diabetes, and Metabolism - American Board of Internal Medicine - ABIMDocument3 pagesEndocrinology, Diabetes, and Metabolism - American Board of Internal Medicine - ABIMabimorgNo ratings yet
- Surgical TechniqueDocument6 pagesSurgical TechniqueDavid PalomequeNo ratings yet
- WMed Residency Match 2023Document3 pagesWMed Residency Match 2023WWMTNo ratings yet
- ACOG SMFM Joint Practice Bulletin Multiple Gestation 2004Document15 pagesACOG SMFM Joint Practice Bulletin Multiple Gestation 2004Reza ZulkarnainNo ratings yet
- Philippine Health Care SystemDocument86 pagesPhilippine Health Care SystemKhylamarie VillalunaNo ratings yet
- NRHM MONTHLY PHC REPORTDocument7 pagesNRHM MONTHLY PHC REPORTnaga vijayNo ratings yet