Professional Documents
Culture Documents
SD-V9N1 Bosshart Complete
Uploaded by
Anonymous gjrAZMXB3Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SD-V9N1 Bosshart Complete
Uploaded by
Anonymous gjrAZMXB3Copyright:
Available Formats
SD-V9N1 CMYK.
qxd:Layout 1
56
12/18/09
5:40 PM
Page 56
Spectrum dialogue Vol. 9 No. 1 January 2010
Introduction
The study from Suguru Kimoto et
al.4 showed greater satisfaction of
the patient wearing dentures with a
lingualised occlusion concept.
The article The effect of occlusal
contact localisation on the stress
distribution in complete maxillary
denture5 describes the connections
which contribute to broken
dentures. According to this study, it
is the form of occlusion and the
positioning of the teeth in relation
to the alveolar ridge which leads to
an unstable load and to broken
dentures.
Functional Reasons Causing
Broken Dentures
Complete Denture
Stability During
Chewing
Max Bosshart
To obtain unilateral chewing stability: forget about balanced occlusion, it
doesnt work, but: Perfect equilibrated occlusion is essential during
parafunctional mandibular movements to prevent unbalanced loads on the
supporting alveolar ridges.
1. Food is almost always chewed on one side only (Hiltebrandt, 1933/35)1.
2. During mastication the teeth of the denture wearer only finally come into
con-tact when the food load has become softened (A. Gerber, 1946)2, 3.
3. Therefore the bi-lateral equilibrium is ineffective for chewing stability.
4. For the unilateral chewing stability of dentures, immobility is the key.
5. Parafunctional contacts are occurring both day and night. In order to
distribute these forces evenly, correct centric and equilibrating contacts are
necessary.
Incorrect positioning of posterior
teeth The ideal point of pressure
on the tooth is the area shown in
Figure 1 with a green arrow. The
chewing force is directed to the middle of the alveolar
ridge. Forces directed in a more buccal direction
progressively increase the deformation of the denture. The
denture is no longer well fitting (blue area) and, in time,
could initiate a crack zone in the palatal part of the
denture.
Also of importance is the contour of the teeth. By losing
the main palatal cusps on the upper denture we get too
much pressure on the buccal cusps, resulting in a crack in
the palatinal part of the denture (Fig. 2). Because of the
inclination of the occlusal surface, shown in figure 2, the
resulting orientation of the forces, upwards and outwards,
is increasing the deformation of the denture base. It can
lead to crack formation in the denture base and damage
the alveolar bone.
Usually we can easily distinguish between a functional
breakage and an accidental breakage of a denture. Of
course we can ask the patient what happened. For the
denture construction it is important to know the
functional origin of the break.
By abrasion of the posteriors, premature contacts and an
anterior or canine guidance are created. It can provoke a
tilting action which would result in a dropping of the
denture in the post dam region leading to a lack of
security. Breaking of the upper denture can also be
expected.
Conclusion: Broken dentures are a good indication of
instability caused by unstable positions or wrong contacts
of the artificial teeth. It is in these cases that pathological
damage is caused. We can use high-impact acrylic or just
repair the denture, but, in both cases the pathological
damage will continue. The results are flabby ridges and
increased bone resorption. The mastication efficiency is
very restricted and the patient could experience pain.
To avoid these problems we need to correct the teeth
contacts and to have periodic recalls every 2 years.
Tooth Position and Denture Stability
In the past Many years ago different authors discovered
the problem of the unstable denture (Hiltebrandt 19331,
Payne 19416, Gerber 19462). All of them proposed
aspecific lingualised occlusal concept to solve the
problem.
SD-V9N1 CMYK.qxd:Layout 1
12/18/09
5:40 PM
Page 57
Spectrum dialogue Vol. 9 No. 1 January 2010
57
In Europe, 1958, Albert Gerber from Zurich developed
the so called Gerber-Method. It is still recognised as one
of the best systems available 7, 8.
Conventional Set-up
Fig. 1: The ideal point of pressure on the tooth is the area shown with a
green arrow. The chewing force is directed to the middle of the alveolar
ridge. Forces directed in a more buccal direction, as the red arrows show,
progressively increase the deformation of the denture. The denture is no
longer well fitting (blue area) and in time, could initiate a crack zone in
the palatal part of the denture.
Fig. 2: The lower teeth exert pressure on the upper teeth in a buccal
direction (red arrow). This multiple cyclic reaction can lead to a crack in
the denture and a gap developing between the denture and the torus
palatinus.
In the conventional set-up, the lower buccal cusps are on
the crest of the ridge (or more lingual) in the upper, the
central groove is straight over the crest of the ridge
(Gysi 1914/17)9. Buccal cusp contact in a conventional
set-up during mastication is a handicap. Too much force is
exerted buccal of the ridge, resulting in an unstable
denture (Fig. 3). With the reduction of the buccal cusps
(minimum 2mm) we have the mastication force directed
over the lingual-palatal area and over the centre of the
ridge. This way the denture is stable during mastication
(Fig. 4). A correlation of denture instability and
progressive resorption of the alveolar bone4 exists.
A personal observation, made by the author of the
anatomic situation of Japanese edentulous patients showed
a significantly better situation in comparison with the
Caucasian population. Their alveolar ridges are showing
significantly less resorption in width. Also, the width of
the dental arch is distinctly greater. These characteristics
are clearly favouring the transversal denture stability. It
may explain the reason, why Kumutu et al. found little or
no difference in the mastication performance of the
patients. Long term results could show different results
when the fit of the dentures deteriorates.
The Gerber System
In this system we put the upper vertical direction to the
crest of the ridge (Fig. 4). The denture will remain stable
with the advantage that the teeth can be placed more
buccally. This not only provides better cheek contact and
more tongue space but also stops food from slipping under
the denture.
The Lower Denture
Fig. 3: Buccal cusp contact during mastication is a handicap. Too much
force is placed buccally of the ridge during mastication, resulting in a
tilting upper denture and furthermore an unsupported direction of
masticatory force.
The lower denture bearing area can have a difficult shape
with many different inclined levels.
Everyone knows what happens if you stand on an
inclined slope on ice or snow in Switzerland, we slide
downhill without any effort, known as skiing! Teeth
standing on the retro-molar ascending part of the ridge
push the denture forward during mastication (Gysi 1917)9.
Figure 5 depicts a common case. The last molar is
SD-V9N1 CMYK.qxd:Layout 1
58
12/18/09
5:41 PM
Page 58
Spectrum dialogue Vol. 9 No. 1 January 2010
positioned in the area of the ascending part of the ridge
and the force to the lower denture hits the inclined area.
The force will be deflected forward and as a result the
denture will slip down the slope and will lift up at
the front.
The Upper Denture
Can this also happen with the upper denture? Yes! This
case shows that both dentures are unstable. As the patient
chews food the dentures move making it virtually
impossible to masticate. Pressure areas are preassigned and,
with time, cause resorption of the ridge.
Under mastication force the upper denture slips forward
and only the patients lip holds the denture in position.
This has a negative effect on Aesthetics, making the lips
appear tensed.
Fig. 4 : With the reduction of the buccal cusps (minimum 2mm) we have
the mastication force in the lingual/palatal area, which is orientated
almost vertically. Sagittal Stability
Model Analysis
Anyone building a house knows that he has to analyse the
ground it will be supported on. When setting up a denture
we need to do the same, we call it model-analysis.
We draw on the side of the model the different zones,
positive, neutral and negative/unstable areas. We use
different colours to get a quick analysis of the situation
(Fig. 7).
Posterior Tooth Position
The second upper molar in figures 8a and 8b is 3mm out of
contact to its antagonist and therefore it is not possible to
chew with it. These last teeth serve only as a support to
the cheeks, prevent food slipping up or down under the
denture and prevent cheek biting 10.
If sufficient space is lacking, we recommended not to
place any upper molar at all (Figs. 9a and 9b)
Fig. 5: In a textbook conventional set-up the last molar is positioned
correctly; the occlusal level and curve of Spee have been observed.
However, the masticatory force is not at 90 to the ridge, thus the
denture moves down the sloping ridge and moves forward and upward.
Balanced Occlusion
The arrangement of the teeth is still recognised as being a
balanced occlusion and the molar teeth are important in
parafunctional jaw movement. (Figs. 10a and 10b). Apart
from unilateral chewing stability as described above,
continuous posterior contacts are important during nonfunctional tooth contacts. The even distribution of the
forces over the complete upper and lower alveolar ridges
will protect the natural tissues from overload or at least
diminish the forces to a minimum. During all functional
and parafunctional movements, the elimination of all
prematurities is indispensable.
Fig. 6: This image shows in which direction the mastication force on the
upper jaw is directed. As a consequence of the poor position of the teeth,
according to the Spee curve, the force is in a disadvantageous angle to
the ridge and the pressure pushes the upper denture forward
SD-V9N1 CMYK.qxd:Layout 1
60
12/18/09
5:43 PM
Page 60
Spectrum dialogue Vol. 9 No. 1 January 2010
Fig. 8a
Fig. 7:
1. The positive zones are mostly in the pre-molar area (green).
During mastication the axis of the pre-molars pushes the
denture backwards to the respective ridge, giving a super
stable situation.
2. The deepest area in the lower jaw and the highest part of the
upper jaw are the neutral zones (blue). In this area we set the
first molars (largest teeth).
3. We can recognise on figures 5 and 6 that the retro-molar
area is critical (red). The directions of the upper and lower
ridge in the posterior part are not parallel to each other. We
cannot set any teeth in this area that will be stable during
masticatory function.
Fig. 8b
Figs. 8a and 8b: In this set-up the second upper molar is 3mm out of
contact. Therefore it is not possible to chew with it. Also we can observe
the large gap between upper and lower buccal cusps on the first molar.
SD-V9N1 CMYK.qxd:Layout 1
62
12/18/09
5:55 PM
Page 62
Spectrum dialogue Vol. 9 No. 1 January 2010
For instance, the registration of a physiological centric
relation is of major importance. The stability of dentures is
directly related to it. It is symptomatic that upper dentures
drop down irrespective of a perfect impression, when
centric is not correct. Especially in edentulous patient
cases it is difficult to obtain a reliable centric relation. The
intraoral gothic arch tracing (Fig. 11) has given most
satisfaction, especially in full denture cases, for implant
work, extensive reconstructions11 and in TMD cases12.
The Articulator, an Important Instrument in
Prosthodontics
An incorrect centric or a straight-line commonly used
articulator cannot reproduce an immediate side shift, a
Fischer angle or a correct protrusive movement. Lateral
movements, simulated without an ISS produce too steep
buccal facets on the lower molars (hyper-balances)13. The
Fischer angle is due to the transversal angulations of the
TMJ (Fig. 13). The mandibular movement back and down
occurs during swallowing and together with a lateral
displacement during chewing. (Gibbs Lundeen 14)
underneath the artificial joint. It shows an amazing
similarity between, the artificial and the natural elements.
Final Remarks
In order not to detract from the principles of the Gerber
System we have, on purpose, not gone into too many
details. It is important to understand the forces during
mastication and the way they interact. (Who knows why,
knows how!). Of course many other factors are to be
observed, from medical history to the very important
aesthetics, impression taking and many more.
The method developed by Professor Gerber15 guarantees
success when all the relevant aspects are respected. Those
aspects contain all steps of a treatment, beginning with
the first appointment, continuing with the preprosthetic
treatment, first and second impressions, centric
registration, set-up of the teeth poviding aesthetic and
static/dynamic requirements, trying-in, properly executed
Retrusive Movement
A simple test shows, if a retrusive movement exists. With
the head in an upright position and by keeping the teeth
slightly closed, incline the head backwards, a slight sliding
of the lower teeth can be observed.
With the condyle centred in its physiologic place (due
to the form of the glenoid fossa) the retrusive movement is
also oriented downwards. There is no other way for the
condyle than down because of the posterior wall (Fig. 14).
Denture occlusion must be balanced; the correct
simulation allowing the physiologic mandibular
movements is of major importance.
Fig. 9a
The Fischer Angle
During lateral movements, the roof shaped TMJ (Fig. 13),
i.e. the medial wall, is providing, together with the
condyle path inclination, an additional guidance down of
the condyle.
The pure protrusive movement and the added
inclination of the movement inward, are producing the so
called Fischer angle.
This angle becomes of importance during the simulation
of the ISS. If these angles of the medial and the external
wall are missing, the occlusion becomes too flat. Figure 15
has been composed by the transversal picture of Gerbers
first articulator from 1948 with picture 13, placed just
Fig. 9b
Figs. 9a and 9b: If sufficient space is lacking, we recommended not to
place any upper molar at all.
SD-V9N1 CMYK.qxd:Layout 1
64
12/18/09
5:56 PM
Page 64
Spectrum dialogue Vol. 9 No. 1 January 2010
Fig. 13: Frontal view of a left
Condyle. The roof shape is
clearly visible.
Fig. 10
Fig. 11
Figs. 10 and 11: Beside the static orientation of the posterior teeth,
balanced occlusion is an absolute must to protect the soft and hard
natural tissues from local overload, occurring specially during
parafunctional jaw movements.
Fig. 14: Sagittal view of a TMJ. By the form of the posterior wall
it is obvious that the retrusive movement must also be directed
downward.
Fig. 12: Gothic arch
registration of an
edentulous case to
determine centric
relation.
Fig. 15: This figure is a combination of two
pictures. The upper picture shows the artificial
fossa and the lower second picture a condyle. The
medial and external angulations of both elements
are very similar.
SD-V9N1 CMYK.qxd:Layout 1
12/18/09
5:57 PM
Page 65
Spectrum dialogue Vol. 9 No. 1 January 2010
lab procedures and remounting with perfect selective
grinding-in. All these basic rules are valid whether its
for over-dentures on implants, over-dentures on natural
roots and by partial denture cases with free end saddles16.
Acknowledgements
The authors acknowledgements go to Dr. A. Johnson, Mr. M. Boxhoorn and Mrs.
A. Bruelhart for their assistance with the translation of this article.
References
1. HILTEBRANDT, C.: Die physiologischen und statischen Grundlagen der
totalen Prothese. Published byVita Zahnfabrik GmbH Essen; 1935.
2. GERBER, A.: Die artikulre Funktion und die Schleimhautbelastung beim
Kauen von Prothesen, Vortrag am SSO-Kongress in Lugano, 1946.
3. GERBER, A.: Beitrge zur Technologie in der totalen Prothetik I & II.
Quintessenz der Zahntechnik12/ 1976; 11-21 & 3/1977; 12-21. Quintessenz
Verlags GmbH Berlin. As well pblished 1977 by Quintessenz Chicago in
english language.
4. KIMOTO, S., Gunji, A.; YAMAKAVA, A.; AJIRO H., KANNO, K.,
SHINOMIYA, M., KAWARA, M., KOBAYASHI, K.: Prospective Clinical
Trial Compairing Lingualized Occlusion to Bilateral Balanced Occlusion in
Complete Dentures: A Pilot Study. Quintessence Publishing Co. Inc., Volume
19, Number 1, 2006; 103-109
5. ATES, M., CILINGIR, A., SLN, T., SNBULOGLU, E. BOZDAG, E.:
The effect of occlusal contact localisation on the stress distribution in complete
maxillary denture. Journal of Oral Rehabilitation, 2006 33; 509-513. Blackwell
Publishing Ltd.; Oxford
65
6. PAYNE S.H.: A posterior set-up to meet individual requirements, >Dent.Dig.
1941,47: 20-22
7. GERBER, A.: Okklusion und Artikulation in der Prothetik; 1960. Published by
Condylator Service; Zurich.
8. GERBER, A.: Progress in full denture prosthesis. Int. Dental Journal 2/1957;
325.
9. GYSI, A.: Montage d'Appareils avec les Dents Anatoform et les Blocs Gysi,
12.7.1917; S. 28. De Trey & Co. Ltd. (A. Gysi, Sammelband III); Londres.
10. BOSSHART, M.: Funktion des zweiten Molaren. Das Dental Labor, Heft
6/2007 (853-854); Mnchen.
11. GOBERT, B.: Variations cliniques implantaires avec lEnregistrement IntraOral Gerber. Revue Implantologie, Mai 2006; 39-46. A. Girot, Megve France.
12. GERBER, A.; STEINHARDT G.: Dental Occlusion and Temporomandibular
Joint, 1989. Quintessence Publishing Co. Chicago.
13. GERBER, A.: Condylator Modell 4. Der Zahntechniker r. 6, 1959; 2 -19;
Schw. Zanhtenchnikervereinigung, Zrich.
14. GIBBS, C., LUNDEEN, C., MAHAN, P., Fujimoto, J.: Chewing movements
in relation to border movements at the first molar. J Prosth. Dent. 1981:
46(12); 308-322. Mosby (Elsrevier, Amsterdam).
15. HAMPSON, E.L.; M.S.D., F.D.S.; ASKEW, P.A., B.D.S., F.D.S.; TANNER,
A.N., B.D.S.; WHITE, G.E.: A technique for constructing full dentures using
the Gerber articulator and Condyloform teeth (I and II). Quintessence
International 4 and 5, 1973 (45 54, and 45 51); Chcago/Berlin.
16. GEERING; A., KUNDERT, M., KELSEY, Ch.: Complete Denture and
Overdenture Prosthetics. Thieme Medical Publishers, Inc., New York. 1993
You might also like
- Anatomy MnemonicsDocument4 pagesAnatomy Mnemonicskiara91% (56)
- The Pressurestat Model Explains The Craniosacral RhythmDocument3 pagesThe Pressurestat Model Explains The Craniosacral RhythmkabshielNo ratings yet
- Combination SyndromeDocument3 pagesCombination SyndromeNandya ZhafirahNo ratings yet
- Fixed Partial Denture 1Document93 pagesFixed Partial Denture 1siddu76No ratings yet
- Respiratory SystemDocument3 pagesRespiratory SystemAnna Dominique JimenezNo ratings yet
- Occlusion in Fixed Prosthodontics PDFDocument37 pagesOcclusion in Fixed Prosthodontics PDFfloraNo ratings yet
- Otorhinolaryngology NotesDocument25 pagesOtorhinolaryngology NotesFako Filipinas100% (3)
- Tooth Selection in Removablre DentureDocument53 pagesTooth Selection in Removablre Denturejohn mwambuNo ratings yet
- Patients Complaints Following Partial Denture InsertionDocument50 pagesPatients Complaints Following Partial Denture InsertionHector Sa50% (2)
- Let S Be Your Guide-PoundDocument8 pagesLet S Be Your Guide-PoundFaheemuddin MuhammadNo ratings yet
- Rests Rest SeatsDocument42 pagesRests Rest SeatsSahana RangarajanNo ratings yet
- Single DentureDocument37 pagesSingle DentureDentist Dina SamyNo ratings yet
- Esthetics Considerations in Complete DentureDocument34 pagesEsthetics Considerations in Complete Dentureمنتظر الحمدانيNo ratings yet
- Recent Advances in Procthodontics - LD (AMAR)Document102 pagesRecent Advances in Procthodontics - LD (AMAR)Archana PanwarNo ratings yet
- An Overview of Removable Partial DentureDocument7 pagesAn Overview of Removable Partial DenturePatra PrimadanaNo ratings yet
- Dentsply Sirona Anterior Posterior Tooth Arrangement Manual 2Document43 pagesDentsply Sirona Anterior Posterior Tooth Arrangement Manual 2Eslam ElghazoulyNo ratings yet
- Beahrs Triangle The Surgical AnatomyDocument2 pagesBeahrs Triangle The Surgical AnatomySharath ChandraNo ratings yet
- Treatment Planning Single Maxillary Anterior Implants for DentistsFrom EverandTreatment Planning Single Maxillary Anterior Implants for DentistsNo ratings yet
- Teeth Selection and ArrangementDocument118 pagesTeeth Selection and Arrangementaakankshakanwar100% (2)
- Textbook of Prosthodontics SECOND EDITIO RemovedDocument78 pagesTextbook of Prosthodontics SECOND EDITIO Removeddelfi simatupangNo ratings yet
- Prosthetic 6Document5 pagesProsthetic 6زهراء فاضل اجبير فعيلNo ratings yet
- Hanau's Quint Rudolph. L. Hanau ProposedDocument49 pagesHanau's Quint Rudolph. L. Hanau ProposedArunNo ratings yet
- Managing Problems in Complete Dentures - LectureDocument18 pagesManaging Problems in Complete Dentures - LectureMarlisa Zhong100% (1)
- Difficulties in Complete Denture Construction & Solutions IIDocument13 pagesDifficulties in Complete Denture Construction & Solutions IIIndrani DasNo ratings yet
- Basic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionFrom EverandBasic Level of Dental Resins - Material Science & Technology: 4th Edition, 2nd VersionNo ratings yet
- Jaw Relation Record, Lec 6Document12 pagesJaw Relation Record, Lec 6JustDen09100% (1)
- THE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSFrom EverandTHE ORTHODONTIC ROADMAP: GUIDELINES FOR THE DIAGNOSIS AND TREATMENT OF ORTHODONTIC MALOCCLUSIONSNo ratings yet
- Nsal InstillationDocument4 pagesNsal InstillationNeelofur Ibran Ali100% (4)
- Basic Principles of Obturator Design For Partially Edentulous Patients. Part I: ClassificationDocument69 pagesBasic Principles of Obturator Design For Partially Edentulous Patients. Part I: ClassificationDrFarha NazNo ratings yet
- 5 Elements of Abdominal DiagnosisDocument14 pages5 Elements of Abdominal Diagnosiscelliastt100% (3)
- Incisal Guidance & Anterior Occlusion TypesDocument14 pagesIncisal Guidance & Anterior Occlusion TypesAmar BhochhibhoyaNo ratings yet
- Over Dentures Jan 2012Document40 pagesOver Dentures Jan 2012Mohsin HabibNo ratings yet
- Denu 2017 44 9 821Document7 pagesDenu 2017 44 9 821Yolanda EvansNo ratings yet
- 06 Silverman 1953 The Speaking Method in Measuring Vertical DimensionDocument7 pages06 Silverman 1953 The Speaking Method in Measuring Vertical DimensionCoRal Partida BenitezNo ratings yet
- Denture Insertion, Patient Education and ManagementDocument46 pagesDenture Insertion, Patient Education and ManagementkaliapreetiNo ratings yet
- Relining and Rebasing of Complete Dentures: Bds MSC MRD Rcsed 4 Year/removable Prosthodontics 441-442Document33 pagesRelining and Rebasing of Complete Dentures: Bds MSC MRD Rcsed 4 Year/removable Prosthodontics 441-442Aya ShahrouriNo ratings yet
- DentureDocument80 pagesDentureDrShweta SainiNo ratings yet
- Prostho Lec - OverdenturesDocument14 pagesProstho Lec - Overdenturesdrgayen6042No ratings yet
- CD Relining & Rebasing Complete DenturesDocument42 pagesCD Relining & Rebasing Complete DenturesMohsin HabibNo ratings yet
- Lingualized Occlusion in RDPDocument37 pagesLingualized Occlusion in RDPmujtaba100% (1)
- Dent 343 Lect 9 - HandoutDocument18 pagesDent 343 Lect 9 - HandoutAnas AmerNo ratings yet
- Complete Denture StabilityDocument5 pagesComplete Denture StabilityAmit ShivrayanNo ratings yet
- The Neutral Zone in Complete DenturesDocument8 pagesThe Neutral Zone in Complete DenturesToDownload81No ratings yet
- Journal of Prosthetic DentistryDocument7 pagesJournal of Prosthetic DentistryAmar BhochhibhoyaNo ratings yet
- 10 Non-Anatomic Tooth Arrangement 1-16 at 96 DpiDocument89 pages10 Non-Anatomic Tooth Arrangement 1-16 at 96 Dpitrangy77No ratings yet
- Surgical Extrusion: A Dental TechniqueDocument6 pagesSurgical Extrusion: A Dental TechniqueDragos CiongaruNo ratings yet
- Waxing and Carving of Complete DentureDocument9 pagesWaxing and Carving of Complete Dentureعبدالرحمن عدي عبدالفتاحNo ratings yet
- Repair of Complete DenturesDocument25 pagesRepair of Complete Denturesjohn mwambu100% (2)
- Impression C DDocument48 pagesImpression C DZaid KhameesNo ratings yet
- Prosthodontic Diagnostic Index (PDI) Classification SystemDocument1 pageProsthodontic Diagnostic Index (PDI) Classification SystemevvallartaNo ratings yet
- Posterior Palatal Seal and Speech Considerations With Complete DenturesDocument32 pagesPosterior Palatal Seal and Speech Considerations With Complete Denturesasop06No ratings yet
- Amalgam Cavity Preparation Class 1Document51 pagesAmalgam Cavity Preparation Class 1Hadil Altilbani100% (1)
- Fiber Post System - Critical ReviewDocument7 pagesFiber Post System - Critical ReviewKirti SharmaNo ratings yet
- Fundamentals of Cavity PreparationDocument76 pagesFundamentals of Cavity Preparationragakodali0% (1)
- Space MaintenanceDocument44 pagesSpace Maintenancedr parveen bathlaNo ratings yet
- Finish LinesDocument17 pagesFinish LinesWaseem AhmedNo ratings yet
- Lingualised Occ RevisitedDocument5 pagesLingualised Occ RevisitedDrPrachi AgrawalNo ratings yet
- Retention of Teeth for OverdenturesDocument29 pagesRetention of Teeth for OverdenturesShyam K MaharjanNo ratings yet
- Lingualized Occlusion ReviewDocument3 pagesLingualized Occlusion ReviewJessy ChenNo ratings yet
- Prosthodontics LL Laboratory 3Document22 pagesProsthodontics LL Laboratory 3براءة أحمد السلامات100% (1)
- Support - Complete DentureDocument25 pagesSupport - Complete DentureSalim MalikNo ratings yet
- Fixed Orthodontic Appliances: A Practical GuideFrom EverandFixed Orthodontic Appliances: A Practical GuideRating: 1 out of 5 stars1/5 (1)
- Essential Tissue Healing of the Face and NeckFrom EverandEssential Tissue Healing of the Face and NeckRating: 5 out of 5 stars5/5 (2)
- How To Lose WeightDocument2 pagesHow To Lose WeightAdroit JayTrishNo ratings yet
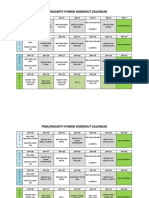
- Hybrid Workout P90x/insanityDocument3 pagesHybrid Workout P90x/insanityVelagarza92100% (1)
- Throat AnatomyDocument70 pagesThroat AnatomyMegan ShanzuNo ratings yet
- Erb's Palsy: Deformity, Nerve Roots, and TreatmentDocument1,852 pagesErb's Palsy: Deformity, Nerve Roots, and TreatmentSK RaulNo ratings yet
- Abdominal Wall: Um-Hani'S Qbank Um-Hani'S QbankDocument5 pagesAbdominal Wall: Um-Hani'S Qbank Um-Hani'S QbankmedisharedNo ratings yet
- PSAU Toad DissectionDocument10 pagesPSAU Toad DissectionCatilago ClarissaNo ratings yet
- Try-In of The Trial Denture by Dr. Mahmoud RamadanDocument9 pagesTry-In of The Trial Denture by Dr. Mahmoud RamadanDrRahul Puri GoswamiNo ratings yet
- Physiology A (GLORIANIESCOTO) - Gastrointestinal Tract Physiology Part 1Document7 pagesPhysiology A (GLORIANIESCOTO) - Gastrointestinal Tract Physiology Part 1Raian Isabelo SuyuNo ratings yet
- E5 - Makalah Pleno Blok 7 Sken 2Document20 pagesE5 - Makalah Pleno Blok 7 Sken 2Dian PalinNo ratings yet
- Clinical Teaching Birth InjuriesDocument15 pagesClinical Teaching Birth InjuriesAjit M Prasad PrasadNo ratings yet
- Ayesha MuzaffarDocument31 pagesAyesha MuzaffarpashaNo ratings yet
- MBCHB Semester 2Document15 pagesMBCHB Semester 2Muhindi JoanNo ratings yet
- What Are The Symptoms of Hydronephrosis?Document10 pagesWhat Are The Symptoms of Hydronephrosis?Rajendra GautamNo ratings yet
- 4 NCV1Document115 pages4 NCV1sridhar100% (2)
- 01.2 Craniotomy and CraniectomyDocument1 page01.2 Craniotomy and Craniectomyfebi novrizalNo ratings yet
- Middle Ear AnatomyDocument28 pagesMiddle Ear AnatomySriharsha TikkaNo ratings yet
- Hormones Endocrine Gland: (Clipart Edited From Corel Presentations 8)Document3 pagesHormones Endocrine Gland: (Clipart Edited From Corel Presentations 8)Zheena S. JaroNo ratings yet
- Principles and Pitfalls in Coronary Vasomotor Function TestingDocument26 pagesPrinciples and Pitfalls in Coronary Vasomotor Function TestingRamón López PalopNo ratings yet
- Arteries of Lower LimbDocument6 pagesArteries of Lower LimbAlli NdahuraNo ratings yet
- Angsoka Ward Patient ListDocument136 pagesAngsoka Ward Patient ListngurahNo ratings yet
- A Double Reverse Kleinert Extension Splint For Extensor Tendon Repairs in Zones VI To VIIIDocument3 pagesA Double Reverse Kleinert Extension Splint For Extensor Tendon Repairs in Zones VI To VIIIElizabeth BrugesNo ratings yet
- Medi Pro: Instruction ManualDocument69 pagesMedi Pro: Instruction ManualVivian Marcela Arias BernalNo ratings yet
- Management of Ureteral InjuryDocument8 pagesManagement of Ureteral Injuryfpampaloni1970100% (1)